Levitra enthält Vardenafil, das eine kürzere Wirkdauer als Tadalafil hat, dafür aber schnell einsetzt. Männer, die diskret bestellen möchten, suchen häufig nach levitra kaufen ohne rezept. Dabei spielt die rechtliche Lage in der Schweiz eine wichtige Rolle.
Kendoff.de
One stage exchange arthroplasty:
the devil is in the detail
The general management of periprosthetic infections after total approach in the revision of an infected TJR. Emphasis is given
joint replacement (TJR) remains a challenging procedure to
to all detailed requirements that provide the basis for a high
any arthroplasty surgeon. The infection rate after primary TJR
surgical and post-operative success rate.
is reported to be between 0.5% and 2%, however in the field of
revision arthroplasty, this might increase to over 10%.1-4
Etiology and Classification
Consequently, periprosthetic infections remain a serious
Every periprosthetic infection is a foreign body associated
problem, despite modern techniques, implants and rigorous
infection and should be clearly differentiated from other bone
perioperative prophylaxis. The therapeutic goal in either one
or more staged revisions of periprosthetic infections is, in
Most micro-organisms from human bacterial flora gain
general, defined by a complete eradication of the infection and
access to the surface of the prosthesis during the operation
maintenance of the joint function.
and more than 90% of infections during the first year after
While it has been widely accepted that the treatment of a late
operation are due to contamination during the procedure.21
chronic infection should be undertaken with a two- or more-
Haematogenous infections are less frequent. In the presence of
staged revision technique, a distinct single-staged revision
foreign bodies, a contamination as low as 100 colony-forming
approach has shown similar good results within the last 30
units (CFU) is sufficient to induce an infection. In comparison,
years in our own clinical setup.5-8
when no foreign material is present, it takes 10 000 cfu.22 This
In general, both revision techniques should be available
effect is due to the diminished clearing capacity of phagocytosis
depending on the clinical situation, the local setup and the
by leucocytes in the presence of foreign material.23,24
surgeon expertise. In the most frequent scenario, implant
Furthermore, the bacteria are adhesive to the implant
removal is followed by a defined six week or longer course of
surface by forming a biofilm. This biofilm blocks natural defense
systemic antibiotic treatment and delayed implantation.
mechanisms. These sessile bacteria are also highly resistant to
In particular, the introduction of antibiotic impregnated spacers
antimicrobial agents and the minimal inhibitory concentration
in infected total knee and hip revisions, seemed to improve the
can be elevated up to the 1000-fold within the biofilm.25
functional outcome of the two-staged approach and has gained
The general period between colonisation and clinically
increasing popularity within the last five to ten years.9-11
detectable infection may last for months or years and as
However, looking carefully at the current literature and
a result, local signs of infection may occur very late. It is
guidelines for the treatment of infected TJRs, there is no clear
important to realise that periprosthetic infection does not only
evidence that a two- or more-staged procedure has a higher
indicate an infection of the prosthetic interface, but also of the
success rate than a one-staged approach.(Della Valle)12
surrounding bone and soft tissues.
Although a larger number of relevant articles4,10,13-15, describe
the two-staged technique as the benchmark procedure for
the eradication of infection, most of the recommendations
Infection can be classified in two ways; 1) acute infection -
(duration of antibiotic treatment, static
vs mobile spacer,
occurring within the first three post-operative weeks; 2) late
interval of spacer retention, cemented
vs uncemented new
infection - occurring after the third post-operative week.
implant fixation and especially overall success rates) are based
Consequently we aggressively treat an acute infected TJR
on expert opinions and evidence level IV to III studies, rather
with a local debridement, soft-tissue revision and lavage,
than on prospective, randomised or comparative data.4,10,11,13-18
polyethylene liner exchange, including preservation of the
We consequently believe that a distinct one-stage exchange
initially implanted prosthesis. Systemic antibiotics are adapted
still offers certain advantages with a comparatively high
to the algorithm described by Zimmerli, Trampuz and Ochsner.26
success rate. The major advantages are the need for only
Late infection, however, is treated with complete implant
one procedure (if no recurrence), reduced hospitalisation
removal. Independent from a one- or two-staged approach,
time, reduced overall cost and relatively improved patient
a further re-implantation of a new prosthesis should be
scheduled as soon as possible after infection eradication.
Although obvious advantages exist, there are obligatory
Earlier classification guidelines mostly defined stages of
pre- and peri-operative details which need to be meticulously
periprosthetic joint infection (PJI) into early, acute and late
respected to achieve a successful one-staged revision.
infection types. Due to the general advancements of diagnostic
Consequently this article describes the author's experience
algorithms and further developments of systemic and local
of their current institution's management strategies, which
treatment options, we also adapted our classifications system
have been in place for over 30 years, with the one-staged
to the staging system described by McPherson et al.27,28 This
2012 British Editorial Society of Bone and Joint Surgery
D. KENDOFF, T. GEHRKE
includes, besides type and timing of infection, mainly the
current systematic medical and immune status of the host
Serial conventional radiological comparison can be useful to
patient, as well as the current local extremity grade based on all detect obvious osseous infections signs. For the diagnosis
possible local compromising factors.
of PJI however, we do not tend to use nuclear imaging in
our setup. Although highly sensitive, bone scans, as labeled
leukocyte imaging, Gallium imaging or PET imaging have
The first symptoms of early infection usually present around
shown to be non-specific with consequently only moderate
four to eight days after a TJR. With the presence of purulent
reliable study data.12 Bone scans have been shown to visualise
secretion, infection is clear. However, any prolonged wound
suspicious enhancements for several years following TKR and
discharge (> 12 days), continued soft-tissue swelling and
THR. Enhancements occur especially after the early phase of
induration, or wound dehiscence should be taken seriously.
implantation, therefore can represent bone remodeling and
We suggest in these cases that a pro-active and aggressive
may be misleading.
approach is taken at all times by the surgeon. If an early
In addition to conventional radiological imaging of the
infection (within three weeks) occurs after the patient is
affected joint, we recommend clinical and radiological
discharged from the hospital, often superficial wound healing
evaluation of all other joint replacements of each PJI patient,
problems, hematomas and seromas are evident, which might
e.g. contralateral affected THR.
correlate with the presence of deep infection of the implant.
This however, is not always obvious and the clinical signs can
In general we see very few arguments against a one-staged
According to our experience, current evidence and recent
revision protocol, and are able to successfully treat over 85%
clinical practice guidelines by the American Academy of
of all infected cases using this technique. The mandatory
Orthopaedic Surgeons, we defined the following mandatory
infrastructural requirement is based on the evidence of the
pre-operative testing, for every case of a TJR patient with
bacteria in combination with a distinct patient specific plan for
unexplained pain.12
the topic and systemic antibiotic treatment by an experienced
• Laboratory monitoring of CRP and erythrocyte
sedimentation rate (ESR).29,30
• Knee and hip joint aspiration with prolonged microbiologic
culture time of at least 14 days, with patients being off
We defined the following criteria to alter our one-staged
antibiotics for a minimum of 14 days.31
approach to a two-staged procedure:
• Synovial fluid analysing of white blood cell count and
• Failure of ≥ two previous one-staged procedures
percentage of neutrophils.32-34
• Infection spreading to the nerve-vessel bundle
• Repeated aspiration in cases of own negative cultural
• Unclear pre-operative bacteria specification
results in combination with either obvious infection signs
• Non-availability of appropriate antibiotics
or pre-existing external positive cultural results.
• High antibiotic resistance
• Biopsy of the knee joint in cases of persistent negative
aspiration results, with obvious infections signs.35
Pre-operative preparation and planning
To undertake a one-stage procedure a positive bacterial culture
must be present and a respective antibiogramm must exist.
The mandatory and most relevant pre-operative diagnostic
The proposed cemented fixation using antibiotic loaded acrylic
test needed in any case of a planned one-staged exchange,
cement is considered to be the treatment of choice in order
is based on knee joint aspiration with an exact identification
to achieve a high topic therapeutic level of antibiotic elution
of the bacteria. The presence of a positive bacterial culture
from the cement.36,40 In the future, antibiotic local implant or
and respective antibiogramm is needed for the one-staged
silver coatings might be viable alternatives for the one-staged
procedure in order to define which antibiotic loaded acrylic
cement is required to achieve a high topic therapeutic level of
The success of a one-staged approach not only depends
antibiotic elution.13,14,36-40
on the meticulous removal of all hardware material (including
This protocol has become mandatory in our clinic for
cement and restrictors) in combination with the antibiotic
every planned TJR revision including all late or early aseptic
loaded acrylic cement, but also an aggressive and complete
loosening, furthermore in all other cases of unexplained pain or debridement of any infected soft-tissues and bone material
malfunction after primary or revision TJR.
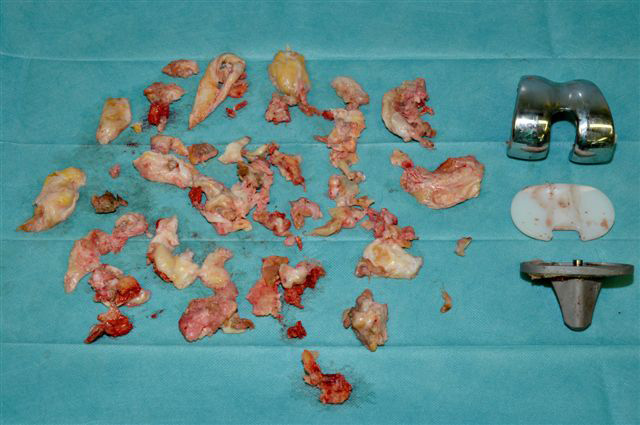
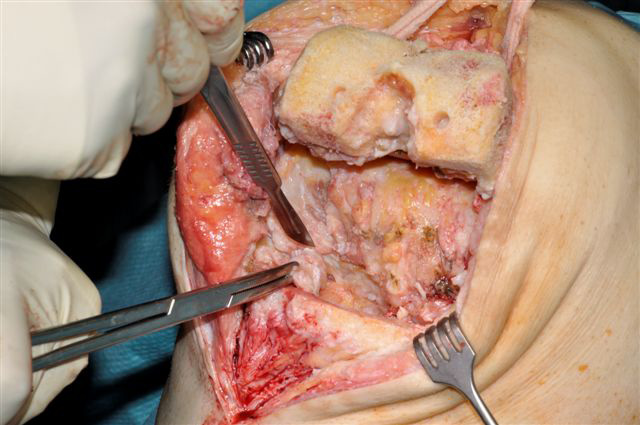
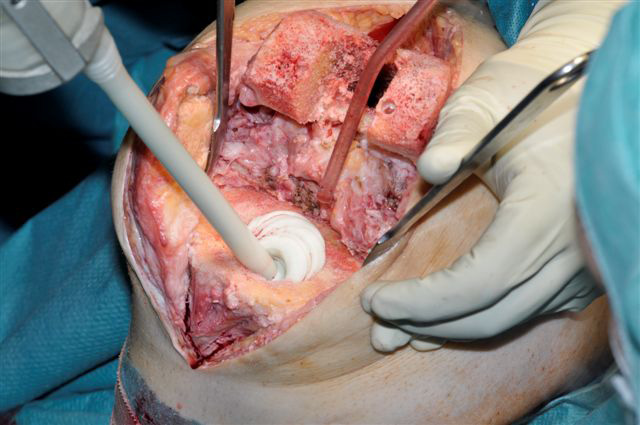
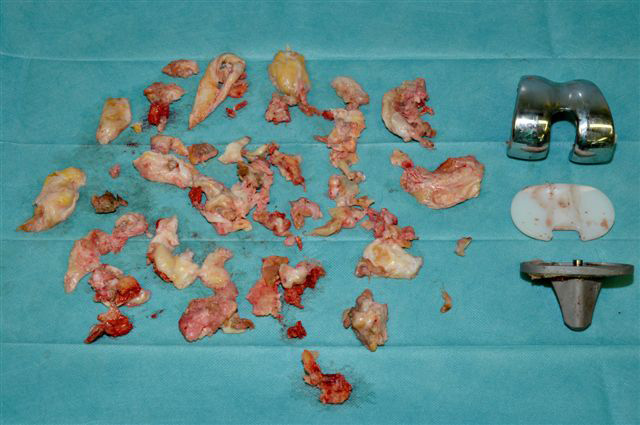
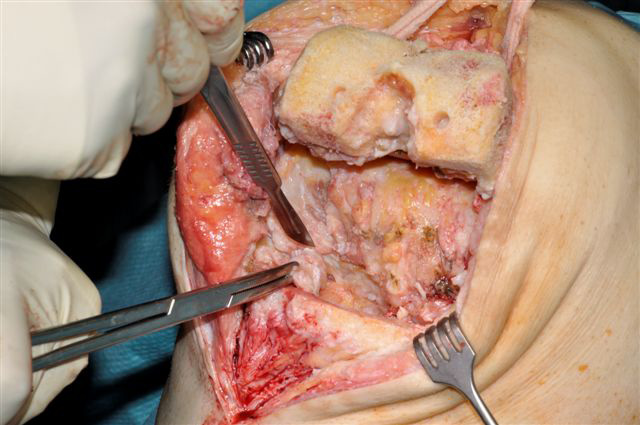
(Fig. 1). For example, this should include a full synovectomy in
In a previous aspiration study, we were able to show that
the posterior aspects of the knee or radical debridement of the
between 4% and 7% of our patients who were initially planned
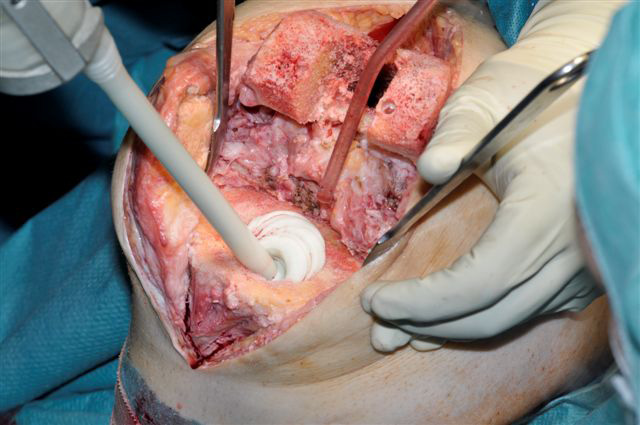
anterior and posterior capsule of the hip (Figs. 2 and 3).
to have an aseptic total hip or knee replacement revision had
In the knee this approach might also include sacrificing the
evidence of a subtle low grade infection, without any obvious
collateral ligaments to perform a complete and radical soft-
clinical symptoms or relevant laboratory elevations as described tissue resection. Thus the definitive pre-operative planning
should consider the use of a of a semiconstrained or even full
THE JOURNAL OF BONE AND JOINT SURGERY

ONE STAGE EXCHANGE ARTHROPLASTY
contrained implant, also based on the surgeons preference and
General Pre-Operative Planning
• There should be clinical and anaesthesiological
assessment of the general operative risk
• An adequate supply of available donor blood
• In the case of long exchange operations, pre-operative
administration of fibrinolysis inhibitors (e.g. tranexamic
acid) is recommended
Specific risks to patients
• The risk of recurrent or new infection between 10% and
Fig. 1. Meticulous debridement of all affected soft tissues in a one-staged
revision total knee replacement.
• A risk of reoperation for haematoma, wound debridement
or persistent infection
• Damage to the sciatic / peroneal nerve
• Post-operative stiffness and loss of function (extensor
• Intra- and post-operative fracture
• Increased risk of aseptic loosening
Surgical Preparation
Implants and Cement:
• The surgeon should have experience of the type of
implant to be revised and be familiar with its removal
and disassembly. Occasionally the use of implant-specific
instrumentation will be necessary
• Pre-existing ligament deficiencies in the knee require
constraint implants; however ligament deficiency may also
result during intra-operative debridement – hence the
Fig. 2. Aggressive debridement also includes the posterior knee aspects.
need for rotating or fixed hinged implants in general. Based
on our aggressive soft-tissue debridement, this is the case
in over 90% of our one-staged knee revision cases
• Inadequate bone stock, possible intra-operative
complications as acetabular / femoral or tibial shaft
fractures, perforations of the cortex, osseous windows
and tibial/femoral disintegration must be taken into
consideration when choosing an appropriate implant.
• Distal femoral or proximal tibial replacement implants
may have to be chosen in patients with significant bone
deficiency in the knee. Bone loss is usually significantly
more extensive than radiologically evident. Custom-made
implants with extra-long or narrow stems may have to
be ordered prior to surgery. The need for total femoral
replacement implants is rare.
• Significant damage to the extensor mechanism of the knee
can require an arthrodesis nail, which should be available
as a last option in necessary cases (with patient consent)
• Antibiotic loaded acrylic cement with additional antibiotics
in powder form to be added intra-operatively is obligatory
in all cases. Invariably at least two or three mixes of
cement (between 80 g and 120 g) are required. Large
mixing systems and appropriate cement guns are required.
In patients with a narrow diaphysis extra narrow nozzles
allow for appropriate retrograde cementing technique.
Fig. 3. Aggressive debridement of the hip includes the ventral capsule and
• Knowledge about possible type of antibiotic loaded acrylic
even very caudal aspects of the an affected hip joint.
cement used at primary implantation, as resistance to the
D. KENDOFF, T. GEHRKE
previously used antibiotics must be expected.
must be as radical as possible (Fig. 1). It must include all
• Often industrially pre-manufactured antibiotic loaded
areas of osteolysis and non-viable bone.
acrylic cement may be appropriate. However, for the
• Completing the debridement often exceeds the amount
success of any one-staged procedure, the antibiogramm
of resected material than seen in a two-staged approach
for the final topic cement impregnation is mandatory.
• We recommend the general use of pulsatile lavage
Operative Technique
throughout the procedure, however after all implant
Skin Incision and debridement:
removal and completed debridement, the intramedullary
• Old scars in the line of the skin incision should be excised.
canals are packed with polymeric biguanid-hydrochlorid
The prior incision from the last operative approach should
(polyhexanid) soaked swabs. Furthermore the swabs are
be used, if possible. In cases of multiple scars, the most
placed over the wound area before re-draping the patient.
lateral one should be considered.
• The whole team should re-scrub and new instruments be
• Fistulae should be integrated into the skin incision and
obtained for re-implantation.
radically excised to the joint capsule. If the need for
• A second dose of antibiotics should be given after 1.5
muscular-cutaneous flaps can be anticipated, a plastic
hours operating time or if blood loss at this point exceeds
surgeon should be available.
• An anticipated operative time exceeding two hours should
include an above knee tourniquet, but not inflated. The
knee procedure should be started without tourniquet;
• Inadequate bone stock may require the use of allografts,
consequently interfaces between infected tissue, scar
although ideally this should be avoided. We even prefer to
and surrounding healthy bleeding soft tissue can be
fill large defects with antibiotic loaded acrylic cement, and
distinguished more clearly during the debridement. All
do not favour the use of any allograft.
non-bleeding tissues and related bone need to be excised
• Alternatively the use of tantalum based acetabular
very aggressively. After debridement and implant removal,
wedges, femoral and tibial cones have been implemented
maintaining the tourniquet can be helpful for the removal
in our regular clinical use for over four years. Variations
of intramedullary and the re-cementation.
of depth and width of those augments allow for a proper
• Biopsy material, preferably five or six samples, should
reconstruction of the resulting bone loss, including an
be taken as a routine measure from all relevant areas
excellent biocompatibility and related stiffness and cellular
of the operation site for combined microbiological and
structure. Consequently a combined fixation of the cement
histological evaluation,21,35,41 after the defined antibiotics
with the prosthesis and tantalum augment becomes
have been administered. This commonly comprises a wide
possible. It has been postulated that tantalum has some
spectrum cephalosporin with further antibiotic related
antibacterial potential; however this has not been clinically
• The antibiotic loaded cement is prepared in the meantime,
Implant removal and completion of debridement
fulfilling the following criteria:
• Removing cemented implants can be easier and less
- Appropriate antibiotic (antibiogramm, adequate elusion
invasive than removing ingrown cementless components.
characteristics)
• In cases of well-fixed uncemented components, cortical
- Bactericidal (exception Clindamycin)
windows are required to gain access to the interface.
- Powder form (never liquid)
High speed burrs and curved saw blades can aid removal,
- Maximum concentration of 10%/PMMA powder
however, occasionally significant destruction and related
• Antibiotics (e.g. Vancomycin) might change the
loss of bone stock can occur.
polymerisation behaviour of the cement, causing
• Narrow, straight osteotomes with symmetrically coned
acceleration of cement curing.
blades should be used to remove all accessible bone
• Current principles of modern cementing techniques should
cement, being careful not to cause further loss of bone.
be applied (Fig. 4). In order to achieve an improved cement
• A multiple osteotome technique should be used in the
bone interface, the tourniquet should be inflated prior to
knee to drive cement from between the tibial base plate
cementing in TKR cases.
and medial and lateral component. This may be less
destructive than aggressive extraction with the mallet.
• Extraction of the implant necessitates special or universal
Associated post-operative systemic antibiotic administration
extraction instruments, if available. Otherwise general
is followed for 10 to 14 days (exception: streptococci). While
punches are required.
a prolonged administration of intravenous antibiotics for six
• Special curved chisels, long rongeurs, curetting
weeks is common in the two-staged approach, the rational
instruments, long drills and cement taps are used to
for this prolonged period of time has not been clarified in the
remove the cement. In the hip joint, retrograde chisels can
literature. There is, however, clear evidence of relevant systemic
be helpful in many cases.
and organ-specific complications after prolonged antibiotic
• General debridement of bone and posterior soft-tissues
THE JOURNAL OF BONE AND JOINT SURGERY
ONE STAGE EXCHANGE ARTHROPLASTY
staged exchange. The general risk of intra- and post-operative
fractures should be comparable to the two-staged exchange.
The two-staged approach has become the method of choice
for most surgeons worldwide, with reported re-infection in
between 9% and 20% of cases.15,18,42 Although advocated as the
benchmark procedure, we have established and followed the
one-staged approach in our clinic for over 35 years and in over
85% of all our infected TJR patients.
Accordingly, far more studies have been published
and emphasised about the two- or more-stage revision
technique.1-14,16,18,23,28,27,35 Few studies evaluating the one stage
exchange and its techniques are available.5,8,19,20,43-46
Although most reports are from our own institution, some
Fig. 4. Aggressive debridement of the hip includes the ventral capsule and
international experience using this technique exists with rates
even very caudal aspects of the an affected hip joint.
of success between 75% and 90% depending on the time of
Besides the obvious benefit by eliminating a second major
Post-operative care and rehabilitation
operation, further major advantage arise from the reduced
Post-operative stay in hospital ranges between 12 and 20 days
duration of post-operative systemic antibiotics. This rarely
(mean, 14) in our setup. The physiotherapeutic approach in any
prolongs more than 14 days in our setup. The rational for
one-staged approach cannot be generalised. Due to the variety
this has also been evaluated in a study by Hoad-Reddick et
of soft-tissue and bone damage, and the extent of infection,
al,16 where the authors concluded that a prolonged course of
an individual plan is developed in most cases. Compromises
antibiotics does not seem to alter the incidence of recurrent or
between necessary immobilisation due to structural damage
persistent infection, even after a two-staged revision.
and attempts for an early mobilisation, especially in an elderly
multimorbid patient, have to be made. However, we recommend Summary
an early and aggressive mobilisation within the first eight days
The one-staged infected TJR approach is used sparingly in
post-operatively. Weight-bearing should then be adapted to the
the orthopaedic community. From our perspective the one-
intra-operative findings and substance defects. In TKR patients, stage revision offers certain obvious advantages. The key to
a similar mobilisation strategy compared to the primary
success is based on the well-defined and detailed intra-hospital
situation allows the patients to fulfil an early rehabilitation
infrastructure, including a meticulous pre-operative aspiration
process, which should reduce associated muscular movement
regime, planning, aggressive intraoperative surgical approach
restrictions, stiffness or fibrosis of the affected knee.
and post-operative specific patient care
In patients with adequate bone stock and relatively low
soft-tissue involvement, an immediate full-weight-bearing
mobilisation often becomes possible.
D. Kendoff MD, PhD
Persistent or recurrent infection remains the most relevant
Orthopaedic Surgery
complication in the one-staged technique. As failure rates with
ENDO-Klinik Hamburg
a two-staged exchange have been described as being between
9% and 20% in non-resistant bacteria, our experience shows
comparative results after eight years of follow-up using the
one-staged approach (unpublished data).12,15,17,42 As a result, we E-mail: [email protected]
discuss with patients, at the time of consent, a possible risk of
recurrent or new infection in between about 10% and 20% of
Although we are unable to present comparative data
1. Bozic KJ, Kurtz SM, Lau E, et al. The epidemiology of revision total knee
evaluating the functional outcome under a one- versus two-
arthroplasty in the United States. Clin Orthop Relat Res 2010;468:45-51.
staged approach, we don't believe that an articulating spacer,
2. Bozic KJ, Ries MD. The impact of infection after total hip arthroplasty on hospital
or a partial or complete immobilisation of the affected joint, will
and surgeon resource utilization. J Bone Joint Surg [Am] 2005;87-A:1746-51.
result in a better functional outcome.
3. Kurtz SM, Lau E, Schmier J, et al. Infection burden for hip and knee arthroplasty in
the United States. J Arthroplasty. 2008;23:984-91.
We consider the risk of direct damage to the sciatic or
4. Kurtz SM, Ong KL, Lau E, Bozic KJ, Berry D, Parvizi J. Prosthetic joint infection
peroneal nerve and main blood vessels as low, under the
risk after TKA in the Medicare population. Clin Orthop Relat Res 2010;468:52-6.
guidance of an experienced surgeon, even in such an extended
5. Kordelle J, Frommelt L, Kluber D, Seemann K. Results of one-stage
aggressive debridement, and relatively comparable to a two-
endoprosthesis revision in periprosthetic infection cause by methicillin-resistant
D. KENDOFF, T. GEHRKE
Staphylococcus aureus. Z Orthop Ihre Grenzgeb 2000;138:240-4 (in German).
28. Hanssen AD, Osmon DR. Evaluation of a staging system for infected hip
6. Siegel A, Frommelt L, Runde W. Therapy of bacterial knee joint infection by radical
arthroplasty. Clin Orthop Relat Res 2002;403:16-22.
synovectomy and implantation of a cemented stabilized knee joint endoprosthesis. Der
29. Parvizi J GE, Menashe S, Barrack RL, Bauer TW. Periprosthetic infection: what
Chirurg 2000;71:1385-91 (in German).
are the diagnostic challenges? J Bone Joint Surg [Am] 2006;88-A:138-47.
7. Steinbrink K, Frommelt L. Treatment of periprosthetic infection of the hip using one-
30. Schinsky MF, Della Valle CJ, Sporer SM, Paprosky WG. Perioperative testing
stage exchange surgery. Orthopade 1995;24:335-43 (in German).
for joint infection in patients undergoing revision total hip arthroplasty. J Bone Joint Surg
8. Schmitz HC, Schwantes B, Kendoff D. One-stage revision of knee endoprosthesis
due to periprosthetic infection and Klippel-Trenaunay syndrome. Orthopade 2011;40:624-
31. Schafer P, Fink B, Sandow D, et al. Prolonged bacterial culture to identify late
periprosthetic joint infection: a promising strategy. Clin Infect Dis 2008;47:1403-9.
9. Fehring TK, Odum S, Calton TF, Mason JB. Articulating versus static spacers in
32. Della Valle CJ, Sporer SM, Jacobs JJ, et al. Preoperative testing for sepsis
revision total knee arthroplasty for sepsis: The Ranawat Award. Clin Orthop Relat Res
before revision total knee arthroplasty. J Arthroplasty. 2007;22(Suppl):90-3.
33. Ghanem E, Parvizi J, Burnett RS, et al. Cell count and differential of aspirated
10. Haddad FS, Masri BA, Campbell D, et al. The PROSTALAC functional spacer in
fluid in the diagnosis of infection at the site of total knee arthroplasty. J Bone Joint Surg
two-stage revision for infected knee replacements: prosthesis of antibiotic-loaded acrylic
cement. J Bone Joint Surg [Br] 2000;82-B:807-12.
34. Trampuz A, Hanssen AD, Osmon DR, et al. Synovial fluid leukocyte count and
11. Pietsch M, Wenisch C, Traussnig S, Trnoska R, Hofmann S. Temporary
differential for the diagnosis of prosthetic knee infection. Am J Med 2004;117:556-62.
articulating spacer with antibiotic-impregnated cement for an infected knee
35. Fink B, Makowiak C, Fuerst M, et al. The value of synovial biopsy, joint aspiration
endoprosthesis. Orthopade 2003;32:490-7 (in German).
and C-reactive protein in the diagnosis of late peri-prosthetic infection of total knee
12. Della Valle C, Parvizi J, Bauer TW, et al. Diagnosis of periprosthetic joint
replacements. J Bone Joint Surg [Br] 2008;90-B:874-8.
infections of the hip and knee. J Am Acad Orthop Surg 2010;18:760-70.
36. Gehrke T, Frommelt L, G. vF, eds. Pharmakokinetik Study of a Gentamycin/
13. Fink B, Vogt S, Reinsch M, Büchner H. Sufficient release of antibiotic by a spacer
Clindamycin Bone Cemnet Used in One Stage Revision Arthroplasty. In: Bone Cement and
6 weeks after implantation in two-stage revision of infected hip prostheses. Clin Orthop
Cementing Technique. Springer; 1998.
Relat Res 2011;469:3141-7.
37. Trampuz A, Osmon DR, Hanssen AD, Steckelberg JM, Patel R. Molecular and
14. Hanssen AD, Spangehl MJ. Practical applications of antibiotic-loaded bone
antibiofilm approaches to prosthetic joint infection. Clin Orthop Relat Res 2003;414:69-
cement for treatment of infected joint replacements. Clin Orthop Relat Res 2004;427:79-
38. Wahlig H, Dingeldein E, Buchholz HW, Buchholz M, Bachmann F.
15 Haleem AA, Berry DJ, Hanssen AD. Mid-term to long-term followup of two-stage
Pharmacokinetic study of gentamicin-loaded cement in total hip replacements:
reimplantation for infected total knee arthroplasty. Clin Orthop Relat Res 2004;428:35-9.
comparative effects of varying dosage. J Bone Joint Surg [Br] 1984;66-B:175-9.
16. Hoad-Reddick DA, Evans CR, Norman P, Stockley I. Is there a role for extended
39. Kordelle J, Klett R, Stahl U, et al. Infection diagnosis after knee-TEP-implantation.
antibiotic therapy in a two-stage revision of the infected knee arthroplasty? J Bone Joint
Z Orthop Ihre Grenzgeb 2004;142:337-43 (in German).
Surg [Br] 2005;87-B:171-4.
40. Frommelt L. Periprosthetic infection: bacteria and the interface between prosthesis
17. Goldman RT, Scuderi GR, Insall JN. 2-stage reimplantation for infected total knee
and bone. In: Learmonth ID, ed. Interfaces in total hip arthroplasty. London: Springer
replacement. Clin Orthop Relat Res 1996;331:118-24.
Verlag, 153-61.
18. Azzam K, McHale K, Austin M, Purtill JJ, Parvizi J. Outcome of a second
41. Spangehl MJ, Masri BA, O'Connell JX, Duncan CP. Prospective analysis of
two-stage reimplantation for periprosthetic knee infection. Clin Orthop Relat Res
preoperative and intraoperative investigations for the diagnosis of infection at the
sites of two hundred and two revision total hip arthroplasties. J Bone Joint Surg [Am]
19. Buechel FF. The infected total knee arthroplasty: just when you thought it was over.
J Arthroplasty 2004;19(Suppl):51-5.
42. Kilgus DJ, Howe DJ, Strang A. Results of periprosthetic hip and knee infections
20. Buechel FF, Femino FP, D'Alessio J. Primary exchange revision arthroplasty
caused by resistant bacteria. Clin Orthop Relat Res 2002;404:116-24.
for infected total knee replacement: a long-term study. Am J Orthop (Belle Mead NJ)
43. von Foerster G, Klüber D, Käbler U. Mid- to long-term results after treatment
of 118 cases of periprosthetic infections after knee joint replacement using one-stage
21. Atkins BL, Bowler IC. The diagnosis of large joint sepsis. J Hosp Infect.
exchange surgery. Orthopade 1991;20:244-52 (in German).
44. Parkinson RW, Kay PR, Rawal A. A case for one-stage revision in infected total
22. Frommelt L. Diagnosis and treatment of foreign-body-associated infection in
knee arthroplasty? Knee 2011;18:1-4.
orthopaedic surgery. Orthopade. 2009;(Eupub ahead of print) PMID: 19756495.
45. Silva M, Tharani R, Schmalzried TP. Results of direct exchange or debridement of
23. Elek SD, Conen PE. The virulence of Staphylococcus pyogenes for man; a study of
the infected total knee arthroplasty. Clin Orthop Relat Res 2002;404:125-31.
the problems of wound infection. Br J Exp Pathol 1957;38:573-86 (in English, Italian).
46. Winkler H. Rationale for one stage exchange of infected hip replacement using
24. Zimmerli W, Lew PD, Waldvogel FA. Pathogenesis of foreign body infection:
uncemented implants and antibiotic impregnated bone graft. Int J Med Sci 2009;6:247-
evidence for a local granulocyte defect. J Clin Invest 1984;73:1191-200.
25. Costerton JW, Stewart PS, Greenberg EP. Bacterial biofilms: a common cause of
47. Lu H, Kou B, Lin J. One-stage reimplantation for the salvage of total knee
persistent infections. Science 1999;284(:1318-22.
arthroplasty complicated by infection. Zhonghua Wai Ke Za Zhi Aug 1997;35:456-8 (in
26. Zimmerli W, Trampuz A, Ochsner PE. Prosthetic-joint infections. N Engl J Med.
27. McPherson EJ, Woodson C, Holtom P, et al. Periprosthetic total hip infection:
48. Selmon GP, Slater RN, Shepperd JA, Wright EP. Successful 1-stage exchange
outcomes using a staging system. Clin Orthop Relat Res 2002;403:8-15.
total knee arthroplasty for fungal infection. J Arthroplasty 1998;13:114-15.
THE JOURNAL OF BONE AND JOINT SURGERY
Source: http://www.kendoff.de/pdf/one-stage-exchange-arthroplasty.pdf
Policy Brief • April 2016 GPE's Work in Conflict-affected and Fragile Countries Accelerated Support in Emergency and Early Recovery Situa-tions, GPE has successfully promoted coordinated deci-sions about the best way to utilize resources in crisis settings, such as shifting them to non- governmental 28 GPE's developing country partners are classified providers for direct service provision during acute
The NEW ENGL A ND JOUR NA L of MEDICI NE Helping Smokers Quit — Opportunities Created by the Affordable Care ActTim McAfee, M.D., M.P.H., Stephen Babb, M.P.H., Simon McNabb, B.A., and Michael C. Fiore, M.D., M.P.H., M.B.A. In its review of tobacco-dependence treatments, thereby increase rates of cessa- the 2008 clinical practice guideline of the U.S.