Levitra enthält Vardenafil, das eine kürzere Wirkdauer als Tadalafil hat, dafür aber schnell einsetzt. Männer, die diskret bestellen möchten, suchen häufig nach levitra kaufen ohne rezept. Dabei spielt die rechtliche Lage in der Schweiz eine wichtige Rolle.
Dentalbooks.bg
Contemporary Restoration of
TREATED TEETH
Evidence-Based Diagnosis and Treatment Planning
Nadim Z. Baba, dmd, msdProfessor of Restorative DentistryDirectorHugh Love Center for Research and Education in TechnologyLoma Linda University School of DentistryLoma Linda, California
Quintessence Publishing Co, IncChicago, Berlin, Tokyo, London, Paris, Milan, Barcelona, Beijing,Istanbul, Moscow, New Delhi, Prague, São Paulo, Seoul, Singapore, and Warsaw
Foreword viiPreface viiiContributors ix
Part I: Treatment Planning for Endodontically Treated Teeth
Impact of Outcomes Data on Diagnosis and Treatment Planning
3
1
Charles J. Goodacre and W. Patrick Naylor
Treatment Planning Considerations for Endodontically Treated Teeth
19
2
Robert A. Handysides and Leif K. Bakland
Treatment Options and Materials for Endodontically Treated Teeth
33
3
Nadim Z. Baba and Charles J. Goodacre
Part II: Methods of Restoration for Endodontically Treated
Principles for Restoration of Endodontically Treated Teeth
61
4
Nadim Z. Baba, Charles J. Goodacre, and Fahad A. Al-Harbi
Cementation of Posts and Provisional Restoration
75
5
Faysal G. Succaria and Steven M. Morgano
Tooth Whitening and Management of Discolored Endodontically
6 Treated Teeth
91
Part III: Management of Severely Damaged Endodontically
Crown Lengthening
107
7
Nikola Angelov
Preprosthetic Orthodontic Tooth Eruption
115
8
Joseph G. Ghafari
Intra-alveolar Transplantation
127
9
Antoanela Garbacea, Nadim Z. Baba, and Jaime L. Lozada
Autotransplantation and Replantation
137
10
Leif K. Bakland and Mitsuhiro Tsukiboshi
Osseointegrated Dental Implants
149
11
Juan Mesquida, Aladdin J. Al-Ardah, Hugo Campos Leitão, Jaime L. Lozada,
and Aina Mesquida
Part IV: Treatment of Complications and Failures
Repair of Perforations in Endodontically Treated Teeth
167
12
George Bogen, C. John Munce, and Nicholas Chandler
Removal of Posts
181
13
Ronald Forde, Nadim Z. Baba, and Balsam Jekki
Removal of Broken Instruments from the Root Canal System
195
14
David E. Jaramillo
Endodontic Treatment of a Tooth with a Prosthetic Crown
201
15
Mathew T. Kattadiyil
Retrofitting a Post to an Existing Crown
207
16
Nadim Z. Baba, Tony Daher, and Rami Jekki
It is an honor to have been invited to write the foreword
Dentists encountering treatment planning dilemmas, such
for Dr Nadim Baba's text on the restoration of endodonti-
as determining when to extract a compromised tooth and
cally treated teeth. The last book on this topic, published by
when to retain it and restore it, can find the answers to most
Quintessence, was authored by Shillingburg and Kessler in
of their questions in this first-rate text. Traditional principles
1982. Three decades later, this new book is much needed
and techniques are reviewed and reinforced, along with
and long overdue.
modern materials and methods, all with a firm foundation
Dr Baba's interest in the restoration of pulpless teeth
in the best available scientific evidence and with an em-
dates back to his graduate-school days. I served as his
phasis on clinical studies. Many of the chapters provide
program director and his principal research advisor during
comprehensive, step-by-step descriptions of technical pro-
his studies at Boston University in the postdoctoral pros-
cedures with accompanying illustrations to guide the read-
thodontic program, where the title of his master's project
er through all aspects of restoring pulpless teeth, including
and thesis was "The Effect of Eugenol and Non-eugenol
fabrication of various foundation restorations, cementation
Endodontic Sealers on the Retention of Three Prefabricated
techniques, and methods of provisionalization of endodon-
Posts Cemented with a Resin Composite Cement." Dr Baba
tically treated teeth. Preprosthetic adjunctive procedures,
certainly has come a long way since receiving his certifi-
such as surgical crown lengthening, repair of perforations,
cate of advanced graduate study and master of science in
and orthodontic measures, are also described and illus-
dentistry degree in 1999. He is now a Diplomate of the
American Board of Prosthodontics and a full professor at
Dr Baba has assembled a group of renowned experts on
Loma Linda University School of Dentistry, and he is about
various topics related to the restoration of pulpless teeth,
to publish this comprehensive book on the restoration of
and these experts have collectively produced this outstand-
endodontically treated teeth.
ing text, which will remain a definitive reference for years
This new text has a wealth of evidence-based information
to come. The profession as a whole is very fortunate to
on all facets of restoration of endodontically treated teeth
have this text. Many thanks must go to Dr Baba for under-
and will serve as an indispensable reference not only for
taking this monumental task and to all contributing authors
dentists involved in the restoration of pulpless teeth, such
for their time and efforts in helping Dr Baba produce this
as general practitioners and prosthodontists, but also for
new book on such a very important subject.
dentists who do not place restorations but are engaged in
planning treatment for structurally compromised teeth, such
as endodontists, periodontists, and oral surgeons. With
Steven M. Morgano, dmd
the well-documented success of osseointegrated implant-
Professor of Restorative Sciences and Biomaterials
supported fixed restorations, combined with a better un-
Director, Division of Postdoctoral Prosthodontics
derstanding of the factors that can influence the prognosis
Boston University Henry M. Goldman School of Dental
of severely broken down teeth, the profession's approach
to planning treatment for these teeth has evolved, and this
Boston, Massachusetts
text offers a well-balanced, contemporary approach to the
topic of treatment planning.
My interest in the restoration of endodontically treated
teeth dates back to my graduate-school days at Boston Uni-
versity. When working on my master's project and thesis
and later while studying for the American Board of Pros-
I wish to express my appreciation and indebtedness to
thodontics exam, I realized that very few books dealt with
all my friends and colleagues who contributed chapters,
the restoration of pulpless teeth. The first book on that topic
sections of chapters, or clinical cases in specific areas in
was published by Quintessence in 1982; two decades
which they are experts. Without them the book would not
later, three books were published but all were somewhat
have been possible.
limited in their scope. They dealt mainly with fiber posts,
I would like to take the opportunity to thank Leif Bakland,
their characteristics, and their clinical applications.
Zouheir Salamoun, W. Patrick Naylor, and the dean of
This book is primarily intended to be a manuscript that
my school, Loma Linda University, Charles J. Goodacre,
reviews the basic principles of diagnosis and treatment
for their counsel and help during the preparation of the
planning and describes numerous treatment options and
the techniques recommended for contemporary treatment
Most importantly, I extend my special thanks to Ms Lisa
of endodontically treated teeth. The purpose of this book is
Bywaters and the staff of Quintessence Publishing for their
to provide general dentists, endodontists, prosthodontists,
professionalism and guidance in bringing my book to life.
and dental students (postgraduate and predoctoral) with a
I also would like to acknowledge my teachers and men-
comprehensive review of the literature and evidence-based
tors who had a great impact on my visions, attitude, and
information for the treatment of endodontically treated
career: Pierre Boudrias, Hideo Yamamoto, Steven M. Mor-
teeth, keeping in mind the integration of systematic assess-
gano, David Baraban (deceased), and Charles J. Goodacre.
ments of clinically relevant scientific evidence.
They remind me of the Lebanese-American poet and writer
Four major themes are discussed. The first part focuses
Gibran Khalil Gibran, who said: "The teacher who is indeed
on treatment planning, treatment options, and materials
wise does not bid you to enter the house of his wisdom but
used for the restoration of endodontically treated teeth. The
rather leads you to the threshold of your mind."
second part reviews the principles and methods of restora-
I feel blessed, lucky, and proud to have had the chance
tion along with cementation, provisional restoration, and
to know and work with each one of these people in various
management of discolored endodontically treated teeth.
stages of my professional career.
The third part describes the different aspects of the man-
agement of severely damaged pulpless teeth. In the final
part, treatment of complications and failures is reported.
Aladdin J. Al-Ardah, dds, ms
Nicholas Chandler, bds, msc, phd
Assistant Professor
Associate Professor of Endodontics
Advanced Education Program in Implant Dentistry
University of Otago School of Dentistry
Loma Linda University School of Dentistry
Dundin, New Zealand
Loma Linda, California
Tony Daher, dds, msed
Fahad A. Al-Harbi, bds, msd, dscd
Associate Professor of Restorative Dentistry
Dean and Assistant Professor
Loma Linda University School of Dentistry
College of Dentistry
Loma Linda, California
University of Dammam
Dammam, Saudi Arabia
University of California at Los Angeles
Nikola Angelov, dds, ms, phd
Los Angeles, California
Professor and Director
Predoctoral Program in Periodontics
Ronald Forde, dds, ms
Loma Linda University School of Dentistry
Chair and Assistant Professor of Restorative Dentistry
Loma Linda, California
Loma Linda University School of Dentistry
Loma Linda, California
Nadim Z. Baba, dmd, msd
Professor of Restorative Dentistry
Antoanela Garbacea, dds
Hugh Love Center for Research and Education in Technology
Santa Rosa, California
Loma Linda University School of Dentistry
Loma Linda, California
Joseph G. Ghafari, dmd
Head and Professor
Leif K. Bakland, dds
Division of Orthodontics and Dentofacial Orthopedics
Ronald E. Buell Professor of Endodontics
Department of Otolaryngology, Head and Neck Surgery
Loma Linda University School of Dentistry
American University of Beirut Medical Center
Loma Linda, California
George Bogen, dds
Professor of Orthodontics
Private practice limited to endodontics
Lebanese University School of Dentistry
Los Angeles, California
Adjunct Professor of Orthodontics
New York University College of Dentistry
New York, New York
Charles J. Goodacre, dds, msd
Aina Mesquida, dds
Dean and Professor of Restorative Dentistry
Loma Linda University School of Dentistry
Advanced Education Program in Implant Dentistry
Loma Linda, California
Loma Linda University School of Dentistry
Loma Linda, California
Robert A. Handysides, dds
Chair and Associate Professor of Endodontics
Juan Mesquida, dds
Loma Linda University School of Dentistry
Assistant Professor
Loma Linda, California
Advanced Education Program in Implant Dentistry
Loma Linda University School of Dentistry
David E. Jaramillo, dds
Loma Linda, California
Clinic Director and Associate Professor of Endodontics
Loma Linda University School of Dentistry
Steven M. Morgano, dmd
Loma Linda, California
Professor of Restorative Sciences and Biomaterials
Balsam F. Jekki, bds
Division of Postdoctoral Prosthodontics
Assistant Professor of Restorative Dentistry
Boston University Henry M. Goldman School of Dental
Loma Linda University School of Dentistry
Loma Linda, California
Boston, Massachusetts
Rami Jekki, dds
C. John Munce, dds
Assistant Professor of Restorative Dentistry
Assistant Professor of Endodontics
Loma Linda University School of Dentistry
Loma Linda University School of Dentistry
Loma Linda, California
Loma Linda, California
Mathew T. Kattadiyil, dds, mds, ms
Assistant Professor of Endodontics
Associate Professor of Restorative Dentistry
University of Southern California Ostrow School of
Advanced Specialty Education Program in Prosthodontics
Los Angeles, California
Loma Linda University School of Dentistry
Loma Linda, California
W. Patrick Naylor, dds, mph, ms
Hugo Campos Leitão, dmd, msd
Advanced Dental Education
Assistant Professor in Periodontics
Professor of Restorative Dentistry
Universitat Internacional de Catalunya
Loma Linda University School of Dentistry
Loma Linda, California
Yiming Li, dds, msd, phd
Faysal G. Succaria, dds, msd
Professor of Restorative Dentistry
Chair and Assistant Professor
Department of Prosthodontics
Center for Dental Research
Boston University Institute for Dental Research and
Loma Linda University School of Dentistry
Loma Linda, California
Dubai, United Arab Emirates
Jaime L. Lozada, dmd
Mitsuhiro Tsukiboshi, dds, phd
Professor and Director
Advanced Education Program in Implant Dentistry
Tsukiboshi Dental Clinic
Loma Linda University School of Dentistry
Loma Linda, California


Treatment Planning for
Endodontical y Treated Teeth
Impact of Outcomes Data on
1. Diagnosis and Treatment Planning
Treatment Planning Considerations
2. for Endodontically Treated Teeth3. Treatment Options and Materials
for Endodontically Treated Teeth

2 Treatment Planning Considerations for Endodontically Treated Teeth
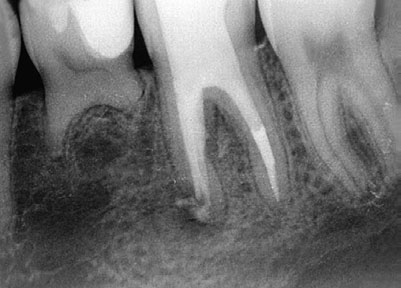
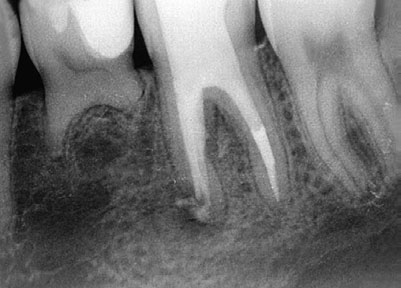
Fig 2-4 (a) The complexity of the root canal system is well illustrated in these sections of maxillary molars. Note the variety of canal configurations
in the mesiobuccal roots and in particular the location of the second mesiobuccal canal in the molar on the right. (b) A radiograph of a maxillary
molar seems to show two palatal roots (arrows). (c) On the patient's request, the tooth was extracted; two palatal roots were identified (arrows).
In addition, Schilder12 named four biologic objectives for
Assessment of other conditions
these preparations:
1. Treatment procedures are confined to the roots.
2. Necrotic debris is not forced beyond the apical foram-
Fracture lines involving cusps of teeth have been a prob-
lem in dentistry, probably throughout human history. The
3. All pulp tissues are removed from the root canal space.
pain associated with such fracture lines was described by
4. Sufficient space exists for intracanal medicaments and
Gibbs,16 who termed it cuspal fracture odontalgia. Every
dentist has probably had a patient who complains about
pain on chewing and later shows up with the broken-off
These objectives provide a basis for assessing the qual-
cusp, usually from a premolar tooth. Whether or not the
ity of the endodontic procedure prior to restoration of the
pulp is directly involved (by exposure), it is usually neces-
tooth. Deviation from the original canal shape is referred to
sary to complete RCT before the tooth is restored. Diagno-
as transportation of the canal. The greater the transporta-
sis of a fracture line under a cusp, before it breaks off, can
tion, the greater the likelihood of a poor endodontic out-
be a challenge and will be discussed in the next section on
come, resulting in the need for either endodontic retreat-
ment or extraction of the tooth.
Teeth may develop cracks and fracture for a number of
reasons, including trauma, excessive masticatory forces,
Root canal systems
and iatrogenic incidents. Regardless of etiology, when
cracks or fractures develop in dental hard tissues it is not
The root canal system is complex (Fig 2-4), and its anatomy
possible to repair them, except for a short period of time
has been studied extensively for many years. Of special
with bonding agents. In contrast, bone and cartilage rou-
interest in the current context, Weine et al13 called atten-
tinely undergo repair following fracture. Although tooth
tion to the frequent presence of two canals in the mesio-
fractures and cracks cannot be healed, it is possible in
buccal roots of maxillary molars. Pineda and Kuttler14
many cases to maintain such teeth for various periods of
and Vertucci15 developed classification systems for canal
time following identification and diagnosis.
configurations in individual roots. Research in root canal
For convenience in discussing cracks and fractures, three
morphology has led to descriptions of more than 20 canal
categories will be used: enamel craze lines, infractions,
and vertical root fractures (VRFs).
These considerations are important for the evaluation of
a tooth that has undergone RCT. They also point to the chal-
Enamel craze lines. Craze lines are small cracks that are
lenges inherent to treating teeth with endodontic disease
confined to the enamel of teeth (Fig 2-5). They are not typi-
prior to restoration to full function. Achieving full function
cally visible unless light rays highlight them incidentally.
requires that the treatment-planning process be a teamwork
They develop over time, so they probably can be found in
process: RCT can be performed on almost any tooth, but
most teeth eventually. Occasionally they will show stains
restorability must be determined prior to the endodontic
from exposure to liquids such as coffee and red wine. Be-
component of treatment. Communication among the vari-
cause these cracks are confined to enamel, they have no
ous treating dentists before, during, and after RCT offers
pulpal impact, and no treatment is necessary, except op-
the best possibility of an optimal outcome.

Diagnosis and Treatment Planning
Fig 2-5 Enamel craze lines (arrow) are common and pre-
Fig 2-6 (a) Infractions (arrow) can be identified visually with the help of dyes, in
sent no particular problem other than their potential for
this case a red dye. Infractions usually run in a mesiodistal direction; they may be
asymptomatic or associated with pain on chewing and cold stimuli. (b) A tooth
extracted because of symptoms associated with an infraction shows the presence of
the infraction (arrow). They typically originate in the crown of the tooth and pro-
gress in an apical direction. (c) On rare occasions, infractions run in a faciolingual
tional bleaching if they are stained. There is no evidence
that can mimic trigeminal neuralgia; chronic orofacial pain
that craze lines progress to involve more than enamel.
can also develop. The wide range of pain experiences is
probably why Cameron18 used the term syndrome to de-
Infractions (cracked teeth). The term cracked tooth is com-
scribe this dental situation. The etiology of infractions is
monly used to describe a tooth that has developed an
probably in most cases related to occlusal forces, whether
infraction, which is defined as "a fracture of hard tissue
from regular daily chewing or isolated trauma such as
in which the parts have not separated"17 (Fig 2-6). Cam-
blows to the underside of the mandible.19–25
eron18 incorrectly defined this condition as cracked tooth
It is likely that teeth with infractions become symptomatic
syndrome; the use of syndrome is not appropriate for pain
when the infractions become invaded by bacteria26 (Fig
associated with fractures in teeth. It is, however, a situation
2-7). Bacteria stimulate inflammation in the pulp, whether
with a variety of symptoms, and diagnosis can be very
or not the infraction communicates directly with the pulp tis-
sue. The inflamed tissue is responsible for the exaggerated
Mandibular molars and maxillary molars and premo-
cold response. It is also likely that the tooth will become
lars are the teeth most frequently associated with infrac-
sensitive to biting when the infraction progresses from the
tions. The teeth usually have vital pulps and the infractions
tooth crown to the root, and the bacteria that will soon
typically run in a mesiodistal direction. They begin in the
occupy the infraction then stimulate an inflammatory re-
crowns of teeth and progress in an apical direction. Not all
sponse in the adjacent periodontal ligament (PDL).
teeth with infractions are symptomatic, but when symptoms
Diagnosis of infractions is complicated by many factors.
develop they can range from pain on chewing, to an exag-
Because infractions are usually located in a mesiodistal di-
gerated response to cold stimuli, to severe pain episodes
rection in the crown, they are not visible on radiographs.
3 Treatment Options and Materials for Endodontically Treated Teeth
Fig 3-17 (a and b) A provisional fixed dental prosthesis is fabricated in resin composite material. The restoration has proper contours, thickness,
proximal contacts, and adequate occlusal contacts. (c) Gutta-percha is removed from the orifice of the canals to aid in retention of the core. (d) A
carbide rotary cutting instrument is used to make an occlusal access opening on the provisional prosthesis, toward the center of the foundation. (e)
The FPD is cemented, and the amalgam is condensed in the prepared post spaces. (f and g) A tapered rotary cutting instrument is used carefully
to make a vertical groove in the lingual surface in order to section the provisional prosthesis. (h and i) The amalgam foundation is refined for the
definitive tooth preparation, and a final impression is taken.
3. Remove 1 to 2 mm of gutta-percha from the orifice of
endodontic plugger. Fill the remaining pulp chamber
the canals to aid in retention of the core. This is only
with amalgam up to the occlusal surface of the pro-
necessary when the pulp chamber is smaller than 3
visional FPD to ensure an adequate seal, and make
mm in depth (Fig 3-17c).
occlusal adjustments as needed (Fig 3-17e).
4. Use a carbide rotary cutting instrument to make an oc-
9. At the following appointment, carefully section the pro-
clusal access opening in the abutment retainer toward
visional FPD by using a tapered rotary cutting instru-
the center of the foundation.
ment to make a vertical groove in the buccal surface
5. Place the modified provisional FPD on the remaining
(Figs 3-17f and 3-17g).
tooth structure, and confirm adequate access to the
10. Refine the amalgam foundation for the definitive tooth
cavity for ideal amalgam placement and condensation
preparation, and take the definitive impression (Figs
(Fig 3-17d).
3-17h and 3-17i).
6. Confirm proper fit and marginal adaptation of the pro-
11. Fabricate and cement a new provisional FPD with pro-
visional FPD.
visional cement.
7. Cement the modified provisional FPD with a small
amount of provisional cement placed only on the mar-
The same procedure is used when a provisional crown is
gins of the provisional FPD.
used as a matrix for an amalgam core buildup (Fig 3-18).
8. Condense the first increments of amalgam into the pre-
pared post spaces using a periodontal probe or an
Types of Posts and Cores
Fig 3-18 (a) The mandibular right first molar was endodontically treated and presented with enough remaining coronal tooth structure and adequate
depth of the pulpal chamber. (b) Tooth preparation is finished, and the post space is prepared in the distal canal to receive a prefabricated metallic
post. (c) The provisional crown is fabricated using resin material with proper contours, thickness, proximal contact, and adequate occlusal contacts.
(d) An occlusal access opening in the provisional crown is made so only a peripheral shell of resin is retained using a carbide rotary cutting
instrument. The provisional crown is cemented with a luting agent. The length of the prefabricated post is adjusted to the appropriate height, and
the post is cemented with zinc phosphate cement. (e) The amalgam is condensed into the prepared post space. (f and g) After the amalgam has
hardened or at a subsequent appointment, the provisional crown is sectioned carefully by making a vertical groove in the labial surface using
a tapered rotary cutting instrument. (h) The amalgam foundation is refined for the definitive tooth preparation, and a final impression is taken.
(Courtesy of Dr Carlos E. Sabrosa, Rio de Janeiro, Brazil.)
Composite resin
Oliva and Lowe255 found that composite resin cores were
not dimensionally stable when exposed to moisture. How-
Composite resin is a popular core material because it is
ever, Vermilyea et al257 found that the use of a well-fitting
easy to use and satisfies esthetic demands. Certain proper-
provisional restoration will provide the composite resin
ties of composite resins are inferior to those of amalgam
core with some degree of moisture protection. Hygroscopic
but superior to glass-ionomer materials.234,247 Kovarik et al234
expansion of composite resin cores and cements in layered
showed that composite resin is more flexible than amal-
structures with an overlying ceramic layer can generate sig-
gam. It adheres to tooth structure, may be prepared and
nificant stresses that have the potential to cause extensive
finished immediately, and has good color under all-ceramic
cracking in the overlying ceramic layer. Clinically, this im-
crowns. Composite resin appears to be an acceptable
plies that all-ceramic crown performance may be compro-
core material when substantial coronal tooth structure re-
mised if the crowns are luted to composite cores that have
mains235,248–253 but a poor choice when a significant amount
undergone hygroscopic expansion.258
of tooth structure is missing.234,254
Another disadvantage is that composite resin is dimen-
One disadvantage of composite resin cores is the insta-
sionally unstable (setting shrinkage). Shrinkage during po-
bility of the material in oral fluids (water sorption).255,256
lymerization causes stress on the adhesive bond, resulting



CH 12 Repair of Perforations in Endodontically Treated Teeth
Fig 12-8 (a) Mandibular left first molar with a mesial root periapical radiolucency in a 13-year-old asymptomatic girl. The molar exhibits both strip
and apical perforations from previous root canal treatment. (b) Strip perforation visible under the DOM at the furcal side of the mesial root (arrow).
(c) Working length determination after removal of previous obturation material. (d) White MTA canal obturation to the level of the pulpal floor. (e)
Final radiograph of obturation and the fiber post and bonded core. (f) Radiograph at 7 years, showing the complete-coverage restoration and
complete periradicular healing. The patient is asymptomatic with the molar in full function. (Courtesy of Dr Marga Ree, Amsterdam.)
Fig 12-9 (a) Maxillary left second premolar in a symptomatic 24-year-old man with a suspected post perforation to the mesiobuccal root aspect.
Note the well-circumscribed periradicular radiolucency adjacent to the perforation. (b) Completed access through the metal-ceramic crown. The
coronal aspect of the post has been uncovered. (c) Post following removal. (d) Chamber after debridement of the perforation site and preparation
for MTA placement. (e) Immediate postoperative radiograph following MTA perforation repair and subsequent completion of nonsurgical endodon-
tic retreatment. (f) Ten-month radiographic review showing complete resolution of the periradicular pathosis. The patient is asymptomatic. (Courtesy
of Dr Ryan M. Jack, Colorado Springs, CO.)
Management of Perforations
Fig 12-10 (a) Mandibular left first molar in a symptomatic 32-year-old man. Note the presence of a separated file at the mesial root apex and
concomitant transportation and perforation of the mesial root canal during previous treatment. (b) Identification of the perforation site. (c) Canal
obturation with gray MTA. (d) Surgical resection of the mesial roots, removal of the separated file, and MTA retrofill. (e) Nine-month radiographic
review. (f) Three-year recall radiograph showing complete remineralization of the osteotomy site.
calcium hydroxide followed by placement of gutta-percha
Retrograde management of perforations
as a perforation repair and filling technique.5,128–132 MTA
can be placed with or without a matrix barrier; however,
The goal of surgical repair of root perforations is to pro-
root-end resection may be indicated if the original canal
vide a reliable seal so that bacteria and their by-products
is not accessible after the repair.11 Where apical surgery
are prevented from entering the periodontium through the
is not an option, advanced techniques can also provide
root canal system. This procedure should encourage an
dedicated channels for conventional obturation after MTA
environment that promotes regeneration of the damaged
placement and hardening.
periodontal tissues and maintains immune cell surveillance.
Hemorrhage at the perforation site can be challenging
The indications for surgical treatment include excessive ex-
when nonobservable subcrestal perforations are being pre-
trusion of the repair material, combination (orthograde and
pared apically or beyond the view of the DOM. Once the
retrograde) therapies, perforations inaccessible by nonsur-
perforation is identified, 1.25% to 6.0% NaOCl provides
gical means, and failure of nonsurgical repairs3,5,15,23,106
an environment that removes inflammatory tissue, controls
(Fig 12-10). The location of the perforation is the prime
hemorrhage, disinfects the perforation site, and conditions
determinant in the strategy and material used in the surgi-
the surrounding dentin.133–137 However, the solution must
cal approach.144
not be propelled into perforation areas because this can
According to Gutmann and Harrison,106 certain aspects
often cause severe tissue damage and paresthesia.138–143
of the case must be considered before surgical treatment
Sodium hypochlorite should always be delivered passively,
can be initiated:
using pipette carriers or cotton pellets, or placed in the pulp
chamber and gently transported along the main canal us-
• The amount of remaining bone and any surrounding os-
ing hand files, avoiding penetration at the wound site. The
solution may also be delivered by inserting a small suction
• The overall periodontal status
cannula into the canal beyond the perforation and then
• The duration and size of the defect
placing the liquid in the chamber to be passively drawn
• The surgical accessibility
into the canal to beyond the defect. If the perforation does
• The soft tissue attachment level
not include the main canal, then NaOCl is gently brought
• The patient's oral hygiene and medical status
to the limit of the defect interface and frequently replen-
• The surgeon's soft tissue management expertise
ished until hemostasis is achieved.
CH 13 Removal of Posts
Fig 13-3 (a) Schematic of a cast post and core that requires removal
for endodontic retreatment. (b) A rotary instrument is used to reduce
the diameter of the core. (c) The core is further reduced with a
Gonon bur. (d) The core is threaded with a Gonon trephine bur.
(e) A mandrel with a washer and cushions in place is threaded on
the post, and then the knurled knob is turned to remove the post.
(Courtesy of Dr Nadim Z. Baba, Loma Linda, CA.)
31-mm-long Endodontic
Cariesectomy Bur
Endodontic Shallow
shaft (0.7 mm) on the
#1/4, #1/2, & #1
Fig 13-4 Gonon post puller device.
Fig 13-5 Munce Discovery Burs (CJM Engineering).
Mechanical Devices
Fig 13-6 (a) Radiograph of a maxillary right lateral incisor with an apical lesion requiring the
removal of a cast post and core and endodontic retreatment. (b) The cast post and core is
isolated with rubber dam. (c) The cast post and core is shaped into a roughly cylindric shape. (d)
A Munce Discovery Shallow Troughers (CJM Engineering) is used to remove the cement around
the post. (e) A special bur is used to thread the head of the cast post and core. (f) Application
of counterclockwise rotational force using the wrench. (g) Gonon post in place and ready to be
used. (h) The screw is turned to open the jaws and create an extraction force. (i) Removal of post
and preservation of the tooth structure. (j) Postoperative radiograph showing the endodontically
retreated root canal and the definitive restoration. (Courtesy of Dr Marga Ree, Amsterdam.)
post to protect the tooth from the lifting action of the pliers
(Fig 13-6). Should the post be successfully removed at this
point, the retreatment of the tooth may proceed following
inspection of the root to verify its integrity.
The Gonon post removal system is less invasive then the
Masserann Kit and the LGPP and requires less removal of
tooth structure.11,38
Page numbers followed by "f" indicate fig-
ures; those followed by "t" indicate tables; Bacteria, 24f, 139
cast post and core, 80–82, 80f–82f
those followed by "b" indicate boxes
Balanced forces technique, 195
ferrule effect on, 84
Base metal alloy, 36
fiber-reinforced resin post, 82–83, 83f
intraradicular disinfection, 78, 78b
Abutment teeth, 4
description of, 127, 169
Acrylic resin provisional restorations, 84–85
implant placement and, 124f
post surface treatment, 79
Aluminum oxide, 79
orthodontic forced eruption and, 116,
provisional restorations, 86–87
Alveolar ridge, 123, 150–152
radicular dentin, 78–79
Amalgam cores, 48–50, 49f–50f
surgical crown lengthening and, 108–109
Amalgam restorations
tooth fracture effects on, 111f
techniques of, 78–84, 80f–83f
complete-crown restoration versus, 6
treatment modalities for maintaining,
voids created during, 79, 79f
discoloration caused by, 92
mercury release from, after tooth bleaching, Bis-acryl composite resin, 85
Cervical root resorption
Bite test, 24, 24f
intracoronal tooth bleaching as cause of,
Amelogenesis imperfecta, 93
Bleaching. See Tooth bleaching.
Bond strength, extracoronal bleaching effects
invasive, 29f, 29–30
Ankylosis-related root resorption, 28f, 29,
Cervical tooth structure, for ferrule, 68–69
Broken instruments
Chairside extracoronal bleaching, 100
Anterior teeth. See also specific teeth.
illustration of, 196f
Combined endodontic-periodontal
anchorage for, 118
prevalence of, 196
conditions, 26–27
endodontically treated
removal of, 181, 196–199
Complete-crown restoration, 6
complete coronal coverage in, 7
Complex amalgam restorations, 6
description of, 6–7
Composite resin cores, 51–52
restorations for, 8, 34–35
Calcium hydroxide-containing sealer, 77–78
Composite resin restorations
discoloration caused by, 92
Apical lesions, 20
Carbamide peroxide, 94–95
endodontically treated teeth, 5–6
Apical perforations, 169, 173
Carbon fiber–reinforced epoxy resin posts,
fracture resistance of, 35
Apical seal, 10, 63, 67
41–43, 41f–43f, 42t
At-home extracoronal bleaching, 100, 102
Cast posts and cores. See Custom cast posts
time until failure with, 5–6
Computer-aided design/computer-assisted
antibiotics use in, 139
definition of, 137
glass-ionomer, 76b, 76–77
Cone beam computed tomography, 141
dietary considerations, 139
polycarboxylate, 76
Core ferrules, 68
examples of, 137–138, 138f
post type and, 76b, 77
Cores. See Posts and cores.
general principles of, 139–141
properties of, 75, 76b–77b
Coronal teeth preparation, 66
molars, 141f–142f, 141–143
resin, 77, 79, 82–84
Coronal-coverage crowns
premolars, 143f, 143–144
resin-modified glass-ionomer, 77
anterior teeth, endodontically treated, 34
prognosis after, 140–141
ultrasonic post removal affected by, 191
posterior teeth, endodontically treated, 34
root resorption concerns, 139–140, 140f
zinc phosphate, 76, 76b
Cracked teeth, 22–26
Avulsed tooth, 138f, 144, 145f
Craze lines, 22–23, 23f, 70, 70f
Crestal perforations, 169, 171, 173, 174f
cuspal deflection of, 7–8
for orthodontic tooth movement, 121
flexibility of, 7
Forced eruption, orthodontic. See
crown-root ratio, 116–117, 124
fracture of, 4–5
Orthodontic forced eruption.
See also Orthodontic extrusion.
length of, post length correlation with,
moisture content in, 7, 35
root. See Root fracture.
prosthetic. See Prosthetic crown.
physical properties of, 7–8
tooth. See Tooth fractures.
Crown lengthening, surgical. See Surgical
posterior teeth. See Posterior teeth.
Free radicals, 95, 100
crown lengthening.
posts and cores effect on, 36
Furcation perforations, 169, 173
Crown-root fractures
proprioception of, 8
diagnosis of, 128
prosthetic crown, 201–205, 203f–204f
incidence of, 132
provisional restorations in, 87
Gates Glidden instruments, 11, 64
proximal contact of, 4
shear strength of, 8
augmentation of, 123
sound tooth structure, 14
excessive display of, 109f
Cuspal deflection, 7–8
survival rates for, 4, 20
irritation of, from tooth bleaching, 101
Cuspal fracture odontalgia, 22
time until failure, 5–6
postrestorative recession of, 155f
Custom cast posts and cores
ultrasonic vibration effects on, 192
treatment planning for. See Treatment
Gingival connective tissue, 192
cementation of, 80–82, 80f–82f
Glass fiber–reinforced epoxy resin posts,
direct fabrication technique for, 37–38,
vital teeth versus, 4
43f, 43–45, 44t, 45f
Epoxy resin posts
indications for, 37
carbon fiber–reinforced, 41f–43f, 41–43
core buildup material use of, 52
indirect fabrication technique for, 38–41
glass fiber–reinforced, 43f, 43–45, 44t,
silver alloys added to, 52
lost-wax technique, 36, 37f
Glass-ionomer cement, 76b, 76–77, 191
for posterior teeth with divergent roots,
Extracoronal bleaching
resin-modified, 77
at-home, 100, 102
surface treatment of, 79
Gonon post removal system, 183, 184f
zinc phosphate cementation of, 80–82,
dental professionals' role in, 101–102
enamel effects of, 101
apical seal and, 10, 63, 67
gingival irritation secondary to, 101
condensation of, 67f
in-office, 99f, 99–100
immediate versus delayed removal of,
restorations and, 101
risks associated with, 100–102
instruments for removal of, 67
Dental fluorosis, 93–94
tooth sensitivity secondary to, 100–101
removal of, 66–67, 67f
craze lines in, 70
orthodontic. See Orthodontic extrusion.
surgical. See Intra-alveolar transplantation.
post diameter effects on, 64
Hereditary hypophosphatemia, 93
residual thickness of, 11, 70–71
H O . See Hydrogen peroxide.
Hydrogen peroxide, 94–96, 100–102
thickness of, 11, 70–71
intra-alveolar transplantation for improving,
Dentogingival junction, 108
Idiopathic root resorption, 30, 30f
restoration retention affected by, 68f,
Immediate implant placement. See
Osseointegrated implants, immediate
Direct core materials, 48–52
surgical crown lengthening consideration
placement of.
Discoloration of teeth. See Tooth
osseointegrated. See Osseointegrated
Distofacial root, 13
cementation of, 77, 82–83, 83f
description of, 14–15
biologic width considerations, 124
self-adhesive resin cement for, 82–83, 83f
complications of, 159–160
Eggler post removal, 186, 187f–188f
surface treatment of, 79
in growing patients, 124, 125f
immediate, 123. See also
decalcification of, 93
Osseointegrated implants, immediate
extracoronal bleaching effects on, 101
Fixed partial dentures
placement of.
hypocalcification of, 93
provisional, modification into matrix for
hypoplasia of, 93
amalgam core buildup, 49–50, 50f
nerve injuries during, 159–160
Enamel craze lines, 22–23, 23f
survival rates for, 4–5
orthodontic extrusion effects on, 124
Endodontically treated teeth
Flapless crown lengthening, 112
postextraction, 117, 118f
anterior teeth, 6–7
Incisors, 12–13
characteristics of, 7–8
for forced eruption, 118, 119f
Indirect fabrication, of custom cast posts and
endodontically treated
description of, 35
Occlusal forces, 6
Indirect provisional restorations, 85–86
provisional crown as matrix for amalgam
Orthodontic extraction, 123
Infection-related root resorption, 27–28,
core buildup in, 50, 51f
Orthodontic extrusion
crown-root ratio improvements through,
Infractions, 23–25
infraction risks, 23
In-office extracoronal bleaching, 99f,
root morphology of, 13
implant placement benefits of, 124
intra-alveolar transplantation advantages
Instrument Removal System, 199
Mandibular premolars
infraction risks, 23
mechanical application guidelines for,
broken. See Broken instruments.
post placement in, 14
diameter of, root fracture and perforation
root morphology of, 13
periodontal advantages of, 123
Masserann Kit, 185–186, 186f
success factors, 116
intra-alveolar transplantation, 129
Masserann Micro Kit, 196
Orthodontic forced eruption. See also
post space preparation using, 11, 64
Maxillary canines, 12
rotary. See Rotary instruments.
Maxillary first molars
advantages of, 125
Intentional replantation, 138, 138f, 176
post diameter excess in, 65
Interdentin cracks, 182
root morphology of, 12–13
application of, 118–121, 119t–120t
Internal resorption, 28, 28f
Maxillary first premolars
biologic width and, 116, 124f
Interproximal papillae, 124
post placement in, 14
biology of, 121–122
root morphology of, 12
brackets and wires for, 118, 120
adjunctive procedures, 128–129
two-rooted, 12, 14
coronal restoration goals of, 116–117
advantages of, 132
Maxillary incisors
crown fracture and, 116
case report of, 129, 130f–131f
endodontically treated
esthetics of, 123
complications of, 132–133
canal filling material in access cavity of,
contraindications for, 132
goals of, 116–117
disadvantages of, 132
with natural crowns, 35
guidelines for, 120t
esthetics affected by, 132
forced eruption of, 120f
indications for, 116
ferrule effect improved through, 132
post placement in, 14
maxillary incisors, 120f
fixation after, 131
root morphology of, 12
mechanics of, 118–120, 119f–120f,
histologic evaluation of outcome of,
infraction risks, 23
modalities of, 119t
palatal roots in, 71, 71f
orthodontic considerations, 123
indications for, 132
root morphology of, 12–13
instruments used in, 129
periodontal considerations, 123, 123f
outcomes of, 131–133
Maxillary premolars
principles of, 118, 119f
periodontal healing after, 131
endodontically treated, 35
progression of, 115–116
prognosis after, 133
infraction risks, 23
surgical technique of, 128–129
root morphology of, 12
research considerations, 124–125
Intracoronal tooth bleaching, 96–99,
scope of, 123–125
Intrapulpal hemorrhage, 92, 93f
Mesio-occlusal restorations, 6
Intraradicular disinfection, 78, 78b
Orthodontic tooth movement, 121, 123
Intrusive luxation, 132
Mineral trioxide aggregate, 171–173, 172f
Orthodontic wire, 39f
Irreversible pulpitis, 20, 24
Moisture content, 7, 35
Orthopedic force, 118
Orthopedic implant site preservation or
autotransplantation of, 137, 141f–142f,
Lasers, for crown lengthening, 112
Osseointegrated implants
Little Giant Post Puller, 183, 183f
advantages of, 149
Loosening of posts, 9–10, 15
infraction risks, 23
buccolingual positioning of, 157f
Lost-wax technique, 36, 37f
mandibular. See Mandibular molars.
complications of, 159–160
Luting agents, 75–77. See also Cement.
maxillary. See Maxillary molars.
coronoapical positioning of, 157f
perforation of, 172f, 174f–175f
description of, 125
post and core placement in, 71
immediate placement of
Mandibular canines, 13–14
Mottled tooth, 93–94
advantages of, 155
Mandibular fractures, 160
alveolar wall gap effects on, 158
Mandibular incisors
Mucoperiosteal flap, 153
contraindications for, 155–156
endodontically treated
Multiple idiopathic root resorption, 30, 30f
definition of, 154
with natural crowns, 36
dehiscence effects on, 158–159
post avoidance in, 14
factors that affect, 156–159
root morphology of, 13
Nickel-titanium files, 195–196
fenestration effects on, 158–159
Mandibular molars
indications for, 155–156
distal roots in, 71, 71f
periapical pathosis effects on, 159
primary stability during, 158
timing of repair, 168–169
tooth fracture secondary to, 182
scientific validation for, 154–155
tooth retention affected by, 167–168
ultrasonic devices for, 190–192
surgical protocols, 156
Periapical pathosis, 159
tooth position effects on, 156
Periodontal disease, 26, 124
instruments used to create, 11, 64
tridimensional position effects on, 156–
Periodontal ligament, 121, 139, 143–144
root fracture risks, 13
Periradicular lesions, 27
Post space preparation
mesiodistal positioning of, 157f
Peritubular dentin, 35
definitive restoration placement after,
Peroxides, for tooth bleaching, 94–96
contraindications, 152
Pivot crowns, 33–34
gutta-percha removal and, 66–67
description of, 149–150
PMMA. See Polymethyl methacrylate.
provisional restoration placement after, 88f
in healed sites, 152–154, 153f–154f
Polycarboxylate cement, 76
root perforation caused during, 27f, 170
immediate loading of, 154
Polyethylene fiber–reinforced posts, 45f,
immediate provisionalization, 153–154
amalgam, 48–50, 49f–50f
indications for, 152
carbon fiber–reinforced epoxy resin, 41–
nonsubmerged technique, 153
acrylic resin provisional restorations, 84
scientific validation for, 152
eugenol effects on, 78
complications of, 9–14
submerged technique, 153
shrinkage during, 51
composite resin, 51–52
Osseointegration, 152
Polymethyl methacrylate, 84–86
custom cast. See Custom cast posts and
cementation of. See Cement; Cementation.
description of, 41
Palatal canal, 71f
depth of, 11–12
direct materials, 48–52
Passive eruption, 108, 109f
diameter of, 11, 64, 65f
for endodontic treatment of tooth under a
fiber. See Fiber posts.
glass fiber–reinforced epoxy resin, 43f,
classification of, 170, 170b
guidelines for, 9
43–45, 44t, 45f
combined endodontic-periodontal
laboratory data findings regarding, 8–9
glass ionomer, 52
conditions caused by, 27
length of. See Post length.
in molars, 71, 71f
crestal, 169, 171, 173, 174f
loosening of, 9–10, 15, 191
in multirooted teeth, 71, 71f
definition of, 167
materials for, 14–15
polyethylene fiber–reinforced posts, 45f,
description of, 9
diagnosis of, 168–170
misconceptions about, 8
prefabricated. See Prefabricated posts.
prefabricated, 14
factors that affect, 10–13
provisional, 87–88
removal of. See Post removal.
furcation, 169, 173
purpose of, 35–36
retrofitting of, to existing crown, 207–211
hemorrhage at site of, 175
removal of. See Post removal.
tooth strengthening benefits of, 36
retrofitting of, to existing crown, 207–211
types of, 36–52
illustration of, 27f
sealer effect on retention of, 77–78
zirconia, 46f, 46–47
instrument diameter and, 11
Posterior teeth. See also specific teeth.
intentional replantation for, 176
surface treatment of, 79
anchorage for, 118
endodontically treated
management of, 172–176
crown restoration of, 34
mineral trioxide aggregate for, 171–173,
crown length and, 62–63, 71
custom cast posts and cores for, 40–41
excessive, 62–63
restorations for, 8, 34–35
molars, 172f, 174f–175f
fiber posts, 14–15
survival rate of, 34
orthograde management of, 172–175
guidelines for, 63–64
Prefabricated posts
post length excess as cause of, 62, 63f
post loosening affected by, 10
cementation or bonding of, 47, 48f
post space preparation as cause of, 27f
retentive ability and, correlation between,
description of, 14
premolar, 168f–169f, 173f–174f
prevention of, 13–14, 170–171
root curvature effects on, 71
types of, 41–47
prognostic factors for, 168–170, 170b,
root fracture risks and, 11, 62–63
autotransplantation of, 143f, 143–144
pulpal floor, 168
infraction risks, 23
repair materials for, 171–172
endodontist referral for, 181
retrograde management of, 175f, 175–
factors that affect, 181
illustration of, 184f–185f
perforation of, 168f–169f, 173f–174f
risk factors for, 14
mechanical devices for, 182–188,
post and core placement in, 71
root fracture and, differentiation of, 64
two-rooted, 12, 14
signs and symptoms of, 168
post characteristics that affect, 181
Pressure-related root resorption, 29, 29f
risks associated with, 182
Primary roots, 64
subcrestal, 173–175, 174f
root fracture secondary to, 182
Proprioception, 8
supracrestal, 169, 171, 173
rotary instruments for, 188–190,
surgical management of, 175f, 175–176
access cavity through, 203, 204f
amalgam cores under, 49
endodontic treatment of tooth with, 201–
amalgam. See Amalgam restorations.
anterior teeth, 8, 34–35
maxillary, 12–13
posterior teeth, 34
composite resin. See Composite resin
Root perforations. See Perforations.
retrofitting of post to, 207–211
Root resorption, 27–30, 139–140, 140f,
sound tooth structure amount necessary for,
extracoronal bleaching effects on, 101
factors that affect
Root surface conditioning agents, 176
time until failure with, 5–6
anatomical and structural, 70–71
Rotary instruments
Provisional fixed partial dentures, 49–50,
craze lines, 70, 70f
broken, 199f. See also Broken instruments.
dentin thickness, 11, 70–71
description of, 66
Provisional restorations
ferrule effect, 68f, 68–69, 84
post removal using, 188–190, 189f–191f
acrylic resin, 84–85
post diameter, 64, 65f
cementation of, 86–87
post length, 61–64, 62f–64f, 84
characteristics of, 84, 85b
provisional restorations, 67–68, 68f
composite resin, 85
root canal preparation, 66–68
immediate versus delayed removal of, 67
computer-aided design/computer-assisted
posterior teeth, 8, 34–35
post retention affected by, 77–78
manufacture of, 86
provisional. See Provisional restorations.
Setting shrinkage, 51–52
coronal access, 67–68
selection guidelines for, 8
Shear strength, 8
in endodontically treated teeth, 87
Retrofitting of post to existing crown, 207–
Shrinkage, 51–52
fabrication of, 85–86, 86b, 86f
Silver alloys, added to glass ionomer, 52
indirect, 85–86
Reversible pulpitis, 20, 21f, 24
Silver-palladium alloy, 36
luting of, 86–87
Single-tooth implants
materials for, 84–85
crown-root ratio, 116–117, 124
contraindications, 152
description of, 149–150
post and core, 87–88
perforation of. See Perforations.
in healed sites, 152–154, 153f–154f
surgical crown lengthening and, 111
immediate loading of, 154
Proximal contact, 4
Root canal preparation, 66–68
immediate provisionalization, 153–154
indications for, 152
instruments used to increase, 47
nonsubmerged technique, 153
overenlargement of, 13
scientific validation for, 152
Root canal system
submerged technique, 153
Pulpal disease, 26, 26f
broken instruments in. See Broken
Pulpal necrosis, 26f, 92, 93f, 128
Sodium hypochlorite, 78
Pulpitis, 20, 21f, 24
description of, 22, 22f
Sodium perborate, 94
Pulpless teeth. See Endodontically treated
smear layer created during cleaning and
Soft tissue crown lengthening, 110
Sound tooth structure, 14
Root canal therapy. See also Endodontically
S.S. White Post Extractor, 183
treated teeth.
Structural tooth defects, 93–94
Radicular dentin, 78–79
anatomical considerations, 21–22
Subcrestal perforations, 173–175, 174f
Radicular invaginations/grooves, 27
factors that affect, 20
Subgingival fractures, 4, 128
inadequately performed, 20f
Supracrestal perforations, 169, 171, 173
antibiotics use in, 139
Surgical crown lengthening
of avulsed tooth, 138, 138f, 144, 145f
root canal preparation for, 21–22
in anterior areas, 108, 109f
dietary considerations, 139
survival rates for, 20
biologic width considerations, 108–109
extraction and, 145–147, 146f
treatment planning for. See Treatment
description of, 69, 107
general principles of, 139–141
esthetic concerns, 108, 109f, 112
intentional, 138, 138f, 176
vertical root fractures versus, 25
factors that affect, 110
prognosis after, 140–141
ferrule considerations, 109–110
root resorption concerns, 139–140, 140f
crown fracture and. See Crown-root
Research, 124–125
Resin bonding, 78–79
factors that affect, 10–13
indications for, 107, 110, 111f
glass fiber–reinforced epoxy resin posts
description of, 77, 79
provisional restorations used with, 111
fiber-reinforced resin post cementation
instrument diameter and, 11
recommendations for, 112–113
using, 82–83, 83f
orthodontic extrusion contraindications,
restorative procedures after, 111
indications for, 84
ultrasonic post removal affected by, 191
post diameter and, 11, 65
in subgingival preparation margins, 110,
Resin-based sealer, 77–78
post removal as cause of, 182
Resin-modified glass-ionomer cement, 77
prevention of, 13–14
technique of, 110–112, 111f
residual dentin thickness effects on, 11
root perforation and, differentiation of, 64
endodontically treated teeth, 4
root. See Root resorption.
threaded posts as risk factor for, 10
fixed partial dentures, 4–5
vertical, 25–26, 26f
pulpal status assessments, 20, 21f
Tetracycline-related tooth stains, 92–93, 93f
events after, 150–151
Tetragonal zirconium polycrystals, 46
healing after, 150f
tooth fractures, 22–26
Thermocatalytic method, for intracoronal
implant replacement after, 117, 118f
vertical root fractures, 25–26, 26f
tooth bleaching, 98
Threaded posts, 9–10
replantation and, 145–147, 146f
Tissue engineering, 123
resorption after, 151
Ultrasonic devices, for post removal, 190–
ridge preservation after, 150–152
autotransplantation for. See
socket defects, 158–159, 159f
Ultrasonic tips, 198–199
for vertical root fracture, 25–26
Ultraviolet photo-oxidation technique, for
description of, 137
intracoronal tooth bleaching, 98
Tooth avulsion, 138f
biologic width affected by, 111f
Urea hydrogen peroxide, 94
in endodontically treated teeth, 4–5
Urethane dimethacrylate, 85
carbamide peroxide for, 94–95
post removal as cause of, 182
definition of, 93
types of, 22–26
extracoronal. See Extracoronal bleaching.
Vertical root fractures, 25–26, 26f
causes of, 5, 137
Vital teeth, endodontically treated teeth
hydrogen peroxide for, 94–96, 100–102
data analysis of, 5
intracoronal, 96–99, 97f–99f
fracture-related, 5
outcome of, 101–102
Tooth movement, orthodontic, 121, 123
over-the-counter products for, 94, 100
Tooth sensitivity, 100–101
Walking bleach, 96–98, 97f
peroxides for, 94–96
Tooth stains, 92–94
residual oxygen produced during, 99
Tooth stiffness, 35
sodium perborate for, 94
Tooth structure loss, 116
Yttrium-stabilized tetragonal polycrystalline
Tooth whitening, 93. See also Tooth
Tooth discoloration
aging-related, 92
calcific metamorphosis, 92
Transplantation. See Autotransplantation;
Zinc oxide–eugenol-based sealer, 77–78
diseases that cause, 93
Intra-alveolar transplantation;
Zinc phosphate cement
extrinsic causes of, 92
cast post and core cementation using,
intrapulpal hemorrhage, 92, 93f
Transportation of the canal, 22
80–82, 80f–82f
intrinsic causes of, 92–94
Trauma-related root resorption, 27
description of, 76, 76b
pulpal necrosis, 92, 93f
Treatment planning
provisional restoration cementation using,
structural tooth defects that cause, 93–94
combined endodontic-periodontal
tetracycline-related, 92–93, 93f
problems, 26–27
ultrasonic post removal affected by, 191
cracked teeth, 22–26
Zirconia posts, 46f, 46–47
forced. See Orthodontic forced eruption.
enamel craze lines, 22–23, 23f
normal process of, 121
infractions, 23–25
Source: http://www.dentalbooks.bg/PDF-2015/contemporary-restorations-Baba.pdf
The Gender Politics of Criminal Insanity: "Order-in-Council" Women in British Columbia, 1888–1950 DOROTHY E. CHUNN* Between 1888 and 1950, 38 women were confined for indeterminate periods toBritish Columbia's psychiatric system under executive "Orders-in-Council".Enlisting clinical, organizational, and government records, the authors explore thepsychiatric practices of control through which a male medico-legal establishmentstrove to comprehend and discipline these "criminally insane" women. Theauthoritative discourses and activities that shaped these women's forensic careersreflected a gendered conception of social order that was hegemonic during thisperiod. Such discourses helped to fashion the images of women, crime, and madnessthat continue to permeate public and official culture.
Le coût du hadj sera annoncé la semaine prochaine Lire en page 3 N° 5152 - MERCREDI 22 AVRIL 2015 QUALIFIÉE DE MASCARADEPAR LES PROCHES DU CHEIKH La statue de Benbadis«évacuée» du centre Lire en page 7 Enlèvement de la marchandise prohibée du port sec Anisfer de Rouiba NEUF DOUANIERS SOUS MANDAT DE DÉPÔT Le juge d'instruction de la deuxième chambre près le tribunal de Sidi-M'hamed (Alger), a ordonné hier, la mise en détention préventive de