Levitra enthält Vardenafil, das eine kürzere Wirkdauer als Tadalafil hat, dafür aber schnell einsetzt. Männer, die diskret bestellen möchten, suchen häufig nach levitra kaufen ohne rezept. Dabei spielt die rechtliche Lage in der Schweiz eine wichtige Rolle.
Microsoft powerpoint - vajer.peter-smoking.cessation.ppt


Section 1: Burden of Disease
Tobacco Dependence, Attitudes
� Smoking is highly prevalent worldwide
and Treatment Strategies
� Smoking increases morbidity and mortality� The benefits of quitting have been
Department of Family Medicine
Semmelweis University
Gender-Specific Smoking
Smoking Prevalence of Adults vs
Prevalence Across the World
Youths: Young People Are Also at Risk
1.25 billion smokers worldwide1-2
*Young men/women = 15-year-old students who smoke cigarettes.
1. Shafey O, et al (eds). Tobacco Control Country Profiles 2003, American Cancer Society, Atlanta, Georgia, 2003. Available at: http://www.who.int/tobacco/globaldata/countryprofiles/en/. 2. Mackay J, et al. The Tobacco Atlas. Second
1. Mackay J, et al. The Tobacco Atlas. Second Ed. American Cancer Society Myriad Editions Limited, Atlanta,
Edition. American Cancer Society Myriad Editions Limited. Atlanta, Georgia, 2006. Also available online at:
Georgia, 2006. Also available online at: http://www.myriadeditions.com/statmap/.
Smoking: Leading Preventable
US Mortality From Smoking-Related
Cause of Disease and Death1
Top 3 Smoking-Attributable Causes of Death in US
#2 Ischemic heart disease
Lung (#1)* Leukemia
(AML, ALL, CLL)2-4
Pregnancy complications
Lung, Trachea, Bronchus Cancer †
Oral cavity/pharynx Laryngeal
Reduced fertility
Esophageal Stomach
Sudden Infant Death Syndrome
Ischemic Heart Disease †
Pancreatic Kidney
Respiratory Diseases
Cerebrovascular Disease
Ischemic heart disease (#2)*
Adverse surgical outcomes/wound healing
Stroke – Vascular dementia5
Peripheral vascular disease6
Abdominal aortic aneurysm
Peptic ulcer disease†
COPD (#3)*Pneumonia
Poor asthma control
Approximately 438,000 annual US deaths attributable to cigarette smoking
*Top 3 smoking-attributable causes of death. †In patients who are Helicobacter pylori positive.
AML = Acute myeloid leukemia; ALL = acute lymphocytic leukemia; CLL = chronic lymphocytic leukemia; COPD =
between 1997 and 2001
chronic obstructive pulmonary disease; SIDS = sudden infant death syndrome.
1. Surgeon General's Report. The Health Consequences of Smoking; 2004. 2. Sandler DP, et al. J Natl Cancer Inst. 1993;85(24):1994-2003. 3. Crane MM, et al. Cancer Epidemiol Biomarkers Prev. 1996;5(8):639-
*Percentage of deaths attributable to specific smoking-related diseases, 1997–2001.
644. 4. Miligi L, et al. Am J Ind Med. 1999;36(1):60-69. 5. Roman GC. Cerebrovasc Dis. 2005;20(Suppl 2):91-100. 6.
†Includes secondhand smoke deaths.
Willigendael EM, et al. J Vasc Surg. 2004;40:1158-1165.
1. CDC. MMWR. 2005;54:625–628.
Annual Deaths Attributable to
Four Stages of the Tobacco Epidemic:
Tobacco: Worldwide Estimates
Mortality Is Increasing in Many Countries1
% of Total Deaths Attributable to Tobacco*
Russian Federation
• Eastern Europe
• Western Europe,
• Southern Europe
• Southeast Asia
• Latin America
If current smoking patterns continue, deaths from smoking in Asia—home to a third of
the world's population—are expected to increase by 2020 to 4.9 million annually.2
1. Lopez AD, et al. Tobacco Control. 1994;3:242-247. 2. Shafey O, et al (eds). Tobacco Control Country Profiles 2003,
*Regional estimates in 2000 in men aged >35 years.
American Cancer Society; 2003; Atlanta, Georgia. Available at:
1. Mackay J, Eriksen M. The Tobacco Atlas. Second Ed. World Health Organization; 2006.
Smoking Reduces Survival an
What's in a Cigarette?
Average of 10 Years
Results From a Study of Male Physician Smokers in the United Kingdom
� Tobacco smoke: ≥4000 chemicals, ≥250 toxic or
Chemical in Tobacco Smoke2
Physician Nonsmokers
Physician Smokers
Car exhaust fumes
Industrial solvent
� Nicotine is addictive, but not carcinogenic3
� Smoking cigarettes with lower tar and nicotine
provides no health benefit4
1. National Toxicology Program. 11th Report on Carcinogens; 2005. Available at: http://ntp-server.niehs.nih.gov. 2. Mackay J, Eriksen M. The Tobacco Atlas. World Health Organization; 2006. 3. Harvard Health Letter. May 2005. 4.
1. Doll R, et al. BMJ. 2004;328:1519–1527.
Surgeon General's Report. The Health Consequences of Smoking; 2004.
Mechanisms of Action:
What Does Secondhand Smoke Do?
How Smoking Causes Disease
� Estimated lung cancer risk increased by
– Direct respiratory cell exposure to potent mutagens
and carcinogens in tobacco smoke
� Believed to cause and worsen diseases such as
� Ischemic heart disease
asthma, COPD, and emphysema2
– Toxic products in the bloodstream create a
� Increases risk for developing heart disease by
pro-atherogenic environment
– Leads to endothelial injury and dysfunction,
� Increases risk of nonfatal acute myocardial
thrombosis, inflammation, and adverse lipid profiles
infarction in a graded manner3
� Chronic Obstructive Pulmonary Disease (COPD)
– Accelerated decline in respiratory function
1. News release, June 27, 2006; US Department of Health & Human Services. Available at: http://www.hhs.gov/news/press/2006pres/20060627.html. 2. Mackay J, et al. The Tobacco Atlas. World Health
1. Surgeon General's Report. The Health Consequences of Smoking; 2004.
Organization; 2002. 3. Teo KK, et al. Lancet. 2006;368:647-658.

What Does Secondhand Smoke Do
Smoking During Pregnancy
to Infants and Children?
� Almost 60% of US children are exposed to secondhand smoke1
� Exposure during pregnancy associated with1–3
� In some countries, ≥80% of youth live in homes where others smoke
– Increased risk of miscarriage, stillbirth, sudden infant
in their presence2
death syndrome (SIDS); eg
� Secondhand smoke increases disease burden and hospitalisation in
infants and children. For example:
– Low-birth weight
– UK - 17,000 children under the age of 5 years hospitalised annually3
• 4-fold risk1: eg, 9700–18,600 cases related to secondhand
– Australia - 56% higher risk for hospitalisation if mother smoked in same
smoke annually in US*3
room as infant, 73% if smoked while holding infant, and 95% if smoked
– Impaired infant lung function2
while feeding infant (N = 4486)4
– Hong Kong - higher likelihood for hospitalisation for infants living with
– Possible association with cognitive and
any smoker at home with poor smoking hygiene (<3 metres away)5
1. Secondhand smoke; Fact sheet, June 2006. Available at:
http://www.cdc.gov/tobacco/factsheets/secondhand_smoke_factsheet.htm. 2. Mackay J, Eriksen M. The Tobacco
1. Fagerström K. Drugs. 2002;62(Suppl 2):1–9. 2. Le Souef PN. Thorax. 2000;55:1063–1067.
Atlas. World Health Organization; 2006. 3. Fagerstrom K. Drugs. 2002;62(suppl 2):1-9. 4. Blizzard L, et al. Arch
3. Mackay J, et al. The Tobacco Atlas. World Health Organization; 2002. 4. Hellstrom-Lindahl E,
Pediatr Adolesc Med. 2004;158:687-693. 5. Leung GM, et al. Arch Pediatr Adolesc Med. 2004;158:687-693.
et al. Respiration. 2002;69:289-293.
Importance of NOT Smoking
Why Quit? Potential Lifetime Health
Benefits of Quitting Smoking
Cardiovascular heart disease (CHD) risk is similar to never smokers
Rate of Infants with Low-Birth Weight
Lung cancer risk is 30-50% that of continuing smokers
in Taiwanese Infants by Smoking Status of the Mother (N=9499)
Stroke risk returns to the level of people who have never
smoked at 5-15 years post-cessation
CHD: excess risk is reduced by 50%
Lung function may start to improve
with decreased cough, sinus
congestion, fatigue, and shortness of
Rate of Infants With
Low Birth Weight
Never Smoked Quit Smoking‡
1. CDC. Surgeon General Report 2004: http://www.cdc.gov/tobacco/sgr/sgr_2004/sgranimation/flash/index.html. American Cancer Society. Guide to Quitting Smoking. Available at: http://www.cancer.org. Accessed June 2006. 2. American Cancer Society. Guide to Quitting Smoking. Available at: http://www.cancer.org. Accessed June 2006. 3.US Department of Health & Human Services. The Health Benefits of Smoking Cessation: A Report of the Surgeon
†P<0.05 vs never smoked. ‡Before or during first trimester.
General. Centers for Disease Control and Prevention (CDC), Office on Smoking and Health. 1990. Available at:
1. Wen CP, et al. Tob Control. 2005;14(Suppl 1):i56–i61.
http://profiles.nlm.nih.gov/NN/B/B/C/T/. Accessed July 2006.
Quitting at Any Age May Increase
Quitting at Any Age May Increase
Results From a Study of Male Physician Smokers in the United Kingdom
Results From a Study of Male Physician Smokers in the United Kingdom
Stopped Age 55-64
Stopped Age 45-54
Cigarette Smokers
Cigarette Smokers
1. Doll R, et al. BMJ. 2004;328:1519–1527.
1. Doll R, et al. BMJ. 2004;328:1519–1527.

Quitting at Any Age May Increase
Risk of Cardiovascular Disease
(CVD) Reduced By Quitting Smoking
Results From a Study of Male Physician Smokers in the United Kingdom
Stopped Age 35-44
Cigarette Smokers
� Quitting associated with
– 36% reduction in odds of all-cause mortality among patients with
coronary heart disease (CHD)1
– Decreases in CVD events in cardiac patients, even in those who
� Quitting sooner appears most beneficial
*Defined as self-reported smokers who were cotinine negative.
1. Doll R, et al. BMJ. 2004;328:1519–1527.
1. Critchley JA, Capewell S. JAMA. 2003;290:86-97. 2. Twardella D et al. Eur Heart J. 2004;25:2101–2108.
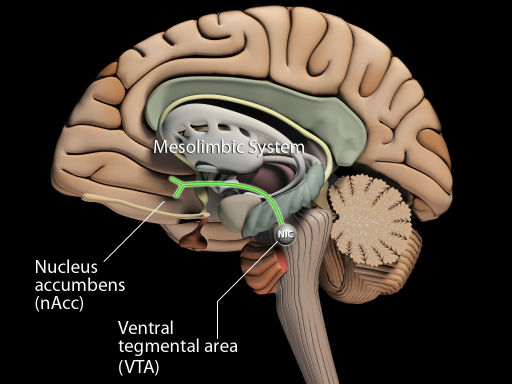
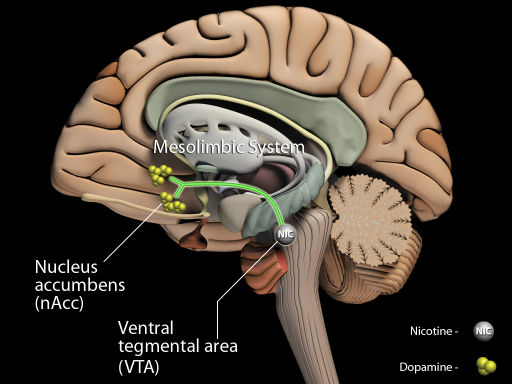
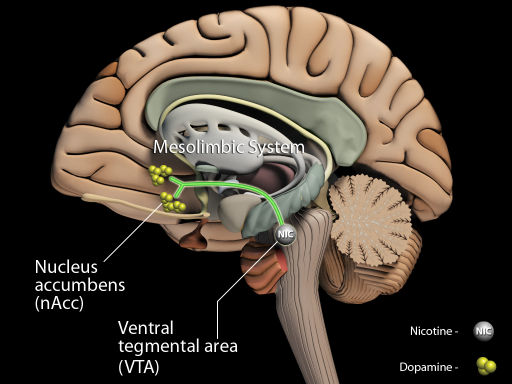
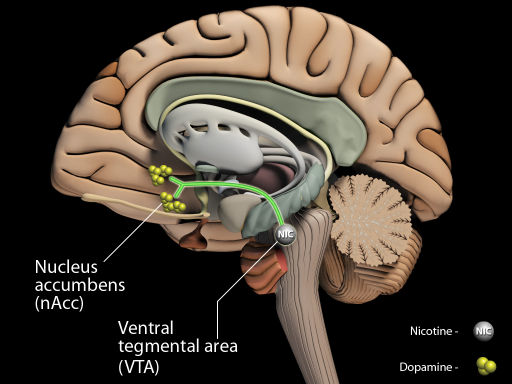
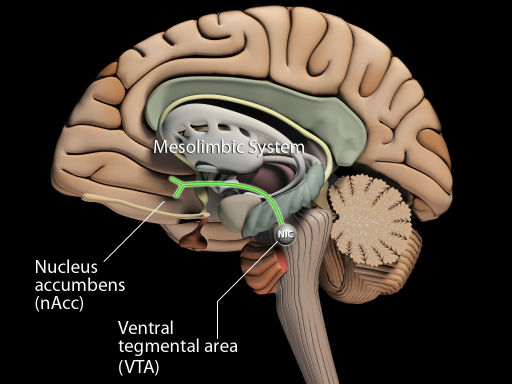
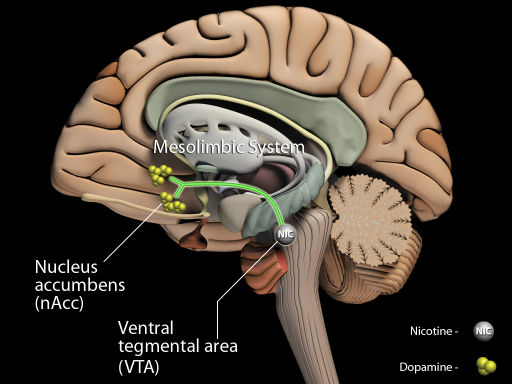
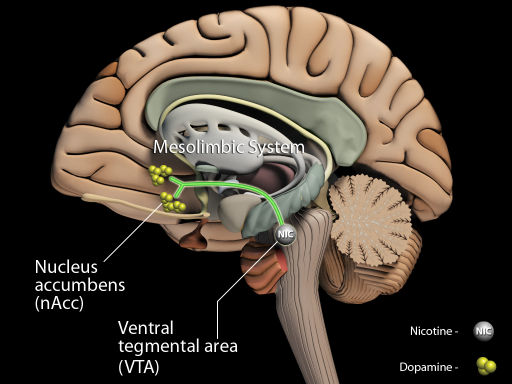
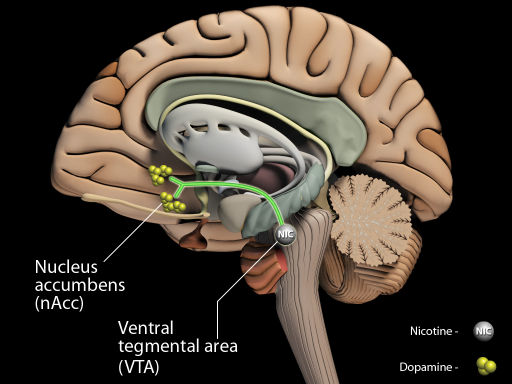
Mechanism of Action of Nicotine in
the Central Nervous System
Tobacco Dependence
and Treatment Strategies
Nicotinic Receptor
Nicotine binds preferentially to nicotinic acetylcholinergic (nACh) receptors in the central nervous system; the primary is the α4β2 nicotinic receptor in the Ventral Tegmental Area (VTA)
After nicotine binds to the α4β2 nicotinic receptor in the VTA, it results in a release of dopamine in the Nucleus Accumbens (nAcc) which is believed to be linked to reward
Nicotine Stimulates Dopamine
Nicotine May Cause Up-Regulation and
Desensitization of Receptors Resulting in
� Nicotine activates α4β2 nicotinic receptors in the ventral
� Tolerance typically develops after long-term nicotine use1
tegmental area resulting in dopamine release at the
� Tolerance is related to both the up-regulation (increased number)
nucleus accumbens. This may result in the short-term
and the desensitization of nicotine receptors in the VTA1
reward/satisfaction associated with cigarette smoking.
� A drop in nicotine level, in combination with the up-regulation and
decreased sensitivity of the nicotinic receptor, can result in withdrawal symptoms and cravings1
� Smokers have the ability to self regulate nicotine intake by the
frequency of cigarette consumption and the intensity of inhalation1
� In order to maintain a steady nicotine level, smokers generally titrate
their smoking to achieve maximal stimulation and avoid symptoms
of withdrawal and craving2
− α4β2 Nicotinic Receptor
Adapted from Picciotto MR, et al. Nicotine and Tob Res. 1999: Suppl 2:S121-S125.
1. Schroeder SA. JAMA. 2005;294:482-487. 2. Jarvis MJ. BMJ. 2004; 328:277-279.
The Cycle of Nicotine Addiction
So Why Do People Smoke?
� Nicotine binding causes an increase in
Addiction – Habitual psychological and physiological dependence
release of Dopamine1,2
on substance or practice which is beyond voluntary control
� Dopamine gives feelings of pleasure
– Stedman's Medical Dictionary
� The Dopamine decrease between
� Since at least the 1988 Surgeon General's Report1
cigarettes leads to withdrawal symptoms of irritability and stress1
– Addiction defined as compulsive use despite damage to the
� The smoker craves Nicotine to release
individual or society and drug-seeking behavior can take
more Dopamine to restore pleasure
precedence over important priorities
– Addiction persists despite a desire to quit or even repeated
� Competitive binding of Nicotine to
nicotinic acetylcholinergic receptors causes prolonged activation,
� Most people smoke primarily because they are addicted
desensitization, and upregulation2
� As Nicotine levels decrease, receptors
revert to an open state causing
� There is a clear link between smoking, nicotinic
hyperexcitability leading to cravings1,2
receptors, and addiction2
1. Centers for Disease Control and Prevention. The Health Consequences of Smoking: Nicotine Addiction; A Report of the Surgeon General. Washington DC: US Department of Health and Human Services; 1988.
1. Jarvis MJ. BMJ. 2004; 328:277-279. 2. Picciotto MR, et al. Nicotine and Tob Res. 1999: Suppl 2:S121-S125.
2. Jarvis MJ. BMJ. 2004;328:277-279.
Nicotine Addiction: A Chronic
Tobacco Dependence and Environmental
Relapsing Medical Condition
Behavior Reinforcement
� True drug addiction1� Requires long-term clinical intervention, as do other addictive
� Pharmacologic effects
– Nicotine is a primary reinforcer
– Failure to appreciate the chronic nature of nicotine addiction
� Non-pharmacologic effects
• Impair clinicians' motivation to treat tobacco dependence long-term
– Environmental/social stimuli associated with smoking
• Impede acceptance that condition is comparable to diabetes,
play a role in reinforcing nicotine dependence
hypertension, or hyperlipidemia, and requires counseling, support, and appropriate pharmacotherapy
– Environmental/social stimuli enhance the reinforcing
effects of nicotine
– The nature of addiction, not the failure of the individual3
Direct pharmacologic effects of nicotine are necessary but not
• Long-term smoking abstinence in those who try to quit unaided† = 3%–5%
sufficient to explain tobacco dependence; these effects
• Most relapse within the first 8 days
must take into account the environmental/social context
in which the behavior occurs
1. Fiore MC, Bailey WC, Cohen SJ, et al. Clinical Practice Guideline: Treating Tobacco Use and Dependence. US Department of Health and Human Services. Public Health Service; June 2000. Available at: www.surgeongeneral.gov/tobacco/default.htm. 2. Jarvis MJ. Why people smoke. BMJ. 2004;328:277-279.
1. Caggiula AR et al. Psychol Behavior. 2002;77:683–687.
Withdrawal Syndrome: a Combination of
Why Some Smokers May Need More
Physical and Psychological Conditions, Making
Smoking Hard to Treat1,2
Withdrawal Syndrome
� Studies show some groups may be less
frustration, or anger
– Higher level of dependence1
Increased appetite
• Cigarettes per day
(may increase or
• Time to first cigarette upon awakening
with quitting)1,2
– Living with a current smoker1
– Fewer educational qualifications2
– Lower socioeconomic class2
Difficulty concentrating
– Co-morbid psychiatric disorders3
1. Diagnostic and Statistical Manual of Mental Disorders, IV-TR. Washington, DC: APA; 2006: Available at http://psychiatryonline.com. Accessed November 7, 2006. 2. West RW, et al. Fast Facts: Smoking Cessation. 1st ed.
1. Hyland A et al. Nicotine Tob Res. 2004;6(Suppl 3):S363-S369. 2. Chandola T et al. Addiction. 2004;99:770-777.
Oxford, United Kingdom. Health Press Limited. 2004.
3. Kalman D et al. Am J Addict. 2005;14:106–123.
Multiple Quit Attempts
Most Smokers Are Willing to
� More than 70% of US smokers have attempted to quit1
� Of smokers who relapsed following a quit
– Approximately 46% try to quit each year
– Less than 5% who try to quit are abstinent 1 year later
– 98% were willing to try again
– Similar percentages in countries with established tobacco control
programs (eg, Australia, Canada, UK)2
– 50% immediately
• 30% to 50% try to quit; <5% achieve long-term abstinence
– 28% within 1 month
� Some smokers succeed after making several attempts3
� Of those willing to try again immediately
– Past failure does not prevent future success
– Percentage did not differ based on time since
– Length of prior abstinence is related to quitting success
� Some smokers may prefer a waiting period
before attempting to quit again
1. Fiore MC, et al. US Department of Health and Human Services. Public Health Service. June 2000. 2. Foulds J, et al. Expert Opin Emerg Drugs. 2004;9:39–53. 3. Grandes G, et al. Br J Gen Pract. 2003;53:101–107.
1. Joseph A, et al. Nicotine Tob Res. 2004;6:1075–1077.
Length of Prior Abstinence Is
Related to Quitting Success
Advice and Support
� Previous quit attempts of ≥ 3 months
� All smokers should be1
positively predicted sustained,
– Advised to quit (the "5As")
– Offered assistance irrespective of motivation
biochemically confirmed abstinence1
� Three types of non-pharmacologic therapies are
– N = 1768; OR* = 1.8; 95% CI = 1.1–2.7
– Practical counseling (problem solving/skills training)
� Duration of previous quit attempts
– Social support as part of treatment
influenced continuous abstinence at 6
– Securing social support outside of treatment
� Effectiveness increases with treatment intensity1,2
– N = 509; OR* = 1.73; 95% CI = 1.09–2.75
1. Fiore MC, et al. Clinical Practice Guideline: Treating Tobacco Use and Dependence. US Department of Health and Human Services. Public Health Service; June 2000. Available at: www.surgeongeneral.gov/tobacco/default.htm.
*OR = odds ratio.
2. National Institute for Health and Clinical Excellence. Brief interventions and referral for smoking cessation in
1. Grandes G et al. Br J Gen Pract. 2003;53:101–107. 2. Aubin HJ et al. Addiction. 2004;99:1206-1218.
primary care. Available at: www.nice.org.uk/page.aspx?o=299611. Accessed September 2006.
Tobacco Dependence Support:
The "5As": Ask About Tobacco Use
� Identify and document tobacco use status for
� Ask about tobacco use
every patient at every visit
� Implement an office-wide system that ensures
� Assess willingness to make a quit attempt
tobacco-use status is queried and documented
� Assist in quit attempt
– Expand vital sign documentation to include tobacco
� Arrange follow-up
– Tobacco-use stickers on charts
– Computer reminder systems for electronic medical
1. Fiore MC, et al. US Department of Health and Human Services. Public Health Service. June 2000.
1. Fiore MC, et al. US Department of Health and Human Services. Public Health Service. June 2000.
The "5As": Assess Willingness to
The "5As": Advise to Quit
Make a Quit Attempt
� In a clear, strong, and personalized manner, urge every
tobacco user to quit at least once per year
� Is the tobacco user willing to make a quit attempt
• "I think it is important for you to quit smoking now, and I can help
– If patient is willing to attempt quitting, offer assistance
– If patient is unwilling to quit now, provide motivational
• "As your clinician, I need you to know that quitting smoking is very
important to protecting your health now and in the future."
• Tie tobacco use to health/illness (reason for office visit),
social/economic costs, motivation level, and impact on others (children)
1. Fiore MC, et al. US Department of Health and Human Services. Public Health Service. June 2000.
1. Fiore MC, et al. US Department of Health and Human Services. Public Health Service. June 2000.
The "5As": Assist in Quit Attempt
The "5As": Arrange Follow-up
� For the patient willing to make a quit attempt, use
� Schedule follow-up contact, preferably within the first
counseling and pharmacotherapy
week after the quit date
– Provide practical counseling (problem solving and skills training)
� Follow-up can occur either in person or via telephone
– Provide social support
� Follow-up actions
– Offer pharmacotherapy as appropriate
– Congratulate success
– Provide supplementary materials
– Review circumstances of lapse – elicit recommitment to
• World Health Organization: www.who.int
• Centers for Disease Control and Prevention: www.cdc.gov/tobacco
– Identify and anticipate challenges
• Society for Research on Nicotine and Tobacco: www.srnt.org
– Assess pharmacotherapy use
– Consider need for referral to formal program
– Consider referral for more intensive treatment
• Telephone or internet-based
1. Fiore MC, et al. US Department of Health and Human Services. Public Health Service. June 2000.
1. Fiore MC, et al. US Department of Health and Human Services. Public Health Service. June 2000.
Patient Satisfaction Linked With
Effectiveness Increases with
"5A" Interventions
Treatment Intensity
� Regardless of readiness to quit, smokers receiving 5A
interventions were more satisfied with their health care
Minimal Counseling
13.4 (10.9, 16.1)
(less than 3 minutes)
Low Intensity Counseling
16.0 (12.8, 19.2)
(3 to 10 minutes)
Higher Intensity Counseling
22.1 (19.4, 24.7)
(more than 10 minutes)
Very Satisfied (%)
N=1160. *P<0.0001; †P= 0.0014.
1. Fiore MC, et al. Clinical Practice Guideline: Treating Tobacco Use and Dependence. US Department of Health and
1. Conroy MB, et al. Nicotine Tob Research 2005;7(Suppl 1):S29–S34.
Human Services. Public Health Service; June 2000. Available at: www.surgeongeneral.gov/tobacco/default.htm.
Pharmacotherapy for Tobacco
for Smoking Cessation
� Nicotine replacement therapy (NRT)1
– Long acting1-3
Physician advice1
Brief vs no advice (usual care)
1.74 (1.48–2.05)
Intensive vs minimal advice
1.44 (1.24–1.67)
– Short acting1-3
Individual counseling2
Vs minimal behavior intervention
1.56 (1.32–1.84)
Group counseling3
2.04 (1.60–2.60)
Vs no intervention
2.17 (1.37–3.45)
• Sublingual tablets/lozenges
Proactive Telephone counseling4
� Antidepressants4
Vs less intensive interventions
1.56 (1.38–1.77)
– Bupropion SR4
Vs no intervention
1.24 (1.07–1.45)
– Nortriptyline3 (not approved for smoking cessation)
*Abstinence assessed at least 6-months following intervention.
1. Lancaster T, Stead LF. Cochrane Database Syst Rev. 2004;(4):CD000165. 2. Lancaster T, Stead LF. Cochrane Database Syst Rev. 2005;(2):CD001292. 3. Stead LF, Lancaster T. Cochrane Database Syst Rev. 2005;(4):
1. Silagy C, et al. Cochrane Database Syst Rev. 2004;(3):CD000146. 2. Stead L, et al. Int J Epidemiol.
CD001007. 4. Stead LF et al. Cochrane Database Syst Rev. 2005;(4):CD002850. 5. Lancaster T, Stead LF. Cochrane
2005;34:1001–1003. 3. Henningfield JE, et al. CA Cancer J Clin. 2005;55:281-299.
Database Syst Rev. 2005;(3):CD001118.
4. Hughes JR et al. Cochrane Database Syst Rev. 2004;(4):CD000031.
Nicotine Replacement Therapy (NRT): Nicotine
Nicotine Replacement Therapy (NRT)
Delivery by Cigarettes and NRT Products
Cigarette (nicotine delivery, 1-2 mg)
Gum (nicotine delivery, 4 mg)
– NRT has been shown to be safe and effective in
Nasal spray (nicotine delivery, 1 mg)
helping people stop using cigarettes when used as
Transdermal patch
part of a comprehensive smoking cessation program1
� Delivers nicotine that binds to the nAChR
� Does not generally counter the additional
satisfaction from smoking1
� NRTs may not deliver nicotine to the circulation
as fast as smoking2
80 90 100 110 120
Time post-administration (minutes)
1. American Heart Association website: http://www.americanheart.org/presenter.jhtml?identifier=4615, accessed November 5, 2006. 2. Sweeney CT, et al. CNS Drugs. 2001;15:453-467.
1. Sweeney CT, et al. CNS Drugs. 2001;15:453-467.
Efficacy of Nicotine Replacement
Bupropion SR (Zyban®)
� ZYBAN (bupropion SR hydrochloride) is a non-
nicotine sustained-release tablet for smoking
1.66 (1.52–1.81)
� Initially developed as an antidepressant, later
1.81 (1.63–2.02)
found to have efficacy in smoking cessation1
2.35 (1.63–3.38)
� There are 2 potential MOAs:
2.14 (1.44–3.18)
– Blocks reuptake of dopamine2,3– Non-competitive inhibition of α3β2 and α4β2 nicotine
2.05 (1.62–2.59)
Combination vs single type
1.42 (1.14–1.76)
Any NRT vs control
1.77 (1.66–1.88)
1. Package Insert. bupropion SR hydrocloride [Zyban®]. GlaxoSmithKline. 2. Henningfield JE, et al. CA Cancer J Clin.
1. Silagy C et al. Cochrane Database Syst Rev. 2004;(3):CD000146. 2. Stead L, Lancaster T. Int J Epidemiol.
2005;55:281–299. 3. Foulds J, et al. Expert Opin Emerg Drugs. 2004;9:39–53. 4. Slemmer JE, et al. J Pharmacol
Exp Ther. 2000;295:321–327. 5. Roddy E. Br Med J. 2004;328:509–511.
Comparison of Nicotine Replacement Therapy (NRT)
Champix (varenicline): A Highly
and Bupropion SR Therapy for Quitting Smoking1
Selective α4β2 Receptor Partial Agonist
� Only study comparing NRT and antidepressant
therapy for quitting smoking2
Placebo (n = 160)
Nicotine Patch (n = 244)
Bupropion SR (n = 244)
Bupropion SR + Patch (n = 245)
Binding of nicotine at the α4β2 nicotinic receptor
Champix is an α4β2 nicotinic receptor partial agonist,
in the VTA is believed to cause release of
a compound with dual agonist and antagonist
dopamine at the nAcc
activities. This is believed to result in both a lesser amount of dopamine release from the VTA at the
nAcc as well as the prevention of nicotine binding at
1 Year Continuous Abstinence
the α4β2 receptors.
(Week 2 to Week 52)
1. Coe JW et al. Presented at the 11th Annual Meeting and 7th European Conference of the Society for Research on
*P ≤ 0.001 vs placebo and patch alone.
Nicotine and Tobacco. 2005. Prague, Czech Republic. 2. Picciotto MR et al. Nicotine Tob Res. 1999; Suppl 2:S121-
1. Jorenby DE, et al. N Engl J Med. 1999;340:685–691. 2. Talwar A et al. Med Clin North Am. 2004;88:1517–1534.
Varenicline Mechanism of Action:
1: Findings from the STOP survey
Efficacy for Tobacco Dependence
� Efficacy of varenicline in tobacco dependence
Other things have higher priority
– Believed to result from partial agonist activity at the α4β2
nicotinic receptor
Helping patient stop is part of job
� By preventing binding of nicotine, varenicline
– Reduces craving and withdrawal symptoms (agonist activity)
Stopping is primarily down to willpower
– Produces a reduction of the rewarding and reinforcing effects of
smoking (antagonist activity)
Smoking is addictive
� The most frequently reported adverse events (>10%)
Smoking is a medical condition
with varenicline were nausea, headache, insomnia, and abnormal dreams.
Smoking is a lifestyle choice
Pfizer-sponsored survey: Interviews with 2836 smoking and non-smoking general practitioners in 16 countries
1. Champix Summary of Product Characteristics. Pfizer Ltd, Sandwich, UK. 2006.
1: Apparent paradoxes
1: What does this mean?
Smoking is an addiction
stopping is a matter of
Need a message that recognises the
duality of beliefs about smoking
Smoking should be
is primarily a lifestyle
"Smokers must take responsibility for
regarded as a medical
stopping smoking, and they will need
determination to succeed; but when
determination is not enough, the
Helping patients to stop
other things have a
physician has effective tools to help the
is part of the job
2: A simple model of nicotine
2: The process of stopping
Chronic intake of
Motivational tension
When smokers think about their smoking
most, they are unhappy about it, but many
1. Think it meets certain needs
2. Is a source of enjoyment
3. Think stopping will be difficult
controlling motivation
Something needs to prompt them to make a quit attempt using a method that maximises
their chances of success
A biologically driven
Cues associated with
Experience of relief
of nicotine withdrawal
The treatment needs to be of a type and
when nicotine levels
symptoms leads to
intensity that meets the individual smoker's
in the brain are low
expectations of more
needs, and available whenever and for as
long as the smoker needs it
3: The physician's role
3: A simple consultation model
Yes, I know I should
Every month you put off
• To give professional, expert
stopping, you may lose another
advice on health matters
week off your life
• To provide treatment to those
You have to question whether it is
worth the pain and suffering
who want and need it
you will endure later
Now is not a good time
Now is always a good time for
stopping, smoking doesn't really
• Now is a good time to stop
• It is always worth having
I am worried that
Most smokers make many
attempts before they succeed
to a clear, firm
• There are things available that
Addictions can be conquered,
will make it easier
especially when you get help
It's never too late…
Source: http://csot.semmelweis.hu/download/gradualis/angol/vajer.peter-smoking.cessation.pdf
HEALTH CARE BENEFITS IN CANADA March 2006 We Take a Closer Look Wendy Murkar Vice-President, Claims Administration Green Shield Canada State of health care in Canada Issues affecting benefit utilization Impact on benefit plan design STATE OF HEALTH CARE IN CANADA Benchmarking of
20th International Congress for Analytical Psychology; Kyoto, August 28 to September 2, 2016 Pre-Congress Workshop on Authentic Movement: Danced and Moving Active Imagination ANIMA MUNDI IN TRANSITION: Cultural, Clinical, And Professional Challenges (English) Psyche is as much a living body as body is living psyche.