Conmedlinvatec.ae
Anesthesiology 2002; 97:820 – 6
2002 American Society of Anesthesiologists, Inc. Lippincott Williams & Wilkins, Inc.
Goal-directed Intraoperative Fluid Administration Reduces
Length of Hospital Stay after Major Surgery
Tong J. Gan, M.B., B.S, F.R.C.A.,*
Andrew Soppitt, B.Sc., M.B., B.S., F.R.C.A.,†
Mohamed Maroof, M.D.,‡
Habib El-Moalem, Ph.D.,§
Kerri M. Robertson, M.D.,*
Eugene Moretti, M.D.,†
Peter Dwane, M.D.,‡
Peter S. A. Glass, M.B., F.F.A. (S.A.)储
Background: Intraoperative hypovolemia is common and is a
rapid, minimally invasive, and continuous estimation of
potential cause of organ dysfunction, increased postoperative
cardiac output.6 The cardiac output measurements ob-
morbidity, length of hospital stay, and death. The objective of
tained with the EDM have been shown to correlate well
this prospective, randomized study was to assess the effect
of goal-directed intraoperative fluid administration on length of
with the thermodilution method by different investiga-
postoperative hospital stay.
tors.7–11 Using the EDM to guide intraoperative plasma
Methods: One hundred patients who were to undergo major
volume expansion, Sinclair
et al.4 demonstrated signifi-
elective surgery with an anticipated blood loss greater than
cant improvement in postoperative recovery and short-
500 ml were randomly assigned to a control group (n ⴝ
50) that
ened hospital stay in patients undergoing proximal fem-
received standard intraoperative care or to a protocol group
(n ⴝ
50) that, in addition, received intraoperative plasma vol-
oral neck fracture repair. Mythen and Webb,3 in a study
ume expansion guided by the esophageal Doppler monitor to
in cardiac patients, demonstrated a reduction in the
maintain maximal stroke volume. Length of postoperative hos-
incidence of gastrointestinal mucosal hypoperfusion and
pital stay and postoperative surgical morbidity were assessed.
major complications in patients who received plasma
Results: Groups were similar with respect to demographics,
surgical procedures, and baseline hemodynamic variables. The
protocol group had a significantly higher stroke volume and
In this study, we investigated whether goal-directed
cardiac output at the end of surgery compared with the control
intraoperative plasma volume expansion guided by the
group. Patients in the protocol group had a shorter duration
EDM would shorten the length of hospital stay and
of hospital stay compared with the control group: 5 ⴞ
3 versus
improve postoperative outcomes (gastrointestinal and
7 ⴞ
3 days (mean ⴞ
SD), with a median of 6 versus 7 days,
renal dysfunction) in patients undergoing moderate-risk
respectively (P ⴝ
0.03). These patients also tolerated oral intake
of solid food earlier than the control group: 3 ⴞ
0.5 versus 4.7 ⴞ
0.5 days (mean ⴞ
SD), with a median of 3 versus 5 days,
respectively (P ⴝ
0.01).
Conclusions: Goal-directed intraoperative fluid administra-
tion results in earlier return to bowel function, lower incidence
of postoperative nausea and vomiting, and decrease in length of
postoperative hospital stay.
After we obtained approval from the institutional re-
view board, written informed patient consent was ob-
INTRAOPERATIVE hypovolemia is common and may be
tained from 100 patients with American Society of An-
a potential cause of organ dysfunction, increased post-
esthesiologists (ASA) physical status I, II, and III who
operative morbidity, and death.1,2 Goal-directed plasma
were to undergo major elective general, urologic, or
volume expansion during the intraoperative period is
gynecologic surgery with an anticipated blood loss of
associated with improved outcome and reduction in
greater than 500 ml. Exclusion criteria included patients
hospital stay in patients undergoing cardiac and major
with age less than 18 yr, emergency surgery, preopera-
orthopedic surgery.3–5
tive bowel obstruction, coagulopathy, significant renal
The esophageal Doppler monitor (EDM) is an Food
and hepatic dysfunction (creatinine ⬎ 50% or liver en-
and Drug Administration–approved device that permits
zymes ⬎ 50% upper limit of normal values), congestiveheart failure, and esophageal pathology (avoid potentialcomplications of the esophageal probe), and those un-dergoing gastric or esophageal surgery or who were on
This article is featured in "This Month in Anesthesiology."
antiemetic medication within 3 days of surgery.
Please see this issue of ANESTHESIOLOGY, page 5A.
All patients were premedicated with midazolam and
fentanyl. Before induction of anesthesia, an intravenous
* Associate Professor, † Associate, ‡ Assistant Professor, § Assistant Research
bolus of 5 ml/kg lactated Ringer's solution was adminis-
tered, followed by an intravenous infusion of lactated
储 Professor, University Medical Center at Stony Brook, Department of
Anesthesiology Health Sciences Center, Stony Brook, New York.
Ringer's solution at a rate of 5 ml · kg⫺1 · h⫺1, which was
Received from the Department of Anesthesiology, Duke University Medical
continued for the duration of surgery. Anesthesia was
Center, Durham, North Carolina. Submitted for publication September 27, 2001.
induced by an intravenous technique and maintained
Accepted for publication May 30, 2002. Supported in part by Deltex Medical,Inc., Irving, Texas.
with a balanced inhalational technique incorporating
Address reprint requests to Dr. Gan: Box 3094, Department of Anesthesiology,
isoflurane 0.5–1.5% and 50% nitrous oxide in oxygen.
Duke University Medical Center, Durham, North Carolina 27710. Address elec-
Tracheal intubation was facilitated with succinylcholine,
tronic mail to:
[email protected]. Individual article reprints may be pur-chased through the Journal Web site, www.anesthesiology.org.
and neuromuscular blockade was maintained using pan-
Anesthesiology, V 97, No 4, Oct 2002
GOAL-DIRECTED FLUID ADMINISTRATION REDUCES HOSPITAL STAY
curonium. All patients received 1.25 mg droperidol as
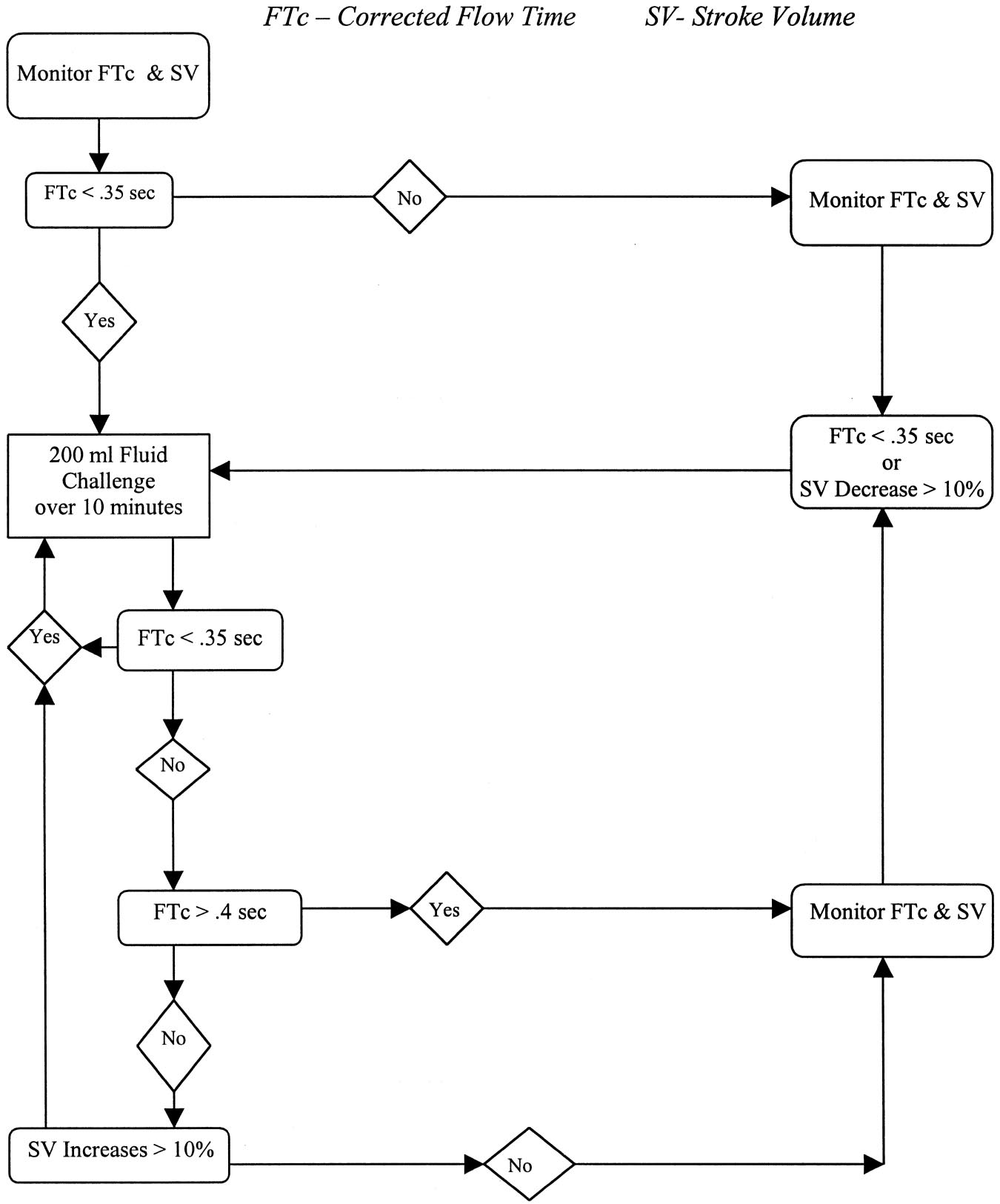
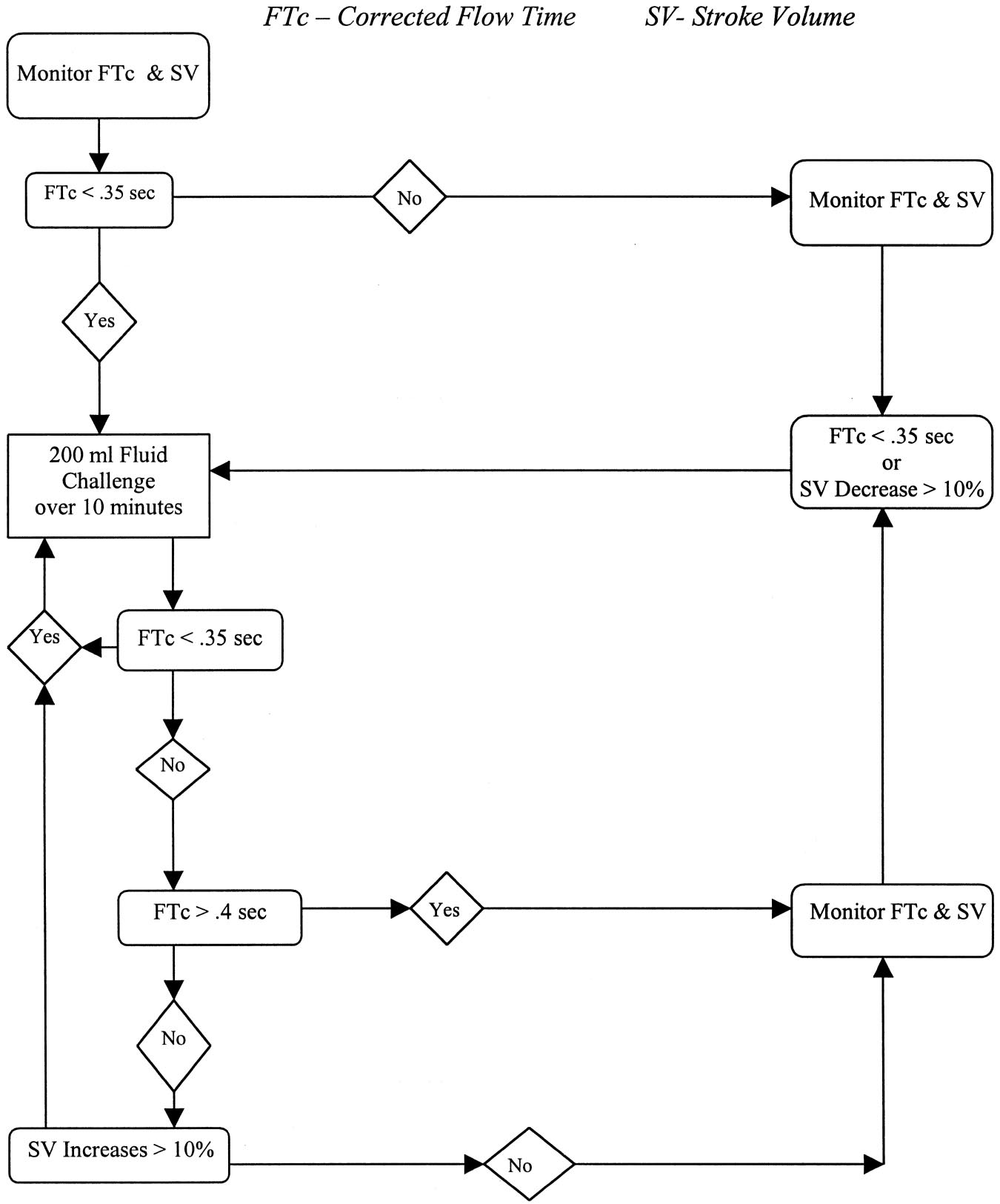
given when the FTc was less than 0.35 s. If the stroke
a prophylactic antiemetic. Additional fentanyl up to 3
volume was maintained or increased by the fluid chal-
g · kg⫺1 · h⫺1 was given as required. Ventilation was
lenge and the FTc remained below 0.35 s, the fluid
adjusted to maintain arterial carbon dioxide partial pres-
challenge was repeated. If the stroke volume increased
sure at 35– 40 mmHg, and temperature was maintained
by more than 10% and the FTc exceeded 0.35 s, the fluid
at greater than 35°C throughout surgery. If an epidural
challenge was repeated until no further increase in
catheter was placed preoperatively for postoperative
stroke volume occurred. If the FTc increased above
pain management, a 3-ml test dose consisting of lido-
0.40 s with no change in stroke volume, further fluid was
caine 1.5% with 1:200,000 epinephrine was adminis-
not then administered until the stroke volume decreased
tered, and no subsequent epidural local anesthetic drugs
by 10% of the last value. The procedure was started
were administered intraoperatively. Postoperative anal-
immediately after probe placement and continued every
gesia was provided by either epidural (bupivacaine
15 min until maximum stroke volume and targeted FTc
0.125% and hydromorphone 0.001%) or patient-con-
values had been reached. Further aliquots of fluid were
trolled analgesia with fentanyl. Anesthesia was main-
given to keep the FTc at the targeted values. In addition,
tained at a constant level as judged by standard clinical
patients also received fluid equivalent to that judged to
be lost as a result of surgical hemorrhage. When
Following induction of anesthesia, an esophageal
20 ml/kg of 6% hydroxyethyl starch in saline had been
Doppler probe (EDM™; Deltex Medical, Inc., Irving, TX)
given, lactated Ringer's solution was used for further
was greased with lubricating gel and inserted orally into
fluid boluses as required. The designation of an upper
the midesophagus in all patients. Blood flow signals
limit of 20 ml/kg of 6% hydroxyethyl starch in saline
were identified. Once achieved, satisfactory position
represents the standard practice within our institution.
was maintained by taping the probe cable to either the
Crystalloid was used in a 3:1 ratio for the replacement of
patient's face or the endotracheal tube. The EDM mon-
surgical blood loss.
itor displays a blood flow velocity waveform that repre-
In the control group, the EDM monitor was turned
sents the velocity of blood flow within the descending
away from the anesthesia care provider, and the screen
thoracic aorta. A nomogram incorporated in the monitor
was covered with an opaque card. The EDM variables
is used to estimate aortic cross-sectional area, enabling
were collected by an independent research personnel.
calculation of the left ventricular stroke volume from the
Hemodynamic variables triggering fluid administration
area of the velocity–time waveform. This nomogram
involved a urinary output less than 0.5 ml · kg⫺1 · h⫺1, an
includes the patient's height, weight, and age.6 The total
increase in heart rate more than 20% above baseline or
amount of time that blood is traveling in a forward
more than 110 beats/min, a decrease in mean systolic
direction within the aorta is the systolic flow time. This
blood pressure less than 20% below baseline or less than
is corrected for heart rate to give the corrected flow time
90 mmHg, or central venous pressure less than 20% of
(FTc). The FTc has been shown to be a good index of
baseline. Boluses of 200 ml of fluid were administered
systemic vascular resistance and is sensitive to changes
until the above target was restored. The anesthesiolo-
in left ventricular preload.12 Direct intraarterial pressure
gists would also administer additional fluid if deemed
was monitored in addition to electrocardiography, non-
clinically indicated and were instructed to conduct an-
invasive blood pressure, heart rate, end-tidal carbon di-
esthesia according to their customary practice.
oxide tension, temperature, and pulse oximetry. When
For the treatment of anemia and hypocoagulation, the
clinically indicated, a central venous catheter was placed
protocol called for the administration of blood products
following induction of anesthesia. All cardiovascular vari-
(erythrocytes, platelets, fresh frozen plasma, cryoprecip-
ables and urinary flow were monitored and recorded
itate, or fibrinogen) when clinically indicated and sup-
during general anesthesia. Types and volumes of all flu-
ported by the laboratory evidence of a hematocrit less
ids administered intraoperatively (including but not lim-
than 23% or abnormal coagulation (platelet count ⬍
ited to colloid and crystalloid solutions, blood, and blood
100,000/l, prothrombin time ⬎ 1.5 times control, acti-
products) were recorded, as were the volumes and
vated partial thromboplastin time ⬎ 1.5 times control, or
doses of any drugs given during general anesthesia and
fibrinogen ⬍ 100 mg/dl). Patients were extubated, ei-
an estimation made of blood loss.
ther in the operating room or postoperatively, when
Following insertion of the EDM probe, the patients
they fulfilled standard clinical criteria (adequate protec-
were randomized into either the protocol or control
tive reflexes, adequate oxygenation, and stable hemody-
group using a random number generator in sealed enve-
namics). They were visited daily in the immediate post-
lopes. In the protocol group, boluses of fluid were ad-
operative period by independent research personnel
ministered, guided by an algorithm depending on the
unaware of the patient's randomization until hospital
Doppler estimations of stroke volume and FTc (fig. 1).
discharge or death. During the visit, the patients were
This algorithm was similar to that used by Sinclair
et al.4
asked specific questions on adverse events and presence
A 200-ml aliquot of 6% hydroxyethyl starch in saline was
of flatus. The information was recorded in a data collec-
Anesthesiology, V 97, No 4, Oct 2002
GAN ET AL.
Fig. 1. Intraoperative fluid management
algorithm. FTc ⴝ corrected flow time;
SV ⴝ stroke volume.
tion form modified from a previous study in the same
methodology. The results were used to estimate the
institution.13 Those who had flatus were started on oral
necessary sample size for this prospective study. A sam-
fluids, which were followed by solid food if tolerated
ple of 50 patients in each group was calculated to have
(without emetic symptoms within 4 h). The length of
at least 90% power to detect a difference in mean of
postoperative stay was recorded. Postoperative care and
length of hospital stay of 2 days between the two groups,
discharge criteria were predefined using the hospital
using a two-group t test with a 0.05 two-sided
care map and protocol. Rescue antiemetic treatment
(4 mg intravenous ondansetron) was administered withtwo or more emetic episodes or on patient's request.
Data were analyzed comparing patients in the protocol
group with those in the standard practice group on anintent-to-treat basis. The groups were compared using
One hundred patients were enrolled. Two patients
t test or Wilcoxon rank-sum tests as appropriate. The
were not included for analysis (one patient in each
volumes of intravenous colloid and crystalloid adminis-
group) as neither had their scheduled surgery. The two
tered to the two groups were compared using a one-way
groups were well matched with regard to demographics,
analysis of covariance adjusting for each patient's esti-
ASA physical status, duration of anesthesia, intraopera-
mated blood loss. The incidence of adverse events was
tive fentanyl use, and type of surgery (table 1).
compared using the two-tailed Fisher exact test. A
The volume of colloid and crystalloid, erythrocyte, and
P value ⬍ 0.05 was considered statistically significant.
blood product administration for the two groups is
An earlier separate pilot study was conducted with
shown in table 2. Patients in the protocol group received
20 patients to familiarize researchers with the equip-
more 6% hetastarch compared with the control group.
ment and to determine the feasibility of the proposed
Eleven patients in the protocol group received erythro-
Anesthesiology, V 97, No 4, Oct 2002
GOAL-DIRECTED FLUID ADMINISTRATION REDUCES HOSPITAL STAY
Table 1. Demographic Data
7 ⫾ 3 days (mean ⫾ SD), 6 versus 7 days (median),respectively (P ⫽ 0.03). Patients in the protocol group
also tolerated an oral solid regimen earlier than the con-trol group: 3 ⫾ 0.5 versus 4.7 ⫾ 0.5 days (mean ⫾ SD),
3 versus 5 days (median), respectively (P ⫽ 0.01). Fewer
patients in the protocol group experienced severe post-
operative nausea and vomiting requiring rescue anti-
emetic treatment (P ⬍ 0.05; table 4). There were no
differences in the incidence of other complications
ASA physical status
Surgery type/epidural for
This prospective, randomized, controlled study dem-
onstrates that goal-directed intraoperative fluid administra-
tion during major surgery results in earlier gastrointestinal
Patients with central
function, a reduction in postoperative complications,
and a shortened hospital stay.
Use of vasoactive drugs
Hypovolemia is common among patients scheduled
for surgery. In addition to the inevitable losses in the
perioperative period caused by surgical trauma, evapo-
Hemoglobin (g/dl)
ration, and the use of dry anesthetic gases, the majority
of patients are routinely required to fast for a minimum
of 6 h preoperatively to reduce the risk of acid aspiration
Intraoperative fentanyl (g)
Duration of surgery (min)
syndrome.14 Hypovolemia during the perioperative pe-riod has been associated with a significant increase in
Data are number of patients or mean ⫾ SD. Vasoactive drugs were phenyl-
postoperative morbidity and mortality, ranging from
ephrine or esmolol administered in single doses.
postoperative nausea and vomiting15 to more serious
ASA ⫽ American Society of Anesthesiologists.
complications such as organ dysfunction,3 as well asprolongation of hospital stay.4
cyte transfusion versus nine in the control group, and
Bennett-Guerrero et al.13 recently demonstrated that
one patient each in the protocol group received fresh
gastrointestinal dysfunction is the most common post-
frozen plasma (351 ml) or platelets (538 ml), respec-
operative complication in patients undergoing moder-
tively. Baseline hemodynamic variables were similar be-
ate-risk surgery, especially those procedures involving
tween the two groups (table 3). There were no signifi-
laparotomy. Gastrointestinal dysfunction was the most
cant changes in heart rate and mean intraarterial blood
frequent reason for a prolonged length of hospital stay.
pressure between the two periods in both groups. How-
At postoperative day 5, 55% of the patients studied were
ever, there was a significant increase in Doppler-derived
unable to tolerate an enteral diet. More than 50% of
variables (stroke volume, cardiac output, and FTc) from
patients who were still hospitalized on postoperative
baseline to end of surgery in the protocol group com-
day 15 exhibited gastrointestinal dysfunction. Their find-
pared with the control group (table 3).
ings echo the results of our study. The reduction in
The length of hospital stay was shorter for the protocol
hospital stay observed was primarily the result of pa-
group compared with the control group: 5 ⫾ 3 versus
tients tolerating a solid regimen earlier. We also foundthe incidence of severe postoperative nausea and vom-
Table 2. Intraoperative Fluid, Blood, and Blood Product
iting requiring rescue antiemetic therapy was higher in
the control group compared with the protocol group. Itis conceivable that improved perfusion of gastric mucosa
as a result of additional fluid administration in the pro-tocol group could have resulted in less postoperative
6% hetastarch in saline
Lactated Ringer's solution
nausea and vomiting, as was demonstrated by previous
observation. In the same study, Bennett-Guerrero et al.13
Estimated blood loss
found a significant correlation between intraoperative
indices of tissue hypoperfusion (e.g., gastric pHi, arterial
Data are mean ⫾ SD (volume in ml).
base deficit) and gastrointestinal dysfunction. While we
* P ⬍ 0.01.
did not assess gastric mucosal perfusion, several studies
Anesthesiology, V 97, No 4, Oct 2002
GAN ET AL.
Table 3. Hemodynamic and Doppler-derived Variables at Baseline and at End of Surgery for Both Protocol and Control Groups
Heart rate (beats/min)
Mean arterial pressure (mmHg)
Stroke volume (ml)
Cardiac Output (l/min)
Corrected flow time (s)
* P ⬍ 0.05 comparing changes at end of surgery and baseline between the two groups.
Baseline ⫽ following induction of anesthesia and satisfactory placement of the esophageal Doppler probe as defined in the methods; End of Surgery ⫽ beforereversal of neuromuscular blocking effects and emergence of anesthesia.
have shown a direct relation between hypovolemia and
several limitations to the use of EDM. The monitor makes
gut hypoperfusion.3,16 Hence, it is plausible that the
assumptions on the diameter of the aorta based on the
protocol group that had optimal fluid administration
weight and height of the patient. There is a learning
during the intraoperative period may have had better gut
curve to achieve proficient placement of the probe to
perfusion, which resulted in a lower incidence of gas-
capture maximal signal. Insertion of 12 EDM probes
appears to be necessary to achieve adequate proficien-
We use the EDM to guide intraoperative fluid admin-
cy.19 There are other relatively noninvasive devices that
istration. The EDM is a minimally invasive method for
measure stroke volume and cardiac output that may also
continuous monitoring of the circulation. There is good
be useful for goal-directed intraoperative fluid adminis-
agreement between measures of cardiac output made
tration. These include noninvasive cardiac output using
simultaneously with the esophageal Doppler and a ther-
partial carbon dioxide rebreathing, transesophageal
modilution pulmonary arterial catheter.9,10 Pulmonary
echocardiography, Fick indicator dilution technique us-
arterial catheter insertion, however, requires technical
ing lithium, and thoracic impedance.
skill and may be associated with life-threatening compli-
We used FTc to guide volume replacement as it has
cations. Despite its widespread use, there is little or
been shown to be a more sensitive indicator of cardiac
limited evidence that the use of a pulmonary arterial
filling than pulmonary arterial diastolic pressure and pul-
catheter benefits patients. Indeed, there is evidence that
monary arterial occlusion pressure.8,20 For pulmonary
it may increase morbidity and mortality.17,18 There are
arterial diastolic pressure or pulmonary arterial occlu-sion pressure to increase, the left ventricle must be
Table 4. Incidence of Postoperative Complications
loaded sufficiently to increase left ventricular end-dia-
stolic pressure. In a ventricle with normal diastolic com-
pliance, major volume changes may not produce sub-stantial pressure changes, thus limiting the usefulness of
Acute renal dysfunction (urine output
the pulmonary arterial diastolic pressure as a marker for
Respiratory support for ⬎ 24 h
filling. In contrast, the FTc value represents the amount
of time required to eject the stroke volume, corrected
pulmonary edema, arrhythmia)
for heart rate. As the ventricle is filled, it requires more
Chest infection (clinical diagnosis)
Severe PONV requiring rescue
time to eject the greater stroke volume, even in ventri-
cles with normal compliance.
Other investigators have demonstrated that optimal
fluid administration during the intraoperative period ap-
Data presented as number of patients (%). Postoperative complications def-
pears to reduce morbidity and length of hospital stay.
inition based on Bennett-Gurrerro et al.13
Sinclair et al.4 demonstrated that plasma volume aug-
* P ⬍ 0.05 Fisher exact test.
mentation in patients undergoing open reduction of a
Acute renal dysfunction ⫽ presence of oliguria (⬍ 500 ml/day), increased
femur fracture was associated with significantly faster
serum creatinine (30% from preoperative value); Respiratory support ⫽ me-chanical ventilation or continuous positive airway pressure; Cardiovascular ⫽
recovery, with a reduction in the median time to being
hypotension requiring pharmacologic therapy, arrhythmias requiring pharma-
medically fit for discharge from 15 to 10 days, compared
cologic therapy or cardiogenic pulmonary edema; Chest infection ⫽ clinical
with a control group. In another study, Mythen and
diagnosis accompanied by an increase in leukocyte count above the normalrange; PONV ⫽ postoperative nausea or vomiting; Coagulopathy ⫽ platelet
Webb3 demonstrated that esophageal Doppler-guided
count ⬍ 100,000/l, prothrombin time ⬎ 1.5 times control, activated partial
plasma volume augmentation significantly reduced the
thromboplastin time ⬎ 1.5 times control, and/or fibrinogen ⬍ 100 mg/dl;
incidence of gastric mucosal hypoperfusion (56% to 7%)
Wound infection ⫽ clinical diagnosis, positive wound culture results, or in-crease in leukocyte count.
with significantly reduced complication rates and length
Anesthesiology, V 97, No 4, Oct 2002
GOAL-DIRECTED FLUID ADMINISTRATION REDUCES HOSPITAL STAY
of hospital stay following cardiac surgery. No patients in
as we wanted the control group to simulate as close as
the treatment group developed major complications
possible to receive "standard of care." Hence, the differ-
compared with six in the control group. The mean
ences between the groups could be attributed to the
hospital stay was also shorter in the treatment group
differences in the type of fluids administered. While
(6.4 vs. 10.1 days; P ⫽ 0.01). This improvement in
there were five more females in the control group com-
outcome could potentially reduce healthcare costs. The
pared with the protocol group, these differences were
results from these two studies are consistent with our
not statistically significant. The overall difference in hos-
findings and suggest that proactive intraoperative fluid
pital length of stay between the groups was admittedly
administration can improve postoperative recovery in
small, a difference of 1 day (median) or 2 days (mean).
patients undergoing moderate- to high-risk surgery.
These differences could be a result of unidentified group
However, this study does not address if optimal fluid
differences and factors other than goal-directed fluid
administration without the EDM would result in similar
benefits. This requires further investigation. Neverthe-
In summary, for patients undergoing moderate- and
less, intraoperative fluid augmentation appears to confer
high-risk surgery, goal-directed fluid administration with
significant benefits compared with customary practice.
6% hetastarch is associated with improved patient out-
In the current study, we have also demonstrated that
come and a slight reduction in the length of hospital
routinely measured standard cardiovascular variables
such as blood pressure, heart rate, and oxygen saturationwere unreliable indicators of mild hypovolemia. This has
been previously demonstrated.3,4 The immediate re-sponse to a reduction in circulating blood volume is
1. Boyd O, Bennett ED: Achieving the goal. Crit Care Med 1999; 27:2298 –92. Mythen MG, Webb AR: Intra-operative gut mucosal hypoperfusion is asso-
redirection of blood flow from less vital organs, e.g.,
ciated with increased post-operative complications and cost. Intensive Care Med
splanchnic bed, in favor of organs that are more sensitive
1994; 20:99 –104
3. Mythen MG, Webb AR: Perioperative plasma volume expansion reduces the
to ischemia.21 The measurement of normal central ve-
incidence of gut mucosal hypoperfusion during cardiac surgery. Arch Surg 1995;
nous pressure or pulmonary arterial occlusion pressure
4. Sinclair S, James S, Singer M: Intraoperative intravascular volume optimisa-
will not exclude hypovolemia unless the response to a
tion and length of hospital stay after repair of proximal femoral fracture: Ran-
fluid challenge is considered.22 Baek et al.23 found that
domised controlled trial. BMJ 1997; 315:909 –12
5. Gan TJ, Arrowsmith JE: The oesophageal Doppler monitor (editorial). BMJ
more than half of a group of high-risk postoperative
1997; 315:893– 4
patients developed a decrease in central venous pressure
6. Singer M: Esophageal Doppler monitoring of aortic blood flow: Beat-by-beat
cardiac output monitoring. Int Anesthesiol Clin 1993; 31:99 –125
and pulmonary arterial occlusion pressure in response to
7. Mark JB, Steinbrook RA, Gugino LD, Maddi R, Hartwell B, Shemin R, Disesa
plasma volume expansion. While we only studied pa-
V, Rida WN: Continuous noninvasive monitoring of cardiac output with esoph-ageal doppler ultrasound during cardiac surgery. Anesth Analg 1986; 65:1013–20
tients with no known history of congestive cardiac fail-
8. DiCorte CJ, Latham P, Greilich P, Cooley MV, Grayburn PA, Jessen ME:
ure, it would not be possible to speculate if fluid admin-
Esophageal doppler monitor determintion of cardiac output and preload duringcardiac operations. Ann Thorac Surg 2000; 69:1782– 6
istration guided by EDM would have a detrimental effect
9. Singer M, Bennett ED: Noninvasive optimization of left ventricular filling
on patients with compromised myocardial function or
using esophageal Doppler. Crit Care Med 1991; 19:1132–7
10. Klotz KF, Klingsiek S, Singer M, Wenk H, Eleftheriadis S, Kuppe H,
Schmucker P: Continuous measurement of cardiac output during aortic cross-
There are limitations in this study. While the data were
clamping by the oesophageal Doppler monitor ODM 1. Br J Anaesth 1995;74:655– 60
collected by independent dedicated research personnel
11. Penny JA, Anthony J, Shennan AH, deSwiet M, Singer M: Acomparison of
not involved in the intraoperative management of pa-
hemodynamic data derived by pulmonary artery floatation catheter and theesophageal Doppler monitor in pre-eclampsia. Am J Obstet Gynecol 2000; 183:
tients, we were unable to blind the anesthesiologists as
to the treatment group, and hence may have introduced
12. Singer M, Allen MJ, Webb AR, Bennett ED: Effects of alterations in left
ventricular filling, contractility and systemic vascular resistance on the ascending
bias. However, intraoperative fluid administration in
aortic blood flow velocity waveform of normal subjects. Crit Care Med 1991;
both groups was guided by specific fluid administration
13. Bennett-Guerrero E, Welsby I, Dunn TJ, Young LR, Wahl TA, Diers TL,
protocols, which should minimize bias. It is conceivable
Phillips-Bute BG, Newman MF, Mythen MG: The use of a postoperative morbidity
that the use of certain medications intraoperatively as
survey to evaluate patients with prolonged hospitalization after routine, moder-ate-risk, elective surgery. Anesth Analg 1999; 89:514 –9
well as postoperatively may have influenced bowel func-
14. Anonymous: Practice guidelines for preoperative fasting and the use of
tion (i.e., postoperative epidural analgesia, intraopera-
pharmacologic agents to reduce the risk of pulmonary aspiration: Application tohealthy patients undergoing elective procedures. A report by the American
tive nitrous oxide, and postoperative opioid). Nitrous
Society of Anesthesiologist Task Force on Preoperative Fasting. ANESTHESIOLOGY
oxide was used in all patients. There was no difference
1999; 90:896 –905
15. Yogendran S, Asokumar B, Cheng DC, Chung F: A prospective randomized
in the number of patients who received epidural or
double-blinded study of the effect of intravenous fluid therapy on adverse
patient-controlled analgesia between the groups, and the
outcomes on outpatient surgery. Anesth Analg 1995; 80:682– 6
16. Mythen MG, Webb AR: The role of gut mucosal hypoperfusion in the
pain scores and opioid use were similar. All patients
pathogenesis of post-operative organ dysfunction. Intensive Care Med 1994;
were visited daily in the postoperative period, and all
17. Connors AF Jr, Speroff T, Dawson NV, Thomas C, Harrell FE Jr, Wagner D,
adverse events were systematically collected. Patients in
Desbiens N, Goldman L, Wu AW, Califf RM, Fulkerson WJ Jr, Vidaillet H, Broste
the protocol group also received, on average, larger
S, Bellamy P, Lynn J, Knaus WA: The effectiveness of right heart catheterizationin the initial care of critically ill patients. SUPPORT Investigators. JAMA 1996;
volumes of hetastarch compared with the control group,
Anesthesiology, V 97, No 4, Oct 2002
GAN ET AL.
18. Anonymous: Pulmonary Artery Catheter Consensus conference: Consen-
21. Price HL, Deutsch S, Marshall BE, Stephen GW, Behar MG, Neufeld GR:
sus statement. Crit Care Med 1997; 25:910 –25
Hemodynamic and metabolic effects of hemorrhage in man with particular
19. LeFrant JY, Bruelle P, Aya AGM, Saïssi G, Dauzat M, de La Coussaye JE,
reference to the splanchnic circulation. Circ Res 1966; 18:469 –74
Eledjam JJ: Training is required to improve the reliability of esophageal Doppler
22. Weil MH, Shubin H, Rosoff L: Fluid repletion in circulatory shock. JAMA
to measure cardiac output in critically ill patients. Intensive Care Med 1998;
1965; 192:668 –74
23. Baek SM, Makabali G, Byron-Brown CW, Kusek JM, Shoemaker WC: Plasma
20. Madan AK, UyBarreta VV, Aliabadi-Wahle S, Jesperson R, Hartz RS, Flint
LM, Steinberg SM: Esophageal Doppler ultrasound monitor versus pulmonary
expansion in surgical patients with high central venous pressure: The relatioship
artery catheter in the hemodynamic management of critically ill surgical patients.
of blood volume to hematocrit, CVP, pulmonary wedge pressure, and cardiore-
J Trauma Inj Infect Crit Care 1999; 46:607–11; discussion 611–2
spiratory changes. Surgery 1975; 78:304 –15
Anesthesiology, V 97, No 4, Oct 2002
Source: http://www.conmedlinvatec.ae/Patient%20Care%20PDF/Gan_Goal_directed_Intraoperative_Fluid_Administration.12.pdf
Behavior Research Methods The final publication is available at Springer via http://dx.doi.org/10.3758/s13428-014-0536-1 Spontaneous facial expression in unscripted social interactions can be measured automatically Jeffrey M. Girard University of Pittsburgh University of Pittsburgh Carnegie Mellon University Michael A. Sayette Carnegie Mellon University University of Pittsburgh
MESTIZO ARTS PLATFORM Mestizo Arts Platform (MAP): Innovación y investigación artística en ciudades como Amberes, Malinas, Gante, Turnhout (Bélgica), Rotterdam (Holanda), Buenos Aires y México DF. Una nueva corriente de artistas que tienen la mirada hacia el mundo entero. Una mezcla de teatro, baile, videoarte, etc. MAP va en busca de todo lo que se mueve en las ciudades a través de proyectos como Los Viernes MAF, BRAINS, MAPping, Studio Urbanization y Work in Progress. Todo este movimiento artístico fluye hasta juntarse en el anual Mestizo Arts Festival en octubre. MAP es un proyecto de Fiëbre, una asociación cultural y artística belga que tiene como punto de partida el mestizaje de culturas y disciplinas de arte, siempre buscando nuevas perspectivas, formas de presentación y de interpretación. Fiëbre organizó el primer Mestizo Arts Festival (entonces llamado Mestizo Club) en 2007. MAP fue creado en 2015 para juntar todos las iniciativas de Fiëbre en un concepto total. La riqueza de las ciudades nuevas en evolución contínua. Vivimos en un momento emocionante de la historia. Personas de todas partes se encuentran y conviven en un espacio geográfico compartido: la ciudad. Al mismo tiempo nuevas tecnologías les permiten de comunicar de forma constante con los paises de origen. Todo eso da una riqueza abundante de información y historias en las ciudades. "El Mestizo Arts Platform es como un atlas de aventura de nuestras ciudades híperdiversas. Al vagar por el laberinto que es la ciudad encontramos artistas con raíces en sus calles efervescentes que musan sobre qué significa para ellos la ciudad. MAP es una declaración de amor a la ciudad." Plataforma y festival artístico multidisciplinario. MAP es una plataforma para el intercambio de estrategias e impulsos creativos de artistas y compañías nacionales e internacionales. Con MAP queremos ofrecer un podio que refleja la contínua evolución de las ciudades, mediante conceptos y proyectos, presentaciones y coproducciones que representan nuestra visión innovadora acerca del arte urbano. "Proclamamos el arte, en todo tipo de voces y lenguas. Así reverbera en nuestras calles efervescentes donde brilla con orgullo y donde se oye artistas de diversas disciplinas que rinden honor a lo maravilloso y lo fuerte que es la ciudad." La mezcla, el encuentro y la polinización. Partimos de una mezcla rica (‘mestizo') de y un diálogo entre las formas de arte, las culturas, las organizaciones, los artistas y el público. Nos gusta ir hasta los límites de lo desconocido. "Buscamos una lengua en común, meneamos como locos entre registros y intermediamos como traductores entre las visiones del mundo. Los artistas te cuentan como ellos miran hacia la ciudad y te invitan a abrir la perspectiva." Communidad y cooperación. Más de 150 artistas y más de 50 socios dan su voz para celebrar con nosotros la riqueza cultural de las ciudades. Construimos puentes y reenforzamos vínculos entre artistas, casas culturales, asociaciones fuera del mundo artístico y, claro, los habitantes de la ciudad. "Te dio curiosidad? Pónte pues las botas en los pies, los binoculares en la nuca y abastécete de provisiones. No te asústes! El mugido y rugido intimidante de la ciudad requiere coraje y perseverancia. Pero, te rogamos: atrévete! Y crece con la ciudad. Sube a