Levitra enthält Vardenafil, das eine kürzere Wirkdauer als Tadalafil hat, dafür aber schnell einsetzt. Männer, die diskret bestellen möchten, suchen häufig nach levitra kaufen ohne rezept. Dabei spielt die rechtliche Lage in der Schweiz eine wichtige Rolle.
Carmen1.doc
PASSIVE INFRARED HEMOENCEPHALOGRAPHY, 4 YEARS AND 100
MIGRAINES LATER (Accepted for publication in the Journal of
Neurotherapy.)
By: Jeffrey A. Carmen Ph.D.
4016 Henneberry Road, Manlius, New York 13104-9567
Phone: (315) 682-5272
carmen
[email protected]
ABSTRACT
Background
100 migraine sufferers were treated using Passive Infrared
Hemoencephalography (pIR HEG) over a period of four years. All subjects met
the criteria for at least one of the categories set forth in the International
Headache Society (IMS) classification criteria for headache disorders (IMS,
1988) for primary migraine.
Methods
Subjects were treated using the pIR HEG system in 30 minute sessions. A
central forehead placement (approximately Fpz) was used for the sensor
assembly for all subjects. Changes in headache patterns were examined. In
addition, after two years, an infrared video imaging system was added to the
data collection process. This was available for 61 of the 100 subjects. Infrared
forehead images were captured at the start and end of each session to
examine changes in prefrontal cortical brain activity.
Results
Most of the subjects improved control over their migraine headaches. Over
90% of those subjects who completed at least 6 sessions, reported significant
improvements in migraine activity.
Conclusions
pIR HEG appears to have a strong impact on migraine headaches, even for
people who have not had a positive response to medication. Headache
response by the end of 6 sessions appears to be a good predictor of
probability of improvement.
KEYWORDS: pIR HEG, HEG, Hemoencephalography, migraine, headache,
biofeedback, neurofeedback, frontal, inhibition.
BACKGROUND
Introduction to pIR HEG.
The term Hemoencephalography was first used by Hershel Toomim in 1997
(Toomim, 2002) to describe his process of Near Infrared Spectrophotometry
(NIRS HEG) system. The Passive Infrared Hemoencephalography (pIR HEG)
system evolved from Carmen's application of infrared technology to peripheral
thermal biofeedback (Carmen, 2002). The evolution was in part, based on the
psychophysiological concepts developed by Toomim (Toomim & Carmen,
1999) with his NIRS HEG system.
Both systems (pIR HEG and NIRS HEG) respond to blood flow dynamics as a
source of data. They also share a total freedom from eye roll and surface EMG
artifacts. This makes both systems well suited for exercising brain activity in
the prefrontal cortex, without any concern for the effects of these artifacts on
the integrity of the acquired signal.
The pIR HEG system was specifically developed as a potential intervention
technique for migraine headaches. As such, most of the developing data
regarding efficacy relates to migraine headaches. The conceptualization for
training cerebrovascular control to produce migraine control was based on the
tentative assumption that if a person could learn to control cerebrovascular
activity, especially control over excessive vasodilation, control over migraine
activity would follow.
Unfortunately, training a person to directly constrict excessively dilated
cerebrovascular structures did not work, regardless of whether a person had a
migraine headache at the time or not. Most people could easily learn to
increase the pIR HEG signal, but few could reduce it at all.
The hypothesis that reducing excessive vasodilation in the cerebrovascular
system would reduce migraine pain was based on the vascular theory of
migraine pathophysiology that was popular at that time (Diamond, 1994).
Migraine researchers have since rejected that theory in favor of a more
comprehensive theory of migraine pathophysiology involving the trigeminal
nerve and its interactions with the brainstem and cerebrovascular system
(Goadsby, 2001). This may be an interesting example of an intervention
process that failed to work as anticipated because it was conceptually based
on a theory that was later invalidated.
Based on Toomim's pioneering application of NIRS HEG to the prefrontal
cortex (Toomim & Carmen, 1999) to increase brain activity, the pIR HEG
process was modified to train increases instead of decreases. This turned out
to be a very good idea. When the pIR HEG sensor assembly was placed at
Fpz, and the training process was directed towards increasing prefrontal
cortical brain activity, the effects were direct and positive on both migraine
prophylaxis and actual abortion of migraine headaches. This effect on migraine
activity may have more to do with training control over the inhibitory effects of
the prefrontal cortex than training direct vascular control. The effects are also
more consistent with current thinking regarding the pathophysiology of
migraine (Goadsby, 2001).
The nature of migraine
The true nature of migraine headaches remains elusive. Migraines represent a
complex paroxysmal neurovascular phenomenon. They occur in two major
stages, although some researchers have postulated three and four stages.
The first stage represents a steady state of readiness to have the headache
and is sometimes associated with unusual neurological and
neuropsychological phenomenon, but no headache. Some of the best
descriptions of this stage of migraine activity can be found throughout Oliver
Sacks' book "Migraine" (Sacks, 1992).
The second stage is the headache. This often occurs on sudden relief from a
prolonged period of psychological or physiological stress (Diamond, 1994).
The fact that the second stage of a migraine correlates with excessive dilation
of cerebrovascular structures was one of the pieces of data that caused
migraine researchers to erroneously hypothesize a cerebrovascular
pathophysiological mechanism. The excessive vasodilation appears to be a
migraine effect rather than cause. It probably participates in pain generation
rather than originates the pain (Goadsby, 2001).
Within the field of headache research, the standard for headache classification
is still the International Headache Society (IHS) manual (Headache
Classification Committee of the International Headache Society, 1988). The
classification categories set forth in this manual represented an attempt to
stabilize headache categories for the purpose of communicating research
findings.
These classification categories were set forth at a time when the
understanding of the pathophysiology of migraine was less clear than it is
currently. Now that migraines have been subjected to sophisticated imaging
techniques such as fMRI and PET, the precise pathophysiology is still unclear,
although it is more clear now than when the IMS classification system was
developed.
The theory of migraine pathophysiology that currently has the most support
among migraine researchers is that migraine is involved with and possibly
caused by paroxysmal activity of the trigeminovascular system (Goadsby,
2001). This system includes all branches of the trigeminal nerve, the entire
cerebrovascular system, as well as the brainstem.
It is even unclear as to whether or not primary migraine (that which is not
caused by head trauma or disease) represents pathology at all. Most
physiologically based behaviors and internal mechanisms that permeate the
entire human race probably have their origins in evolutionary variables (Pinker,
1997). Loader (2002) suggested that the migraine-prone nervous system might
have had a variety of reproductive survival advantages such as causing a
reactive compensation to environmental conditions that produced global brain
hypo-perfusion, or alternatively producing a learned avoidance of external
environmental conditions such as ingestion of toxic plants that would trigger
migraine headaches. In a similar manner Carmen (2002) hypothesized that the
tendency of migraine sufferers to trigger a headache as a direct correlate of
the sudden drop in barometric pressure of an approaching storm may once
have correlated with a reproductive survival advantage by serving as an early
warning system to seek shelter.
Hypothesized mechanisms for the effects of pIR HEG on migraine
The positive effects on migraine management after exposure to the pIR HEG
system when the sensor assembly is placed in the center of the forehead,
behave in a manner consistent with a global increase in the amount of control
generated by the inhibitory and regulatory functions of the prefrontal cortex
(Goldberg, 2001). Using an electronic circuit analogy, this would be equivalent
to increasing the gain of the negative feedback loop in which a portion of an
output signal is fed back to the input to reduce the output. Negative feedback
circuits are inherently stable. (Madhu, 1985)
This inhibitory hypothesis is based in part on the following observations:
1. Patients being treated for migraine headaches using pIR HEG
consistently report spontaneous changes in attending behavior in the direction of easier and smoother sustained attention to tasks. Correlated with this is a reduced distractibility to both internal and external stimuli.
2. Patients being treated for migraine headaches using pIR HEG
consistently report spontaneous changes in emotional reactivity in the direction of emotional responses that are less rapid and less strong in response to stimuli that don't call for a rapid and strong emotional response.
3. pIR HEG requires a significant amount cognitive "effort"; a concept first
clearly defined by Pribram & McGuinness (1975). Sometimes during the first session or two this sustained effort appears to produce the functional equivalent of prefrontal cortical fatigue. When this happens, the behavioral effects appear to be those of disinhibition (difficulty attending to task, rage reactions, severe migraine activity) for the rest of the day. Typically on the following day after a good night's sleep, inhibitory functions are normal or better than normal for that person, suggesting some sort of an exercise/ rest/recovery mechanism.
METHODS
General
This is a collection of cases not a controlled study. The results must be viewed
within that context. The setting was a clinical setting rather than a research
setting. Also, pIR HEG was not the only intervention variable. At each session,
attempts were made to maximize migraine management effects beyond just
using the pIR HEG system. These additional variables included but were not
limited to the following:
1. Discussion of eating patterns and food triggers. 2. Discussion of stress response patterns. 3. Discussion of less obvious potential triggers such as the driving effects
of visual flicker sources.
4. Behavioral methods of migraine management. 5. Behavioral and insight oriented psychotherapy as needed.
These additional interventions represent a potential source of contamination in
terms of isolating effects to the application of pIR tiEG. However, there is one
built-in control over the effects of these additional interventions. They are the
same additional interventions that were used with the biofeedback based
migraine intervention techniques previously used by Carmen that were
considerably less effective than pIR HEG (Carmen, 2002).
Subjects
This population represents a heterogeneous group of 100 patients who
participated in migraine treatment using the pIR HEG system. There was only
one selection criteria applied. All patients met the criteria for at least one of the
migraine categories set forth in the IHS classification criteria for headache
disorders for primary migraine headaches (IHS, 1988).
Patients whose migraines were secondary to head injury or an active disease
process were excluded.
Typically patients were referred by a neurologist or primary care physician, due
to one of three reasons:
1. Poor response to medication. 2. Concerns about the potential negative effects of medication, including
the risk of fetal effects during pregnancy as well as potential health risks directly to the migraine patient.
3. Concerns about addiction to migraine medications.
In most cases migraine medications represent an acceptable risk/benefit ratio.
However, there is one uniquely serious risk category. The "triptans" that
represent the current standard of care for aborting migraines have been
documented to constrict coronary arteries and occasionally produce death
through this mechanism (Tepper, 2001). Anyone who has coronary risk factors
or active coronary disease is generally prohibited from using these drugs. For
these people, behavioral treatments may represent a medical necessity rather
than optional choice.
Procedure variables
Real world environments are not as well controlled as research environments.
For these 100 patients, length of active work with the pIR HEG system was
generally limited to 30 minutes within each office visit, but was sometimes less
than 30 minutes if fatigue, increase in headache, or fading attention made
continuing difficult. Sessions were usually scheduled once per week, although
sometimes sessions were less frequent due to scheduling conflicts.
Sessions were eventually spread out to weeks and months between sessions,
based on how long the patient was maintaining migraine management.
Morning was given preference for time of day, but the actual time of the
sessions was also determined by personal variables such as school and work
schedules. The total number of sessions was determined by patient
preference. Often the response of the headache to the pIR HEG sessions was
rapid but not complete, and patients would elect to continue sessions,
progressively increasing the number of days between sessions, to fine tune
the migraine management. Other times, significant improvement was
considered sufficient, leaving the remaining headaches to be managed with
medication or simply tolerated. Sometimes more sessions were scheduled to
work on other aspects of self management, even though the migraines were
under stable regulation.
Basic descriptive data Table #1 provides a breakdown of the sex and age of 100 subjects. This
reflects the relatively higher ratio of females to males in the general population
who suffer from migraines (Marcus, 1999). The female to male ratio in this
study is approximately 2:1, which is similar to the ratio of 3:1 reported by
Lipton et. al. (2001). The ages of the 100 subjects are somewhat younger than
the general population suffering from migraines (Lipton et. al. 2001). The slight
differences in age and sex between these 100 subjects and the genera!
population probably reflect the age and reason people in this geographical
region seek treatment (or are referred for treatment).
NUMBER OF SUBJECTS
Instrumentation
The pIR HEG system began to be used clinically in September, 1998 (Carmen,
2002). The system captures infrared radiation, within the 7 to 14 micron band,
with a center weighted circular field of view of 32mm. The thermal resolution is
.01 represented in the equivalent of degrees Fahrenheit. Based on the physics
of thermal transmission (Fraden, 1996), the best estimate of the area of the
brain to which the system is most sensitive would approximate the size and
shape of a golf ball, directly under the center of the field of view of the sensor
assembly. The sensor assembly for the pIR HEG system is mounted on the
forehead, recording infrared light waves emitted from the forehead in much the same way that a camera records visible light waves reflected from objects. The thermal activity picked up by the pIR HEG system reflects excess thermal energy generated by the brain as a function of brain activity. Increases in the pIR HEG signal reflect a composite of thermal energy generated by brain cells, vascular supply and vascular return, although there is disagreement among researchers as to which source represents the largest thermal contribution to the increase. Some researchers have hypothesized that the major contribution of the thermal increase comes from brain cells (Kiyaikin, 2002). Others have hypothesized that it comes mostly from the vascular system, (Swerdlow and Dieter, 1991). Shevelev (1992) is more supportive of the composite hypothesis. Regardless of the source, it seems reasonable to view the pIR HEG signal as a thermal waste product of increased brain activity (Carmen, 2002). Whereas the relative magnitude of source contributions to the pIR HEG signal remains an unresolved issue, the only thing that is of immediate importance to treatment issues is that increases in the pIR HEG signal are localized and follow increases in localized brain activity. A second type of equipment was also used, but for data collection only rather than as a feedback source. This equipment was not used with all patients because it was only available for the last two of the fours years. This additional equipment is not part of the pIR HEG system, but is used as a means of monitoring the effects of training. It is an infrared video capture system that captures changes in infrared patterns as thermal energy is emitted from the forehead as a function of focal changes in brain activity. Infrared image capture systems. The initial system was a STARSIGHT model 80 camera manufactured by Insight Vision Systems (Malvern, England). This camera failed after one year of use, and since it is no longer being manufactured, repair parts were not available. It used older technology and had relatively poor image quality. The thermal resolving power was too unstable to accurately specify. The STARSIGHT was replaced with a Raytheon 2000b digital core (Raytheon Corporation, Dallas, Texas), modified for the capture of infrared images of the head. The thermal resolution of this system is .04 degrees Fahrenheit equivalent. Both systems are similar in some respects. They both match the 7 to 14 micron spectral range of the pIR HEG system. What they "see" corresponds to the data captured by the pIR HEG system. They both use a 50mm, f1.0 lens, and have a pixel resolution of 240x320. However the electronic processing of the signal is so different between the STARSIGHT and the Raytheon camera systems that the images captured are not directly comparable. For both systems, image capture from the camera to the Windows 2000 based
computer was carried out using an Integral Technologies FP3D industrial
frame grabber using the Integral Technologies software designed for that
particular hardware (Integral Technologies, Indianapolis, Indiana).
Part of the pIR HEG process involves watching a video, the operation of which
is regulated by a threshold setting on the pIR HEG system. The VCR used was
a Hitachi FX6404, displayed on a standard 20 inch JVC television, viewed at a
distance of 8 feet. Additional Specifications.
The sensor assembly for the pIR HEG system has a response speed of 80
milliseconds.
Response speed is defined by the industry standard definition of the time
required to reach 67% of the full value of the object being measured (Fraden,
1996). The sensor assembly picks up the infrared radiation from the surface of
the forehead as blackbody radiation and then converts the infrared signal into
a dc signal that is fed to the input of the pIR HEG computer. The signal is then
processed and converted to a green digital LED display. Each LED is .56 inch
in height. The data sampling rate is 60 times per second. The display update
rate is 3.5 times per second. The display presents the data as a temperature
equivalent in degrees Fahrenheit with a resolution of .01 degree. There are no
electrodes used, so there is no direct electrical contact with the patient. The
system also interfaces with a universal remote control that provides threshold
based control over external audiovisual sources such as a VCR or DVD. A
threshold is set on the internal computer, above which a movie will turn on,
and below which the same movie will turn off.
61 of the 100 subjects were also monitored with one of two of the infrared
image capture systems previously described.
Procedure
For those subjects who began treatment after the installation of the infrared
video system, an image capture was carried out before and after each session.
A baseline image was captured and stored in digital tiff format. At the end of
the session a second image was captured. Images were captured using the 50
mm lens set at f1.0, at a distance of 3 feet from the subject. With the Raytheon
system, the maximum thermal capture range was set in software at a 10
degree Fahrenheit equivalent.
In the next step, the sensor assembly was placed on the forehead so that the
center of the field of view was in the center of the forehead, roughly at Fpz.
(See figure 1). It was held in place with soft hook and loop straps just tightly
enough to prevent slippage. Since the sensor assembly acquires light wave
infrared data, direct physical contact with the forehead is only necessary to the
extent that it prevents movement of the sensor assembly.
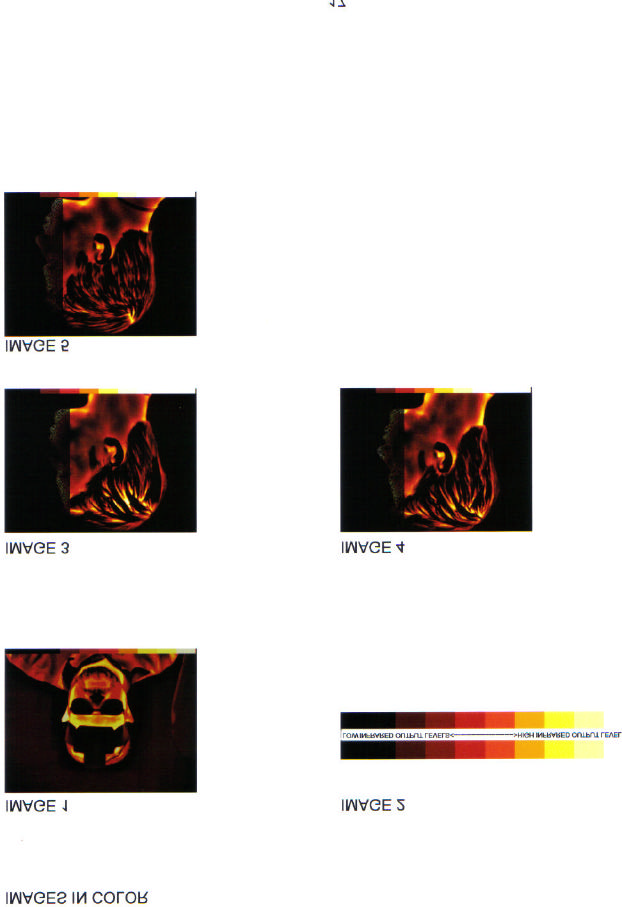
Image #1 is an infrared image of the author wearing the sensor assembly on
his forehead, captured with the Raytheon camera. Please note two significant
things. First, infrared by definition has no color. All of the infrared images in
this article have been digitally converted from grayscale images (the native
format for infrared cameras) to something called "false color" (Kaplan, 1999).
In this case the colors assigned to intensity changes range from black (lowest
intensity) to red to yellow to white (highest intensity). This color code was
selected for its intuitive value, since it is the pattern seen on stove burners and
other heated objects and is easy for people to comprehend the meaning of
these colors. Second, all images (except the one of the author) have been
captured with eye glasses removed. Both glass and plastic eyeglasses are
opaque to this part of the infrared spectrum, resulting in a total loss of infrared
data from that portion of the face covered by the glasses. Glasses were left in
place in this picture to demonstrate that mechanism.
IMAGE 1 (see color plates at the end of the article)
Typically for migraine, the center of the forehead is the only location used. With humans this is a unique location. The human forehead is devoid of hair, making it an ideal location for the radiation of excess thermal energy from the brain. It also makes it an ideal location for recording thermal activity from the prefrontal cortex. After the baseline infrared image was captured, the sensor assembly was placed on the forehead and the pIR HEG display turned on. At the same time, a movie (selected by the subject) was started. After several minutes a threshold was set above the current display reading, causing the VCR to place the movie on "pause". This required the subject to increase the pIR HEG signal to a point in excess of the threshold setting in order to turn the movie back on. The mental state that produces the maximum output of infrared radiation from the forehead is a simultaneous combination of the following:
1. Very low levels of discomfort such as anxiety, anger, or frustration. 2. Very intense levels of sustained concentration.
This is an affective/cognitive combination that usually does not feel familiar or
intuitive. However most were able to learn the concept within a minute or two.
Headache measures
Most, if not all headache research also includes some sort of pain index. A
review of the last 5 years of the IHS journal, Cephalalgia revealed various pain
scales from 0 to 3, all the way up to 0 to 100. Some researchers also used
faces that smile or frown as a correlated measure of pain. The commonality of
these measures among all the studies is that the lowest number or face
represents no pain and the highest number or face represents the worst pain
the person can imagine. There is however a problem with all of these
measures. When headaches start to improve, people forget how bad the
headaches used to be. Without realizing it, they start to assign higher numbers
to headaches of pain levels to which they used to assign lower numbers.
All of the subjects included in this study rated their headaches on a 0 to 10
scale. However, the only consistently reliable number was "0". Regardless of
the rating system used, total lack of pain is a stable, universal concept.
An additional, and probably more stable migraine change measure is the point
at which the person reports having a headache, but is no longer able to tell
whether it was a migraine or not. That was the primary head pain change
measure used in this study to measure "significant improvement".
It is a concept that at face value appears vague, but has turned out to be one
of the more robust measures, at least for the people in this study. For people
who are still getting some headaches, this is a more useful measure than "no
pain" because it reflects the point at which the headaches are discernable but
not troublesome. Although it does not have a numeric intensity equivalent, it
appears to be a more reliable and valid measure. It also allows a frequency
measure to continue as an added headache variable.
For the purpose of this study, "significant improvement" has been functionally
defined as that point at which the subject was still getting some headaches but
was unable to clearly identify them as migraine because the pain level was so
much less.
Infrared imaging provided a different type of measure. Although it reliably
displayed patterns of thermal energy emitted through the forehead, for many of
the subjects the migraine itself was visible.
During a migraine headache, the painful areas of the head were often visible
as high output areas on the infrared image. Although the meaning of this is not
entirely clear in terms of the underlying pathophysiological mechanisms, the
correlation with pain and location is very high.
Typically subjects who viewed the image would spontaneously say something
like "that's exactly where it hurts". The intensity of this image reliably
decreased by the end of the session, even though the output of the forehead
region increased. In addition, the amount of the reduction of the intensity of the
headache area correlated with the pain reduction by the end of the session.
SAMPLE CASES
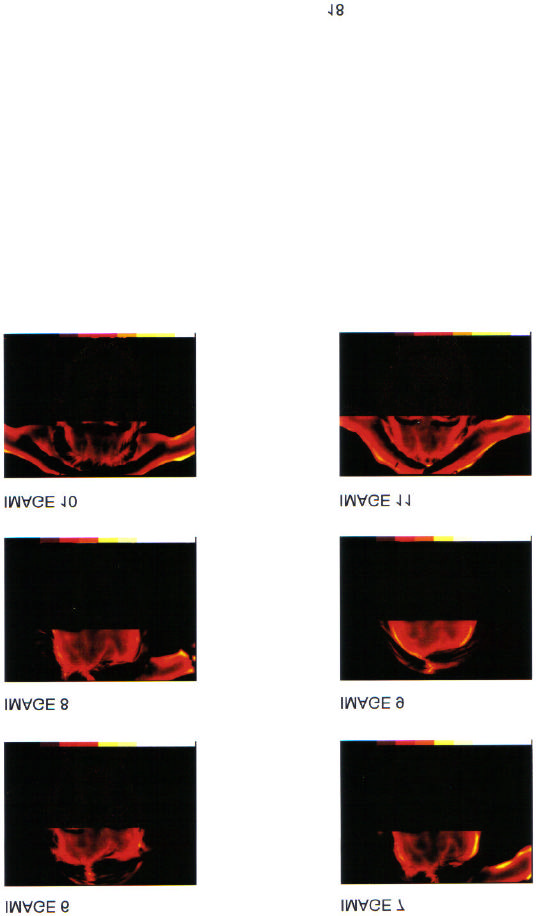
Color code
The following cases were drawn from those for whom infrared images were
available. The images follow a color code of thermal output ranging from black
(least thermal output) to red to yellow to white (most thermal output). Migraine
activity is generally correlated with yellow, and sometimes white. The
reference color bar is inserted below as image #2. Each bar in this image
reflects a 1.0 degree Fahrenheit equivalent. Actual captured images display a
minimum resolvable temperature difference (MRTD) (Kaplan, 1999) that is
much more sensitive, by blending colors and intensities.
IMAGE 2 (see color plates at the end of the article)
Patient #90
This was a 15 year old male, referred for 4 years of headache activity that had
evolved into chronic migraine activity of variable pain level for the previous 6
months. There was no identified disease process associated with the
headache activity. He had a strong family history for migraines. That combined
with the family history suggested a familial/genetic etiology. He had been on a
variety of prophylactic medications but they were having minimal to no effect.
Abortive prescription and over the counter (OTC) medications had been taken
as often as daily. There were no identifiable environmental triggers. He was an
excellent student but not attending school when first entered treatment due to
the headache activity. He would wake with a mild to moderate headache daily,
7 days per week, including vacations.
Migraines that are active 7 days a week and on vacations tend to be especially
stubborn. His headaches would usually become gradually worse by afternoon
and get somewhat better after abortive medication. The location of the
headaches was unstable, sometimes focal and sometimes generalized
throughout the whole head. Appointments were scheduled for mornings when
headache activity was at the lowest level, because high pain levels made
concentration difficult. Parts of his face are "grayed out" in these images to
help preserve anonymity.
Even after the first session, the low level headache that he came in with was
gone by the end of the session. Initially, the relief obtained was temporary and
did not last more than one day. As the sessions progressed, the headache
control lasted progressively longer.
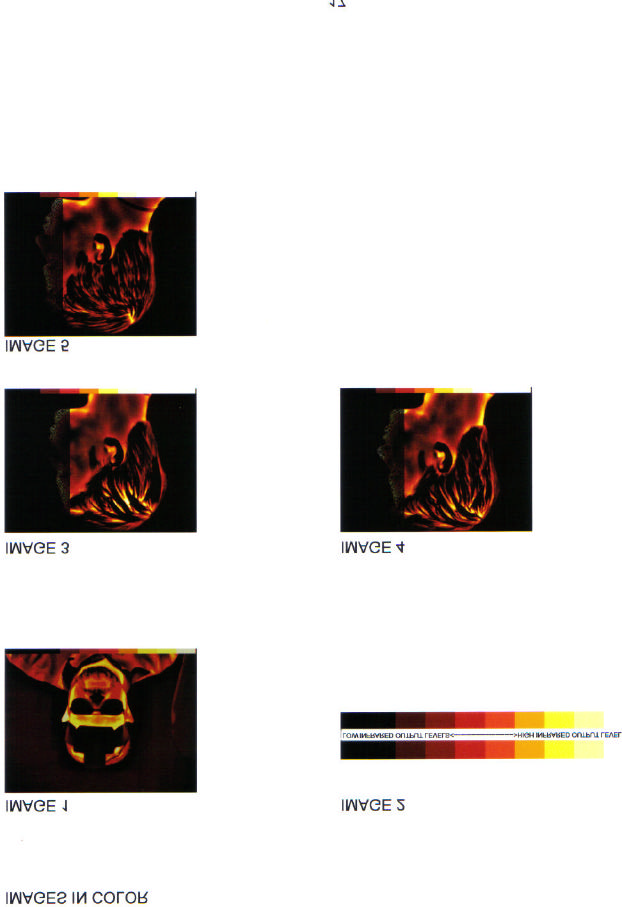
On session #5 he came in with a severe left sided posterior migraine that he
rated as a "10" on a 0 to 10 pain scale. The baseline infrared image (IMAGE
#3) is inserted here.
IMAGE 3 (see color plates at the end of the article)
After a 30 minute session of pIR HEG, the pain level dropped to "3 or 4" pain
level. That image (IMAGE #4) is inserted here.
IMAGE 4 (see color plates at the end of the article)
IMAGE 4 shows a post session lower intensity of thermal output in the left
posterior region of his head, corresponding to a reduced level of pain. Both pre
and post images delineated almost exactly the area of his head pain.
On session #10 he came in with the same headache in the same location but
the pain level was so low that the actual level was very difficult to determine.
This is an example of the type of change that is considered "significant
improvement". He could feel it, but not strongly. He rated it as a "1". That
image is inserted here as IMAGE #5. Note, hair interferes with infrared
transmission in these frequencies. The yellow mark in the back of his head is
where the hair is parted and does not represent pathological signal intensity.
IMAGE 5 (see color plates at the end of the article)
By session #12 the headache activity was no longer chronic, all medications
were discontinued, and he was back in school. Sessions were stretched to one
every 3 weeks. By session #17 he was still getting occasional mild headaches,
lasting an average of 30 minutes. He was no longer using abortive or
prophylactic medication, and headaches were no longer interfering with his life.
Comments: This case used more sessions than most, but may have had
elements of rebounding from excessive medication use. It is not typical to be
able to image migraines as precisely as these, which is one reason for the
inclusion of this particular case.
Patient #3.
This was an 11 year old pre-pubescent female who had been getting focal and
generalized migraines for the previous two years. They varied from daily to
weekly, usually towards the end of the day. There was no identified disease
process associated with the headache activity. Everyone in the immediate
family had migraines, making a familial/genetic etiology a high probability. The
only medications used were OTC analgesics and then only for the very severe
headaches. She responded very rapidly. By the 6th session she was under
complete control with no headaches. At a two month follow-up there were no
further headaches.
Comments: Migraines often start up in girls as adolescent hormones start to
kick in, and it is not unusual for the migraines to begin prior to the onset of first
menstruation. One to two years prior is somewhat typical. Often as
adolescence progresses, the migraines get worse.
In this case it is too early to tell whether they are just completely gone, or if she
will be back in another year or two with another bout of severe headaches. In
any case, based on experience with others, if she does have a recurrence, it
will probably take less work than the first time to bring them back under
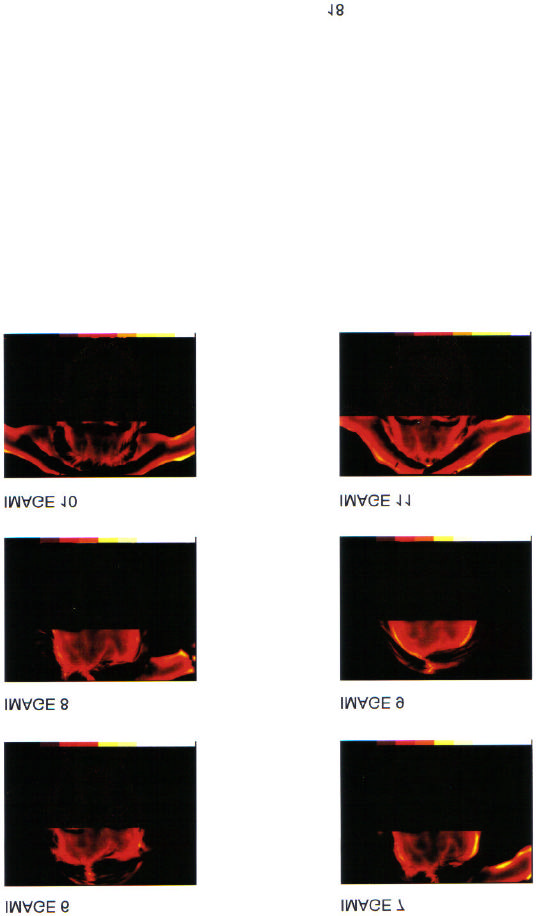
control. Image #6 is her first session baseline without headache present. The
relatively dark frontal image suggests relatively low overall prefrontal brain
activity. Experience suggests that this can be either part of the problem in
terms of allowing the brainstem migraine generator to be too active, or it could
be a product of being in pain much of the time.
IMAGE 6 (see color plates at the end of the article)
Image #7 is the baseline image from the second session. She came in with a
left frontal migraine, which imaged nicely in yellow around the area of the left
temporal artery, which is the area to which the migraine was localized. This
does not mean that the migraine was being generated by the left temporal
artery, although it might have been. That still represents a theoretical issue.
IMAGE 7 (see color plates at the end of the article)
Image #8 is the post session image from the same session. The migraine is
not completely gone, but down from severe to mild ("8" down to "3" by her
rating). Note that the right and left sides of the forehead are reasonably
balanced in terms of thermal output, and that the dark areas of the forehead
are less dark. In many patients, the dark areas appear to take on meaning in
terms of focal brain activity deficits and tend to correlate with emotions and
attentional patterns. However as a general guideline, when the dark areas
become lighter, people feel better physically and mentally.
IMAGE 8 (see color plates at the end of the article)
Image #9 is the baseline image from the final (6th) session. This is significantly
lighter in the forehead region, indicating greater prefrontal brain activity. There
was no headache present and no further headaches were reported on 1 and 2
month follow-up.
IMAGE 9 (see color plates at the end of the article)
It is not unusual for these forehead infrared images to become progressively
lighter over time. This generally correlates with symptom reduction and may
indicate a general increase in normal prefrontal cortical activity.
Patient #37.
This 24 year old woman started and finished treatment prior to the installation
of either of the infrared imaging systems, but is worth mentioning because of
the urgency of the situation. She had a long standing history of severe
migraines since early adolescence. The migraines were debilitating when they
occurred but tended to be infrequent. They sometimes hit once a week,
sometimes once a month, sometimes months between migraines. These were
managed reasonably well with various abortive medications. Most recently she
had been very successfully managing her migraines using oral Imitrex. Imitrex
is the first of the new breed of drugs called "triptans", and for many people has
allowed them to live much more normal lives.
The problem is that this young woman found herself pregnant, and although
sometimes migraines get better during pregnancy (Marcus, 1999), hers got
worse. The triptan drugs are powerful vasoconstrictors, and have been shown
in animal studies to have teratogenic effects (Tepper, 2001). She needed an
alternate way to manage her migraines during pregnancy, that did not carry
potential risks to the health of the unborn baby.
The migraines came under rapid control, reducing first in intensity and then
frequency. (As previously noted, reduction in frequency is a difficult thing to
measure because if the intensity is reduced sufficiently it is difficult to tell if a
migraine actually happened or not). In any case, after 3 sessions over a period
of 3 weeks, her migraines seemed to be greatly diminished or completely
gone, depending on the criteria used for defining the headaches. 5 more
sessions were completed just because it seemed like a good idea. There was
some continued headache activity through the balance of her pregnancy but it
was unclear whether or not they were migraines or just general pregnancy
related mild to moderate headaches. They did not require medication for pain
management.
Patient #49.
This 41 year old woman had been suffering from severe migraines for the
previous 6 years. They were severe enough to require occasional trips to the
local emergency room for injected narcotics. Prophylactic and abortive
medications had been only somewhat useful. Frequency varied from 1 per
month to almost daily.
This case is less clear than the others in terms of etiology. Her mother also
had occasional migraines, but not with such a severe frequency or intensity.
Correlated with the onset of her migraines was severe chronic psychological
stress from both work and home. She slept very poorly in that she would toss
and turn all night and wake exhausted. The sleep patterns would rise and fall
with the amount of psychological stress she was experiencing, although it was
not clear as to whether the sinusitis played a role as well. In addition, there
were a variety of comorbid physical disorders that fall into the category of
"migraine aggravators" rather than migraine causes. These included
temporomandibular joint problems, chronic bilateral maxillary sinus infections,
and some ill defined generalized health problems. The headaches correlated
positively with her menstrual cycle in that one severe migraine was predictable
premenstrually. Others could come at any time. Usually she woke with a mild
dull headache that was qualitatively different from the migraine. The migraine
was usually left sided and throbbing.
The morning headache was more generalized and dull. In terms of etiology,
this is a difficult diagnostic judgment call. While there was probably a genetic
component, there were enough physical problems to possibly account for the
headaches. Also, the relatively late onset of the migraines is a little suspicious
for secondary rather than primary migraine.
Surprisingly, her response to pIR HEG was very rapid, although the rapid
response did not hold for extended periods of time. The other physical and
psychological stressors remained relatively constant, but her migraines got
better between sessions. This suggested that these migraines were in fact
primary rather than being caused by some other physical disorder, although
the physical problems were clearly making management difficult.
She completed 11 pIR HEG sessions over a period of 6 months. The first 5
sessions were 1 per week. After that the sessions were spread farther apart.
Each session had what appeared to be both abortive and prophylactic effects.
If she came in with a migraine, she left either without it, or greatly diminished.
Any migraine activity between sessions was greatly diminished in terms of
intensity. After the first 5 visits, her life became too complex to continue except
on an intermittent basis. She would still get approximately 7 days of improved
migraine control from each session, but the headaches would still creep back
to previous levels by the end of the 2nd or 3rd week. She still comes in for an
occasional session, but on an irregular basis.
This case represents a very complex set of circumstances. It has been
included here as an example of the potential complexity of working with
migraine headaches, since they usually seem to be affected if not actually
driven by life stressors. The pIR HEG sessions clearly helped her a great deal.
However she also had been living under unbelievable levels of psychological
and physical stress, so it is not likely that the migraines were going to
disappear altogether. In cases like this, sometimes it seems worthwhile to
continue weekly sessions for a long period of time, or switch to home training.
However in her particular life situation, neither was a viable option.
It is likely that when her life circumstances straighten out and her physical
problems start to become less intense, her migraines will also become less
troublesome. When that happens, further pIR HEG sessions may bring her
migraines under exceptionally smooth control.
Image #10 is a baseline from a recent scheduled session. She came in with a
very bad migraine, localized to the right temporal region. In the image, that
region can be seen to be relatively brighter and covering a relatively larger
area than the left side. The "wings" on either side of her head are her hands
holding her hair out of the picture. This was also unusual for her in that most of
her migraines have been left sided.
IMAGE 10 (see color plates at the end of the article)
Image #11 was captured immediately after the session was completed. The
headache was completely gone.
IMAGE 11 (see color plates at the end of the article)
The thermal output from the forehead on this image shows less of a right/left
difference, and the forehead is generally lighter in color, indicating increased
overall prefrontal cortical activity. The same caveats apply in this situation as
the previous two sets of images. These images correlate with migraine pain or
lack of it. They may or may not represent the underlying physiological
mechanism generating the pain. Regardless, the reliability of these images is
very high. The utility of these images becomes greater when studied as
specific patterns that are unique to each individual. Under those conditions,
they become predictable and useful, especially as part of an ongoing
differential diagnostic process.
RESULTS
The typical response pattern for all those who improved was to have the intensity level of the migraines change before anything else changed. The headaches, when they occurred were less intense. The point of "significant improvement" was defined as the point at which it had become difficult to identify headaches as "migraine". From the standpoint of headache patterns, the focal location of the pain usually remained the same as the "migraines", but the pain level was much less, sometimes becoming almost indiscernible. Reduction in headache frequency typically came weeks or months after reduction in pain levels. This is an even more complex and unreliable measure than pain level because as pain levels drop it becomes more and more difficult to determine if a headache (migraine) actually happened. Detailed questioning has revealed that many people will continue to nave very low intensity "events" that are probably actual migraines but have an intensity so low that it requires very careful data collection for identification as a migraine. Often they are not even identified as headaches. Sometimes the only way to identify them is by patterns of events. For example, if the person's migraines typically triggered on a Friday after a long hard week, that person might continue to have very low intensity "events" at the time and day that they used to get a migraine headache. These are probably still migraine headaches, but they lack intensity. These "events" can be non pain events that present only as altered sensations. This observation may lend support to the hypothesis that the mechanism of action of the pIR HEG system on migraine headaches is through inhibition of the migraine generator. Functionally the migraines appear to become weaker. It may be that the frequency actually remains constant. Self reports are inadequate for this level of discrimination, and the infrared images are so sensitive to intensity that they don't help much either. The decision to terminate treatment was typically based on a variety of variables, most of them personal. Given the option of continuing sessions as long as needed, they were continued weekly until the headaches had stabilized to a comfortable point. Then the sessions were spread out progressively farther apart until a mutual agreement was reached to completely terminate. Personal preferences varied as to the degree of migraine management desired. Most were satisfied with relative freedom from debilitating headaches, relying to some extent on medication for the occasional very bad headache. For those 61 individuals for whom pre/post infrared images were recorded, the following observations also apply: The strongest correlate of the impact of the session was a decrease in dark areas in the image rather than the total increase in lightness of the image. This is somewhat consistent with the "cold patch" observed by Swerdlow & Dieter (1991). However because of the age and technology of their infrared camera, their images are not directly comparable with either of the image data sets in this study.
TABLE 2
PATTERNS OF HEADACHE IMPROVEMENT
NUMBER OF SUBJECTS
"SIGNIFICANT IMPROVEMENT" IN 6 SESSIONS OR
ADDITIONAL SUBJECTS WITH "SIGNIFICANT
IMPROVEMENT" IN 7 SESSIONS OR MORE
REGARDED THEMSELVES AS "COMPLETELY CURED" 2 (6%)
DID NOT IMPROVE AT ALL
DROPPED OUT BEFORE 6 SESSIONS
TOTAL IMPROVED (OF THOSE SUBJECTS WHO DID
NOT DROP OUT BEFORE 6 SESSIONS)
TABLE 3
VARIABLES ASSOCIATED WITH DROPPING OUT BEFORE 6 SESSIONS
DRUG ADDICTION (MIGRAINE MEDICATION)
PSYCHOLOGICAL REASONS
For both males and females, the majority started to see signs of improvement in 6 sessions or less. Of the 36 males in this study, 23 improved enough in 6 sessions to consider themselves significantly improved. Of the 64 females, 38 improved enough in 6 sessions to consider themselves significantly improved. Most continued on for more sessions, terminating when it felt comfortable or when the financial or time inconvenience of coming to an appointment was greater than the inconvenience caused by the relatively minor headaches. The number of sessions does appear to have some predictive importance in that most who eventually achieved "significant improvement" showed signs of improvement by session #6.
A relatively smaller number of males (5) and females (6) took more than 6
sessions before they saw signs of improvement. The cutoff point of 6 sessions
appears to have considerable predictive value in that if someone has not seen
signs of improvement by session number 6, it is only somewhat likely that
more sessions will help. For those who needed more sessions to see
improvement, typically they needed much more. Some went as high as 20 or
30 sessions.
Other observations.
4 people regarded themselves as completely cured. Followup suggests that
this may in fact be the case.
Not everyone improved. 8 of the males and 20 of the females did not improve
at all. However, all of the males who did not improve, and 16 of the females
who did not improve, had dropped out prior to 6 sessions. It is unknown if
these would have converted into "significantly improved" had they continued.
An analysis of the patterns of reasons for dropping out, showed great
variability and the reasons given may not have always been the real reasons.
1 male and 10 females dropped out for financial reasons. The reason for the
extreme female/male ratio on this variable is unclear. The psychological
reasons for dropping out were also quite variable and idiosyncratic. Some
people were addicted to the migraine medications and did not or could not stop
taking them. These drugs would often produce a once or twice daily rebound
headache. Breaking the cycle required a total withdrawal from abortive
medication, that these people were either unwilling or unable to accomplish.
The infrared images added a very useful measure for those for whom it was
available. If a person came into the session with a headache, painful areas
could usually be identified as high intensity areas on the images. Not everyone
came to a session with a headache, but it happened often enough to gather
some data. Typically the high intensity painful areas would reduce to a lower
intensity by the end of the session, correlated with a reduced pain level. This
was a very consistent finding.
Observations and impressions
These are general subjective impressions from working directly with all of
these patients using the pIR HEG process. Most people like the process, and
learn it quickly, in spite of the fact that the high intensity cognitive "effort"
combined with a very relaxed emotional state is an unfamiliar concept to
almost everyone.
The reasons for change in migraine status remain unclear. It is likely that the
mechanisms involve the inhibitory functions that are closely associated with
the prefrontal cortex, but at this point that is hypothesis rather than proven fact.
CONCLUSIONS
The results of this study support the observations of other clinicians using the
pIR HEG system with migraine patients. Migraine patients appear to improve
strongly, and quickly, usually seeing positive effects within the first 6 sessions.
In addition, the effects appear to be both prophylactic and abortive. Because
the system is so new, long term data is not yet available. It must still be
considered an experimental intervention.
More precise pre/post psychophysiological measures such as fMRI, QEEG
and related imaging processes may eventually help to clarify the specific brain
mechanisms activated by this process. As more data is gathered, it may even
contribute meaningful information to ongoing attempts to clarify the basic
pathophysiological mechanisms associated with migraine headaches.
REFERENCES
Bednarczyk, E., Remier, B., Weikert, C., Nelson, A., Reed, R. (1998). Global
blood flow, blood
volume, and oxygen metabolism in patients with migraine headache.
Neurology, 50 (6), 1736-
1740.
Breslau, N. (1998) Psychiatric comorbidity in migraine. Cephalalgia, 18 (22),
56-61.
Carmen, J. A. (2002). Passive Infrared Hemoencephalography, 4 Years and
100 migraines later. Presented at 2002 Society for Neuronal Regulation
conference, Scottsdale, AZ.
Diamond, S. (1994). Head Pain: diagnosis and management. Clinical
Symposia, 46 (3), 2-34.
Fraden, J (1996). Handbook of modern sensors, physics, designs, and
applications. New York:
Springer-Verlag New York, Inc.
Goadsby, P. (2001). Pathophysiology of headache, 57-72, in Silberstein, S.,
Lipton, R., and Dalessio, D. eds Wolff s Headache and other Head Pain, 7th
edition. New York: Oxford University Press, Inc.
Goldberg, E. (2001). The executive brain. New York: Oxford University Press,
Inc.
Kaplan, H. (1999). Practical applications of infrared thermal sensing and
imaging equipment.
Bellingham, Washington: International Society for Optical Engineering.
Kiyaikin, E. A. (2002) Brain temperature fluctuation: a reflection of functional
neural activation.
European Journal of Neuroscience, 16 (1), 164-168. Lipton, R. B., Stewart, W. F., Diamond, S., Diamond, M., Reed, M. L. (2001). Prevalence and burden of migraine in the United States: Results from American Migraine Study II. Headache. 41 (7), 646-657. Madhu, S. (1985). Electronic circuits and systems. Indianapolis: Howard W. Sams Co., Inc. Marcus, D. (1999), Special considerations in the management of headache in women. Headache Quarterly, 10(1), 37-43. Mitsikostas, D., Thomas, A., (1999) Comorbidity of headache and depressive disorders. Cephalalgia, 18(22), 22-25. Moskowitz, M. (1998), Migraine and stroke - a review of cerebral blood flow. Cephalalgia, 18 (22), 22-25. Pinker, S. (1997). How the mind works. New York: W. W. Norton & Company, Inc. Pribram, K & McGuinness, D. Arousal, activation, and effort in control of attention. Psychological Review, 1975, 82 (2), 116-149. Sacks, O., (1992). Migraine. England: University of California Press. Shevelev, I.A., (1992) Temperature topography of the brain cortex: Thermoencephaloscopy. Brain Topography, 6 (2), 77-85. Shevelev, I.A., (1998) Functional imaging of the brain by infrared radiation (thermoencephaloscopy) Progress in Neurobiology. 56 (3), 269-305. Swerdlow, B. & Dieter, J. (1991) The value of medical thermography for the diagnosis of chronic headache. Headache Quarterly, 2 (2), 96-104. Tepper, S.J. (2001), Safety and rational use of the triptans. Medical Clinics of North America. 85 (4), 959-970. Toomim, H., Carmen, J. (1999). Hemoencephalography (HEG). Biofeedback, 27 (4), 10-14, 27. Toomim, H. (12/2002) Personal communication.
Source: http://www.eeginfo.ch/fileadmin/images/was_ist_neurofeedback/literatur/pIR_carmen.pdf
a ient Guide Continent Di ersion Find A LocalSupport Groupwww.uoaa.org or A publication of Welcome to the United Ostomy Associations of America Dear New Ostomy Patient, support and educational meetings where you can get answers to those questions that so many new patients
J Vet Intern Med 2007;21:1340–1346 Adjuvant Immunother apy of Feline Fibrosarcoma with Recombinant Feline Interferon-v Verena Hampel, Bianca Schwarz, Christine Kempf, Roberto Ko¨stlin, Ulrike Schillinger, Helmut Ku¨chenhoff, Nora Fenske, Thomas Brill, and Johannes Hirschberger Background: Recombinant feline interferon-v (rFeIFN-v) was tested as a treatment option for cats with fibrosarcoma to