Microsoft word - pediatric 6-.doc
PEDIATRIC PROTOCOLS
EMS and Children with Special Healthcare Needs.6-3
AIRWAY / BREATHING PROTOCOLS
Pediatric Airway.6-5 Pediatric Foreign Body Airway Obstruction (FBAO) .6-7 Pediatric Respiratory Distress – Upper Airway .6-9 Pediatric Respiratory Distress – Lower Airway .6-11
ARRYTHMIAS / ACLS
Pediatric Sinus Bradycardia.6-13 Pediatric Narrow Complex Tachycardia (SVT) .6-15
CARDIAC ARREST / ACLS
Pediatric Asystole / Pulseless Electrical Activity (PEA) . 6-17 Pediatric Ventricular Fibrillation (V-FIB) and Pulseless Ventricular Tachycardia . 6-19
MEDICAL PROTOCOLS
Pediatric Altered Level of Consciousness . 6-21 Pediatric Diabetic Emergencies. 6-23 Pediatric Heat Illness. 6-25 Pediatric Hypothermia . 6-27 Pediatric Neonatal Resuscitation. 6-29
APGAR Scoring Chart . 6-30
Pediatric Esophageal Foreign Body . 6-31 Pediatric Seizure . 6-33 Pediatric Shock – Non Trauma. 6-35 Pediatric Toxic Ingestion / Exposure . 6-37 Pediatric Trauma .
Head. 6-39 Multiple . 6-41
PEDIATRIC ASSESSMENT CHARTS
Glascow Coma Scale . 6-43
Normal Vital Signs .
Pediatric Pharmacology Review . 6-45
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
THIS PAGE INTENTIONALLY LEFT BLANK
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
MEDICAL PROTOCOLS
PEDIATRIC
EMERGENCIES IN CHILDREN WITH SPECIAL HEALTCHCARE NEEDS
GENERAL CONSIDERATIONS
1. Treat the ABC's first. Treat the child, not the equipment. If the emergency is due to an equipment
malfunction, manage the child appropriately using your own equipment.
cared for in hospitals or chronic care facilities are often cared for in homes by
parents or other caretakers. These children may have self-limiting or chronic diseases. There are multitudes of underlying medical conditions that may categorize children as having special needs. Many are often unstable and may frequently involve the EMS system for evaluation, stabilization, and transport. Special needs children include technology-assisted children such as those with tracheostomy tubes with or without assisted ventilation, children with gastrostomy tubes, and children with indwelling central lines. The most serious complications are related to tracheostomy problems.
3. Children with Special Healthcare Needs (CSHCN) have many allergies. Children with spina bifida are
often allergic to latex. Before treating a patient, ask the caregivers if the children are allergic to latex or have any other allergies. Stock latex-free equipment. (Some regularly used equipment that contains latex includes gloves, oxygen masks, IV tubing BVM, blood pressure cuff, IV catheters, etc.)
4. Knowing which children in a given area have special needs and keeping a logbook is encouraged.
5. Parents and caretakers are usually trained in emergency management and can be of assistance to
EMS personnel. Listen carefully to the caregiver and follow his/her guidance regarding the child's treatment.
6. Children with chronic illnesses often have different physical development from well children.
Therefore, their baseline vital signs may differ from normal standards. The size and developmental level may be different from age-based norms and length based tapes used to calculate drug dosages. Ask the caregiver if the child normally has abnormal vital signs. (i.e. a fast heart rate or a low pulse oximeter reading)
7. Some CSHCN may have sensory deficits (i.e. they may be hearing impaired or blind) yet may have
age-appropriate cognitive abilities. Follow the caregivers' lead in talking to and comforting a child during treatment and transport. Do not assume that a CSHCN is developmentally delayed.
8. When moving a special needs child, a slow careful transfer with two or more people is preferable. Do
not try to straighten or unnecessarily manipulate contracted extremities as it may cause injury or pain to the child. Certain medical conditions will require special care. Again, consult the child's caregiver.
9. Caregivers of CSHCN often carry "go bags" or diaper bags that contain supplies to use with the
child's medical technologies and additional equipment such as extra tracheostomy tubes, adapters for feeding tubes, suction catheters, etc. Before leaving the scene, ask the caregivers if they have a "go bag" and carry it with you.
10. Caregivers may also carry a brief medical information form or card. The child may be enrolled in a
medical alert program whereby emergency personnel can get quick access to the child's medical history. Ask the caregivers if they have an emergency information form or some other form of medical information for their child.
11. Caregivers of CSHCN often prefer that their child be transported to the hospital where the child is
regularly followed or the "home" hospital. When making the decision as to where to transport a CSHCN, take into account: local protocols, the child's condition, capabilities of the local hospital, caregivers' request, ability to transport to certain locations.
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
THIS PAGE INTENTIONALLY LEFT BLANK
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
AIRWAY / BREATHING
PEDIATRIC
MED CONTROL
Respiratory Rate, Effort,
Basic maneuvers first ---
Respirations Obstruction
Nasal / Oral Airway
Positive Gag Reflex
See Pediatric Foreign
Body Airway Obstruction
Direct Laryngoscopy
Continue Bag – Valve –
Mask Ventilations
KEY POINTS
•
Capnometry is mandatory with all methods of intubation. Document results of SPO2.
•
Limit intubation attempts to 3 per patient.
• If unable to intubate, continue BVM ventilations, transport rapidly, and
notify receiving hospital early
• Maintain C-spine immobilization for patients with suspected spinal injury.
• Do not assume hyperventilation is psychogenic -- use oxygen, not a paper bag.
• Sellick's maneuver should be used to assist with difficult intubations.
• Continuous pulse oximetry should be utilized in all patients with an inadequate respiratory function.
• Consider c-collar to help maintain ETT placement for all intubated patients .
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
THIS PAGE INTENTIONALLY LEFT BLANK
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
AIRWAY / BREATHING
PEDIATRIC
FOREIGN BODY AIRWAY OBSTRUCTION (FBAO)
Infant (0 – 12 months)
Head Tilt / Chin Lift/ Jaw Thrust / Airway Maneuvers
MED CONTROL
Complete Obstruction
Complete Obstruction
Encourage patient to cough
5 Back Blows / 5 Chest thrusts
(Only if visualized / attainable)
10 – 15 L Pediatric Mask,
Laryngoscope/ Magill Forceps
Open airway / ventilate
(May reposition repeat)
5 Back Blows / 5 Chest thrusts
If unable to ventilate,
repeat / continue sequence
Child (1 – 8 years)
Head Tilt / Chin Lift/ Jaw Thrust / Airway Maneuvers
Complete Obstruction
Complete Obstruction
Encourage patient to cough
(Only if visualized / attainable)
10 – 15 L Pediatric Mask,
Laryngoscope/ Magill Forceps
Open airway / ventilate
(May reposition repeat)
5 Abdominal Thrusts
If unable to ventilate,
CONTACT MEDICAL CONTROL
repeat / continue sequence
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
AIRWAY / BREATHING
PEDIATRIC
FOREIGN BODY AIRWAY OBSTRUCTION (FBAO)
SIGNS AND SYMPTOMS
DIFFERENTIAL DIAGNOSIS
• Sudden Episode of Choking
• Inablity to speak
• Audible Stridor
• Unresponsive
• Change in Skin Color
• Increased / Decreased
Respiratory Rate
• Unproductive
KEY POINTS
• Infants 0-12 months DO NOT receive abdominal thrusts. Use chest thrusts.
• NEVER perform blind finger sweeps in infants or children.
• Attempt to clear the airway should only be made if foreign body aspiration is witnessed or very strongly
suspected and there is complete airway obstruction.
• Even with a complete airway obstruction, positive-pressure ventilation is often successful.
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
AIRWAY / BREATHING
PEDIATRIC
Respiratory Distress Upper Airway – CROUP
UNIVERSAL PATIENT CARE PROTOCOL
MED CONTROL
Sit Patient on Parent's Lap
Position Patient Sitting Upright
Do not Lay Patient Down
Do Not Perform Digital Airway Exam
Check Pulse Oximetry
Mild – Moderate Distress
Severe Distress
Evaluate Level of Distress / Pulse Oximetry
Cool Mist with Sterile Water
SPO2 = 97% with retraction
Accessory Muscle Use
With Severe Respiratory Distress
RACEPHINEPHRINE INHALATION
0.5 mL Diluted to 3mL Sterile NS
Nebulized @ 6 L O2
over 15 minutes x1 treatment
DO NOT USE RACEPHINEPHRINE INHALATION
If color is pink or darker than slightly yellow/
temperature > 68 degrees Fahrenheit
EPINEPHRINE 1:1000 (Undiluted Dose)
(Pediatric < 10 kg = 3 mL , Nebulized @ 6 L Oxygen)
(Pediatric > 10 kg = 5 mL, Nebulized @ 6 L Oxygen)
CONTACT MEDICAL CONTROL
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
PEDIATRIC
Respiratory Distress Upper Airway - CROUP
SIGNS AND SYMPTOMS
• Time of onset
• Possibility of foreign body
• Fever or respiratory
• Inability to Swallow
• Congenital heart disease
• History of trauma
• Medication or Toxin
KEY POINTS
•
Exam: Mental Status, HEENT, Skin, Neck, Heart, Lungs, Abdomen, Extremities, Neuro
• Do not force a child into a position. They will protect their airway by their body position.
• The most important component of respiratory distress is airway control.
• Croup typically affects children < 2 years of age. It is viral, possible fever, gradual onset, no drooling is
• Epiglottitis typically affects children > 2 years of age. It is bacterial, with fever, rapid onset, possible stridor,
patient wants to sit up to keep airway open, and drooling is common. Airway manipulation may worsen the condition.
• DO NOT attempt an invasive airway procedures unless the patient is in respiratory arrest.
• Stridor, gagging or choking in the breathing patient with respiratory distress may indicate upper airway
• Wheezing in the breathing patient with respiratory distress indicates lower airway disease, which may
come from a variety of causes. The patient with severe lower airway disease may have altered LOC, be unable to talk, may have absent or markedly decreased breath sounds and severe retractions with accessory muscle use.
• If the patient has signs of respiratory failure, begin to assist ventilations with BVM, even when they are
• Epiglottis should be considered if the patient has drooling, stridor, and is unable to speak or cry. DO NOT
attempt invasive procedures on the conscious patient who is suspected to have epiglottis.
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
PEDIATRIC
RESPIRATORY DISTRESS LOWER AIRWAY
UNIVERSAL PATIENT CARE PROTOCOL
MED CONTROL
Respiratory Insufficiency
Pediatric Airway Protocol
Position to Patient
Attempt if severe
CONTACT MEDICAL CONTROL
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
MEDICAL PROTOCOLS
PEDIATRIC
RESPIRATORY DISTRESS - LOWER AIRWAY
SIGNS AND SYMPTOMS
• Time of onset
• Possibility of foreign body
• Increased heart rate
• Fever or respiratory
• Epiglottitis
• History of trauma
• Congenital heart disease
• Medication or Toxin
KEY POINTS
•
Exam: Mental Status, HEENT, Skin, Neck, Heart, Lungs, Abdomen, Extremities, Neuro
• Do not force a child into a position. They will protect their airway by their body position.
• The most important component of respiratory distress is airway control.
• DO NOT attempt an invasive airway procedures unless the patient is in respiratory arrest.
• For some patients in severe respiratory distress, wheezing may not be heard. Consider Albuterol for the
known asthmatic in severe respiratory distress.
• Stridor, gagging or choking in the breathing patient with respiratory distress may indicate upper airway
• Wheezing in the breathing patient with respiratory distress indicates lower airway disease, which may
come from a variety of causes. The patient with severe lower airway disease may have altered LOC, be unable to talk, may have absent or markedly decreased breath sounds and severe retractions with accessory muscle use.
• If the patient has signs of respiratory failure, begin to assist ventilations with BVM, even when they are
• Contact Medical Direction for patients with a cardiac history.
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
ARRYTHMIAS / ACLS
PEDIATRIC
SINUS BRADYCARDIA
MED CONTROL
UNIVERSAL PATIENT
Pediatric Airway Protocol
Respiratory Insufficiency
Heart Rate < 60
Monitor and Reassess
0.01 mg/kg IV/IO
1:10000 Solution
Repeat every 3- 5 minutes
0.02 mg/kg IV/IO
repeat every 3-5 minutes
Consider External
Pulseless Arrest Protocol
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
ARRYTHMIAS / ACLS
PEDIATRIC
SINUS BRADYCARDIA
SIGNS AND SYMPTOMS
DIFFERENTIAL DIAGNOSIS
• Foreign body exposure
• Decreased heart rate
• Delayed capillary refill or
• Foreign body / secretions
• Croup / Epigolotitis
• Possible toxic or poison
• Hypotension or arrest
• Infection / Sepsis
• Medication or Toxin
• Medication (maternal or
• Hypoglycemia
• Short of Breath
KEY POINTS
• Exam: Mental Status, HEENT, Skin, Heart, Lungs, Abdomen, Back, Extremities, Neuro
• Heart Rate < 100 (Neonates)
• Heart Rate < 80 (Infants)
• Heart Rate <60 (Children > 2 years)
• Infant = < 1 year of age
• Most maternal medications pass through breast milk to the infant.
• The majority of pediatric arrests are due to airway problems.
• Hypoglycemia, severe dehydration and narcotic effects may produce bradycardia.
• Pediatric patients requiring external transcutaneous pacing require the use of pads appropriate for
pediatric patients per the manufacturers guidelines.
• Identify and treat possible causes for pediatric bradycardia:
1. Hypoxia 2. Hypothermia 3. Head
ingestion/exposure
• Refer to Broselow Pediatric Tape when unsure about patient weight, age and/or drug dosage.
• The minimum dose of Atropine that should be administered to a pediatric patient is 0.1 mg/kg.
• If the rhythm changes, follow the appropriate protocol.
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
ARRYTHMIAS / ACLS
PEDIATRIC
NARROW – COMPLEX TACHYCARDIA
UNIVERSAL PATIENT CARE PROTOCOL
MED CONTROL
Continuous Cardiac Monitor
Attempt to Identify Cause
Heart Rate > 240 infant
Heart Rate >180 child
May attempt Vagal Maneuvers
May go directly to Cardioversion
0.1 mg/kg IV, flush
0.2 mg/kg slow IV/IO
2 mg. IV or Atomizer
0.2 mg/kg IV, flush
Repeat SYNCHRONIZED
(1.0 – 2.0 J/kg)
Repeat SYNCHRONIZED
(1.0 – 2.0 J/kg)
CONTACT MEDICAL CONTROL
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
ARRYTHMIAS / ACLS
PEDIATRIC
NARROW – COMPLEX TACHYCARDIA
SIGNS AND SYMPTOMS
DIFFERENTIAL DIAGNOSIS
• HR: Child > 180/bpm
• Heart disease (Congenital)
• Medications or Toxic
Infant > 240/bpm
• Hypo / Hyperthermia
Ingestion (Aminophylline,
• Pale or Cyanosis
• Hypovolemia or Anemia
Diet pills, Thyroid
• Anxiety / Pain / Emotional
Decongestants, Digoxin)
• Fever / Infection / Sepsis
• Congenital Heart Disease
• Hypoglycemia
• Syncope or Near Syncope
• Medication / Toxin / Drugs
KEY POINTS
•
Exam: Mental Status, Skin, Neck, Lung, Heart, Abdomen, Back, Extremities, Neuro
• Carefully evaluate the rhythm to distinguish Sinus Tachycardia, Supraventricular Tachycardia, and
Ventricular Tachycardia
• Separating the child from the caregiver may worsen the child's clinical condition.
• Pediatric paddles should be used in children < 10 kg or Broselow Tape color Purple
• Monitor for respiratory depression and hypotension associated if Diazepam is used.
• Continuous pulse oximetry is required for all SVT Patients if available.
• Document all rhythm changes with monitor strips and obtain monitor strips with each therapeutic
• Possible causes of tachycardia; hypoxia, hypovolemia, fear, and pain.
• A complete medical history must be obtained.
• Do not delay cardioversion to gain vascular access for the unstable patient.
• If you are unable to get the monitor to select low enough joules, then rapid transport to the nearest
appropriate facility is indicated.
• If the patient is stable, do not cardiovert.
• Record 3-Lead EKG strips during adenosine administration.
• Perform a 12-Lead EKG prior to and after Adenosine conversion or cardioversion of SVT.
• If the rhythm changes, follow the appropriate protocol.
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
CARDIAC ARREST / ACLS
PEDIATRIC
ASYSTOLE / PULSELESS ELECTRICAL ACTIVITY (PEA)
MED CONTROL
UNIVERSAL PATIENT CARE PROTOCOL
See Pediatric Airway Protocol
Apply Cardiac Monitor
Identify Possible
Confirm Asystole
Confirm Asystole / PEA
IV PROTOCOL / IO Procedure
0.01 mg/kg IV/IO
1:10000 Solution
Repeat every 3- 5 minutes
NORMAL SALINE IV, BOLUS
Repeat as needed
Blood Glucose Analysis
CONTACT MEDICAL CONTROL
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
CARDIAC ARREST / ACLS
PEDIATRIC
ASYSTOLE / PULSELESS ELECTRICAL ACTIVITY (PEA)
SIGNS AND SYMPTOMS
DIFFERENTIAL DIAGNOSIS
• Time of arrest
•
Ventricular Fibrillation
• Apneic or Agonal
•
Pulseless Ventricular
Tachycardia
• Possibility of foreign body
CONSIDER TREATABLE CAUSES
• Cardiac Tamponade
• Tension Pnuemothorax
• Pulmonary Embolism
• Tricyclic Overdose
• Drug Overdose
• Hypoglycemia
• Hyperkalemia
KEY POINTS
•
Exam: Mental Status
• Always confirm asystole in more than one lead.
• Cardiac arrest in children is primarily due to lack of an adequate airway, resulting in hypoxia
• If the patient converts to another rhythm or has a return of circulation, refer to the appropriate protocol
and treat accordingly.
• When assessing for a pulse palpate the brachial or femoral arteries for infants and the carotid or femoral
artery for children.
• Continue BLS procedures throughout the resuscitation.
• If the patient is intubated, be sure to routinely reassess tube placement.
• If the patient has an IO, routinely reassess for patency.
• When there is an established ETT, DO NOT delay administration of medications for IV/IO attempts.
Administer the appropriate medications down the tube.
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
CARDIAC ARREST / ACLS
PEDIATRIC
VENTRICULAR FIBRILLATION (V-FIB)
PULSELESS VENTRICULAR TACHYCARDIA
UNIVERSAL PATIENT CARE PROTOCOL
MED CONTROL
CPR X 5 cycles / 2 minutes
Apply Cardiac Monitor / AED
Pulseless V-Tach
Defibrillate 2 J/kg
See Pediatric Airway Protocol
CPR X 5 cycles / 2 minutes
0.01 mg/kg IV/IO
1:10000 Solution
Repeat every 3- 5 minutes
CPR X 5 cycles / 2 minutes
Defibrillate 4 J/kg
Give Antiarrhythmic during CPR
25 – 50 mg/kg IV
CPR X 5 cycles / 2 minutes
Defibrillate 4 J/kg
CONTACT MEDICAL CONTROL
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
PEDIATRIC
VENTRICULAR FIBRILLATION (V-FIB)
PULSELESS VENTRICULAR TACHYCARDIA
SIGNS AND SYMPTOMS
DIFFERENTIAL DIAGNOSIS
• Time of arrest
• Unresponsive
• Possibility of foreign body
• Congenital heart disease
• Toxin or medication
• Hypoglycemia
KEY POINTS
•
Exam: Mental Status
• Monophasic and Biphasic waveform defibrillators should use the same energy levels noted.
• In order to be successful in pediatric arrests, a cause must be identified and corrected.
• Airway is the most important intervention. This should be accomplished immediately. Patient survival is
often dependent on airway management success.
• If the patient converts to another rhythm, follow the appropriate protocol and treat accordingly.
• If the patient converts back to ventricular fibrillation or pulseless ventricular tachycardia, defibrillate at the
previously used setting.
• Defibrillation is the definitive therapy for ventricular fibrillation and pulseless ventricular tachycardia.
• Defibrillate 30-60 seconds after each medication administration.
• The proper administration sequence is shock, drug, shock, and drug.
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
MEDICAL PROTOCOLS
PEDIATRIC
ALTERED LEVEL OF CONSCIOUSNESS
MED CONTROL
UNIVERSAL PATIENT CARE PROTOCOL
See Pediatric Airway Protocol
Spinal Immobilization Protocol
Blood Glucose Analysis
Glucose < 60
(Signs of Dehydration)
Check for Hypotension,
(If Alert with no IV Access
Tachcardia, Poor Cap Refill
and no airway compromise)
NORMAL SALINE IV,
(If no IV Access)
Maximum 1 mg
CONTACT MEDICAL CONTROL
Monitor and Reassess
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
MEDICAL PROTOCOLS
PEDIATRIC
ALTERED LEVEL OF CONSCIOUSNESS
SIGNS AND SYMPTOMS
DIFFERENTIAL DIAGNOSIS
• Known diabetic, medic
• Unresponsive
• Drugs, drug paraphernalia
• Inadequate Respirations
seizure, infection)
• Report of illicit drug use or
toxic ingestion
• Shock (septic, metabolic,
• Decreased mental status
• Change in baseline mental
• Diabetes (hyper /
• History of trauma
• Hypoglycemia
diaphoretic skin)
• Acidosis / Alkalosis
• Environmental
KEY POINTS
• Protect the patient airway and support ABCs.
• Document the patient's initial Glasgow Coma Score.
• Naloxone (Narcan) administration may cause acute opiate withdraw, which includes vomiting, agitation,
or combative behavior. Be prepared for the possibility of combative behavior to ensure crew safety.
• Naloxone (Narcan) may wear off in as little as 20 minutes causing the patient to become more sedate and
possibly hypoventilate. All patients receiving Naloxone (Narcan) MUST be transported.
ONLY A FEW CAUSES CAN BE TREATED IN THE FIELD. CARE SHOULD FOCUS ON
MAINTAINING AIRWAY AND RAPID TRANSPORT
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
MEDICAL PROTOCOLS
PEDIATRIC
DIABETIC EMERGENCIES
MED CONTROL
UNIVERSAL PATIENT CARE PROTOCOL
Blood Sugar Analysis
Check for Hypotension,
Tachcardia, Poor Cap Refill
(If Alert with no IV Access
and no airway compromise)
NORMAL SALINE IV,
(If no IV Access)
Maximum 1 mg per dose
Recheck Blood Glucose
CONTACT MEDICAL CONTROL
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
MEDICAL PROTOCOLS
PEDIATRIC
DIABETIC EMERGENCIES
SIGNS AND SYMPTOMS
DIFFERENTIAL DIAGNOSIS
• Known diabetic, medic
• Irritability
• Pre-existing
SIGNS AND SYMPTOMS
DIFFERENTIAL DIAGNOSIS
• Known diabetic, medic
Consciousness / Coma
• Nausea / Vomiting
• Frequent Thirst and
• Hyperventilation
• Deep / Rapid Respirations
KEY POINTS
• Diabetic Ketoacidosis(DKA) is a complication of diabetes mellitus. It can occur when insulin levels
become inadequate to meet the metabolic demands of the body for a prolonged amount of time (onset can be within 12-24 hours). Without enough insulin the blood glucose increases and cellular glucose depletes. The body removes excess blood glucose by dumping it into the urine. Pediatric patients in DKA should be treated as hyperglycemic under the Pediatric Diabetic Emergency Protocol.
• Patients can have Hyperglycemia without having DKA.
• Always suspect Hypoglycemia in patients with an altered mental status.
• If a blood glucose analysis is not available, a patient with altered mental status and signs and symptoms
consistent with hypoglycemia should receive Dextrose or Glucagon.
Dextrose is used to elevate BGL but it will not maintain it. The patient will need to follow up with a meal, if not transported to a hospital.
• If the patient is alert and has the ability to swallow; consider administering oral glucose, have patient drink
orange juice with sugar or a sugar – containing beverage, or have the patient eat a candy bar or meal.
• Check the patient's BGL after the administration of Dextrose, Glucagon, or after any attempt to raise the
• If IV access is successful after Glucagon IM and the patient is still symptomatic, Dextrose 25% 2 ml/kg
IV/IO can be administered.
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
MEDICAL PROTOCOLS
PEDIATRIC
HEAT ILLNESS
MED CONTROL
UNIVERSAL PATIENT CARE PROTOCOL
Document Patient Temperature
Remove Patient from Heat Source
Remove Patient Clothing
Apply Room Temperature Water to Patient
Skin and Increase Air Flow Around Patient
Fever – 20 cc kg, NS Bolus
Heat Exhaustion: IV NS Wide Open
Heat Stroke: IV NS TKO
Monitor and Reassess
Appropriate Protocol Based on Patient
CONTACT MEDICAL CONTROL
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
MEDICAL PROTOCOLS
PEDIATRIC
HEAT ILLNESS
SIGNS AND SYMPTOMS
DIFFERENTIAL DIAGNOSIS
• Altered mental status or
• Exposure to increased
temperatures and humidity
• Hot, dry or sweaty skin
• Hypotension or shock
• Hyperthyroidism
history/medications
• Delirium tremens (DT's)
• Time and length of
• Poor PO intake
• CNS lesions or tumors
• Fatigue and/or muscle
Heat Exhaustion: Dehydration
Heat Stroke: Cerebral Edema
• Muscular/abdominal
• Skin hot, dry, febrile
• BP normal or orthostatic
KEY POINTS
•
Exam: Mental Status, Skin, HEENT, Heart, Lungs, Neuro
• Extremes of age are more prone to heat emergencies (i.e. young and old).
• Predisposed by use of: tricyclic antidepressants, phenothiazines, anticholineergic medications, and
• Cocaine, Amphetamines, and Salicylates may elevate body temperatures. • Sweating generally disappears as body temperature rises above 104EF (40EC).
• Intensive shivering may occur as patient is cooled. • Heat Cramps consists of benign muscle cramping 2E to dehydration and is not associated with an
elevated temperature.
• Heat Exhaustion consists of dehydration, salt depletion, dizziness, fever, mental status changes,
headache, cramping, nausea and vomiting. Vital signs usually consist of tachycardia, hypotension, and an elevated temperature.
• Heat Stroke consists of dehydration, tachycardia, hypotension, temperature >104EF (40EC), and altered
• Patients at risk for heat emergencies include neonates, infants, geriatric patients, and patients with
mental illness. Other contributory factors may include heart medications, diuretics, cold medications and/or psychiatric medications.
• Heat exposure can occur either due to increased environmental temperatures or prolonged exercise or a
combination of both. Environments with temperature >90EF and humidity >60% present the most risk.
• Heat stroke occurs when the cooling mechanism of the body (sweating) ceases due to temperature
overload and/or electrolyte imbalances. Be alert for cardiac dysrhythmias for the patient with heat stroke.
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
MEDICAL EMERGENCIES
PEDIATRIC
HYPOTHERMIA / FROSTBITE
MEDCONTROL
UNIVERSAL PATIENT CARE PROTOCOL
Remove wet clothing
Evidence or decreased core temperature?
Handle patient gently
Apply hot packs indirectly to skin and/or
blankets and turn up vehicle heat
Appropriate Protocol
Based on patient Signs and Symptoms
CONTACT MEDICAL CONTROL
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
MEDICAL PROTOCOLS
PEDIATRIC
SIGNS AND SYMPTOMS
DIFFERENTIAL DIAGNOSIS
• Environmental
• Exposure to environment even
• Mental status changes
• Hypoglycemia
in normal temperatures
• Extremity pain or
• Exposure to extreme cold
• Drug use: Alcohol, barbituates
• Spinal cord injury
• Infections / Sepsis
• Hypotension or shock
• Length of exposure / Wetness
KEY POINTS
• Exam: Mental Status, Heart, Lungs, Abdomen, Extremities, Neuro
• Hypothermic/drowning/near drowning patients that appear cold and dead are NOT dead until they are
warm and dead, or have other signs of obvious death (putrification, traumatic injury unsustainable to life).
• Defined as core temperature < 35° C (95° F).
• Extremes of age are more susceptible (i.e. young and old).
• Patients with low core temperatures will not respond to ALS drug interventions. Maintain warming
procedure and supportive care. Warming procedures includes removing wet clothing, limiting exposure, and covering the patient with warm blankets if available.
• Do not allow patients with frozen extremities to ambulate.
• Superficial frostbite can be treated by using the patient's own body heat.
• Do not attempt to rewarm deep frostbite unless there is an extreme delay in transport, and there is a no
risk that the affected body part will be refrozen. Contact Medical Command prior to rewarming a deep frostbite injury.
• With temperature less than 31° C (88° F) ventricular fibrillation is common cause of death. Handling
patients gently may prevent this. (rarely responds to defibrillation).
• If the temperature is unable to be measured, treat the patient based on the suspected temperature.
• Hypothermia may produce severe bradycardia.
• Shivering stops below 32° C (90° F).
• Hot packs can be activated and placed in the armpit and groin area if available.
• Care should be taken not to place the packs directly against the patient's skin.
• Consider withholding CPR if patient has organized rhythm. Discuss with medical control.
• All hypothermic patients should have resuscitation performed until care is transferred, or if there are other
signs of obvious death (putrification, traumatic injury unsustainable to life).
• Patients with low core temperatures will not respond to ALS drug interventions. Maintain warming
procedure and supportive care. Warming procedures includes removing wet clothing, limiting exposure, and covering the patient with warm blankets if available.
• The most common mechanism of death in hypothermia is ventricular fibrillation. If the hypothermia victim
is in ventricular fibrillation, CPR should be initiated. If V fib is not present, then all treatment and transport decisions should be tempered by the fact that V fib can be caused by rough handling, noxious stimuli or even minor mechanical disturbances, this means that respiratory support with 100% oxygen should be done gently, including intubation, avoiding hyperventilation.
• The heart is most likely to fibrillate between 85-88 degrees F. (29-31 degrees C.) Defibrillate VF / VT at
360 J with affective CPR intervals. May give a total of 3 shocks.
• Do not allow patients with frozen extremities to ambulate.
• Superficial frostbite can be treated by using the patient's own body heat.
• Do not attempt to rewarm deep frostbite unless there is an extreme delay in transport, and there is a no
risk that the affected body part will be refrozen. Contact Medical Command prior to rewarming a deep frostbite injury.
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
MEDICAL PROTOCOLS
PEDIATRIC
NEONATAL RESUSCITATION
UNIVERSAL PATIENT CARE
MED CONTROL
Meconium in Amniotic Fluid?
Dry Infant and Keep Warm.
Bulb syringe suction mouth and
Stimulate infant and note
Respirations Present?
Reassess Heart Rate and
BVM 30 seconds at
40 – 60 Breaths per
minute with 100%
See Pediatric Airway Protocol
Monitor and Reassess
See Pediatric Airway
Appropriate Dysrhythmia
NORMAL SALINE BOLUS
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
MEDICAL PROTOCOLS
PEDIATRIC
NEONATAL RESUSCITATION
SIGNS AND SYMPTOMS
DIFFERENTIAL DIAGNOSIS
• Due date and gestational
• Multiple gestation (twins
mottling (normal)
• Maternal medication effect
• Hypoglycemia
• Congenital heart disease
substance abuse smoking
KEY POINTS
•
Exam: Mental Status, Skin, HEENT, Neck, Chest, Heart, Abdomen, Extremities, Neuro
• Maternal sedation or narcotics will sedate infant (Naloxone effective).
• Consider hypoglycemia in infant.
• Document 1 and 5 minute APGAR scores (see Appendix)
• If the patient is in distress, consider causes such as; hypovolemia. Administer a 10 ml/kg fluid bolus of
• If the BGL less than 40 mg/dl go to the Pediatric Diabetic Protocol.
• Hypothermia is a common complication of home and field deliveries. Keep the baby warm and dry.
• If there is a history of recent maternal narcotic use, consider Naloxone (Narcan) 0.1 mg/kg every 2-5
minutes until patient responds.
• Meconium may need to be suctioned several times to clear airway. It may also be necessary to visualize
the trachea and suction the lower airway. Lower airway suction is achieved by intubating the infant and
suctioning directly through the ET tube. Each time his suctioning is done, the infant will have to be
reintubated with a new tube. This lower airway suction is only done when the infant is
NOT vigorous.
• If drying and suction has not provided enough stimulation, try rubbing the infant's back or flicking their
feet. If the infant still has poor respiratory effort, poor tone, or central cyanosis, consider them to be distressed, Most distressed infants will respond quickly to BVM.
• Use caution not to allow newborns to slip from grasp.
APGAR SCORING
HEART RATE
(Response to
Stimulation)
MUSCLE TONE
Flexion of Extremities Active Motion
RESPIRATORY
Slow and Regular
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
MEDICAL PROTOCOL
PEDIATRIC
ESOPHAGEAL FOREIGN BODY OBSTRUCTION
UNIVERSAL PATIENT CARE PROTOCOL
MEDCONTROL
Airway Obstruction
Esophageal Obstruction
Difficulty Breathing
Unable to Swallow
Difficulty/Unable to Talk
To Airway Protocol
Patient is in Distress
Evaluate Level of
HIGH (Neck Down)
Protected Airway
<16 years give ½ mg well mixed Glucagon IV
PROBLEM RESOLVED?
CONTACT MEDICAL CONTROL
To Consider 0.4 mg S/L NTG
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
MEDICAL PROTOCOLS
PEDIATRIC
ESOPHAGEAL FOREIGN BODY OBSTRUCTION
SIGNS AND SYMPTOMS
• Onset during eating or
• Airway obstruction –
swallowing pills, etc.
• Unable to swallow
coughing, unable to
speak, difficulty breathing
• Able to breathe but may
KEY POINTS
• Rule out airway obstruction first.
• Patient may be helpful in identifying location of bolus obstruction as they can feel it, point to it.
• If bolus is located in neck area, glucagon will not work, just monitor and transport.
• If bolus located from neck down, proceed with glucagon treatment.
• Treat patients <16 years with ½ mg dose of glucagon.
• Discuss use of NTG with Medical Control.
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
MEDICAL PROTOCOLS
PEDIATRIC
MED CONTROL
UNIVERSAL PATIENT CARE PROTOCOL
Position on side to prevent aspiration
Cooling Measures
Blood Glucose Analysis
e of Shock or Trauma?
(If Alert with no IV Access)
no airway compromise
(If no IV Access)
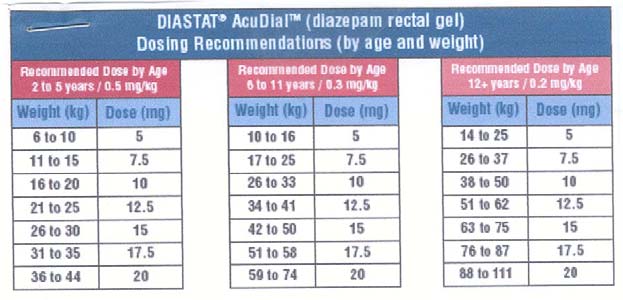
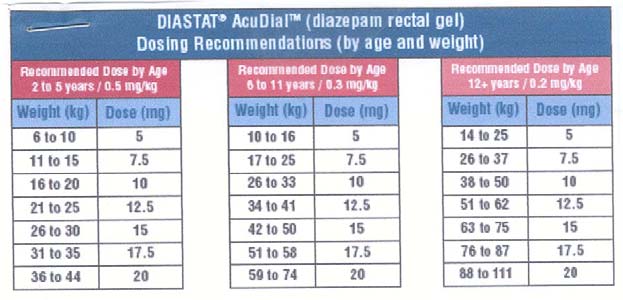
(See Chart in Protocol)
(If no IV Access)
0.2 mg/kg slow IV/IO
0.02 mg/kg slow IV
OR Via Atomizer Nasally
CONTACT MEDICAL CONTROL
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
MEDICAL PROTOCOLS
PEDIATRIC
SIGNS AND SYMPTOMS
• Prior history of seizures
• Altered mental status
• Hot, dry skin or elevated
body temperature
• Medication or Toxin
• History of recent head
• Hypoglycemia
• Metabolic abnormality /
Categories of Seizures
Unconscious
Partial,
Localized
Conscious
Generalized
Generalized
Generalized
KEY POINTS
•
Exam: Mental Status, HEENT, Heart, Lungs, Extremities, Neuro
•
Status Epilepticus is defined as two or more successive seizures without a period of consciousness or
recovery. This is a true emergency requiring rapid airway control, treatment, and transport.
•
Grand mal seizures (generalized) are associated with loss of consciousness, incontinence, and tongue
•
Focal seizures (petit mal) effect only a part of the body and are not usually associated with a loss of
•
Jacksonian seizures are seizures, which start as a focal seizure and become generalized.
• Be prepared to assist ventilations especially if a benzodiazipine is used.
• If evidence or suspicion of trauma, spine should be immobilized.
• If febrile, remove clothing and sponge with room temperature water.
•
In an infant, a seizure may be the only evidence of a closed head injury.
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
MEDICAL PROTOCOLS
PEDIATRIC
SHOCK (NON – TRAUMATIC)
MED CONTROL
UNIVERSAL PATIENT CARE PROTOCOL
Pediatric Trauma
Evidence or history of trauma
Hypovolemic / Septic/ Neurogenic
PERSONAL EPI PEN
Allergic Reaction
Monitor and Reassess
Blood Glucose Analysis
Glucose < 60
(If Alert with no IV Access)
If no airway compromise
Impending Full Arrest & Hypotensive
(If no IV Access)
0.01 mg/kg IV/IO
1:10000 Solution
CONTACT MEDICAL CONTROL
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
MEDICAL PROTOCOLS
PEDIATRIC
SHOCK (NON – TRAUMATIC)
SIGNS AND SYMPTOMS
DIFFERENTIAL DIAGNOSIS
• Restlessness,
• Increased HR, rapid pulse
Pale, cool, clammy skin
• Delayed capillary refill
• Congenital heart disease
• Medication or Toxin
ALLERGIC REACTION / ANAPHYLAXIS
SIGNS AND SYMPTOMS
DIFFERENTIAL DIAGNOSIS
• Onset and location
• Warm Burning Feeling
• Urticaria (rash only)
• Insect sting or bite
• Food allergy / exposure
• Medication allergy /
• Shock (vascular effect)
• New clothing, soap,
• Aspiration / Airway
• Past history of reactions
• Altered LOC / Coma
• Pulmonary Edema
• Facial / Airway Edema
• Urticaria / Hives
KEY POINTS
•
Exam: Mental Status, Skin, HEENT, Heart, Lung, Abdomen, Extremities, Back, Neuro
• Consider all possible causes of shock and treat per appropriate protocol.
• Decreasing heart rate is a sign of impending collapse.
• Most maternal medications pass through breast milk to the infant. Examples: Narcotics, Benzodiazepines.
• Be sure to use the appropriate sized BP cuff.
• Findings in the primary assessment should alert you that the patient is in shock. Pay particular attention
to the patient's mental status, tachycardia, skin color, and capillary refill.
• Shock is not only caused by blood loss. The EMT must evaluate for fluid loss from other causes such as excessive vomiting and/or diarrhea, heat exposure and malnutrition. • Do not use only the patient's blood pressure in evaluating shock; also look for lower body
temperature, poor capillary refill, decreased LOC, increased heart rate and/or poor skin color or turgor
• Routinely reassess the patient and provide supportive care.
• Use caution when using Epinephrine for patients with a cardiac history.
• Use caution when using Epinephrine for patients with a heart rate greater than 120 bpm.
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
MEDICAL PROTOCOLS
PEDIATRIC
TOXIC INGESTION / EXPOSURE / OVERDOSE
MED CONTROL
UNIVERSAL PATIENT CARE PROTOCOL
See Pediatric Airway Protocol
Blood Glucose Analysis
Tricyclic Ingestion?
SODIUM BICARBONATE
Diluted in 1:1 NS
Respiratory Depression
Organophosphates
0.02 mg/kg IV/IO
repeat every 3-5 minutes
CONTACT MEDICAL CONTROL
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
MEDICAL PROTOCOLS
PEDIATRIC
TOXIC INGESTION / EXPOSURE / OVERDOSE
SIGNS AND SYMPTOMS
DIFFERENTIAL DIAGNOSIS
• Ingestion or suspected
• Mental status changes
ingestion of a potentially
• Hypo / Hypertension
• Decreased respiratory rate
• Acetaminophen
• Tachycardia,
• Time of ingestion
• Anticholinergic
accidental, criminal)
• Available medications in
• Insecticides
(organophosphates)
Organophosphates
COMMON TRICYCLICS Brand
Tofranil Imipramine Norpramin
Vivactil Protriptyline Ludimomil
KEY POINTS
• Routinely assess and document the patient's cardiopulmonary status.
• Determine what the patient was exposed to, how much, and when. If it is safe to do so, bring a sample
with you to the hospital.
• Be sure to find out what interventions were administered prior to EMS arrival and document.
• If the patient ingested bleach, monitor the airway and remove contaminated clothing.
• Medical Direction may order antidotes for specific ingestions.
•
DO NOT use syrup of ipecac.
• Reference: Greater Cleveland Poison Control Center 1-800-222-1222.
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 10 – 2006
0406-074.doc
TRAUMA PROTOCOLS
PEDIATRIC
HEAD TRAUMA
UNIVERSAL PATIENT CARE
MED CONTROL
Isolated Head Trauma?
Spinal Immobilization Protocol
Does patient respond to verbal?
No None or Extension
Response to Pain?
Localizes, Flexes, or Withdraws
Pupils Equal and Reactive?
Pediatric Seizure
Blood Glucose Analysis
(If no IV Access)
Monitor and Reassess
CONTACT MEDICAL CONTROL
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 6 – 2006
0406-074.doc
TRAUMA PROTOCOLS
PEDIATRIC
HEAD TRAUMA
SIGNS AND SYMPTOMS
DIFFERENTIAL DIAGNOSIS
• Time of injury
• Pain, swelling, bleeding
• Mechanism (blunt vs.
• Altered mental status
• Brain injury (Concussion,
Contusion, Hemorrhage or
• Loss of consciousness
• Respiratory distress /
• Subarachnoid
• Evidence for multi-trauma
mechanism of injury
KEY POINTS
•
Exam: Mental Status, HEENT, Heart, Lungs, Abdomen, Extremities, Back, Neuro
• If GCS < 12 consider air / rapid transport and if GCS < 8 intubation should be anticipated.
• Hyperventilate the patient only if evidence of herniation (blown pupil, decorticate / decerebrate posturing,
• If hyperventilation is needed (35/minute for infants <1 year and 25/minute for children >1 year)
• Increased intracranial pressure (ICP) may cause hypertension and bradycardia (Cushing's Response).
• Hypotension usually indicates injury or shock unrelated to the head injury.
• The most important item to monitor and document is a change in the level of consciousness.
• Concussions are periods of confusion or LOC associated with trauma, which may have resolved by the
time EMS arrives. A physician ASAP should evaluate any prolonged confusion or mental status abnormality, which does not return to normal within 15 minutes or any documented loss of consciousness.
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 6 – 2006
0406-074.doc
TRAUMA PROTOCOLS
PEDIATRIC
MULTIPLE TRAUMA
MED CONTROL
UNIVERSAL PATIENT CARE PROTOCOL
Rapid trauma assessment
See Pediatric Airway Protocol
Spinal Immobilization Protocol If Indicated
Rapid Transport to
Determine Load and Go Situation
Consider rapid /
Most Appropriate
Vital Signs / Perfusion?
NORMAL SALINE IV
Ongoing Assessment
Appropriate Protocol
Repeat as needed
Reassess Airway Protocol
Check tube placement / hyperventilate
CONTACT MEDICAL CONTROL
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 6 – 2006
0406-074.doc
TRAUMA PROTOCOLS
PEDIATRIC
MULTIPLE TRAUMA
SIGNS AND SYMPTOMS
DIFFERENTIAL DIAGNOSIS
Time and mechanism of
Life Threatening:
Deformity, lesions, bleeding
Damage to structure or
Location in structure or
Hypotension or shock
Others injured or dead
• Intra-abdominal
Speed and details of MVC
Pelvis / Femur fracture
Restraints / Protective
Spine fracture / Cord injury
Head injury (see Head
Extremity fracture /
HEENT (Airway obstruction)
Past medical history
A Pediatric Trauma Victim is a person < 16 years of age exhibiting one or more of the following
physiologic or anatomic conditions:
Physiologic conditions
Anatomic conditions
Glasgow Coma Scale < 13;
Penetrating trauma to the head, neck, or torso;
Loss of consciousness > 5 minutes;
Significant, penetrating trauma to extremities proximal to the
Deterioration in level of consciousness at the scene or
knee or elbow with evidence of neurovascular compromise;
during transport;
Injuries to the head, neck, or torso where the following physical
Failure to localize to pain;
findings are present;
Evidence of poor perfusion, or evidence of respiratory
distress or failure.
Abdominal tenderness, distention, or seatbelt sign;
Injuries to the extremities where the following physical findings are present:
Amputations proximal to the wrist or ankle;
Fractures of two or more proximal long bones;
Evidence of neurovascular compromise.
Signs or symptoms of spinal cord injury;
2nd or 3rd Degree burns > 10% total BSA, or other significant burns involving the face, feet, hands, genitalia, or airway.
KEY POINTS
Exam: Mental Status, Skin, HEENT, Heart, Lung, Abdomen, Extremities, Back, Neuro
Mechanism is the most reliable indicator of serious injury. Examine all restraints / protective equipment for damage.
In prolonged extrications or serious trauma consider air transportation for transport times and the ability to give blood.
Do not overlook the possibility for child abuse.
A trauma victim is considered to be a pediatric patient if they are 15 years old or younger.
Major Trauma patients are to be transported to the closest Pediatric Trauma Center.
Contact the receiving hospital for all major trauma or critical patients.
The Proper size equipment is very important to resuscitation care. Refer to length based drug treatment guide (e.g. BROSELOW PEDIATRIC EMERGENCY TAPE OR SIMILAR GUIDE) when unsure about patient weight, age and/or drug dosage and when choosing equipment size.
Cover open wounds, burns, eviscerations.
With the exception of airway control, initiate ALS enroute when transporting major trauma patients.
If unable to access patient airway and ventilate, then transport to the closest facility for airway stabilization.
The on scene time for major trauma patients should not exceed 10 minutes without documented, acceptable reason for the delay.
When initiating an IV and drawing blood, collect a red top blood tube to assist the receiving hospital with determining the patient's blood type.
All major trauma patients should receive oxygen administration, an IV(s), and cardiac monitoring.
Provide a documented reason if an intervention could not be performed.
Pediatric Trauma Centers include MetroHealth Medical Center and Rainbow, Babies, and Children's Hospital.
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 6 – 2006
0406-074.doc
PEDIATRIC ASSESSMENT CHARTS
PEDIATRIC
GLASCOW COMA SCALE
EYE OPENING
Spontaneous Spontaneous
VERBAL RESPONSE
Irritable cry, inconsolable
MOTOR RESPONSE
Normal movements
Withdraws to touch
Withdraws to pain
Withdraws to pain
Extension Extension
* NOTE: MOTOR RESPONSE IS MOST INDICATIVE OF LEVEL OF INJURY
PEDIATRIC ASSESSMENT CHARTS
PEDIATRIC
NORMAL VITAL SIGNS
HEART RATE
SYSTOLIC BLOOD PRESSURE
Newborn 126-160 30-60
Blood pressure is a late and unreliable indicator of shock in children
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 6 – 2006
0406-074.doc
THIS PAGE INTENTIONALLY LEFT BLANK
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 6 – 2006
0406-074.doc
PEDIATRIC
PHARMACOLOGY REVIEW
MEDICATION
• Acetaminophen (Tylenol)
Useful for musculoskeletal pain and fever control
• Activated charcoal
Do not give to child with altered level of consciousness
• Adenosine
Indicated for SVT. First dose 6mg, second dose 6mg. Max dose 12mg
• Albuterol
Indicated for wheezing as per protocol
• Amiodarone
Over 20-60 minutes, maximum 15 mg/kg per day. For shock-refractory pulseless VT/VF: 5 mg/kg rapid IV/IO
• Atropine
Minimum dose 0.1 mg; max dose for child 0.5 mg; max dose for adolescent 1.0 mg; may repeat x1; Also useful before intubating children < 5 years old, blocks bradycardia due to vagal nerve stimulation
• Dextrose 25%
Try to obtain bedside glucose level before administering ----administer if blood glucose < 60; dilute 50% 1:1 with sterile water; consult Medical Control if infant < 1 month as solution may need to be further diluted.
• Diazepam (Valium
Indicated for uncontrolled seizure mg/kg activity; anticipate respiratory depression. Max. dose 10 mg.
• Diazepam (Valium)
Indicated for uncontrolled seizure activity; anticipate respiratory depression. Max. dose 10 mg.
• Diphenhydramine
Useful in allergic reactions and anaphylaxis. Max dose 50 mg
(Benadryl)
• Epinephrine
Commonly used in cardiac arrest rhythms as first dose.
(1:10,000)
Increase second dose 10 X (may use 1:1,000 solution).
• Epinephrine
Commonly used in cardiac arrest rhythms.
(1:1,000)
Use for all ET doses, and second and subsequent IV/IO doses. *The ET route has limited absorption, use IV/IO route whenever possible
Used for anaphylaxis. Max dose is 0.3ml
• Lidocaine
Can repeat once. If successful start continuous infusion at 20-50 mg/kg/min. Also useful before intubating for cerebral protection and decreases airway reactivity.
• Morphine
Useful for moderate pain, may cause respiratory depression. Hypotension and reflex bradycardia may develop from histamine release
• Midazolam (Versed)
Indicated for uncontrolled seizure activity; anticipate respiratory depression Useful to facilitate advanced airway management in combative patients
• Naloxone (Narcan)
Useful for unknown unconscious, known narcotic overdoses
• Procainamide
Over 30-60 minutes. Alternative treatment for recurrent or refractory VT, SVT.
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 6 – 2006
0406-074.doc
EUCLID, HILLCREST, HURON, AND SOUTH POINTE HOSPITALS EMS PROTOCOLSAND PROCEDURES - PEDIATRIC PROTOCOLS REVISED 6 – 2006
0406-074.doc
Source: http://www.cchseast.org/Portals/23/ems/EMSProtocols/6_0%20Pediatric.pdf
olume 5, Issue 1, June 2015 ragyaan: Journal of Law a bi-annual refereed Journal Affordability of Medicine: A Serious Concern to Achieve Health for All Dr. Gargi Chakrabarti Social Stigma Surrounding Surrogacy and Prostitution in Indian Society: A Critique Ms. Sonali Kusum Role of Panchayati Raj Institutions in the Decentralization of Governance: A Critique Mr. Divyesh Choudhary, Ms. Sayantika Ganguly
AUTORESDepartamento de Control del Comité Aragonés de Agricultura Ecológica (CAAE).Departamento de Agricultura, Ganadería y Medio Ambiente Dirección General de Alimentación y Fomento Agroalimentario (SSA). LGM. FOTOGRAFíASDepartamento de Control del CAAE. Comisión Europea (nº 9, 18, 20, 21 y 23) DIRECCIÓN EDITORIALComité Aragonés de Agricultura Ecológica