Levitra enthält Vardenafil, das eine kürzere Wirkdauer als Tadalafil hat, dafür aber schnell einsetzt. Männer, die diskret bestellen möchten, suchen häufig nach levitra kaufen ohne rezept. Dabei spielt die rechtliche Lage in der Schweiz eine wichtige Rolle.
Poseido 2013.1(3).165-75 barone

POSEIDO. 2013;1(3) 165
Post-‐extraction implant: immediate vs delayed restoration
Research article
Immediate versus delayed restorations for implants
placed in fresh extraction sockets: a 1-year comparative
cohort study
Antonio Barone,1,2,* Valentina Borgia,2 Fortunato Alfonsi,2 Paolo Toti,1,2
and Ugo Covani.1,2
1 Department of Surgical, Medical, Molecular and Critical Area Pathology, University of Pisa, Pisa, Italy
2 Tuscan Dental Institute, Versilia General Hospital, Lido di Camaiore (LU), Italy *Corresponding author: Antonio Barone, [email protected]
Submitted on September 28th, 2013; accepted after minor corrections on October 10th, 2013.
Abstract
Background and objectives. Immediate implant placement can be considered a
predictable protocol, even in esthetic areas. The objective of this study was to compare the
clinical outcomes and the total costs of immediate and delayed restoration of implants with a
specific design placed into fresh extraction sockets after 1 year from the implant placement.
Materials and Methods. Blossom implants (Ossean, Intra-lock, Boca-Raton, FL, USA)
were used. In this prospective cohort study, marginal bone level, facial soft tissue, width of
keratinized gingiva and papilla index were compared in both groups; correlations with
pristine buccal bone thickness were also investigated.
Results. Marginal bone level records were different in the two groups, while no significant
differences were registered in facial soft tissue and keratinized gingiva width. In the delayed
group, a loss and reassessment of the papillary tissue was recorded at the time of restoration.
The immediate restoration group seemed to show better results in terms of healing time and
total costs.
Discussion and Conclusion. The immediate restoration protocol of immediately placed
implant seemed to have the same efficiency as the delayed restoration, besides offering other
clinical advantages.
Keywords. Bone resorption, dental implants, gingival recession, tooth socket.
1. Introduction
The placement of dental implants for replacing missing teeth is a widely used therapy,
also in esthetic areas. In the conventional protocol, implants are placed after the bone
healing, providing a highly predictable outcome [1,2]. The actual demand for reduced
treatment time and simpler protocol led to the immediate placement protocols, where
implants are put into fresh extraction sockets. Even if it is a technically demanding
procedure, the immediate implant procedure shows to be effective in reducing surgical steps,
overall treatment time, morbidity and costs for the patient [3,4].
Several aspects are involved in order to achieve a satisfactory outcome, such as
avoiding to raise a flap for controlling the facial bone resorption; leaving the buccal plate
ISSN 2307-5295, Published by the POSEIDO Organization & Foundation
under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported
(CC BY-NC-ND 3.0) License.
166 Research article: Barone A, et al. (2013)
intact; and placing the implant toward the palatal wall of the socket [5-8]. An adequate
surgical protocol can help to overcome the common difficulties of this technique, such as the
tri-dimensional implant positioning, the primary stability and the management of the bone
wall remodeling after a tooth extraction [9]. In particular, augmentation procedures have
shown to be effective in reducing the dimensional changes of the extraction socket and
correcting the peri-implant bone defects [10].
The immediate restoration of single maxillary implants placed in fresh extraction
sockets is a predictable technique with high survival rates [11,12]. The primary implant
stability and the lack of occlusal and eccentric contact during the healing phase are necessary
to achieve a successful result. Den Hartog at al. in a literature review asserted that there were
no differences in terms of survival rates for immediate and conventional load for implants
placed immediately after tooth extraction [13].
A crucial aspect in the anterior maxilla is the esthetics, but no or little information are
found regarding the soft tissues and the esthetic outcome of the immediate implants. Also,
the achievement of a satisfactory esthetics is influenced by the buccal bone remodeling and
the soft tissue healing, which could compromise the final result. Another factor that will
influence the final treatment plan is the cost-effectiveness of dental implant therapy, which
has been studied for more than twenty years [14,15].
The aim of the present study was to compare the overall clinical outcomes of immediate
and conventional restorations on immediate implants. The null hypothesis was that there were no differences between the two groups, while the alternative hypothesis was that there was a difference. The study reports the 1-year preliminary data.
2. Materials and Methods
2.1. Patient selection
Consecutively treated patients at Versilia General Hospital, University of Pisa, Lido di
Camaiore, Italy, between June 2008 and November 2010, were included in present prospective cohort study. The study was conducted according to the principles outlined in the declaration of Helsinki on clinical research involving human subjects, as revised in 2000. The two operators involved (UC and AB) received a 1-week session training consisting of calibration for surgical and follow-up procedures. Patient were included in and excluded from the study in accordance to the following criteria:
Inclusion criteria:
• 18 years old or older, and able to sign a written informed consent form;
• patients with cuspid/bicuspid failing tooth in the maxillary/mandibular area
requiring a tooth extraction and immediate dental implant placement, with either an immediate or delayed restoration; patients whose progress had been followed for at least one year.
Exclusion criteria:
• history of systemic diseases which would contraindicate surgical treatment;
• long-term steroidal and/or amino-bisphosphonate therapy;
• diabetes mellitus;
• pregnant or lactating;
ISSN 2307-5295, Published by the POSEIDO Organization & Foundation
under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported
(CC BY-NC-ND 3.0) License.
POSEIDO. 2013;1(3) 167
Post-‐extraction implant: immediate vs delayed restoration
• uncontrolled periodontal disease;
• patients declaring to smoke more than 10 cigarettes per day. Subjects smoking
less than 10 cigarettes per day were requested to stop smoking before and after surgery, even though their compliance could not be monitored;
• absence of adjacent teeth;
• extraction sites with a partial or complete deficiency of buccal bone plate;
• failing tooth with acute infection;
• unwillingness to return for the follow-up examination.
For each patient a financial record including cost for clinical treatment and following
aftercare was compiled: total cost for each treatment was calculated [16].
2.2. Surgical Treatment
After an oral hygiene session each patient received clinical evaluation and tooth
extraction at baseline. When immediate implant could not be inserted a ridge preservation procedure was performed, the patient was excluded from the study.
Blossom Implants with Ossean surface (Intra-lock International, Boca-Raton, FL,
USA) were used [17]. Final insertion torque was measured with a calibrated torque wrench
(Torque-Lock 2, Intralock International, Boca-Raton, FL, USA; torque measurement range
from 20 to 75 Ncm). Implants with an insertion torque of at least 45 Ncm were included in
the group of immediate restoration and were temporary restored within 36 hours from
implant placement; if the insertion torque was lower than 45 Ncm, the implant was included
into the delayed restoration group (with a 4 months provisionalization).
All patients received prophylactic antibiotic therapy (2 g of amoxicillin or 600 mg
clindamycin – if allergic to penicillins) 1 hour before the extraction procedure and continued to take the antibiotic postoperatively (1g amoxicillin or 300 mg clindamycin) three times a day for 4 days. All patients rinsed for 1 minute with 0.2% chlorhexidine mouthwash prior to the surgery (and twice a day for the following 3 weeks), and were treated under local anesthesia using lidocaine with adrenaline 1:50.000. A flapless approach was chosen and tooth extractions were carried out with or without elevators to minimize the trauma; great care was taken to maintain the integrity of the buccal bone wall. Ultrasound bone surgery with specific tips was used at the mesial, distal and lingual/palatal sites to allow easier tooth extraction. After extraction, the socket was carefully curetted and, subsequently, the implant bed was prepared according to the standard procedure (with standard drills following the palatal bony wall as a guide, making maximum use of the bone apical to the removed tooth). A periodontal probe was used to verify the integrity of the bone walls and to evaluate the integrity of buccal bone plate after implant osteotomy preparation. The implants (Intra-lock International, Boca-Raton, FL, USA) were placed with the implant platform at the marginal level of the palatal/lingual bone wall.
Cortico-cancellous porcine bone particles (Apatos, Osteobiol-Tecnoss, Coazze, Italy)
and a resorbable membrane (Evolution, Osteobiol-Tecnoss, Coazze, Italy) were used to graft the peri-implant bone defect. Impressions were taken and temporary/resin restorations were prepared using prefabricated abutments (Intra-lock International, Boca-Raton, FL, USA) within 36 hours for the immediately restored implants. Secondary soft tissue healing was left with a collagen membrane exposed to the oral cavity for the delayed restored implants.
ISSN 2307-5295, Published by the POSEIDO Organization & Foundation
under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported
(CC BY-NC-ND 3.0) License.
168 Research article: Barone A, et al. (2013)
Sutures were removed after 10 days and oral hygiene instructions were given. All
patients underwent appropriate antibiotic and analgesic anti-inflammatory therapy (generally ibuprofen 600 mg tablets).
The final impressions were made with individual trays using polyvinyl siloxane
material (Flexitime, Heraeus/Kulzer, Hanu, Germany) to prepare the metal-ceramic crowns, which were cemented on personally tailored titanium abutments.
From each patient, time spent, clinical and financial records were collected. The mean
real salary per hour was obtained from the European Commission website database
<http://ec.europa.eu/index_en.htm> which cites labor costs per hour 2013 in Italy at €27.4.
The time cost for each patient was calculated by multiplying the time per year spent in the
clinic by the mean real salary per hour. The total costs were the costs cumulated during the
twelve months of survey.
2.3. Input variables
Variables were taken by one examiner who was not involved in performing the
surgical treatment, immediately after implant placement (baseline or time 0, or T0), at 4 months after placement (time 1, or T1) and at 12 months after dental implant insertion (time 2 or T2).
• MBL: peri-implant marginal bone level was evaluated on intra-oral radiographs at the
mesial and distal sites (mMBLX and dMBLX, with X = 0,1,2) and corresponded to the distance between the fixture-abutment interface and the most apical point of the marginal bone level. Digital intra-oral periapical radiographs were taken (70 KVp, 7 mA) using a parallel cone technique with digital sensor (Schick Technologies, Long Island City, NY, USA). A standardization of the x-ray geometry was applied and the known diameter, length or thread-pitch distance of the implants (pitch = 1.0 mm) were used for calibration. Measurements were taken to the nearest mm using computer software (UTHSCSA Image Tool, Version 3.00, University of Texas Health Science, San Antonio, TX).
• WKG: width of keratinized gingiva was the distance between the gingival margin and
the mucogingival junction of the interested area, measured midfacially.
• FST: facial soft tissue level was the distance between a reference line, which
connected the facial soft tissue level of the adjacent teeth, and the soft tissue at midfacial point amid the two residual teeth adjacent interested area.
• BT: buccal bone thickness was evaluated by means of a surgical caliper at the moment
of tooth extraction and represented the thickness of the buccal bone plate at the most coronal point of the marginal crest using a surgical caliper.
• Implant failure: it occurred for any mechanical damaging (fracture) or clinical
detriment (peri-implant infection or mobility) which required implant removal.
Cost of the clinical treatment was calculated taking into account the following steps:
preoperative consultations and diagnostic tests, stage-one surgery, number of visits during the healing phase, stage-two surgery, and the prosthodontics phase of treatment. Additional clinical costs, including costs for clinical and medical services, and those resulting from time spent by the patient for staged recall visits (oral hygiene program, with a recall visit every 6 months) and other visits required by the patients, were also calculated.
ISSN 2307-5295, Published by the POSEIDO Organization & Foundation
under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported
(CC BY-NC-ND 3.0) License.
POSEIDO. 2013;1(3) 169
Post-‐extraction implant: immediate vs delayed restoration
2.4. Outcome variables
The outcome variables were obtained subtracting from each input variable the
respective baseline value: a negative value represented a reduction, whereas a gain was given by a positive value.
• ΔMBL: change at the marginal bone level was calculated for the mesial and distal
aspects at 4 and 12 months as reported by the following formula:
nΔMBLX = nMBL0 − nMBLX, (with n as mesial or distal, and X = 1,2)
• ΔFST: facial soft tissue changes were calculated by subtracting the baseline value from
the respective values at T1 or T2, according to the formula:
ΔFSTX = FSTX − FST0 (with X = 1,2)
• ΔWKG : changes in the width of keratinized gingiva for times T1 or T2, according to
ΔWKGX = WKGX − WKG0 (with X = 1,2)
• IP: the index proposed by Jemt was employed to analyze the status of the interdental
papilla [18]
0 = no papilla; 1 = less than one half papilla is present; 2 = greater than half of the papilla height is present but not to the full extent of
the contact point;
3 = papilla fills the entire proximal space and is in good harmony; 4= papilla is hyperplastic.
• SR and CSR: success rates and respective cumulative value were calculated according
to the criteria suggested by Buser with a registered radiological peri-implant bone
resorption not greater than 1.5 mm, during the first year of loading [19], and 0.2 mm
/ year, during the following years [20].
• Time of clinical treatment calculated from the surgery time to the definitive prosthesis
• Total cost (expressed in labor costs per hour) = Costs for the clinical treatment +
Adjunctive clinical cost.
2.5. Statistical analysis
Acquired data were entered into a database for automatic analysis (Database Toolbox,
MatLab 7.0.1, The MathWorks, Natick, MA). Matrix laboratory tools package were employed to perform descriptive and statistical analysis (Statistics Toolbox, MatLab 7.0.1, The MathWorks, Natick, MA). A Lilliefor test was employed to confirm normal distribution of the data related to each procedure. For each of the outcome variables pairwise comparisons were performed using the Wilcoxon signed rank test for matched samples and the Wilcoxon rank sum test for unmatched data and p-values were obtained. All measurements in the text and tables are described as mean and standard deviation, m±std; for ranked variables the results were given by median and interquartile range (IQR: the difference between the 75th and 25th percentiles). The level of statistical significance was set at .01 for all analyses.
ISSN 2307-5295, Published by the POSEIDO Organization & Foundation
under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported
(CC BY-NC-ND 3.0) License.
170 Research article: Barone A, et al. (2013)
3. Results
Thirty patients were treated with tooth extraction and immediate implant placement.
Immediate prosthetic restoration was performed for 15 patients (age of 44.6±10.2 years
within the range 29-62), whereas delayed restoration (3-4 months) was performed for the
remaining 15 patients (age of 49.1±11.9 years within the range 31-67). Tooth position, age,
gender and patient demographic data were reported in Table 1.
Immediate prosthetic
Delayed prosthetic
Procedure
restoration
restoration
Sample size
Age (years)
Age range (years)
Time of clinical
treatment° (days)
Two years total cost°
Genders ratio M/F
Cuspid/bicuspid ratio
Smoking habit Y/N
Buccal plate
thickness (mm)
Table 1. Demographic data for the two different prosthetic loading with description of
variable data related to measurements, given by median and interquartile range, m
(iqr). For both
procedures, a cuspids/bicuspids (C/B) ratio and the thickness value of the buccal plate before dental implant insertion were given.
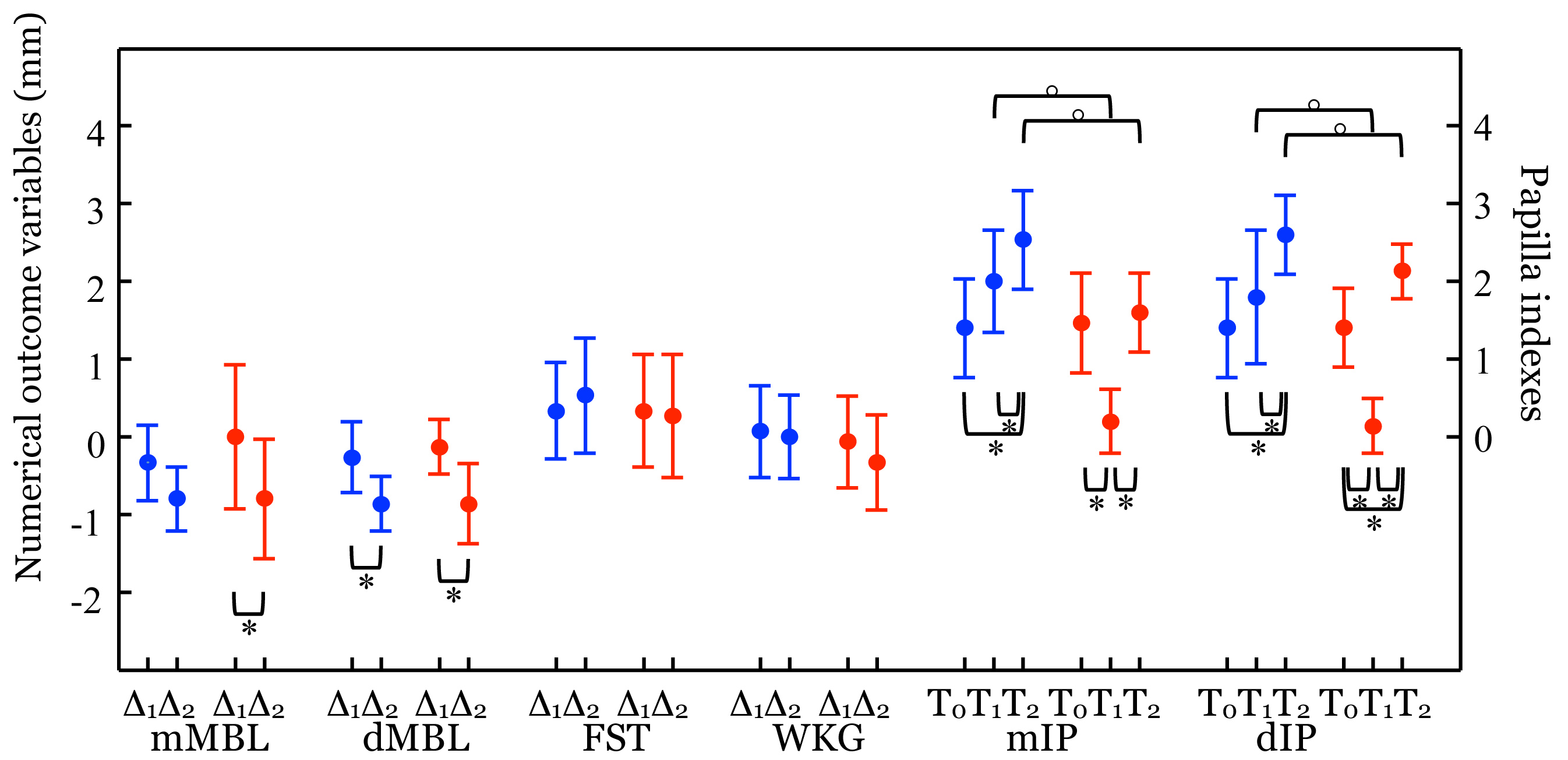
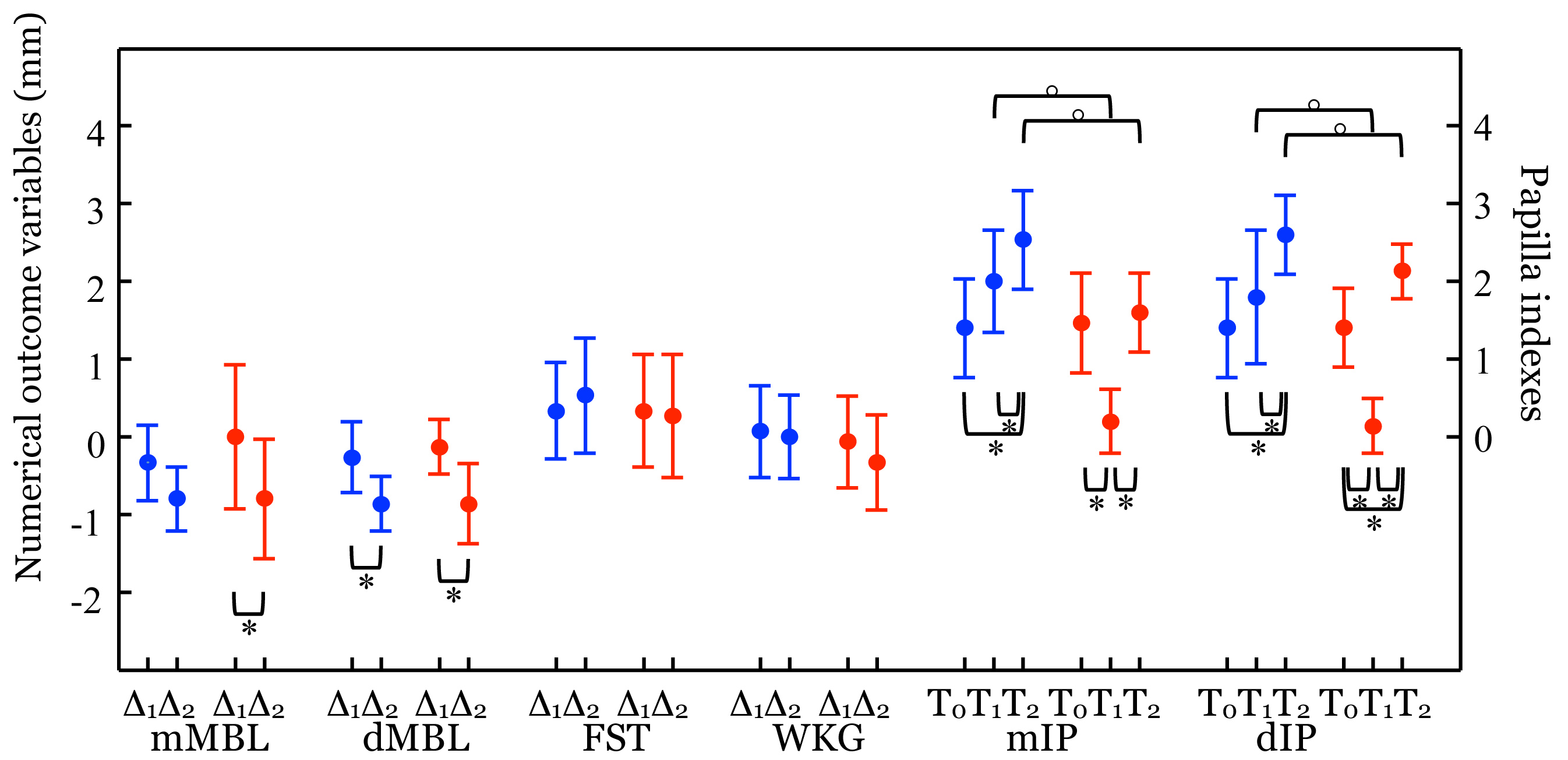
The outcome variables were reported in Table 2 for all the time points considered: T0
was the baseline, T1 and T2 the 4- and 12-month follow-up. Changes of the outcome variables
were calculated giving mesial or distal ΔMBL, ΔFST and ΔWKG between T0 and T1 (marked
as Δ1) and between T0 and T2 (marked as Δ2). The papilla index values for the two procedures
were also showed in Table 2 as median and interquartile range. The dimensional changes of
the hard and soft tissues were visualized in Figure 1. The comparisons between procedures
showed significant differences for the papilla index. The immediate restoration group at 4-
month analysis had 2(0), at 1-year analysis the mean value was 2(1.5). The delayed
restoration group at 4-month analysis had 0(0), at 1-year analysis the mean value was 2(1)
(with significance ranging from .0098 and 2.6⋅10 6−). No significant differences were observed
for changes of facial soft tissue level (ΔFST) and of the width of keratinized gingiva (ΔWKG).
The marginal bone level showed significant differences between the 2 groups. The immediate
restoration group showed significant difference between 4-month (ΔMBL1) and 1 year
analysis (ΔMBL2) only at the distal sites with values of -0.3±0.5 mm and -0.9±0.4 mm,
respectively (p-value = 0.0039). Conversely, the delayed restoration group showed
significant changes between 4-month and 12-month analysis at mesial (p-value = 0,0049)
and distal (p-value = 0,0098) sites.
No dental implant failure was registered during the considered period of time;
moreover, all implants at the final time of the survey were considered successful.
ISSN 2307-5295, Published by the POSEIDO Organization & Foundation
under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported
(CC BY-NC-ND 3.0) License.
POSEIDO. 2013;1(3) 171
Post-‐extraction implant: immediate vs delayed restoration
Procedure
(a) Immediate prosthetic restoration
Values for outcome
p-value Wilcoxon
variables
signed rank test
T0 vs. T1 T0 vs. T2 T1 vs. T2 Δ1 vs. Δ2
±0.8 ±0.5 ±0.4
±0.7 ±0.5 ±0.4
±0.3 ±0.6 ±0.7
±1.1 ±0.6 ±0.5
1(1) 2(1.5) 3(1)
Procedure
(b) Delayed prosthetic restoration
Values for outcome
p-value Wilcoxon
variables
signed rank test
T0 vs. T1 T0 vs. T2 T1 vs. T2 Δ1 vs. Δ2
±0.8 ±0.7 ±0.8 ±0.9 ±0.8
±0.7 ±0.8 ±0.9 ±0.4 ±0.5
±0.8 ±0.9 ±0.5 ±0.7 ±0.8
±0.7 ±0.9 ±0.7 ±0.6 ±0.6
9.8⋅10−
Procedure
(c) Comparison between prosthetic restorations
p-value Wilcoxon rank sum test
Δ1 or at 4 months
Δ2 or at 12 months
mMBL (mm)
dMBL (mm)
Table 2. Overall outcome variables given by mean and standard deviation, ± std for
continue variables and by median and interquartile range, m (iqr) for ranked variables
for both procedures and overall times: baseline (T0), at 4 (T1) and 12 (T2) after implant placement.
Differential value (Δ) at 4 (Δ1) and 12 months (Δ2) are also given. Costs were given in time (total cost /
labor cost per hour) and the significances of the Wilcoxon two-sided signed rank test for matched
samples and of the Wilcoxon rank sum test for unmatched samples (type of provisionalization) for
overall outcome variables were shown in bold.
ISSN 2307-5295, Published by the POSEIDO Organization & Foundation
under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported
(CC BY-NC-ND 3.0) License.
172 Research article: Barone A, et al. (2013)
Figure 1. Summary of the overall outcome variables, showed as mean and standard
deviation for all the times: immediate loading was represented in blue, whereas delayed loading
was showed in red. For the pairwise comparisons by the Wilcoxon two-sided rank sum test for
independent samples (°) and the Wilcoxon signed rank test for matched data (*), significant p-values
are shown as brackets (upper and lower, respectively). For the papilla index were given at baseline
(T0), at 4 (T1) and 12 months (T2) after implant placement, and for differential value (Δ) of the
remaining outcome variables at 4 (Δ1) and 12 months (Δ2).
The mean values for the operating times for the clinical treatments of the two groups
were 120 days and 203 days, for immediate and delayed restorations, with a statistically
significant (p = 3.32⋅10 6−) difference. A difference at a significant level was also obtained
between the medians of the two groups regarding the total costs at year 1 of the survey (141.9
days and 179.0 days for immediate and delayed prosthetic procedures, with p = 2.39⋅10 6−)
(Table 2).
4. Discussion
In this cohort study, implant survival, peri-implant mucosal changes, marginal bone
loss and treatment cost of immediate and delayed restorations of immediate single implants were evaluated and compared. The data were collected after 1 year of function and the two groups were homogeneous, showing similar baseline parameters.
All the implants placed in fresh extraction sockets survived up to one year of function,
and no technical or biological complications were recorded. The overall success rate of the immediate implants was 100%, due to the favorable marginal bone changes. The two experimental groups produced similar outcomes also in soft tissue integration. The results of this study showed that immediate restorations of immediate implants are at least as effective and safe as delayed restorations.
ISSN 2307-5295, Published by the POSEIDO Organization & Foundation
under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported
(CC BY-NC-ND 3.0) License.
POSEIDO. 2013;1(3) 173
Post-‐extraction implant: immediate vs delayed restoration
In a recent literature review [21], the authors calculated the overall survival rate of
both immediately and delayed restored dental implants, but no conclusive results were obtained. Despite other authors' findings, the present study registered no significant buccal soft tissue recession in the delayed restoration group.
Several factors should be taken into consideration to explain this discrepancy. First of
all, the extraction sockets included in the experimental groups presented intact buccal bone plate, adequate soft and hard tissues dimensions and no acute infection. Also, the allocation to the immediate or delayed restoration was guided by the insertion torque value (cut-off value 45 Ncm), excluding a randomization process. Furthermore, an augmentation of the bone contour was performed at all the experimental sites, in order to control the ridge remodeling after tooth extraction. All these surgical steps contributed in managing the risk of the procedure and improving the survival rates and the esthetic results.
All soft tissues outcomes showed no significant differences between the two
experimental groups, except for the papilla index. The mesial and distal marginal bone level in the delayed restoration group registered a statistically significant decrease between the 4 months and the 1-year control. The mesial aspect (mMBL) was 0.5 ± 0.9 mm at 4 months and 0.1 ± 0.8 mm at 1 year, the distal aspect (dMBL) was 0.7 ± 0.7 at 4 months and 0.1 ± 0.7 at 1 year. These findings pointed out that the marginal bone loss started at the same time with the delayed restoration. On the other hand, in the immediate restoration group, the bone loss followed a gradual progression, thus resulting in a final value similar to the delayed group.
In a recent review, Lang et al. [9] analyzed immediate implant placement studies
comparing immediate and conventional loading. The review pointed out that, during the first year of immediate loading, the bone loss is less than 1 mm, while longer-term studies showed a stabilization of the bone level after the first year. On the other hand, a bone loss of 0.05 – 1.16 mm was described in the delayed restoration group, where the baseline measurement was at the time of implant placement.
The soft tissue changes showed similar results in both the immediate and the delayed
group. The buccal mucosal margin (ΔFST) and the width of attached mucosa (ΔWKG) changes were registered at baseline and at final time. The baseline facial soft tissue level was positively correlated to the buccal bone thickness, confirming that a buccal plate > 0.5 mm could improve the buccal soft tissues stability, at least in the delayed group. Nevertheless, both procedures showed a small number of patients presenting a slight soft tissue recession in both groups and the final results were similar for the immediate and delayed procedure. The difference between the two groups was connected to the time of the soft tissue remodeling, since in the immediate restoration it started immediately after the surgery, while in the delayed group it started at the time of restoration.
Among the soft tissues values, the papilla index (PI) showed the greatest differences
between the two groups. Previous studies observed wider papilla shrinkage in delayed
restored implants when compared to immediate provisional restoration procedure. In this
study, the difference between the PIs of the two protocols was statistically significant at 4
months. As other authors assessed, most of the papilla shrinkage showed up in the delayed
restoration at three months, but after this period a progressive re-growth of the mesial and
distal tissue was observed [9]. After 1 year, the two PIs were comparable. Moreover the
replacement of single tooth seemed to lead to a final positive dimensional change after tooth
extraction when compared to the baseline values (median PI = 1) that were registered for
impaired teeth.
ISSN 2307-5295, Published by the POSEIDO Organization & Foundation
under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported
(CC BY-NC-ND 3.0) License.
174 Research article: Barone A, et al. (2013)
Results published in the literature seem to confirm that the most of the hard and soft
tissue changes were focused within the first six months following immediate implant
placement; afterwards the papillae regardless of the restoration procedure, both at mesial
and distal aspects, may undergo a positive remodeling phenomenon leading to a gain in
height attested by analysis both of the linear height measurements and of the distribution of
papilla scores [9].
The re-growth of the papillae was observed in both groups and reached the original
heights. However, adopting an immediate restoration protocol could ensure more predictable soft and hard tissues outcomes. In fact, in the delayed group the soft tissue changes were evident and seemed to follow a loss and restoration process, while in the immediate group the modifications were minimal and slow until a steady state was reached. An immediate provisionalization can improve the patient's compliance and reduce the overall healing time, as found in this paper.
Other Authors compared different strategies to treat partially and totally edentulous
patients, reporting long-term costs [22-26]. The results of these studies were not
comparable with the present work. In the present study, the delayed restoration protocol
resulted to be about 26% more expensive due to the adjunctive stage-two surgery and visits
required.
One limit of this study could be the treatment selection, which was assigned to the
clinician, avoiding a randomization system. Beside this, the differences between the two experimental groups could be so clearly shown because of the absence of a blinded type of measurement. The results of this paper need to be confirmed by a longer period of observation and a larger number of implants studies.
5. Conclusion
Immediate implant's prosthetic restoration could be realized immediately after the
implant surgery or after the bone healing period. Both of the protocols showed similar final results regarding the negative bone remodeling, but different timing since in the delayed group the bone resorption was between 4 months and 1 year, while in the immediate group it was slow and gradual during all the follow-up time. No differences were pointed out in the midfacial gingival margin and the width of keratinized gingiva. In the delayed restoration group a loss and regain of the papillae was observed, while slight modifications were recorded in the immediately restored implants until a complete healing. Regarding the healing time and costs of the two procedures, immediate restoration appeared to be a more promising procedure for implant placed in fresh extraction sockets.
Disclosure of interests
The authors have no conflict of interest to report.
References
Gotfredsen K. A 5-year prospective study of single-tooth replacements supported by the Astra Tech
implant: a pilot study. Clin Implant Dent Relat Res. 2004;6(1):1-8.
[2]
Cordaro L, Torsello F, Roccuzzo M. Clinical outcome of submerged vs. non-submerged implants placed
in fresh extraction sockets. Clin Oral Implants Res. 2009;20(12):1307-13.
[3]
Covani U, Chiappe G, Bosco M, Orlando B, Quaranta A, Barone A. A 10-year evaluation of implants
placed in fresh extraction sockets: a prospective cohort study. J Periodontol. 2012;83(10):1226-34.
ISSN 2307-5295, Published by the POSEIDO Organization & Foundation
under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported
(CC BY-NC-ND 3.0) License.
POSEIDO. 2013;1(3) 175
Post-‐extraction implant: immediate vs delayed restoration
Chen ST, Buser D. Clinical and esthetic outcomes of implants placed in postextraction sites. Int J Oral
Maxillofac Implants. 2009;24(Suppl):186-217.
[5]
Fickl S, Zuhr O, Wachtel H, Bolz W, Huerzeler M. Tissue alterations after tooth extraction with and
without surgical trauma: a volumetric study in the beagle dog. J Clin Periodontol. 2008;35(4):356-63.
[6]
Covani U, Barone A, Cornelini R, Crespi R. Soft tissue healing around implants placed immediately
after tooth extraction without incision: a clinical report. Int J Oral Maxillofac Implants. 2004;19(4):549-53.
[7]
Covani U, Crespi R, Cornelini R, Barone A. Immediate implants supporting single crown restoration: a
4-year prospective study. J Periodontol. 2004;75(7):982-8.
[8]
Covani U, Bortolaia C, Barone A, Sbordone L. Bucco-lingual crestal bone changes after immediate and
delayed implant placement. J Periodontol. 2004;75(12):1605-12.
[9]
Lang NP, Pun L, Lau KY, Li KY, Wong MC. A systematic review on survival and success rates of
implants placed immediately into fresh extraction sockets after at least 1 year. Clin Oral Implants Res.
2012;23(Suppl 5):39-66.
[10]
Barone A, Ricci M, Calvo-Guirado JL, Covani U. Bone remodelling after regenerative procedures
around implants placed in fresh extraction sockets: an experimental study in Beagle dogs. Clin Oral Implants
Res. 2011;22(10):1131-7.
[11]
Covani U, Barone A, Cornelini R, Crespi R. Clinical outcome of implants placed immediately after
implant removal. J Periodontol. 2006;77(4):722-7.
[12]
De Rouck T, Collys K, Cosyn J. Single-tooth replacement in the anterior maxilla by means of immediate
implantation and provisionalization: a review. Int J Oral Maxillofac Implants. 2008;23(5):897-904.
[13]
den Hartog L, Slater JJ, Vissink A, Meijer HJ, Raghoebar GM. Treatment outcome of immediate, early
and conventional single-tooth implants in the aesthetic zone: a systematic review to survival, bone level, soft-
tissue, aesthetics and patient satisfaction. J Clin Periodontol. 2008;35(12):1073-86.
[14]
Jacobson J, Maxson B, Mays K, Peebles J, Kowalski C. Cost-effectiveness of dental implants: a utility
analysis. J Dent Educ. 1990;54(11):688-9.
[15]
Jonsson B, Karlsson G. Cost-benefit evaluation of dental implants. Int J Technol Assess Health
Care. 1990;6(4):545-57.
[16]
Attard N, Wei X, Laporte A, Zarb GA, Ungar WJ. A cost minimization analysis of implant treatment in
mandibular edentulous patients. Int J Prosthodont. 2003;16(3):271-6.
[17]
Freitas AC, Jr., Bonfante EA, Giro G, Janal MN, Coelho PG. The effect of implant design on insertion
torque and immediate micromotion. Clin Oral Implants Res. 2012;23(1):113-8.
[18]
Jemt T. Regeneration of gingival papillae after single-implant treatment. Int J Periodontics
Restorative Dent. 1997;17(4):326-33.
[19]
Buser D, Weber HP, Lang NP. Tissue integration of non-submerged implants. 1-year results of a
prospective study with 100 ITI hollow-cylinder and hollow-screw implants. Clin Oral Implants Res.
1990;1(1):33-40.
[20]
Malchiodi L, Ghensi P, Cucchi A, Corrocher G. A comparative retrospective study of immediately loaded
implants in postextraction sites versus healed sites: results after 6 to 7 years in the maxilla. Int J Oral
Maxillofac Implants. 2011;26(2):373-84.
[21]
Del Fabbro M, Ceresoli V, Taschieri S, Ceci C, Testori T. Immediate Loading of Postextraction Implants
in the Esthetic Area: Systematic Review of the Literature. Clin Implant Dent Relat Res. 2013;In Press.
[22]
Takanashi Y, Penrod JR, Lund JP, Feine JS. A cost comparison of mandibular two-implant overdenture
and conventional denture treatment. Int J Prosthodont. 2004;17(2):181-6.
[23]
Attard NJ, Zarb GA, Laporte A. Long-term treatment costs associated with implant-supported
mandibular prostheses in edentulous patients. Int J Prosthodont. 2005;18(2):117-23.
[24]
Stoker GT, Wismeijer D, van Waas MA. An eight-year follow-up to a randomized clinical trial of
aftercare and cost-analysis with three types of mandibular implant-retained overdentures. J Dent Res.
2007;86(3):276-80.
[25]
Bouchard P, Renouard F, Bourgeois D, Fromentin O, Jeanneret MH, Beresniak A. Cost-effectiveness
modeling of dental implant vs. bridge. Clin Oral Implants Res. 2009;20(6):583-7.
[26]
Bragger U, Krenander P, Lang NP. Economic aspects of single-tooth replacement. Clin Oral Implants
Res. 2005;16(3):335-41.
This article can be cited as:
Barone A, Borgia V, Alfonsi F, Toti P, Covani U. Immediate versus delayed restorations for implants
placed in fresh extraction sockets: a 1-year comparative cohort study. POSEIDO. 2013;1(3):165-75.
ISSN 2307-5295, Published by the POSEIDO Organization & Foundation
under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported
(CC BY-NC-ND 3.0) License.
Source: http://www.poseido.info/publication/volume-1-2013/poseido-201313165-75-barone.pdf
april 2014_Layout 1 3/26/14 10:49 AM Page 1 Publication of New Jersey Carpenters Funds cobra rates revised nj carpenters annuity for active members fund achieves powerful COBRA provides continued health care coverage at group rates to 13 percent return in 2013 eligible employees and family members who have lost coverage due to certain qualifying events or reasons "other than gross misconduct." The
GUIDELINES FOR BERMUDA2011 GOVERNMENT OF BERMUDAMinistry of HealthDepartment of Health HYPERTENSION GUIDELINES FOR BERMUDA Government of Bermuda Ministry of Health Department of Health P.O. Box HM 1195, Hamilton HM EX Bermuda Hypertension Task Group Hypertension Task Group (2011) Hypertension Guidelines for Bermuda