Levitra enthält Vardenafil, das eine kürzere Wirkdauer als Tadalafil hat, dafür aber schnell einsetzt. Männer, die diskret bestellen möchten, suchen häufig nach levitra kaufen ohne rezept. Dabei spielt die rechtliche Lage in der Schweiz eine wichtige Rolle.
Social mishap exposures for social anxiety disorder: an important treatment ingredient

Social Mishap Exposures for Social Anxiety Disorder: An Important
Treatment Ingredient
Angela Fang, Alice T. Sawyer, Anu Asnaani, and Stefan G. Hofmann, Boston University
Conventional cognitive-behavioral therapy for social anxiety disorder, which is closely based on the treatment for depression, has been shownto be effective in numerous randomized placebo-controlled trials. Although this intervention is more effective than waitlist control group andplacebo conditions, a considerable number of clients do not respond to this approach. Newer approaches include techniques specificallytailored to this particular population. One of these techniques, social mishap exposure practice, is associated with significant improvement intreatment gains. We will describe here the theoretical framework for social mishap exposures that addresses the client's exaggerated estimationof social cost. We will then present clinical observations and outcome data of a client who underwent treatment that included such socialmishap exposures. Findings are discussed in the context of treatment implications and directions for future research.
S OCIAL anxiety disorder (SAD) is one of the most
common anxiety disorders in the U.S., with a lifetime
). The cognitive-behavioral model proposes that
and 12-month prevalence of 12.1% and 7.1%, respectively
SAD develops and is maintained by maladaptive cognitive
and behavioral processes, which negatively reinforce
defined by a persistent fear of negative evaluation by others
avoidance strategies and contribute to a cycle of anxiety
in social or performance situations
) and is associated with significant impair-
). The following discussion is based on the mainte-
ment in occupational, academic, and interpersonal func-
nance model developed by which
emphasizes the importance of social cost and social mishap
heterogeneous condition, as individuals with SAD may vary
exposures. A more detailed explanation of this model is
in the kinds of people, places, and situations that cause fear.
described elsewhere ). According to this
However, common fears include formal public speaking,
model, an individual with SAD experiences apprehension
speaking up in a meeting or class, and meeting new people
upon entering a social situation because they perceive the
(Ruscio et al.). It also appears that while these situations may
social standards to be excessively high and experience
differentially provoke anxiety for each individual, most
doubt about being able to meet those standards. Once
clients with SAD share similar underlying core fears, such
confronted with social threat, individuals with SAD
as being rejected, looking stupid or unintelligent, expressing
experience heightened self-focused attention, in which
disagreement or disapproval, and being the center of
attention is turned inwardly toward one's internal physical
sensations and anxious thoughts . Self-
Theoretical Models of SAD
focused attention simultaneously triggers a variety of other
There is strong empirical evidence supporting a
cognitive processes, including a negative self-perception
cognitive-behavioral model of SAD
(e.g., "I am such an inhibited idiot"), high estimated socialcost (e.g., "It will be a catastrophe if I mess up this
Video patients/clients are portrayed by actors.
"), low perceived emotional control (e.g., "I have
no way of controlling my anxiety"), and perceived poor
Keywords: exposure therapy; social mishap exposure; social anxiety
social skills ("My social skills are inadequate to deal with this
situation"). These processes, in turn, lead the client toanticipate a social mishap in which one actually does
something to embarrass oneself, cause negative evaluation,
2012 Association for Behavioral and Cognitive Therapies.
Published by Elsevier Ltd. All rights reserved.
or otherwise violate social norms. This expectation
contributes to the use of avoidance strategies and safety
intentionally create the feared negative consequences of a
behaviors to cope with the anxiety and to avoid the feared
feared social situation. As a result, patients are forced to
outcome, which leads to post-event rumination about one's
reevaluate the perceived threat of a social situation after
performance in a social situation (
experiencing that social mishaps do not lead to the feared
The rumination and avoidance behaviors ultimately feed
long-lasting, irreversible, and negative consequences. A
back into continued apprehension in social situations.
more detailed description of this model is presented in
An important reason why SAD is maintained in the
presence of repeated exposure to social cues is because
Early data suggest that treatment protocols that incor-
individuals with SAD engage in a variety of avoidance and
porate social mishap exposures show considerably greater
safety behaviors to reduce the risk of rejection (e.g.,
efficacy than traditional CBT protocols, which are typically
). These avoidance tendencies, in turn, prevent
associated with only moderate effect sizes (e.g.,
patients from critically evaluating their feared outcomes
Other, more recent studies that include social
and other catastrophic beliefs, leading to the maintenance
mishap exposures (among other techniques) report
and further exacerbation of the problem. Social mishap
considerably larger efficacy rates. For example,
exposures directly target the patients' exaggerated social
reported effect sizes ranging between
cost by helping patients confront and experience the actual
1.41 (pretest to posttest) and 1.43 (pretest to 12-month
consequences of such mishaps without using any avoidance
follow-up; Clark et al.). Similar efficacy data (pre-post effect
size of 1.54) have been found in an early pilot trial).
Obviously, social mishap exposures are not the only
Social Mishap Exposures
aspect that distinguishes traditional CBT protocols from
Consistent with the notion that clients with SAD over-
more modern approaches Depending on
estimate the social costs associated with social mishaps, high
the specific treatment protocol, other aspects include
estimated social costs have been proposed to be an
strategies for attention retraining, changes in self-perception,
important mediator of treatment change (
and post-event rumination. However, in-vivo social mishap
. This hypothesis has been subjected to empirical
exposures are the most obvious differences to traditional
testing, and substantiated in a treatment outcome study that
CBT approaches, which have primarily employed in-session
compared cognitive-behavioral group therapy, exposure
role-play situations with the goal to identify and replace
therapy (without explicit cognitive intervention), and a
maladaptive general automatic thoughts. The purpose of the
wait-list control group . It was found that
current paper is to present a case example from a group
changes in estimated social costs mediated treatment
cognitive-behavioral therapy protocol that emphasizes social
change between pre- to posttreatment in the two active
mishap exposures, and to discuss the benefits and challenges
treatment conditions ). These empirical
associated with its successful implementation. The case that
findings therefore support the utility of social mishap
follows discusses a treatment-seeking individual who pre-
exposures in addressing this overestimation of costs
sented to an outpatient clinic specializing in the treatment of
associated with a social mishap. This is accomplished by
mood and anxiety disorders.
having the client behave in a way that causes a social mishapby purposefully violating the client's perceived social norms
(e.g., singing in a subway).
The Anxiety Disorders Interview Schedule (ADIS-IV;
The difference between social mishap exposures and
) was administered at the
exposure practices that have been typically used in
intake evaluation. The ADIS-IV is a semistructured clinical
cognitive-behavioral therapy protocols for SAD is that social
interview that assesses mood and anxiety disorders
mishap exposures cause clients to experience the feared
according to DSM-IV
outcomes that they try so hard to avoid by clearly appearing
) criteria. The Liebowitz Social Anxiety Scale (LSAS;
incompetent, crazy, obnoxious, and so on. Standard
) is a 24-item clinician-administered mea-
exposure practices of patients with SAD are typically
sure that assesses fear and avoidance of social situations
designed to make patients realize that social catastrophes
(each rated on a 0- to 3-point scale with a range of total
are unlikely to happen, and that patients are able to handle
scores from 0 to 144) in the past week. The LSAS has been
socially challenging situations despite their social anxiety
validated in clinical samples, and has high internal
(e.g., ). In contrast, the goal of
consistency ). The LSAS was
the social mishap exposures is to purposely violate the
administered at every session throughout the course of
patient's perceived social norms and standards in order to
treatment, and also at six major time points: baseline, Week
break the self-reinforcing cycle of fearful anticipation and
8, posttreatment, 1-month follow-up, 3-month follow-up,
subsequent use of avoidance strategies. Patients are asked to
and 6-month follow-up.
Social Mishap Exposures for SAD
In addition, Mary described residual symptoms of
was a 41-year-old married, Caucasian, insurance
depression that never resolved after having lost her job
company analyst, who lived with her husband and two
2 years ago. She had been working as a research analyst at
children. She came to the clinic seeking outpatient
a local bank, and had been fired due to the bad economy
psychotherapy for her social anxiety. She presented with
as well as poor reviews from clients. She reported feeling
primary concerns about having suffered from anxiety
like she had lost interest in many activities that she used to
throughout her life. She reported "always feeling awkward
enjoy, such as shopping and seeing friends, and has been
and self-conscious in groups," and not knowing what it was
feeling excessively guilty and doubtful of her ability to
until she read more about social anxiety in online help
hold her current job. Mary reported not having ever
forums. Mary described her social anxiety as being at its
received cognitive-behavioral therapy for either her
worst when meeting new people in unstructured social
depression or social anxiety concerns, but that she had
gatherings, such as parties and work events, and she
tried supportive therapy with a variety of health-care
described the anticipatory anxiety to be so crippling that
professionals, including counselors and licensed social
she would often turn down invitations. She reported
workers. Last year, Mary visited a psychiatrist to receive
feeling nervous about what to say, asking too many
psychopharmacological interventions for her depression,
questions, and not feeling like herself. Mary's anxiety had
which she reported being effective.
affected her life in many ways. For example, in college she
Based on information obtained from her baseline
had majored in mathematics to avoid courses that
assessment, Mary received a primary diagnosis of SAD,
involved formal presentations; she had lost jobs; and,
generalized subtype, and a diagnosis of major depressive
ultimately, she had chosen a career that involved limited
disorder (MDD), in partial remission. She had no other
social interactions. When Mary was asked what she was
comorbid psychiatric disorders, but reported a family
concerned would happen in these situations, she could
history of MDD. She had also been taking Wellbutrin
not initially give an answer, but later responded that she
(200 mg) for a year for her depression, which she
was worried that others would judge her negatively, reject
discontinued through a psychiatrist-guided taper prior
her or hurt her feelings. She further explained that her
to starting group treatment. Her baseline LSAS score of
worst fear was that she would alienate everyone, even
90 reflected a severe level of SAD.
those who were close to her.
Mary described recent concerns about not performing
Treatment Procedure
well at work due to extreme distress when preparing for
The treatment consisted of 12 weekly, 2.5-hour sessions
group meetings and presentations and extreme anxiety
of group cognitive-behavioral therapy with four to six
making work-related phone calls. During her assessment,
members in total. The protocol was implemented by two
it was gleaned that Mary was worried that she was going to
therapists, master's-level doctoral candidates, who fol-
get fired from her job because she had put off making
lowed the treatment manual.
some important phone calls, and clients had called her
Week-to-week LSAS scores were determined by meeting
supervisor to complain. She described being concerned
separately with a trained independent evaluator before
that she would be perceived as incompetent or un-
the start of each group.
intelligent by clients and coworkers. Mary also hadconcerns about wanting to be more involved in her
Sessions 1–2: Psychoeducation and Cognitive Restructuring
children's lives at school because her husband worked
The first session consisted of an introduction of
much longer hours, but she was very apprehensive about
cotherapists and group members and their reasons for
attending parent-teacher conferences, parent-teacher
seeking treatment. Psychoeducation about the nature of
association meetings, and making small talk with other
SAD as a learned habit and the adaptive aspects of anxiety
mothers at her sons' sporting events and school concerts.
were presented and discussed. An overview of treatment
She described being particularly afraid of unstructured
was presented, with an introduction to the primary
small talk with same-age parents or teachers because they
treatment techniques, which included cognitive restruc-
would think she was awkward. Mary explained that she
turing and in-vivo exposures. The session concluded with
feared other mothers perceiving her as an uninvolved and
identification of automatic negative thoughts related to
bad parent. She also reported severe avoidance of her
attending group treatment specific to each client, and
children's extracurricular events, with the exception of
assignment of thought records (e.g., monitoring of such
dropping them off and picking them up.
automatic thoughts) for homework.
Session 2 began with a review of the homework and an
invitation from group members to share their thought
records. The majority of the session focused on presenting
Client name and other identifying information have been
changed to protect client confidentiality.
the exposure rationale to the group by discussing the role of
avoidance in perpetuating the cycle of anxiety. Examples of
in-session public speaking exposures were structured
safety behaviors and other avoidance behaviors were
similarly to the more traditional SAD group treatment
discussed by using specific recent examples. The short-term
exposures, the concept of purposefully experiencing social
and long-term consequences of these avoidance behaviors
mishaps was introduced very early on (typically by the
for the maintenance of the disorders were discussed. The
second or third in-session exposure) to target these
session concluded with a discussion of concerns and
avoidance behaviors. In collaboration with the other
questions about the start of public speaking exposures at
group members and Mary, the therapist generated specific
the next week's session. For homework, clients were asked
exposure tasks to provide Mary with an opportunity to
to generate a hierarchy of feared social situations for use
examine the actual consequences of what she considered to
be social mishaps. For example, during Session 5, Mary was
Mary attended the group along with four other clients.
asked to give a 3-minute speech about cloning (of which she
The other members varied in age, gender, occupation, and
had little knowledge), and her specific goals were (a) to
SAD symptom severity. At the first two sessions, Mary
make eye contact with every member of the audience at least
engaged in the discussion and appeared to relate to other
once; (b) to stop speaking suddenly in the middle of her
group members' experience of SAD. Similar to other
speech for a long pause and to count 5 "Mississippi" before
members, Mary described strong physiological reactions
resuming; and (c) to pace back and forth across the room
(e.g., racing heartbeat and sweaty palms) to anticipating an
during the entire speech. In accordance with the research
important class presentation or work meeting; she identi-
on high perceived social standards and high estimated social
fied jumping to conclusions as a major cognitive distortion
costs associated with the speech, Mary collaboratively
that emerged for her.
designed an experiment with the therapists to test howhigh the social standards and social costs were for the speech
Sessions 3–7: In-Session Exposures
and to see what would happen if she did run out of things to
Sessions 3 to 7 consisted primarily of conducting
say. Mary reported an anticipatory anxiety of 80 (on a
in-session public speaking exposures, in which each group
100-point scale of subjective units of distress, or SUDS), a
member gave a 3-minute speech on an impromptu topic
peak anxiety of 80, and a final anxiety of 45 at the end of the
that he or she had rated highly on a speech topics
exposure. She described experiencing significant anxiety
hierarchy. Specific behavioral goals were collaboratively
when she stopped speaking at first, but that it gradually came
agreed upon with the therapist at the start of the exposure
down over time. She stated at the end of the exposure that
to address elimination of safety behaviors during the
pausing during the speech was not as bad as it sounded at
exposure, as well as the individual client's core fears.
first. Upon reviewing the videotape feedback, Mary noted
Incorporating social mishap during the speech exposure
that the person in the video did not actually look that
was introduced as a way to disconfirm negative beliefs about
anxious during the long pause. This was an important
feared consequences. Furthermore, automatic thoughts
component of treatment for her, as she mentioned later that
about the speech were identified and challenged before
she was shocked by the discrepancy between how she looked
and after the exposure. Speeches, conducted in front of the
and how anxious she felt on the inside.
group, were videotaped to provide feedback to clients.
Speech exposures can be used to target other fears by
For homework, group members were requested to repeat
reevaluating the patient's estimated social costs. For
their in-session speech exposures in front of the mirror each
example, clients who fear looking silly during the speech
day three times in a row. The mirror exposures were used to
can be asked to put on a costume or prop, such as an
address clients' self-focused attention by allowing them to
attention-grabbing wig or witch's hat. Those who fear
receive live feedback on their appearance (akin to videotape
appearing unintelligent may say something factually incor-
feedback during the session), and to give them a chance to
rect or mispronounce a word during the speech. Those who
engage in the repeated exposure model for anxiety
fear that they will stutter can intentionally stutter during the
speech. Speech exposures have also been used in tandem
Mary described experiencing significant anticipatory
with interoceptive exercises for individuals who fear the
anxiety leading up to these sessions, and even admitted to
physiological sensations that emerge in anticipation of or
almost skipping a session to avoid giving an impromptu
during the speech. Those individuals would conduct
speech. Her speech exposures were particularly useful and
interoceptive exercises (e.g., induced hyperventilation for
relevant for the group presentations that she had to give as
shortness of breath, running in place for racing heartbeat
part of her job. Mary's primary fear in this domain was
and sweating) for 1 minute before the start of the speech.
running out of things to say, which would cause her toengage in safety behaviors such as limiting eye contact with
Sessions 8–11: In-Vivo Mishap Exposures
the audience and freezing up in front of the group to
Sessions 8 to 11 involved targeted in-vivo mishap
minimize attention on her. As a result, while these first few
exposures that were further tailored to the individual
Social Mishap Exposures for SAD
client's core fears. The goals for the exposures were
introduction of herself to at least one individual. Mary
collaboratively discussed and agreed upon with the
reported that these between-session exercises were essential
therapists at the outset. Social costs were incorporated
to her progress, as they translated her therapeutic work to
into each exposure to target specific core fears of the
her real-life social situations and contexts.
individual client. In addition, automatic thoughts about
As stated previously, these exposure exercises should
the exposures were identified and challenged before and
specifically challenge the patient's social cost estimates
after the exposure. When group members returned from
(e.g., walking around with toilet paper hanging out of the
the exposures, the therapists led a discussion of whether
shirt, buying and minutes later returning the same book,
each exposure was successful by reviewing the clients'
walking on a busy street with the zipper of the pants wide
open, spilling water in a restaurant, asking a random woman
Mary's in-vivo mishap exposures were designed to target
on a street out on a date) to be most effective. When
her fears of inconveniencing others, being the center of
conducting these social mishap exposures, it is important to
attention, and being thought of as unintelligent. To address
clearly define the goal of the exposure situation and not to
her fear of inconveniencing others, the therapists worked
link the success or goal of the exposure to the patient's
with Mary to design an exposure in which she negotiated a
anxiety (i.e., "I want to do it nonanxiously" is not an
romantic vacation package at a nearby five-star hotel. Her
acceptable goal). Instead, the goal should be linked to
goals were to ask for tickets to a ballgame, for rose petals to
specific behaviors that allow the patients to test the
be strewn on the bed, and for a horse-drawn carriage tour of
anticipated consequences of the social mishaps. It is essential
the city. At the end of stating those three requests, her goal
that patients refrain from avoidance or safety behaviors,
was to obtain an itemized list with the final price, negotiate
such as apologizing, or any other behavior that might lessen
the price, and then reject the offer because she "changed
the patients' anxiety in the situation. For this reason, it is
her mind" without apologizing or giving any excuses. She
advisable to provide detailed instructions to the patients to
described having automatic thoughts that she would get
give them no room to engage in any such avoidance
kicked out of the hotel, and that the concierge staff would
behaviors. provides further examples of social
roll their eyes at her. Mary's anticipatory anxiety was a 90,
mishap exposures that clinicians may utilize in treatment.
her peak anxiety was a 90, and her final anxiety rating was a
Our research group has filmed a series of treatment
40. Upon completing her exposure, she stated that she was
sessions to exemplify various aspects of the intervention.
surprised by the concierge's accommodating nature,
These can be found online at the Boston University
despite her outrageous requests, and that she did not
Psychotherapy and Emotion Research Laboratory
receive the kind of negative response she had anticipated by
the concierge staff. She met all of her goals and left the
particular, the following video clips depict three treatment
exposure with a sense of accomplishment for minimizing
phases germane to the current paper: Video 1 demon-
any use of safety behaviors (e.g., apologizing excessively for
strates how to set up for an in-vivo exposure
turning down the offer).
Other exposures that Mary conducted in subsequent
Video 2 demonstrates how to conduct a social mishap
sessions addressed similar fears: interrupting a group of
people in a restaurant to practice a toast for a maid-of-
; and Video 3 demonstrates the
honor speech (targeting inconveniencing others and being
postprocessing of a social mishap exposure
the center of attention); asking strangers in a bookstore to
read the back cover of a book because she did not know howto read (targeting being thought of as unintelligent); and,
Session 12: Relapse Prevention
while wearing bandages on her face, asking people on the
The treatment concluded with a discussion of relapse
street if they were "Carl Smith" because his car was being
prevention strategies. Clients reviewed their progress,
towed (targeting inconveniencing others, being the center
discussed areas of improvement, assisted each other in
of attention, and being thought of as weird).
detecting warning signs, and generated ways to maintain
Mary was assigned between-session in-vivo exposures to
their progress. Similar to the recommendations for contin-
practice the effects of repeated exposure. She was encour-
ued use of other treatment components (e.g., cognitive
aged to be creative, be concrete in specifying the behavioral
restructuring techniques, approach to feared situations),
goals of the exposures, and to try out other group members'
ongoing use of social mishap techniques posttreatment were
exposures. During the course of treatment, opportunities
suggested in those cases where overestimated social cost and
arose for Mary to make important phone calls at work and
fear of social norm violation remained a primary issue. For
attend parent meetings at her children's school. She had
instance, Mary was encouraged to continue targeting her
assigned goals for herself that minimized the use of safety
fear of being the center of attention by engaging in behaviors
behaviors, such as not procrastinating and initiating
for which she thought she would be negatively judged. She


Table 1Examples of Social Mishap Exposures
1. Ask three people in the subway if they can spare $20.
2. Walk backwards slowly in a crowded street for three minutes.
3. Wear your shirt backward and inside out and buttoned incorrectly
in a crowded store. Goal: Look three people in the eye.
4. Pay for an embarrassing item with change, and then state that
you don't have enough and leave the store.
5. Approach people on the street asking if they can help you tie
your shoelaces when you're wearing shoes without laces.
6. Recite "Twas the Night Before Christmas" in the subway
7. Go to a fast food restaurant and only order water, then spill the
water, clean it up, and stay in the restaurant.
8. Ask multiple people in a specific and obvious location (e.g., right
Video 1. Demonstrating how to set up an in-vivo social mishap
outside XXX Park, or a T stop) where to find that location
exposure with patient.
("Excuse me, I am looking for XXX Park").
9. Ask a staff member in Barnes and Noble for their opinion
about whether to buy the Kama Sutra or the Joy of Sex, have along conversation about this, buy the books and then returnthem immediately.
10. Initiate conversations with/tell jokes to strangers in Barnes and
Noble while wearing hair in a side ponytail with bandages onface.
11. Dance or sing in the street or subway wearing attention-grabbing
12. Call Barnes and Noble, ask to place on hold The Gas We Pass
and Everybody Poops as well as a chocolate chip cookie fromthe in-house café.
13. Go to a hotel. Have the patient conduct a long conversation
with the concierge about romantic vacation packages (askingabout in-room massages, arranging horse-drawn carriageride, etc.), book a package, and then cancel for no reason
Video 2. Patient conducting in-vivo social mishap exposure in the
except changing their mind.
presence of the clinician.
14. Go to every table in a crowded restaurant asking for Joe Smith.
15. Tell someone at B & N that you don't know how to read and
ask them if they can read the back cover to you.
16. Approach group of people at bar or restaurant and ask if you
can practice a best man's toast.
17. Enter a food establishment and interrupt people asking if
they own a silver Camry because their car is being towed.
was encouraged to try out social mishap exposures that othergroup members had engaged in during the course oftreatment to target this fear (e.g., wearing bright coloredarticles of clothing, talking loudly into her cell phone in acrowded area, and opening her umbrella indoors).
Video 3. Demonstrating how to conduct postprocessing of in-vivoexposure.
Summary of Treatment
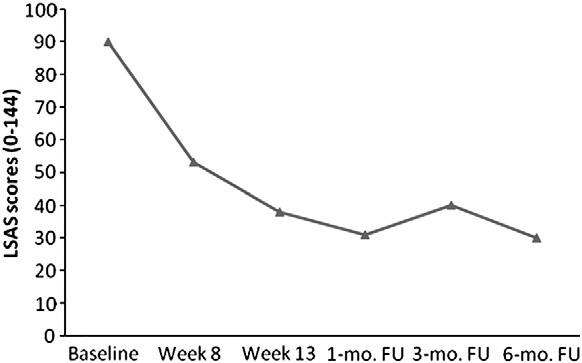
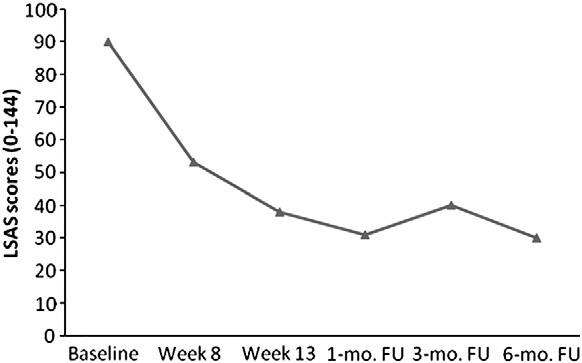
At the end of treatment, Mary's LSAS score decreased
to 38, which represented a 57.8% reduction of SADsymptoms from baseline. Mary continued to improve and
symptom severity and maintenance of such progress even
maintain her progress following acute treatment, as her
6 months later. Please see for a visual represen-
LSAS scores indicated further improvements in SAD
tation of Mary's outcome data at each time point.
Social Mishap Exposures for SAD
group format may provide additional motivation for singlepatients. At the same time, a group format provides lessflexibility to treat comorbid conditions in the context of thisprotocol. Consistent with research indicating that SADrarely occurs in isolation (amajority of the clients in the group had other comorbidclinical disorders. Although Mary's depression remained inpartial remission during the course of treatment, and inlight of research showing the negative impact thatcomorbidities such as depression have on SAD treatmentoutcomes (), the group treatment for SAD may not
Figure 1. Outcome data for case of Mary.
have been appropriate had she experienced anotherdepressive episode. It is also worth noting that the cases
presented in the current study represented a highly
Although Mary improved in a clinically meaningful way
motivated subset of individuals who participated in our
by the end of the treatment, she presented certain
group treatments, which may not be generalizable to the
challenges to the therapists who led her group. One primary
larger population of clients with SAD. This worked to our
difference in Mary's case compared to the other group
advantage because they were not only engaged in the
members was that Mary had a longer duration of illness (she
treatment, but they also served as cotherapists in the group
was the oldest member of the group) and she had a higher
by encouraging other group members to engage in
baseline severity of symptoms than the other members. She
treatment. We recommend that future treatment studies
had therefore developed highly evolved and idiosyncratic
incorporate social mishap exposures and further investi-
avoidance strategies. For example, it was not until the
gate their relative efficacy by directly comparing them to
therapists conducted a functional analysis during treatment
more traditional exposures. Additionally, although in our
that they discovered that Mary's overdelegation of work
experience all patients benefit to some extent from
(related to making phone calls) to the administrative
engaging in social mishap exposures, it is important to
assistants in the office was an avoidance strategy couched
systematically examine whether particular subsets of
in her mind as a justification for enhancing her efficiency at
patients benefit more than others (e.g., patients of certain
work. In other cases, clients have entered treatment with
age groups, clinical presentations, motivation levels).
significant stigma about seeking treatment, and have felt
Appendix A. Supplementary data
initially resistant to in-vivo exposures because of a fear of"being discovered" as having social anxiety by people in the
Supplementary data to this article can be found online
area where they were engaging in exposure exercises. These
thoughts had to be addressed directly through cognitive
restructuring to motivate members to attempt the exerciseassigned, and were even tested as predictions in the
American Psychiatric Association. (1994). Diagnostic and statistical
manual of mental disorders (4th ed.). Washington, DC: Author.
exposures. It was therefore challenging for the therapists
American Psychiatric Association. (2000). Diagnostic and statistical manual
to allot relatively equal amounts of time reviewing home-
of mental disorders (4th ed., text revision). Washington, DC: Author.
work and exposures with each client when some clients
Brozovich, F., & Heimberg, R. G. (2008). An analysis of post-event
processing in social anxiety disorder. Clinical Psychology Review, 28,
needed inordinately more time. There were limitations of
the current study that deserve mention. Some of the
Clark, D. M., Ehlers, A., McManus, F., Hackmann, A., Fennell, M.,
limitations apply for any treatment that is administered in
Campbell, H., . . Louis, B. (2003). Cognitive therapy versus fluoxetinein generalized social phobia: A randomized placebo-controlled trial.
a group rather than individual format. Although there tends
Journal of Consulting and Clinical Psychology, 71, 1058–1067.
to be less emphasis on an individual client in a group
Clark, D. M., & McManus, F. (2002). Information processing in social
treatment, the current protocol allowed for meaningful
phobia. Biological Psychiatry, 51, 92–100.
Clark, D. M., & Wells, A. (1995). A cognitive model of social phobia. In R. G.
tailoring of the treatment to an individual's needs and core
Heimberg, M. R. Liebowitz, D. A. Hope, & F. R. Schneier (Eds.),
Social phobia: Diagnosis, assessment, and treatment (pp. 69–93). New
Our clinical experience is that treatments that involve
York, NY: Guilford Press.
Davidson, J. R. T., Foa, E. B., Huppert, J. D., Keefe, F. J., Franklin, M. E.,
social mishap exposures are not associated with greater
Compton, J. S., . . Gadde, K. (2004). Fluoxetine, comprehensive
dropout rates than traditional CBT. This is consistent with
cognitive behavioral therapy, and placebo in generalized social
other studies utilizing similar social mishap exposure
phobia. Archives of General Psychiatry, 61, 1005–1013.
DiNardo, P. A., Brown, T. A., & Barlow, D. H. (1994). Anxiety Disorders
techniques This is somewhat surprising
Interview Schedule for DSM-IV: Client Interview Schedule. New York, NY:
given the highly unpleasant nature of the exposure tasks. A
Oxford University Press.
Heimberg, R. G., Dodge, C. S., Hope, D. A., & Kennedy, C. R. (1990).
disorders in the National Comorbidity Survey Replication. Archives of
Cognitive behavioral group treatment for social phobia: Comparison
General Psychiatry, 62, 617–627.
with a credible placebo control. Cognitive Therapy and Research, 14,
Liebowitz, M. R. (1987). Social phobia: Modern problems in pharmacopsychiatry,
22, 141–173.
Heimberg, R. G., Horner, K. J., Juster, H. R., Safren, S. A., Brown, E. J.,
Marom, S., Gilboa-Schechtman, E., Aderka, I. M., Weizman, A., &
Schneier, F. R., & Liebowitz, M. R. (1999). Psychometric properties of
Hermesh, H. (2009). Impact of depression on treatment effective-
the Liebowitz Social Anxiety Scale. Psychological Medicine, 29, 199–212.
ness and gains maintenance in social phobia: A naturalistic study of
Heimberg, R. G., Liebowitz, M. R., Hope, D. A., Schneier, F. R., Holt, C. S.,
cognitive behavior group therapy. Depression and Anxiety, 26,
Welkowitz, L. A., . . Klein, D. F. (1998). Cognitive behavioral group
therapy vs phenelzine therapy for social phobia: 12-week outcome.
Rapee, R. M., & Heimberg, R. G. (1997). A cognitive-behavioral model
Archives of General Psychiatry, 55, 1133–1141.
of anxiety in social phobia. Behaviour Research and Therapy, 35,
Hofmann, S. G. (2000a). Self-focused attention before and after treatment
of social phobia. Behaviour Research and Therapy, 38, 717–725.
Ruscio, A. M., Brown, T. A., Chiu, W. T., Sareen, J., Stein, M. B., &
Hofmann, S. G. (2000b). Treatment of social phobia: Potential mediators
Kessler, R. C. (2008). Social fears and social phobia in the USA:
and moderators. Clinical Psychology: Science and Practice, 7, 3–16.
Results from the National Comorbidity Survey Replication.
Hofmann, S. G. (2004). Cognitive mediation of treatment change in social
Psychological Medicine, 38, 15–28.
phobia. Journal of Consulting and Clinical Psychology, 72, 392–399.
Wells, A., Clark, D. M., Salkovskis, P., Ludgate, J., Hackmann, A., &
Hofmann, S. G. (2007). Cognitive factors that maintain social anxiety
Gelder, M. (1995). Social phobia: The role of in-situation safety
disorder: A comprehensive model and its treatment implications.
behaviors in maintaining anxiety and negative beliefs. Behavior
Cognitive Behaviour Therapy, 36, 193–209.
Therapy, 26, 153–161.
Hofmann, S. G. (2012). An introduction to modern CBT: Psychological
Wittchen, H. U., & Fehm, L. (2001). Epidemiology, patterns of
solutions to mental health problems. Chichester, UK: Wiley-Blackwell.
comorbidity, and associated disabilities of social phobia. Psychiatric
Hofmann, S. G., & Otto, M. W. (2008). Cognitive-behavior therapy for social
Clinics of North America, 24, 617–641.
anxiety disorder: Evidence-based and disorder-specific treatment techniques.
New York: Routledge.
Hofmann, S. G., & Scepkowski, L. A. (2006). Social self-reappraisal
Address correspondence to Stefan G. Hofmann, Ph.D., Department of
therapy for social phobia: Preliminary findings. Journal of Cognitive
Psychology, Boston University, 648 Beacon St., 6th floor, Boston, MA
Psychotherapy, 20, 45–57.
02215; e-mail: .
Hofmann, S. G., & Smits, J. A. (2008). Cognitive-behavioral therapy for
adult anxiety disorders: a meta-analysis of randomized placebo-controlled trials. Journal of Clinical Psychiatry, 69, 621–632.
Received: March 7, 2012
Kessler, R. C., Chiu, W. T., Demler, O., Merikangas, K. R., & Walters, E. E.
Accepted: May 9, 2012
(2005). Prevalence, severity, and comorbidity of 12-month DSM-IV
Available online 16 June 2012
Outline placeholder
Source: http://www.doe-psy.nl/therapiemateriaal/sociale_fobie/Social_Mishap_Exposures.pdf
Australasian Society for Immunology Incorporated PP 341403100035 ISSN 1442-8725 Infection Immunity and Immunogenetics Unit, Pathology and Laboratory Medicine, University of Western Australia Can a HIV patient who once progressed to AIDS ever regain a normal immune system on antiretroviral therapy (ART)? Why do some HIV patients beginning ART have an uneventful immune recovery, whilst others develop immune restoration disease? Are the effects of CMV similar in HIV patients, transplant recipients and healthy aging? Why is HCV disease more severe in HIV patients and what determines how HCV patients respond to therapy?
p911 Eggs-tra p914 Under fire: p916 Rebel with a evidence: Scientists NIH scientists say cause: Transgendered they feel punished researcher Ben Barres of proof for fertility for the misdeeds of fights for women in a few colleagues. Threat of pandemic brings flu drug back to life With an effective avian influenza vaccine production capacity to the limit. But Relenza,