Levitra enthält Vardenafil, das eine kürzere Wirkdauer als Tadalafil hat, dafür aber schnell einsetzt. Männer, die diskret bestellen möchten, suchen häufig nach levitra kaufen ohne rezept. Dabei spielt die rechtliche Lage in der Schweiz eine wichtige Rolle.
Neurostation.net
Pseudotumor Cerebri: Brief Review of Clinical
Syndrome and Imaging Findings
SUMMARY: PTC is a clinical entity of uncertain etiology characterized by intracranial hypertension. The
syndrome classically manifests with headaches and visual changes in women with obesity. Tradition-ally, imaging ruled out secondary causes of elevated CSF pressure but now may reveal findingsfrequently seen in patients with PTC, including the following: flattening of the globe, an empty sella,an enlarged ONS, protrusion and enhancement of the optic nerve head, and increased tortuosity of theoptic nerve. Novel imaging methods, including MR venography, have additionally identified sinovenousstenosis as a potential indicator of PTC.
ABBREVIATIONS: BMI ⫽ body-mass index; CN ⫽ cranial nerve; HIV ⫽ human immunodeficiency
virus; ICP ⫽ intracranial pressure; IIH ⫽ idiopathic intracranial hypertension; ISF ⫽ interstitial fluid;
MRI ⫽ MR imaging; ONS ⫽ optic nerve sheath; ONSF ⫽ optic nerve sheath fenestration; IOP ⫽
intraocular pressure; PCOS ⫽ polycystic ovary syndrome; PTC ⫽ pseudotumor cerebri syndrome
Several formalized criteria for IIH exist in the literature and
known and putative etiologies. In the history of this condi-
are subject to extensive debate. The Modified Dandy Criteria
tion, the name given to the clinical syndrome referred to as
first incorporated the use of CT in the diagnosis of IIH, pri-
PTC or more commonly IIH has varied widely and been the
marily as a means of excluding occult causes of intracranial
subject of much contention.1 Heinrich Quincke, an early pio-
hypertension previously missed in the era before diagnostic
neer in the use of lumbar puncture, reported the first recorded
imaging.9 Friedman and Jacobson7 updated these criteria (Ta-
cases of intracranial hypertension of unknown cause in what
ble 2) to reflect the advances of MR imaging and the charac-
he described as "meningitis serosa" in 1893; at that time, he
terization of other etiologies of intracranial hypertension such
posited that inadequate CSF resorption was responsible for
as venous thrombosis.
the syndrome, a theory that is still entertained by some re-
Additional caveats have been proposed as conditions in the
searchers.2 The term "PTC" was coined in 1904 by Nonne to
diagnosis of IIH: excluding patients who have intracranial si-
describe a condition characterized by symptoms associated
nus venous thrombosis, a systemic condition associated with
with intracranial tumors with an unusual course of remission
elevated right heart pressure, or those who have been exposed
and subsequently termed "benign intracranial hypertension"
to medications or toxins associated with increased intracranial
by Foley in 1955.1
hypertension such as those mentioned in Table 1.4,5
The absence of a clear identifiable etiology for a clinical
syndrome characterized by elevated ICP exists in nearly 90%
of cases, and this ambiguity inevitably has led to the replace-
The precise etiology of IIH, as the name suggests, is largely
ment of the misnomer "benign" intracranial hypertension
unknown, despite much clinical investigation and basic sci-
with IIH in light of the incidence of vision loss resulting from
ence research. Theories generally fall under 5 different pro-
this condition.3 Despite numerous revisions during the past
posed mechanisms resulting in elevated intracranial hyperten-
century, these definitions remain inadequate and limited in
sion as outlined in Table 3 and discussed at greater length in
that some cases of IIH have identifiable etiology, such as dural
the article by Walker.10 Older theories, including those of
venous stenosis, which has been implicated in 14%–90% of
Quincke, suggest a disturbance of CSF homeostasis, either im-
patients with IIH.4-6 For this reason, certain authors proposed
pairment of reabsorption or excess production of CSF.1,11
the use of PTC as a catchment for both categories: purely IIH
Many researchers cite case studies showing CSF collections as
and that due to secondary causes of intracranial hypertension
proof of this theory of disordered CSF hydrodynamics.12 Crit-
such as venous stenosis.5 We prefer the more encompassingterm "PTC" to reflect diagnostic limitations in elucidating
ics of this traditional hypothesis point to the intermittent suc-
potential secondary causes of IIH, such as those listed in Table
cess of lumbar puncture, which, from a physiologic stand-
1.7,8 Another argument proposes a classification of isolated
point, should alleviate the symptoms due to excess CSF and, in
intracranial hypertension as being either idiopathic or
addition, the lack of expansion of ventricles, which would oc-
cur if CSF volume was increased as in the case of meningitis-induced hydrocephalus.10
Many cases of PTC may not, in fact, be idiopathic but
From the Department of Radiology, George Washington University Hospital, Washington,
rather secondary to venous thrombosis, which many argue is
frequently missed if MR venography is not used to evaluate
Please address correspondence to Lucien M. Levy, Department of Radiology, GeorgeWashington University Hospital, 900 23rd Street N.W., Washington, DC 20037; e-mail:
patients with suspected PTC.13 As a result, 1 author proposed
classifying benign intracranial hypertension as either idio-pathic (also called PTC) or venogenic, if caused by thrombo-
Indicates open access to non-subscribers at www.ajnr.org
sis, vasculitis, extrinsic venous compression, or intraluminal
Degnan 兩 AJNR 32 兩 Dec 2011 兩 www.ajnr.org
Table 1: Confounding conditions that may present as similar to IIHa
Table 2: Criteria for diagnosing IIHa
Medical disorders
1) If symptoms are present, they may only reflect those of generalized
intracranial hypertension or papilledema
2) If signs are present, they may reflect only those of generalized
Chronic obstructive pulmonary disease
intracranial hypertension or papilledema
Right heart failure with pulmonary hypertension
3) Documented elevated ICP measured in the lateral decubitus position
Obstructive sleep apnea
(findings of assessment of ICP by lumbar puncture are considered
Pickwickian syndrome
abnormal if above 20 cm H O in normal-weight individuals and 25 mm
Polycystic ovary syndrome
H O in obese individuals20); MRI abnormal if above 20 cm H O in normal-
Systemic lupus erythematosus
weight individuals and 25 mm H O in obese individuals20)
4) Normal CSF composition
Severe iron deficiency anemia
5) No evidence of hydrocephalus, mass, structural, or vascular lesion on MRI
or contrast-enhanced CT for typical patients and on MRI and MR
Tetracycline and related compounds (minocycline, doxycycline)
venography for all others
Vitamin A (at doses ⬎25 000 IU daily) and related compounds
6) No other cause of intracranial hypertension identified
(isotretinoin 关Accutane兴, vitamin supplements, excessive intake
a Adapted from Friedman and Jacobson.7
of liver, all-trans retinoic acid)
Anabolic steroidsCorticosteroid withdrawal following prolonged administration
aches occur in nearly all (90%–94%) patients with PTC—they
Growth hormone administration in deficient patients
are characteristically pressurelike, throbbing, and usually un-
remitting and occur with retro-ocular pain and may be ac-
companied by nausea.19,20 Vision loss is the most feared se-
Oral contraceptive useLevonorgestrel implant system
quela of PTC, but most vision loss in this syndrome is transient
in nature and occurs in approximately 68%– 85% of pa-
tients.19-22 This vision loss less frequently takes the form of
impairments in the visual field, with the typical impairment
Obstruction to venous drainage
presenting as tunnel vision.19 Transient ischemia of the optic
Cerebral venous sinus thrombosis
nerve due to pressure is thought to explain the transient vision
Jugular vein thrombosisSuperior vena cava syndrome
changes.22 Pulse-synchronous tinnitus is another commonly
Jugular vein ligation following bilateral radical neck dissection
reported symptom of PTC (58% of patients) and is often de-
Increased right heart pressure
scribed as a unilateral "whooshing" sound by patients and may
be exacerbated by positional changes and relieved by jugular
Compression by tumor process (eg, meningioma)
compression.3,19,22 Other common symptoms include pho-
topsia (54%) and eye pain (44%).22 More severe symptoms are
HIV infection, borreliosisPostvaricella infection in children
less frequently encountered, yet diplopia (38%) and vision loss
(30%) occur in a significant number of patients.22
Adapted from Friedman and Jacobson,7 Szitkar,8 Wall,22 and Alperin et al.79
Ophthalmologic signs of PTC consist of diminished visual
A newer theory stemming from observations of sinus
acuity, visual field losses on formalized testing in nearly all
thrombosis producing a clinical presentation similar to IIH
patients, and, most strikingly, papilledema on funduscopic ex-
suggests that most cases of IIH are due to venous outflow
amination in 40% of patients.19,22 Visual loss is directly corre-
obstruction, which can also take the form of stenosis in the
lated with the extent of disc edema, which is thought to result
absence of thrombosis.14 The observation of stenotic trans-
from elevated IOP referred from elevated CSF pressure.23 An-
verse sinuses in ⬎90% of patients with IIH in 1 study gives
atomic connections between the cranial fossa and orbit are
credence to this thinking.6 There is clinical evidence to sup-
thought to explain why ICP directly correlates with IOP.24
port the idea that impaired venous outflow leads to increased
Absence of papilledema has been reported in many popula-
total blood flow.6 Even if it is assumed that venous stenosisexists in PTC, there is controversy as to whether venous ste-
tions of patients with IIH, but its absence may be more sug-
nosis and elevated venous pressure are due to elevated ICP or
gestive of an alternative etiology for headache and vision
constitute the proximal cause of PTC.14-16 The first explana-
loss.19 Other funduscopic findings that may be seen in PTC are
tion is an application of the Monroe-Kellie doctrine: Expan-
choroidal folds, parallel striae of alternating yellow crests, and
sion of the brain within a fixed space will lead to the compres-
darker troughs; choroidal folds compromise vision and can be
sion of venous sinuses, assuming that these are compressible
seen with elevated ICP, even when papilledema has re-
structures, to vent CSF during systole when ICP increases.17
solved.25,26 Cranial nerve palsies, usually of the abducens
One cadaveric study suggested that the stenosis of the trans-
nerve (CN VI), may occur as well in as many as 10%–20% of
verse sinus observed in IIH might be due to the presence of a
patients.27 Rarely, facial nerve (CN VII) palsies may be associ-
large septum within the venous sinus.18
ated with IIH; all of these CN palsies are thought to occur as aresult of direct compression due to elevated ICP.22
PTC is a rare condition, occurring in the general population
PTC classically presents with headache and, frequently, vision
with an incidence of 0.9 cases per 100,000 population in 2
changes in women with obesity of childbearing age.19 Head-
epidemiologic studies in the United States.28,29 PTC demon-
AJNR Am J Neuroradiol 32:1986 –93 兩 Dec 2011 兩 www.ajnr.org
it is uncertain whether the exact mechanism of this increased
Table 3: Putative theories to explain elevated ICP in PTCa
risk is related to a prothrombotic state, enhanced estrogenic-
Proximal Etiology
ity, inflammatory cytokine expression, endocrinologic dys-
Increased interstitial fluid (ISF)
Increased cerebral volume
function, or some other yet-to-be-ascertained mechanism.
While more common in reproductive-age women, PTC
Increased blood volume
may occur as a slightly different clinical entity in other popu-
Increased tissue volumeIncreased CSF production rate
Increased CSF volume
lations.4 These older patients are more likely to be men, pres-
Increased CSF outflow resistance
ent with different symptoms (fewer headaches, more visual
Loss of cerebral autoregulation
Increased cerebral arterial pressure
changes), and have identifiable etiologies for elevated ICP,
Increased cerebral venous pressure
Increased venous blood volume and
which arguably disqualify these patients from fitting the crite-
ria for IIH on further clinical investigation.4 Men with PTC are
Reduced CSF outflow and increased
less likely to be obese (25% versus 75% of women) and are at a
twice greater risk of vision loss than women with PTC.39,40
(Adapted from Walker.10)
PTC is rare within the pediatric population and generally
strates a strong female predominance, with a female/male ra-
occurs with greater frequency in postpubertal females, obesity
becoming a significant risk factor with older age.41 PTC occur-
Reported risk factors for the development of PTC, includ-
ring in prepubertal children generally lacks any sex predilec-
ing those discussed here, mostly originated from case reports,
tion or association with obesity and is thought to have less risk
whereas very few controlled studies of PTC risk factors exist in
of permanent vision loss.42
the literature.20 As a result, some of these risk factors may beconfounded by their coexistence in the at-risk population; for
Management and Outcomes
example, PCOS occurs more frequently in reproductive-age
IIH and PTC were typically thought of as self-limiting condi-
women with obesity, yet 1 study posited an association be-
tions with little risk of major sequelae, which, in part, explains
tween PCOS and PTC while failing to control for the increased
the historical name "benign intracranial hypertension"; how-
incidence of PCOS in women with obesity, who are already at
ever, severe deficits of visual acuity may occur in as many as
increased risk of PTC.30
one-quarter of patients without treatment.29 Recently, some
Classically, PTC is more commonly observed in overweight
racial disparities in outcome have been noted, in which black
women of reproductive age.24 The incidence of PTC in women
patients are more than 3 times as likely to have severe visual
who are between 20 and 44 years of age and 20% above ideal
loss, even with equivalent access to treatment; severe visual
body weight increases to 19.3 cases per 100,000 population;
loss was present in 23% of black patients versus 7% of non-
the odds ratio of PTC increases from 6.5 for a BMI of 25–29 to
black patients.43 Patients with PTC also appear to have depres-
26.0 for a BMI of ⬎35.28,31 Obesity has long been associated
sion and anxiety to a greater extent than weight-matched con-
with the development of PTC.10,31,32 One mechanistic theory
trols and healthy controls.44 Health-related quality-of-life
proposes that obesity predisposes patients to having elevated
scores are also affected in PTC, with patients reporting signif-
intrabdominal pressure, elevated intrathoracic pressure, and
icantly lower general health than controls and patients with
thus elevated central venous pressure as the final common
other neuro-ophthalmologic conditions.31
pathway leading to IIH.32 Randhawa and Van Stavern26 point
Restoration of visual acuity and resolution of papilledema
out that this explanation fails to elucidate a female predomi-
constitute the primary goals of management in PTC and the
nance. A recent study counters this theory of increased central
benchmark of relative success of a treatment technique. The
venous pressure by discovering lower body (gynecoid) obesity
fact that most cases of PTC spontaneously resolve and that
as a risk factor for IIH, which may suggest that increased es-
most treatment studies lack control groups limits our inter-
trogenicity, rather than elevated intrabdominal pressure, is the
pretation of outcome measures reported for many treatment
inciting element by which obesity propagates IIH.33
modalities.45 Conservative measures are typically recom-
In keeping with enhanced estrogenicity in the obese, others
mended in patients without vision changes as the predomi-
propose endocrinologic dysregulation leading to a prothrom-
nant presentation and consist of weight loss and medication.20
botic state in obesity and, similarly, in pregnancy, as the path-
These conservative approaches may take time to take effect; as
way that promotes PTC.34 Other studies note increased leptin
a result, frequent follow-up, including formal visual field test-
levels in obese patients with IIH compared with both obese
ing at intervals of 1 month, 3 months, and then every 3– 6
and nonobese controls,35 while another group did not find
months, is advisable.20
significant differences between leptin levels of patients and
Weight loss is thought to address 1 of the fundamental risk
controls.36 A recent study found similar CSF leptin levels in
factors for recurrence of PTC and may reduce the risk of PTC
patients with PTC but noted significantly increased CSF levels
and concomitant vision impairment through reductions of
of the inflammatory cytokine CCL2.37 Still another divergent
central venous pressure or a tentative endocrinologic mecha-
explanation for obesity in PTC is that intracranial hyperten-
nism.32 Gastric bypass surgery was associated with remittance
sion leads to hyperphagia; according to this theory, obesity is
of symptoms in all but 1 of 19 patients with a history PTC in 1
the result rather than the proximal cause of PTC.38 However, if
study; notably, symptoms only recurred in the 2 patients who
PTC was the cause of obesity, one would expect more women
regained weight following surgery. Another case report dem-
to present with symptoms of increased ICP before weight gain
onstrated a reduction of dural venous sinus pressure in 2 pa-
under this theory. Thus, while obesity is long-established as a
tients following bariatric surgery.46,47
substantial risk factor for the development of PTC in women,
Medications to treat and prevent recurrence of PTC typi-
Degnan 兩 AJNR 32 兩 Dec 2011 兩 www.ajnr.org
Table 4: Imaging Findings in PTC
Agid et al, 200666
Yuh et al, 200064
Partially empty sella/decreased pituitary height
Agid et al, 200666
Yuh et al, 200064
Brodsky and Vaphiades, 199862
Flattened posterior globe/sclera
Agid et al, 200666
Brodsky and Vaphiades, 199862
Jinkins et al, 199671
Enlarged ONS (perioptic subarachnoid space)
Agid et al, 200666
Brodsky and Vaphiades, 199862
Increased tortuosity of optic nerve
Agid et al, 200666
Brodsky and Vaphiades, 199862
Enhancement of optic nerve
Agid et al, 200666
Brodsky and Vaphiades, 199862
Intraocular protrusion of optic nerve head
Agid et al, 200666
Brodsky and Vaphiades, 199862
Slitlike ventricles
Agid et al, 200666
cally have activity against carbonic anhydrase, which has been
which ONSF relieves symptoms.51 While some studies have
found to decrease the rate of CSF production, and thus address
alleged that the incidence of serious complications from ONSF
1 of the proposed mechanisms of PTC.22 Acetazolamide is
is as low as 1%, ONSF may result in worsening vision, infec-
historically the most commonly used medication to treat PTC,
tion, oculomotor dysfunction (albeit generally temporary),
but topiramate has been shown to have equal effect as a result
and death (in 1 older study).20,22,52 Following ONSF, visual
of partial carbonic anhydrase⫺inhibition activity augmented
acuity stabilized or improved in 94% of eyes and deteriorated
by beneficial analgesic action against headaches and weight
in 6% of eyes in 2 studies.52,53 ONSF in the pediatric popula-
loss as a fortuitous side effect.15,26,48 Corticosteroids may re-
tion improved visual acuity in two-thirds of patients, and vi-
sult in temporary remission of PTC, but the risks of chronic
sion worsened in 17% of patients.54
steroid use in already obese patients preclude their use. Some
Some groups propose the use of venous sinus stent place-
clinicians advocate the use of corticosteroids in patients with
ment to treat IIH on the basis of several imaging studies show-
severe headache, acute papilledema, and very high CSF
ing stenosis of the cerebral venous sinuses and the presump-
tion that venous outflow obstruction constitutes the
Therapeutic lumbar puncture is another common treat-
underlying etiology of most cases of IIH.24,55 One group at the
ment method and addresses the issue of elevated CSF pressure
University of Cambridge reported success with 5 of 12 patients
directly by reducing it immediately; 1 older study suggests that
rendered asymptomatic and 4 of 8 patients demonstrating res-
the effects are short-lived, with a return to initial pressure
olution of papilledema after venous sinus stent placement.55
within just ⬎1 an hour.50 There is little published evidence
Conversely, another group cited 3 cases of restenosis to coun-
comparing lumbar puncture with medication or other treat-
ter the belief that stent placement is a universally applicable
ment modalities.
procedure in IIH; they argued that stenosis in IIH may be the
More aggressive measures for preventing sequelae of PTC
result of the elevated ICP itself and not the cause of the in-
are traditionally reserved for 2 groups of patients: those who
creased ICP.56 Another researcher alleges that restenosis fol-
continue to experience vision loss despite conservative man-
lowing stent placement is the result of failure to support all of
agement and those who initially present with rapid vision loss.
the compliant portions of the venous sinus.57 Notably, the
Lumboperitoneal shunt surgery is a method in which the ele-
retrospective nonrandomized noncontrolled nature of these
vated CSF pressure is referred to the peritoneal cavity; this
studies substantially limits objective assessment of the relative
situation places the patient at risk of serious complications,
success of any of these treatment attempts.
ranging from shunt obstruction and shunt-related meningitisor abdominal infection to tonsillar herniation and death.20
Shunt failure occurs in roughly one-half of patients, and ap-
Historically, imaging of patients with PTC served the purpose
proximately one-tenth of patients have worsening vision fol-
of excluding other pathology responsible for symptoms of in-
lowing shunt surgery for IIH. As a result, shunt placement
creased ICP.58 Some of the earliest radiologic investigations of
necessitates frequent neurologic follow-up.22,49
PTC demonstrated evidence of decreased ventricle size and
Many ophthalmologists advocate ONSF (also called de-
sella turcica demineralization, thought to be a late manifesta-
compression) as an alternative surgical approach associated
tion of increased ICP, on plain film skull x-ray examination.59
with fewer complications and improved outcomes in the man-
The concept of decreased ventricle size as a sign of PTC
agement of refractory PTC.20,51 In this approach, the surgeon
emerged from these early studies.11,45 Early CT studies enabled
cuts slits in the ONS behind the globe to allow CSF to leak
clinicians to evaluate intracranial masses before lumbar punc-
from the subarachnoid space.22,49 Postoperative MR imaging
ture.58 Said and Rosman cautioned against using CT alone,
showing fluid collections adjacent to the site of fenestration
which has the potential of missing important pathology that
supports CSF extravasation into the orbit as the mechanism by
may explain increased ICP, especially in evaluating pediatric
AJNR Am J Neuroradiol 32:1986 –93 兩 Dec 2011 兩 www.ajnr.org
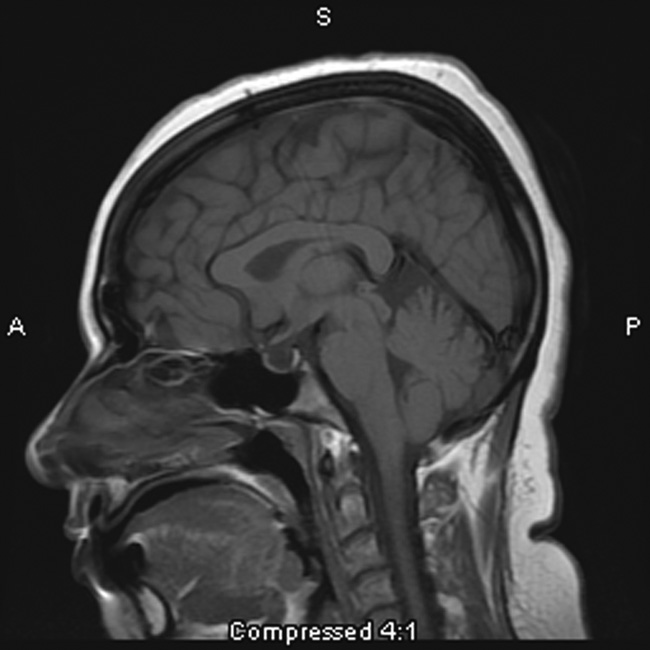

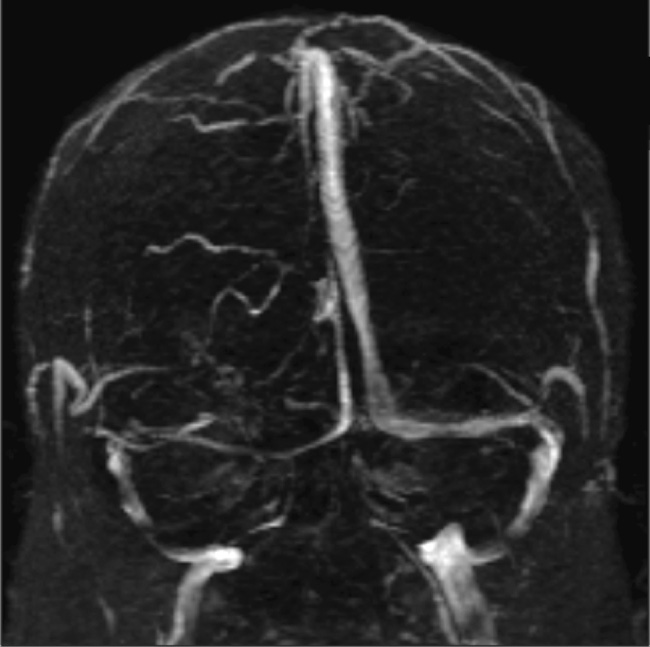
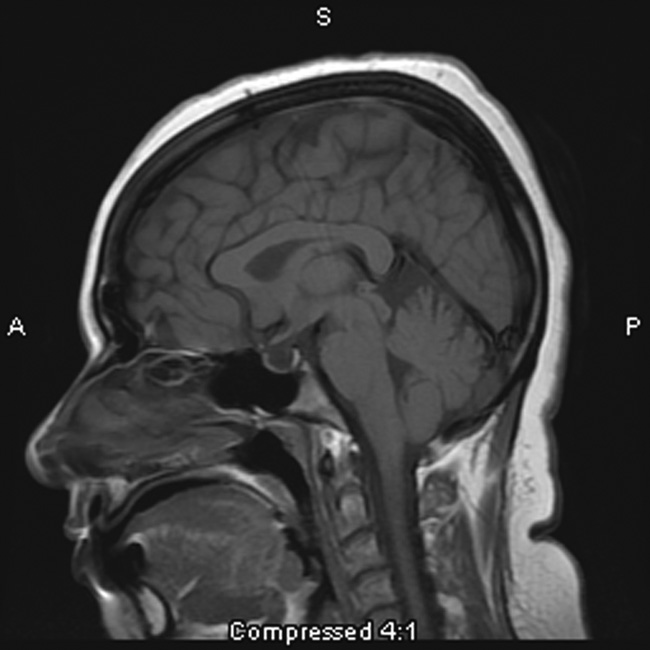
Fig 1. This 31-year-old woman presenting with headache is found to have an empty sella
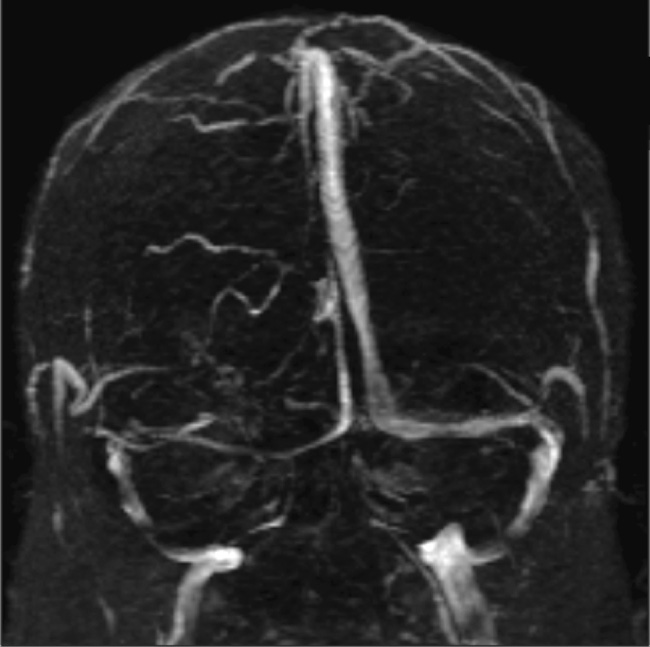
Fig 2. A narrowed right transverse sinus is noted in this 32-year-old woman, seen on MR
on sagittal T1-weighted MR imaging.
venography, in addition to ONS enlargement and a partially empty sella on axial MRimaging.
patients.60 The advent of MR imaging advanced the imagingparadigm in PTC from simply using imaging to rule out other
subject to interpretation.66-68 Globe flattening may be ex-
processes (eg, space-occupying lesions) to detecting signs
plained by the direct correlation between elevated ICP and
thought to indicate PTC itself.
IOP via the transmission of elevated CSF pressure through thesubarachnoid space, extending through the ONS to the poste-
rior globe.24 One possible confounding explanation for poste-
The American College of Radiologists, in their most recent
rior sclera flattening is its detection in the context of ocular
appropriateness criteria, recommended the use of fat-sup-
hypotony; however, this condition is more rare, and this neu-
pressed contrast-enhanced MR imaging of the brain for the
roimaging finding is more likely to be indicative of intracranial
evaluation of any disorder involving vision changes.61 Several
neuroimaging findings have been put forth as signs support-
Intraocular protrusion (Fig 3) is thought to occur in a man-
ing intracranial hypertension or even more specifically PTC.
ner similar to posterior globe flattening and is another sign
Estimates of the occurrence, sensitivity, specificity, and rele-
associated with PTC.70,71 The optic nerve head is considered
vance of these imaging signs vary widely in the published lit-
by some to be the most vulnerable site; thus, this finding on
erature and clinical practice and are summarized in Table 4.
MR imaging may well correspond to the presence of visual
These vast ranges of reported statistics and anecdotes most
symptoms, in light of its absence in patients with PTC lacking
likely result from the varying effort in detecting particular
visual symptoms.70 This finding has also been reported in pe-
signs at the expense of potentially ignoring other findings and
diatric patients as well.72
technical differences (particularly in MR venography).
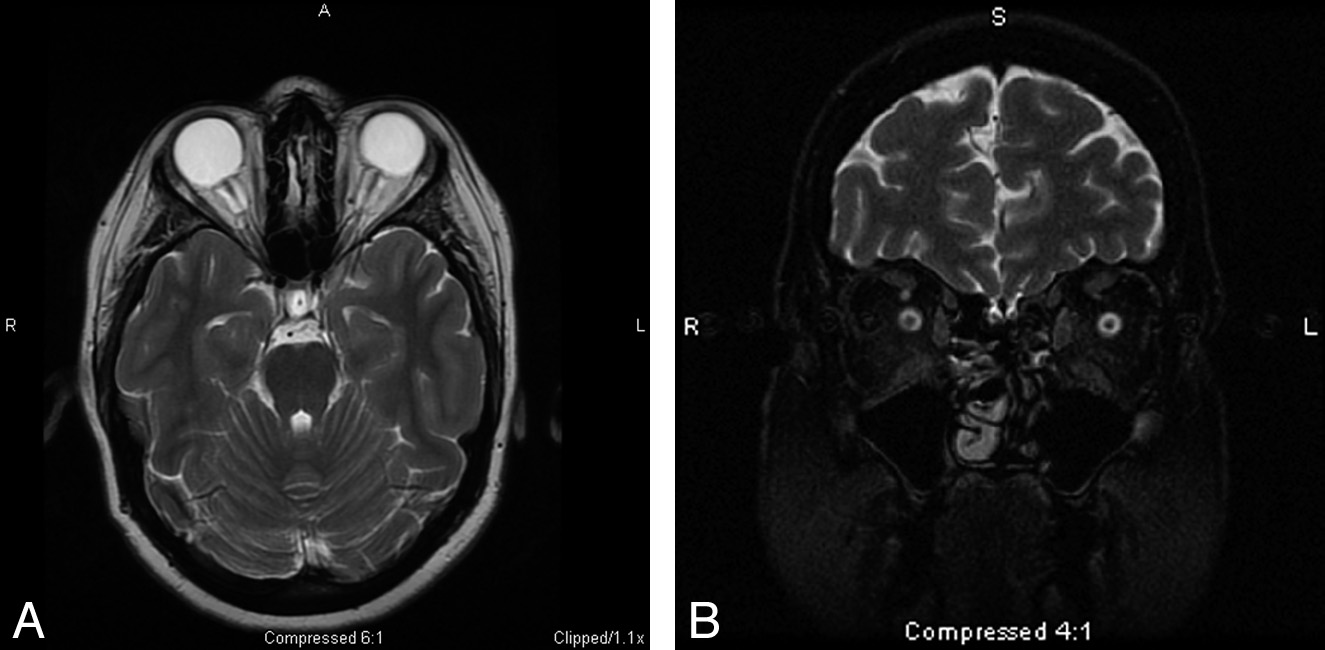
ONS enlargement (Fig 4A, -B) appears as a widened ring of
The "empty sella" sign (Fig 1) is associated with the long-
CSF around an optic nerve, which may appear compressed on
standing effects of increased ICP and is thought to result from
coronal images, and as widened CSF signal intensity on either
a downward herniation of an arachnocele through the dia-
side of the optic nerve on axial images.62 Studies of the effec-
phragma sella.45,62 It was 1 of the first signs noted on plain film
tiveness of ONSF emphasize the importance of this imaging
x-ray examination and subsequently on early MR imaging
finding.73 ONS enlargement on T2-weighted MR imaging re-
studies.59,63 The term "empty sella" should be reserved for
solves in patients in whom ONSF is successful, while those
studies in which the pituitary gland is not visible, and these
patients who remain symptomatic still have enlarged ONSs.73
cases tend to be later manifestations of increased ICP.64 Thereis a wide spectrum of pituitary height changes; thus, manycases of empty sella may, in fact, be better described as a par-tially empty sella or a compressed pituitary gland. The widerange of sensitivities and specificities reported reflects thisambiguity.
Transverse sinus narrowing (Fig 2) can be seen best on MR
venography as well as on sagittal and axial MR imaging and isthought to represent the effect of increased ICP.15 A small orabsent bony groove in the occiput in conjunction with thecompressible nature of the transverse sinus makes this struc-ture vulnerable to tapering with increased ICP.65 This partic-ular imaging finding is more frequently noticed on MR venog-raphy studies, which are discussed at more length below.6
Posterior globe flattening is considered by some authors to
Fig 3. Protrusion of the right optic nerve head and horizontal tortuosity of the optic nerve
be the sine qua non neuroimaging sign of PTC and can be seen
are seen in this 21-year-old woman on axial T2-weighted MR imaging. Clinically, the
on both CT and MR imaging but may be a more subtle finding
patient presented with headaches, vision changes, and papilledema noted on examination.
Degnan 兩 AJNR 32 兩 Dec 2011 兩 www.ajnr.org
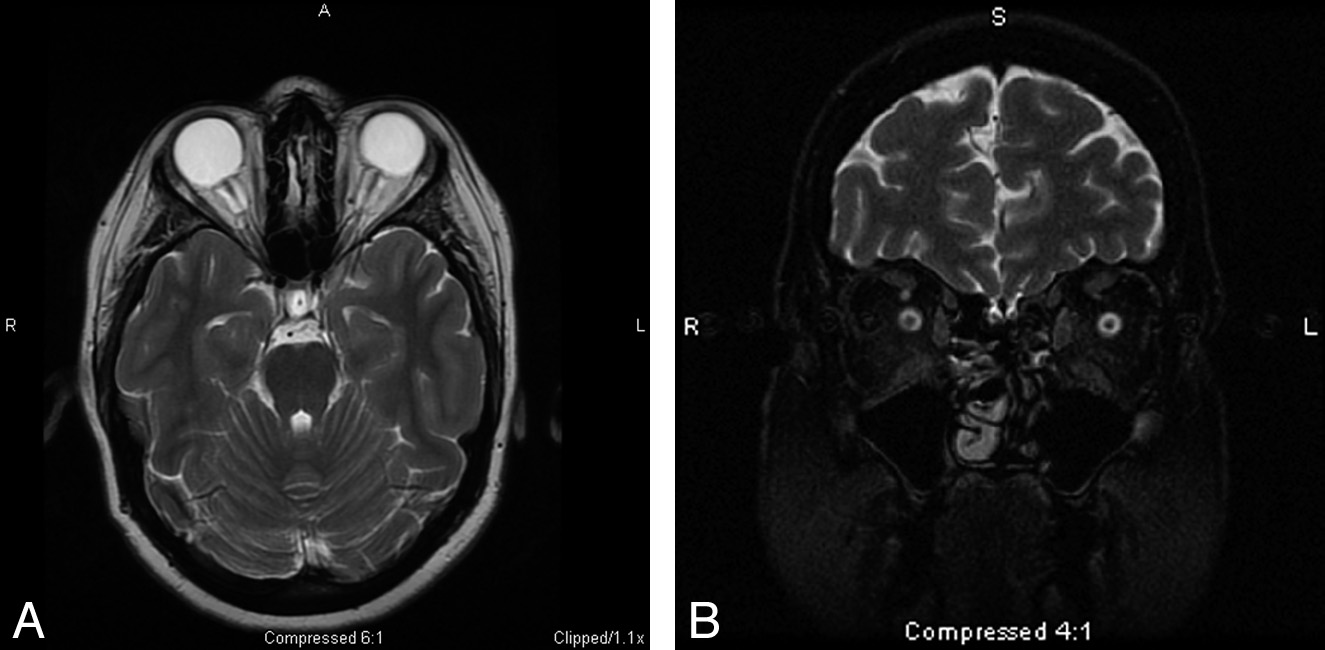
Fig 4. A, The ONS is widened with expanded CSF hyperintensity surrounding the optic nerve, seen on axial T2-weighted MR imaging in conjunction with posterior flattening of the globes.
ONS widening is thought to coincide with papilledema, which is seen in this 27-year-old woman who presented with headaches. B, Coronal T2-weighted MR imaging in a 55-year-old
woman with headache demonstrates increased peri-ONS space marked by hyperintense signal intensity surrounding the optic nerve.
Widening of the optic nerve has also been observed in child-
fied venous stenoses in 90% of patients with IIH with a re-
hood IIH.72 This association of ONS enlargement in PTC is
ported sensitivity and specificity of 93%. These findings have
supported by the converse association of the decreased diam-
similarly been replicated in the CT venography literature.77
eter of the ONS in patients with CSF hypovolemia.74
Further advancements in MR venography may demonstrate
Optic nerve tortuosity (Fig 3) has been associated with in-
stenosis of the venous sinuses to be an excellent indicator of
creased ICP; the distal and proximal points of fixation of the
the presence of elevated ICP.6
optic nerve enable it to kink freely in its course to the globe on
Yet another hypothesized imaging indicator of IIH seen on
protrusion of the intracranial contents under pressure.62 The
MR venography is increased total blood flow.78 In support of
sensitivity of observing optic nerve tortuosity in either the ver-
this finding, Bateman78 noted a 46% increase in total blood
tical or horizontal planes is dependent on section thickness.
flow in 5 patients with IIH and decreased blood flow in 7
Horizontal tortuosity is thought to be less frequently visual-
patients, with secondary intracranial hypertension due to
ized but more specific to intracranial hypertension.
thrombosis and arachnoid granulation in 1 patient. As with
Enhancement of the optic nerve is thought to be reflective
many research inquiries, this form of measurement is a rela-
of the same pathology leading to papilledema. Increased pres-
tive calculation of blood flow in patients compared with con-
sure referred from the cranial fossa generates venous conges-
trols and, as of yet, has no direct clinical application for eval-
tion, capillary leakage, and possible breakdown of the blood-
uating patients with suspected PTC.
retinal barrier.75 To evaluate for this finding, one must usecontrast.62
Other Imaging Methods
Slitlike ventricles appear to be a poor neuroimaging sign of
MR imaging measurement of intracranial elastance and its
PTC in light of the their infrequent occurrence.66 This finding
correlation with ICP is another technique that may prove
was first noted in older studies using ventriculography and
fruitful in averting a more invasive measurement of ICP
also in early CT studies, but it appears to be an insignificant
through lumbar puncture.79 Unfortunately, this imaging tech-
finding of little clinical use now.45,58,59
nique has only been studied in a limited population of healthycontrols and those with chronically elevated ICP, as well as in
baboons; moreover, complex calculations to correlate the elas-
Previously, it was thought that MR venography should be re-
tance index with ICP preclude clinical use at present.79 If val-
served for use in atypical (eg, male, normal weight) patients to
idated, this method would greatly improve the feasibility of
rule out sinovenous thrombosis.76 Now, many authors pro-
repeated measurement of ICP as part of routine evaluation
pose that any patient with suspected elevated intracranial hy-
pertension undergo MR venography in addition to traditionalMR orbital imaging to evaluate venous thrombosis or stenosis
Recommended Imaging Protocol
as the etiology of PTC symptoms.6,8,39,55 Newer imaging
In evaluating patients with headache, clinicians frequently or-
methods have enhanced detection of intracranial sinovenous
der routine brain MR imaging studies; thus, the radiologist
stenoses previously undetected due to artifactual flow voids in
must be cognizant of possible indicators of PTC on axial T2-
the transverse sinuses on traditional time-of-flight MR venog-
weighted images as discussed in this article. If there is an ad-
raphy.6 Higgins et al14 identified bilateral sinus flow gaps in
ditional clinical or imaging indication to suggest a greater like-
65% of patients with IIH by using 3D contrast-enhanced
lihood of PTC, we recommend the addition of coronal T2-
venography. By using a novel MR venography method, auto-
weighted imaging of the orbits to assess ONS widening and
triggered elliptic centric⫺ordered imaging, Farb et al6 identi-
MR venography to evaluate venous sinus thrombosis, sino-
AJNR Am J Neuroradiol 32:1986 –93 兩 Dec 2011 兩 www.ajnr.org
venous narrowing related to PTC, or congenital narrowing of
22. Wall M. Idiopathic intracranial hypertension. Neurol Clin 2010;28:593– 617
the venous sinuses.
23. Wall M. The morphology of visual field damage in idiopathic intracranial
hypertension: an anatomic region analysis. In: Mills RP, Heijl A, eds. Perimetry
Update 1990/1991. Amsterdam, the Netherlands: Kugler Publishers; 1991:20 –27
24. Sajjadi SA, Harirchian MH, Sheikhbahaei N, et al. The relation between intra-
cranial and intraocular pressures: study of 50 patients. Ann Neurol
PTC is a poorly understood clinical entity with a variety of
putative mechanisms, including excessive CSF production,
25. Griebel SR, Kosmorsky GS. Choroidal folds associated with increased intra-
impaired CSF resorption, and obstructed venous outflow. If
cranial pressure. Am J Ophthalmol 2000;129:513–16
26. Randhawa S, Van Stavern GP. Idiopathic intracranial hypertension (pseudo-
PTC is clinically suspected, patients should be imaged by using
tumor cerebri). Curr Opin Ophthalmol 2008;19:445–53
an orbital MR imaging study to rule out secondary causes of
27. Wall M, George D. Idiopathic intracranial hypertension: a prospective study
intracranial hypertension as well as to assess signs frequently
of 50 patients. Brain 1991;114:155– 80
28. Durcan FJ, Corbett JJ, Wall M. The incidence of pseudotumor cerebri: popu-
seen in PTC, including flattened posterior globes, increased
lation studies in Iowa and Louisiana. Arch Neurol 1988;45:875–77
ONS width, empty sella, increased tortuosity and enhance-
29. Radhakrishnan K, Ahlskog JE, Cross SA, et al. Idiopathic intracranial hyper-
ment of the optic nerve, and intraocular protrusion of the
tension (pseudotumor cerebri): descriptive epidemiology in Rochester,
Minn, 1976 to 1990. Arch Neurol 1993;50:78 – 80
optic nerve head. Many, additionally, advocate MR venogra-
30. Glueck CJ, Iyengar S, Goldenberg N, et al. Idiopathic intracranial
phy to detect sinovenous stenosis, which has been seen in
hypertension: associations with coagulation disorders and polycystic-ovary
many patients with PTC. Whether sinovenous stenosis is the
syndrome. J Lab Clin Med 2003;142:35– 45
31. Daniels AB, Liu GT, Volpe NJ, et al. Profiles of obesity, weight gain, and quality
cause or the result of intracranial hypertension remains unre-
of life in idiopathic intracranial hypertension (pseudotumor cerebri). Am J
solved, and the issue of therapeutic stent placement in the
Ophthalmol 2007;143:635– 41
32. Sugerman HJ, DeMaria EJ, Felton WL, et al. Increased intra-abdominal pres-
venous sinuses is contentious. Much more in the way of ran-
sure and cardiac filling pressures in obesity-associated pseudotumor cerebri.
domized controlled clinical trials is needed in the study of this
elusive condition.
33. Kesler A, Kliper E, Shenkerman G, et al. Idiopathic intracranial hypertension is
associated with lower body adiposity. Ophthalmology 2010;117:169 –74
34. Ooi LY, Walker BR, Bodkin PA, et al. Idiopathic intracranial hypertension: can
studies of obesity provide the key to understanding pathogenesis? Br J Neuro-
1. Pearce JM. From pseudotumour cerebri to idiopathic intracranial hyperten-
35. Lampl Y, Eshel Y, Kessler A, et al. Serum leptin level in women with idiopathic
sion. Pract Neurol 2009;9:353–56
intracranial hypertension. J Neurol Neurosurg Psychiatry 2002;72:642– 43
2. Johnston I. The historical development of the pseudotumor concept. Neuro-
36. Subramanian PS, Goldenberg-Cohen N, Shukla S, et al. Plasma ghrelin levels
surg Focus 2001;11:1–9
are normal in obese patients with idiopathic intracranial hypertension (pseu-
3. Giuseffi V, Wall M, Siegel PZ, et al. Symptoms and disease associations in
dotumor cerebri). Am J Ophthalmol 2004;138:109 –13
idiopathic intracranial hypertension (pseudotumor cerebri): a case-control
37. Dhungana S, Sharrack B, Woodroofe N. Cytokines and chemokines in idio-
study. Neurology 1991;41:239 – 44
pathic intracranial hypertension. Headache 2009;49:282– 85
4. Bandyopadhyay S, Jacobson DM. Clinical features of late-onset pseudotumor
38. Hannerz J, Ericson K. The relationship between idiopathic intracranial hyper-
cerebri fulfilling the modified Dandy criteria. J Neuroophthalmol
tension and obesity. Headache 2009;49:178 – 84
39. Kesler A, Goldhammer Y, Gadoth N. Do men with pseudotumor cerebri share
5. Sylaja PN, Ahsan Moosa NV, Radhakrishnan K, et al. Differential diagnosis of
the same characteristics as women? A retrospective review of 141 cases. J Neu-
patients with intracranial sinus venous thrombosis-related isolated intracra-
nial hypertension from those with idiopathic intracranial hypertension.
40. Bruce BB, Kedar S, Van Stavern GP, et al. Idiopathic intracranial hypertension
J Neurol Sci 2003;215:9 –12
in men. Neurology 2009;27:304 – 09
6. Farb RI, Vanek I, Scott JN, et al. Idiopathic intracranial hypertension: the
41. Balcer LJ, Liu GT, Forman S, et al. Idiopathic intracranial hypertension: rela-
tion of age and obesity in children. Neurology 1999;52:870 –72
2003;60:1418 –24
42. Kesler A, Fattal-Valevski A. Idiopathic intracranial hypertension in the pedi-
7. Friedman DI, Jacobson DM. Diagnostic criteria for idiopathic intracranial
atric population. J Child Neurol 2002;17:745– 48
43. Bruce BB, Preechawat P, Newman NJ, et al. Racial differences in idiopathic
8. Szitkar B. A meningioma exclusively located inside the superior sagittal sinus
intracranial hypertension. Neurology 2008;70:861– 67
responsible for intracranial hypertension. AJNR Am J Neuroradiol
44. Kleinschmidt JJ, Digre KB, Hanover R. Idiopathic intracranial hypertension:
relationship to depression, anxiety, and quality of life. Neurology
9. Smith JL. Whence pseudotumor cerebri? J Clin Neuroophthalmol 1985;5:55–56
2000;54:319 –24
10. Walker RW. Idiopathic intracranial hypertension: any light on the mecha-
45. George AE. Idiopathic intracranial hypertension: pathogenesis and the role of
nism of the pressure? J Neurol Neurosurg Psychiatry 2001;71:1–7
MR imaging. Radiology 1989;170:21–22
11. Levine DN. Ventricular size in pseudotumor cerebri and the theory of im-
46. Sugerman HJ, Felton WL, Sismanis A, et al. Gastric surgery for pseudotumor
paired CSF absorption. J Neurol Sci 2000;177:85–94
cerebri associated with severe obesity. Ann Surg 1999;229:634 – 40
12. Najjar MW, Azzam NI, Khalifa MA. Pseudotumor cerebri: disordered cerebro-
47. Nadkarni T, Rekate HL, Wallace D. Resolution of pseudotumor cerebri after
spinal fluid hydrodynamics with extra-axial CSF collections. Pediatr Neuro-
bariatric surgery for related obesity: case report. J Neurosurg 2004;101:878 – 80
48. Celebisoy N, Gokcay F, Sirin H, et al. Treatment of idiopathic intracranial
13. Silberstein SD, McKinstry RC. The death of idiopathic intracranial hyperten-
hypertension: topiramate vs acetazolamide, an open-label study. Acta Neurol
sion? Neurology 2003;60:1406 – 07
14. Higgins JNP, Gillard JH, Owler BK, et al. MR venography in idiopathic intra-
49. Matthews MK, Sergott RC, Savino PJ. Pseudotumor cerebri. Curr Opin Oph-
cranial hypertension: unappreciated and misunderstood. J Neurol Neurosurg
thalmol 2003;14:364 –70
50. Johnston I, Paterson A. Benign intracranial hypertension. II. CSF pressure and
15. Brazis PW. Pseudotumor cerebri. Curr Neurol Neurosci Rep 2004;4:111–16
16. Suzuki H, Takanashi J, Kobayashi K, et al. MR imaging of idiopathic intracra-
51. Yazici Z, Yazici B, Tuncel E. Findings of magnetic resonance imaging after
nial hypertension. AJNR Am J Neuroradiol 2001;22:196 –99
optic nerve sheath decompression in patients with idiopathic intracranial hy-
17. Bateman G. Stenoses in idiopathic intracranial hypertension: to stent or not to
pertension. Am J Ophthalmol 2007;144:429 –35
stent? AJNR Am J Neuroradiol 2008;29:215
52. Banta JT, Farris BK. Pseudotumor cerebri and optic nerve sheath decompres-
18. Subramaniam RM, Tress BM, King JO, et al. Transverse sinus septum: a new
53. Nithyanandam S, Manayath GJ, Battu RR. Optic nerve sheath decompression
2004;48:114 –16
for visual loss in intracranial hypertension: report from a tertiary care center
19. Friedman DI. Pseudotumor cerebri. In: Levin LA, Arnold AC, eds. Neuro-
in South India. Indian J Ophthalmol 2008;56:115–20
Ophthalmology: The Practical Guide. New York: Thieme; 2005:183– 86
54. Lee AG, Patrinely JR, Edmond JC. Optic nerve sheath decompression in pedi-
20. Lueck CJ, McIlwaine GG. Idiopathic intracranial hypertension. Pract Neurol
atric pseudotumor cerebri. Ophthalmic Surg Lasers 1998;29:514 –17
55. Higgins JNP, Cousins C, Owler BK, et al. Idiopathic intracranial hypertension:
21. Rowe FJ, Sarkies NJ. Assessment of visual function in idiopathic intracranial
12 cases treated by venous sinus stenting. J Neurol Neurosurg Psychiatry
hypertension: a prospective study. Eye 1994;12:111–18
2003;74:1662– 66
Degnan 兩 AJNR 32 兩 Dec 2011 兩 www.ajnr.org
56. Rohr A, Dorner L, Stingele R, et al. Reversibility of venous sinus obstruction in
68. Brodsky MC. Flattening of the posterior sclera: hypotony or elevated intracra-
idiopathic intracranial hypertension. AJNR Am J Neuroradiol 2007;28:656 –59
nial pressure? Am J Ophthalmol 2004;138:511
57. Bateman G. Stenoses in idiopathic intracranial hypertension: to stent or not to
69. Westfall AC, Ng JD, Samples JR, et al. Hypotonus maculopathy: magnetic res-
stent? AJNR Am J Neuroradiol 2008;29:215
onance appearance. Am J Ophthalmol 2004;137:563– 66
58. Lightfoote WE, Pressman BD. Increased intracranial pressure: evaluation by
70. Gass A, Barker GJ, Riordan-Eva P, et al. MRI of the optic nerve in benign
computerized tomography. Am J Roentgenol Radium Ther Nucl Med
intracranial hypertension. Neuroradiology 1996;38:769 –73
71. Jinkins JR, Athale S, Xiong L, et al. MR of optic papilla protrusion in patients
59. Jacobson HG, Shapiro JH. Pseudotumor cerebri. Radiology 1964;82:202–10
with high intracranial pressure. AJNR Am J Neuroradiol 1996;17:665– 68
60. Said RR, Rosman NP. A negative cranial computed tomographic scan is not
72. Mandelstam S, Moon A. MRI of optic disc edema in childhood idiopathic
adequate to support a diagnosis of pseudotumor cerebri. J Child Neurol
intracranial hypertension. Pediatr Radiol 2004;34:362
2004;19:609 –13
73. Sallomi D, Hibbert TJ, Sanders MD, et al. The MRI appearance of the optic
61. Wippold FJ. Orbits, vision, and visual loss. AJNR Am J Neuroradiol
nerve sheath following fenestration for benign intracranial hypertension. Eur
2010;31:196 –98
62. Brodsky MC, Vaphiades M. Magnetic resonance imaging in pseudotumor
74. Watanabe A, Horikoshi T, Uchida M, et al. Decreased diameter of the optic
cerebri. Ophthalmology 1998;105:1686 –93
nerve sheath associated with CSF hypovolemia. AJNR Am J Neuroradiol
63. Silbergleit R, Junck L, Gebarski SS, et al. Idiopathic intracranial hypertension
2008;29:863– 64
(pseudotumor cerebri): MR imaging. Radiology 1989;170:207– 09
75. Manfre L, Lagalla R, Mangiameli A, et al. Idiopathic intracranial hypertension:
64. Yuh WT, Zhu M, Taoka T, et al. MR imaging of pituitary morphology in
idiopathic intracranial hypertension. J Magn Reson Imaging 2000;12:808 –13
orbital MRI. Neuroradiology 1995;37:459 – 61
65. Connor SE, Siddiqui MA, Stewart VR, et al. The relationship of transverse
76. Lee AG, Brazis PW. Magnetic resonance venography in idiopathic pseudotu-
sinus stenosis to bony groove dimensions provides an insight into the aetiol-
mor cerebri. J Neuroophthalmol 2000;20:12–13
ogy of idiopathic intracranial hypertension. Neuroradiology 2008;50:999 –
77. Higgins JN, Tipper G, Varley M, et al. Transverse sinus stenoses in benign
1004. Epub 2008 Jul 12
intracranial hypertension demonstrated on CT venography. Br J Neurosurg
66. Agid R, Farb RI, Willinsky RA, et al. Idiopathic intracranial hypertension: the
2005;19:137– 40
78. Bateman GA. Vascular hydraulics associated with idiopathic and secondary
intracranial hypertension. AJNR Am J Neuroradiol 2002;23:1180 – 86
67. Madill SA, Connor SE. Computed tomography demonstrates short axial globe
79. Alperin NJ, Lee SH, Loth F, et al. MR-intracranial pressure (ICP): a method to
length in cases with idiopathic intracranial hypertension. J Neuroophthalmol
measure intracranial elastance and pressure noninvasively by means of MR
2005;25:180 – 84
imaging: baboon and human study. Radiology 2000;217:877– 85
AJNR Am J Neuroradiol 32:1986 –93 兩 Dec 2011 兩 www.ajnr.org
Source: http://neurostation.net/uploads/3/0/3/4/3034921/pseudotumor_cerebri-_brief_review_of_clinical_syndrome_and_imaging_findings.pdf
Available online at www.sciencedirect.com Phytochemistry 69 (2008) 1469–1495 Cordyceps – A traditional Chinese medicine and another fungal therapeutic biofactory? R. Russell M. Paterson * Institute for Biotechnology and Bioengineering (IBB), Centre of Biological Engineering, Campus de Gualtar, University of Minho, 4710-057 Braga, Portugal Received 17 December 2007; received in revised form 17 January 2008
European Journal of Neuroscience, Vol. 24, pp. 229–242, 2006 Progesterone reverses the spatial memoryenhancements initiated by tonic and cyclic oestrogentherapy in middle-aged ovariectomized female rats Heather A. Bimonte-Nelson,1 Kevin R. Francis,2 Claudia D. Umphlet2 and Ann-Charlotte Granholm21Department of Psychology, Arizona State University, PO Box 871104, Tempe, AZ 85287, USA2Department of Neuroscience and the Center on Ageing, Medical University of South Carolina, Charleston, SC 29425, USA