Levitra enthält Vardenafil, das eine kürzere Wirkdauer als Tadalafil hat, dafür aber schnell einsetzt. Männer, die diskret bestellen möchten, suchen häufig nach levitra kaufen ohne rezept. Dabei spielt die rechtliche Lage in der Schweiz eine wichtige Rolle.
Microsoft powerpoint - post partum haemorrhage [compatibility mode]
Post Partum Haemorrhage
Darent Valley Hospital
Risk Factors/Etiology
Communication, Resuscitation, Monitoring & Ix, Arresting the bleeding, drugs used
Patients who refuse blood
How to survive your first PPH

PREVENTION AND MANAGEMENT
OF POSTPARTUM HAEMORRHAGE
� Major cause of maternal death and morbidity despite a fall in
number in this triennium
� In the UK major obstetric haemorrhage is 3.7/1000
� 50% of the 500 000 maternal death globally is due to
� All units should have protocols in place for its identification and
� CMACE 2006-08 9 deaths 0.39/100 000
� Majority of these considered preventable
� Obstetric haemorrhage encompasses antepartum and
� APH often associated with subsequent PPH
Volume 118, Supplement 1, March 2011 BJOG An International
Journal of
Obstetrics and Gynaecology
Saving Mothers' Lives
Reviewing maternal deaths to make
motherhood safer: 2006–2008
March 2011
The Eighth Report of the Confidential
Enquiries into Maternal
Deaths in the United Kingdom
� 2 -Pre-eclampsia and
� 3 -Thromboembolism (18)
� 4- Amniotic fluid embolism
� 5- Early pregnancy deaths
� 6 -Haemorrhage (9)
Loss of >500 ml blood from genital tract within 24h of birth of baby
Minor (500-1000ml)
Major (>1000ml)
Moderate 1000-2000ml
Severe >2000ml
Abnormal/excessive bleeding from birth canal between 24h and 12/52 postnatally
All PPH are audited and reported on a monthly basis
International definition of PPH not unified:
� Traditional WHO definition of primary PPH encompasses all
blood losses > 500ml
� Est loss >1000ml appropriate cut off for major PPH and
initiation of emergency protocol measures other 1500ml
� Estimations of blood volume based on weight (weight kg/12)
� Allowing for physiological increase in pregnancy blood vol at
� Blood loss of >40% (approx 2800ml) total bld vol : ‘life-
� Consideration of antenatal Hb (<11g/dl Ix and Rx pre delivery)
� Evidence that iron-def anaemia assoc with atony secondary to
depleted uterine myoglobin levels (needed for muscle action)
� Visual blood loss estimates often underestimate true loss
Risk Factors for PPH
Most cases of PPH have no identifiable risk factors however the following increase the risk of PPH:
Four T's (Society of Obs and Gynae of Canada)
Lacerations, uterine rupture
Retained products
Coagulation disorders

Regular skill drills
Monitoring & Investigation
Arresting the bleeding
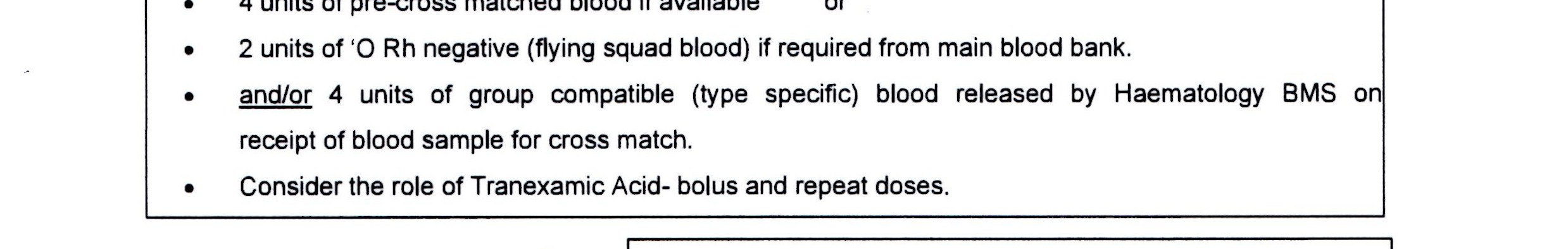
� Basic measures for minor PPH (500-1000ml)
� Alert midwife-in-charge
� Alert first-line obstetric and anesthetic staff
� Full protocol for major PPH
� Call experienced midwife (in addition to midwife in charge)
� Declare "code blue"
� Call obstetric middle grade and alert consultant
� Call anaesthetic middle grade and alert consultant
� Alert consultant clinical haematologist on callIf no code blue in place� Alert blood transfusion laboratory
� Call porters for delivery of specimens/bloodOne member of the team designated to record events, fluids,
drugs and vital signs
QuickTime™ and a
are needed to see this picture.
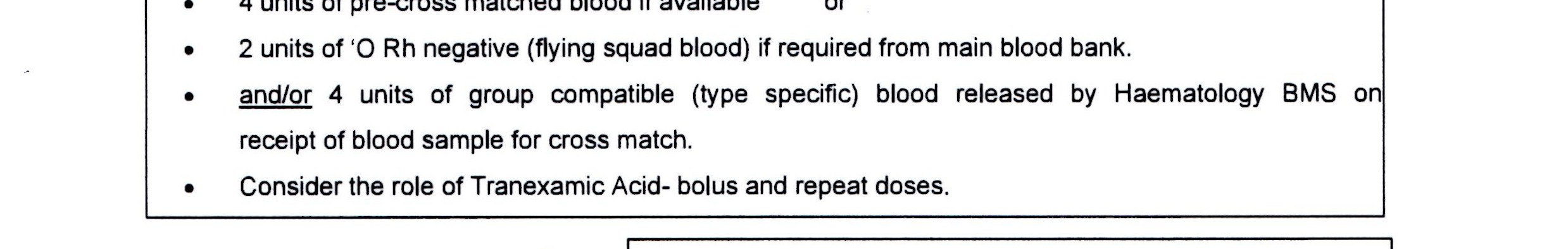
� Assess A, B, C � O2 10-15l/min� IV access (14G x2)� Position flat� Patient warming blanket� Transfuse PRC ASAP� Until available infuse up to 3.5l: of warmed crystalloid:
Hartmann's solution 2l +/- colloid 1-2l as rapidly as required
� Use best device available to achieve RAPID WARMED infusion
of fluids (eg level 1 rapid infusor)
� Special blood filters should NOT be used acutely - slow
� Recombinant factor VIIa therapy should be based on the results
of coagulation (Protocol)
up to 2L Hartmann's or Plasmalyte
up to 1-2L of colloid until the blood products
� Cell salvage if possible
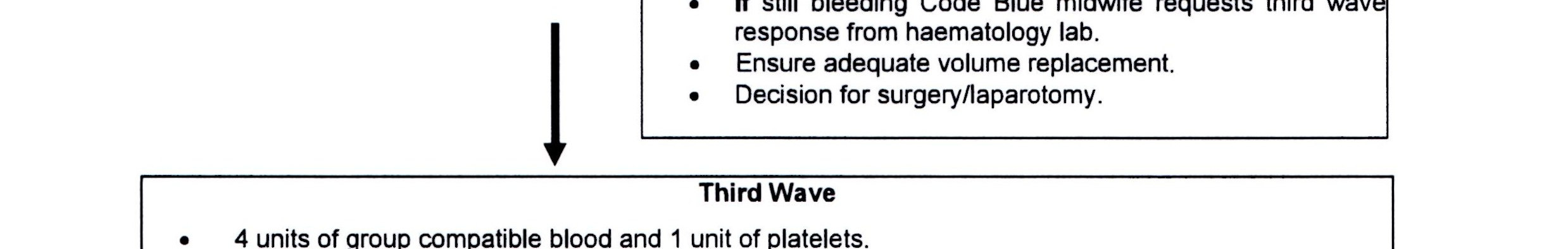
In an organised way, "Code Blue"
to contract the uterus
to help the coagulation
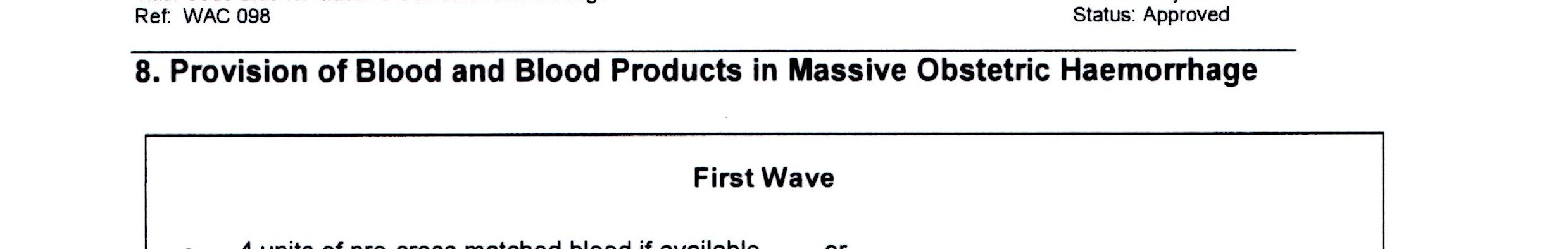
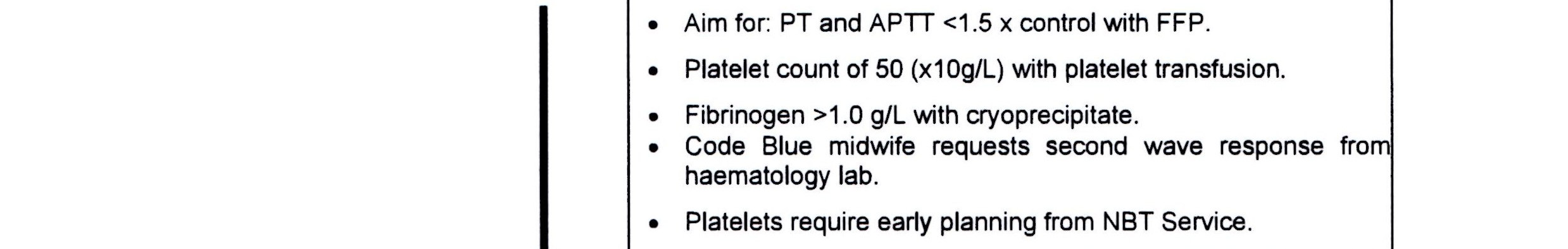
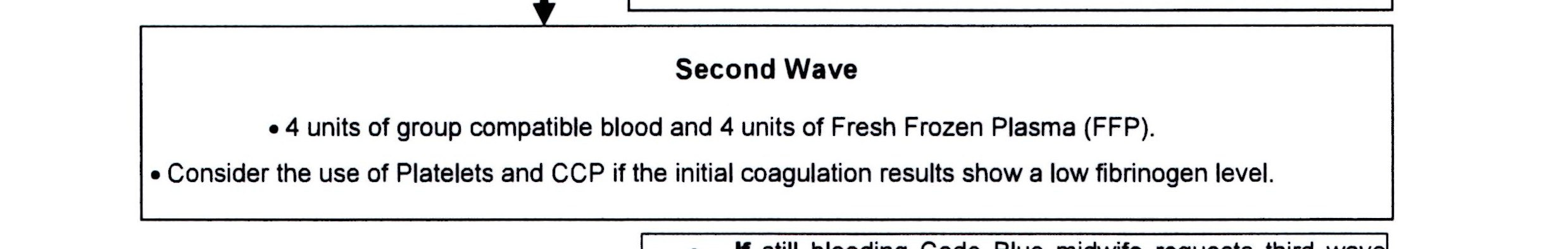
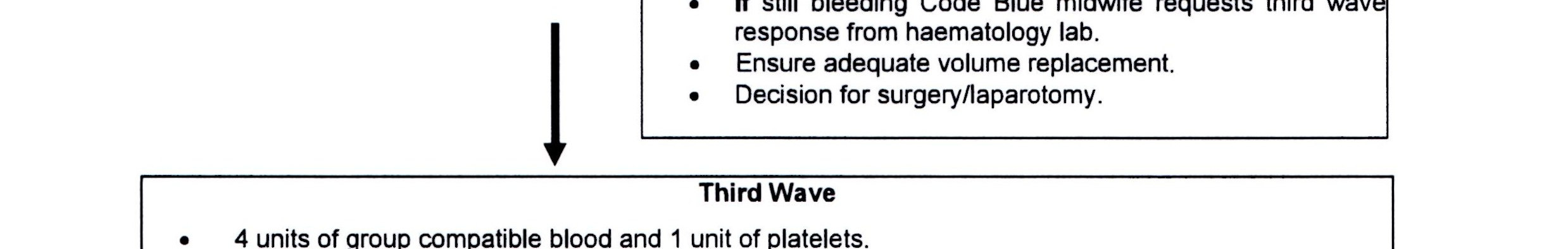
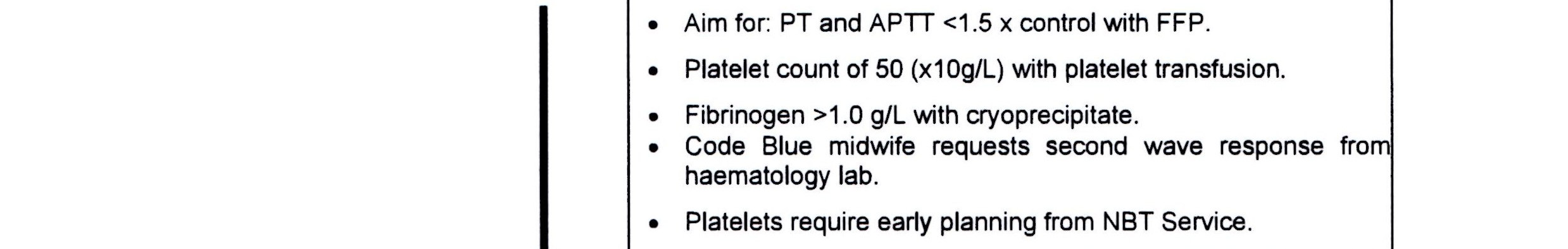
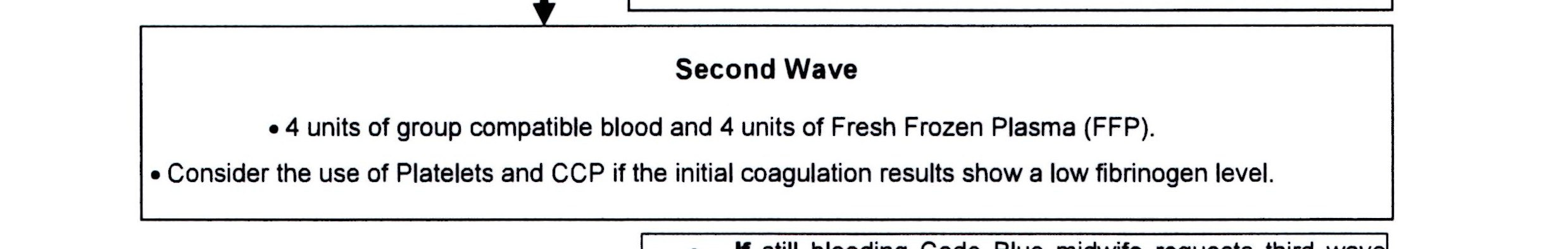
� 2006 guideline from British Committee for Standards in
Haematology - main therapeutic goals of management of massive blood loss is to maintain:
� PLT count > 75 x 10 9/l
� PT <1.5 x mean control
� APTT < 1.5 x mean control
� Fibrinogen > 1.0 g/l
Monitoring & Investigation
� X match if not already done(4 u min), FBC, Coagulation
(incl Fib), U&Es, LFTs
� Monitor temperature every 15 min� Continuous pulse, BP recording and RR (oximeter, ECG, NIBP)� Foley catheter for UO monitoring� 2 x 14/16G cannulae� Consider IABP� Consider transfer to ICU once bleeding controlled/ monitoring
on obstetric HDU if appropriate
� TRALI� Record parameters on HDU or equivalent chart� Documentation of fluid balance, blood, blood products and
How to stop the bleeding
� Causes for PPH may be considered to relate to one of the 4 Ts
� Tone, tissue, trauma, thrombin
� Most common cause of primary PPH is uterine atony
� Clinical examination necessary to exclude other causes:
� Retained products (placenta, membranes, clots)
� Vaginal/cervical lacerations or haematoma
� Ruptured uterus
� Broad ligament haematoma
� Extragenital bleeding (for example, subscapular liver
� Uterine inversion
Uterine Atony: a team effort
� Bimanual uterine compression (rubbing up the fundus) to
stimulate contractions
� Ensure bladder is empty (Foley catheter)
� Syntocinon 5 u by slow IV injection (may have repeat dose)
� Ergometrine 0.5mg by slow IV/IM injection (C/I in HTN)
� Syntocinon infusion (40u in 500ml @ 125ml/hr) or in 50mls if
� Carboprost 0.25mg IM injection repeated at intervals of not less
than 15min to max of 8 doses (C/I in asthma)
� Direct intramyometrial injection of carboprost 0.5mg (C/I in
asthma - responsibility with administering clinician as not recommended for intramyometrial use)
� Misoprostol 1000mcg PR
Surgical Haemostasis
� Intrauterine balloon tamponade
� Haemostatic brace suturing (B Lynch suture) delayed suture
(>2h) increases the rate of hysterectomy
� Bilateral ligation of uterine arteries
� Bilateral ligation of internal iliac arteries
� Selective arterial embolisation
� Resort to hysterectomy SOONER RATHER THAN LATER (esp
if placenta accreta or uterine rupture)
� UKOSS 40.6/100 000 hysterectomies to control haemorrhage
� 39% morbidly adherent placenta, main cause previous LSCS
Drugs to help the coagulation
� Tranexamic acid
� Recombinant Factor VIIa
Management of major PPH
� All women who have had a previous LSCS must have their
placental site determined.
� Identify women "at risk" and be prepared.
� Women delivered by LSCS must have regular obs recorded on
the MEOWS chart for the first 24hrs.
� RCOG recommend that women with major placenta praevia
who have previously bled should be admitted and managed as in patients from 34/40
� All clinicians should be aware of the guidelines for management
of women who refuse blood.
Jehovah's Witness
Optimise Hb during pregnancy, oral iron, IV iron, folic acid, recombinant human erythropoietin.
Advance directives from hospital and JW Hospital Committee
Anaesthetic clinic
Plan delivery as much as possible
Same management as any PPH but without being able to give blood.
Inform the consultant anaesthetist
Alert the consultant haematologist early.
Recombinant factor VIIa
Prothrombin complex concentrate Beriplex
Increase the dose of syntocinon, ensure good uterine contraction.
How to survive your first PPH
� Do not panic, think ABC � Do not join in the mass hysteria� Call for help i.e. consultant and senior
� If in doubt always declare a code blue� Beware of hidden blood loss� Be ahead of the game� Be assertive and ensure adequate
Source: http://www.odpskills.co.uk/pdf/pph.pdf
PROGETTO UNIVA 2013 Journal Club Pietro Gareri, MD, PhD Geriatra ASP Catanzaro Lamezia Terme 3 Luglio 2013 Drug-induced parkinsonism (DIP) was recognized in the early 1950s as a commoncomplication of antipsychotic therapy; initially considered to be present in 4 - 40%of patients treated with the first neuroleptics
Acorda Data on Inhaled Levodopa Therapy CVT-301 Recognized in Blue Ribbon Highlights Session at International Congress of Parkinson's Disease and Movement Disorders ARDSLEY, N.Y.--(BUSINESS WIRE)-- Acorda Therapeutics, Inc. (Nasdaq:ACOR) today announced that data from aPhase 2b clinical trial of CVT-301, an inhaled levodopa (L-dopa) under development for the episodic treatment ofOFF episodes associated with Parkinson's disease (PD), was included in the Blue Ribbon Highlights Session of the19th International Congress of Parkinson's Disease and Movement Disorders (MDS). Selected by a panel of experts,the Blue Ribbon Highlights Session provided a critical review of the best poster presentations, highlightingrelevance, novelty and quality of both clinical data and basic research. "Inhaled Levodopa (CVT-301) Provides RapidImprovement of OFF States in Parkinson's Disease" was one of only 19 posters selected from among the almost1,500 poster presentations at this year's conference.