Introduction
TABLE OF CONTENTS Revised 10/23/06
INTRODUCTION
Introduction . 1
Anthem
Mission and Philosophy . 3
UNDER 65 PRODUCT AND NETWORK DESCRIPTIONS
Blue Access ® PPO/ Alliance . 4
Access Choice PPO/ AllianceChoice . 4
Preferred® HMO/ BlueCHOICE. 4
UNDER 65 PRODUCTS Blue
Access /Blue Access Choice . 5
Access Economy/ Blue Access Choice Economy . 5
Blue Access Value/ Blue Access Choice Value . 5
Preferred® HMO . 6
HIPAA Blue Access . 6
Blue Short Term . 6
Lumenos® Consumer Driven Health Plans . 6
Specialty Products
Blue Preferred Term LifeTM . 7
UNDER 65 UNDERWRITING GUIDELINES
Adding Benefits (Upgrades) . 8
Address and Billing Changes . 9
Determination . 9
Attending Physician's Statement (APS) . 9
Billing and Payment Options . 10
Cancellation . 10
Certificate or Policy Delivery . 11
Child Only Policy . 11
Completion of the Application . 11
Death of a Certificate Holder. 12
Declination . 12
Deleting Benefits (Downgrades) . 12
Dependents Who Reach Age Limitation . 13
Divorce . 13 Dual
Effective Date Assignment . 14
Eligibility . 15 Full-Time
UNDER 65 UNDERWRITING GUIDELINES (Continued) List
Marriage . 16 Medical
Questionnaires. 17
Pregnancy . 18 Premium
Requirements .18-19
Reinstatements . 19 Rate
Increases/Renewals . 20
Requirements . 20
Surviving Spouse/ Dependents. 20
Tobacco/Non-Tobacco
Underwriting Opinion Form . 21
MEDICAL CONDITIONS AND RATING GUIDE
Medical Conditions and Rating Guide. 22 Key Points to Remember . 22 Medical Condition Ratings .23-32 Medical Conditions That Are A Decline.33-34 Medication Denials. 35
HEIGHT AND WEIGHT BUILD CHARTS
Males-Ages 13 & Over . 36
Females-Ages 13 & Over. 36
Super Preferred Build Chart. 37
MEDICAL QUESTIONNAIRES
Abnormal Pap Smear . 38
Arthritis . 41 Asthma/Allergy . 42
Attention Deficit Disorder . 43
Back/Spinal . 44
Colitis/Irritable Bowel Syndrome . 45
Diabetes . 46 Digestive . 47 Ear/Otitis . 48 Endometriosis . 49 Fibromyalgia. 50 Gout . 51
Heart Murmur/Mitral Valve Prolapse . 52
Hypertension . 53 Kidney/Urinary
Migraine . 56 Seizure/Epilepsy . 57 Thyroid . 58 Tumor/Cyst. 59 Ulcer. 60
ONLINE AGENT TOOLS
Introduction/Overview of Tools . 61
Individual Producer Site .62-63
Anthem Rate Generator (Rating CD) .64-65
AgentConnect and AgentServices .66-67
Agent Registration for Voice Signature . 68
Agent Data Entry and Voice Signature .69-70
VAMI (View and Administer Member Information) . 71
Online Order Entry System (Materials) .72-73
MISCELLANEOUS FORMS Application
Product Transition Chart.75
Underwriting Opinion Form . 78
OVER 65 PRODUCTS
Medicare Supplement Plans . 79
BlueMedicare Rx (Part D) . 80
Balance Budget Act (BBA) . 81
Medicare Supplement Guide. 83
IMPORTANT CONTACTS. 85
INTRODUCTION
The Individual Business Unit at Anthem Blue Cross and Blue Shield offers a diverse suite of
individual health coverage products exclusively to direct-pay consumers. This manual provides
guidelines intended to help writing agents solicit, write, and submit applications for individual
health coverage in the state of Missouri.
It is important to remember that these guidelines are for informational purposes only, and
should not be interpreted as a guarantee of underwriting action on any specific case. The
agent and applicant should be aware that the final decision regarding all underwriting actions-
including insurability, rating, and effective date assignment-will always be determined by the
Medical Underwriting department following a thorough assessment of each applicant's
morbidity risk. Various sources of information are used for assessing this risk; however, the
most important source is the application. Therefore, it is important to make sure each
application is complete and accurate.
The information contained in this manual is intended for internal use only and may not be
copied or distributed in any manner. The benefit descriptions are intended to be a brief
overview of some benefits available to Anthem members.
For Internal Use Only
ANTHEM BLUE CROSS AND BLUE SHIELD
Anthem Overview
Anthem, Inc. and WellPoint Health Networks, Inc. completed their merger on November 30, 2004.
WellPoint, Inc. serves approximately 34 million members though its Blue Cross and Blue
Shield operations in 14 states and its non-Blue branded operations in other states. The
company has over 42,000 associates nationwide.
About WellPoint, Inc.
WellPoint, Inc. is the largest publicly traded commercial health benefits company in terms
commercial membership in the United States. Headquartered in Indianapolis, Indiana,
WellPoint is an independent licensee of the Blue Cross and Blue Shield Association and
serves its members as the Blue Cross licensee for California; the Blue Cross and Blue Shield
licensee for Colorado, Connecticut, Georgia, Indiana, Kentucky, Maine, Missouri (excluding 30
counties in the Kansas City area), Nevada, New Hampshire, New York (as Blue Cross Blue
Shield in 10 New York City metropolitan and surrounding counties and as Blue Cross or Blue
Shield in selected upstate counties only), Ohio, Virginia (excluding the Northern Virginia
suburbs of Washington, D. C.) and Wisconsin and through HealthLink and UniCare. Additional
information about WellPoint is available at www.wellpoint.com.
Missouri
Anthem Blue Cross and Blue Shield is the trade name for, in most of Missouri, Healthy
Alliance® Life Insurance Company (HALIC), HMO Missouri, Inc., and RightCHOICE® Managed
Care, Inc. (RIT) (RIT, with certain affiliates, administers non-HMO benefits underwritten by
HALIC and HMO benefits underwritten by HMO Missouri, Inc.). These companies are
independent licensees of the Blue Cross and Blue Shield Association. Blue Cross and Blue
Shield are registered marks of the Blue Cross and Blue Shield Association.
For Internal Use Only
Mission and Philosophy
Our mission is to improve the lives of the people we serve and the health of our communities. At Anthem, we believe health care coverage should actually help people stay healthy. That's why we go beyond simply providing coverage. We help support and encourage our members' wellness by:
• Offering large provider networks that include many of the best physicians,
specialists, and hospitals in each area we serve.
• Encouraging members to have important preventive and health maintenance
• Including coverage for preventive and health maintenance care in many plan
• Providing programs to help members proactively manage chronic health
We work with physicians, hospitals, and other providers to help ensure that care is accessible, coordinated, timely, and provided in a manner and setting that promotes positive patient-provider relationships.1 1 Blue Cross and Blue Shield Association,
Brand Talk
MISSOURI PRODUCT AND NETWORK DESCRIPTIONS
B
LUE ACCESS PPO/ ALLIANCE
Blue Access is a preferred provider organization (PPO) product that utilizes the comprehensive Alliance network of physicians and hospitals. This plan does not require members to select a primary care physician (PCP) or obtain referrals. Blue Access features two levels of benefits: Network and Non-Network. Network care is paid at a higher benefit level. Non-network care is paid at a lower benefit level. Therefore, members have a greater financial responsibility if they obtain care at non-network providers. Blue Access members have access to network providers nationally and worldwide through BlueCard®.
BLUE ACCESS CHOICE PPO/ ALLIANCECHOICE
Blue Access Choice is a Missouri preferred provider organization (PPO) product that utilizes the select
AllianceChoice network of physicians and hospitals. The product is sold only in the city of St. Louis and
the following counties: St. Louis, St. Francois, St. Charles, Warren, Franklin, and Jefferson. This plan
does not require members to select a primary care physician (PCP) or obtain referrals. Blue Accesssm
Choice features two levels of benefits: Network and Non-Network. Network care is paid at a higher
benefit level. Non-Network care is paid at a lower benefit level. Therefore, members have a greater
financial responsibility if they obtain care non-network providers. Blue Access Choice members have
access to network providers nationally and worldwide through BlueCard®.
B
LUE PREFERRED HMO/ BLUECHOICE
Our Blue Preferred HMO product utilizes the BlueCHOICE network of physicians and hospitals, which
is available in approximately two-thirds of the Missouri plan area, including the St. Louis metro area,
Central and Southwest Missouri. This plan is an Open Access HMO, meaning no referrals or primary
care physician (PCP) selections are required. The product covers Network care only. Therefore, the
member has 100% financial responsibility for Non-Network care, except emergency services.
Members also have access to network providers nationally and worldwide through BlueCard®, for
urgent and emergency care situations.
Same Widespread Provider Networks
Previous Network Name
New! Network Name
AccessSM / Alliance
Blue AccessSM Choice/ AllianceChoice
Blue Preferred® HMO/ BlueCHOICE
Under 65 Health Insurance Product Overview
Blue Access® / Blue Access Choice
Blue Access and Blue Access Choice are PPO products designed to offer a broad range of benefits at an affordable monthly premium. Each offers three different plan options, with a choice of deductible levels. All plans have an unlimited lifetime maximum and offer network and non-network benefits. An Optional Maternity Rider is available. There are also 3 Rx options. All plans have a $25 office visit copay that applies to both primary and specialty care. The plan options and deductible levels are:
• Blue Access/ Choice 100 - 0% member coinsurance with deductibles of $500, $1,000, $2,500,
$5,000, $7,500 and $10,000.
• Blue Access/ Choice 90 – 10% member coinsurance with deductibles of $250, $500, $1,000
• Blue Access/ Choice 80 – 20% member coinsurance with deductibles of $500, $1,000, $2,500,
$5,000 and $7,500.
Blue Access Economy / Blue Access Choice Economy
Blue Accesss/ Blue Access Choice Economy are PPO products designed to help consumers obtain affordable health care coverage. These products have 4 deductible levels to help consumers tailor the monthly premium to their needs.
• Deductibles of $1,000, $1,500, $2,500 and $5,000.
• 30% coinsurance after deductible on covered services.
• 3 Rx options
• $30 copay for the first 3 office visits, then deductible and coinsurance for the fourth and any
subsequent visits.
Blue Access Value / Blue Access Choice Value
Blue Access Value/ Blue Access Choice Value are PPO products that can help consumers afford the protection they need against unexpected medical bills. These products feature 4 deductible options and comprehensive inpatient hospitalization benefits, but have more limited outpatient benefits to help lower the overall premium. The plan options are:
• Deductibles of $2,000, $3,000, $5,000, $10,000
• 30% coinsurance after deductible on covered services
• 3 Rx options
• $30 copay for the first 2 office visits. The third, and any subsequent visits, the member is
responsible for 100% of the billed charge.
Blue Preferred® HMO
The Blue Preferred HMO is an open access HMO product that offers low out-of-pocket cost and no annual deductible. The plan offers:
• $25 copay for office visits
• $150 copay for emergency room services
• 10% member coinsurance for other services, such as inpatient hospital care
HIPAA Blue Access
HIPAA Blue Access is a guarantee issue product for eligible individuals who may not qualify for our regular plans because of their health. Applicants must be able to answer "yes" to the 5 HIPAA eligibility questions listed on the application. The plans are:
• HIPAA Blue Access 100 - $1,000 deductible, 0% member coinsurance, Rx $15/$30/$60/25%
• HIPAA Blue Access 80 - $1,000 deductible, 20% member coinsurance, Rx $15 generic only
• Blue Preferred HMO 90 – no annual deductible, 10% member coinsurance, Rx
Blue Short-Term
For individuals who are temporarily without health coverage, Bluesm Short-Term is an affordable plan
designed to provide protection from unexpected health care expenses for a short period of time (30-180
days). This product provides a choice of five deductibles and 20% member coinsurance. The deductible
options are: $250, $500, $1,000, $2,500 and $5,000.
Lumenos® Consumer Driven Health Plans (CDHP)
Anthem's Lumenos Consumer Driven Health Plans provide innovative coverage that will help
customers improve and maintain their health and provide greater control over their health care dollars.
Three Lumenos CDHP plans are available for effective dates of January 1, 2007 and later. All offer
100% coverage for nationally recommended preventive care services and provide members with
access to online tools and information they can use to become more informed and knowledgeable
health care consumers.
Lumenos Health Savings Account Plan (Lumenos HSA) combines a tax-advantaged member-
funded Health Savings Account with a qualified high deductible health plan (HDHP).
• 0% and 20% coinsurance options available • Individual/family deductible options (0% coinsurance): $1,500/$3,000, $3,000/$6,000,
• Individual/family deductible options (20% coinsurance): $1,500/$3,000, $3,000/$6,000
Lumenos Health Incentive Account Plus (Lumenos HIA Plus) combines traditional health coverage
with a plan-funded Health Incentive Account, along with additional dollar incentives if members use
certain tools and services to maintain and improve their health.
• 0% and 20% coinsurance options available • Individual/family deductible options (0% coinsurance): $2,500/$5,000, $5,000/$10,000,
• Individual/family deductible options (20% coinsurance): $2,500/$5,000
Anthem HIA funding: For Lumenos HIA Plus only, Anthem contributes the following amounts
annually to the Health Incentive Account:
• $500 for individual plans, allocated quarterly
• $1,000 for family plans, allocated quarterly
Healthy rewards incentives: Additional Anthem contributions to the Health Incentive Account can
be earned by participating in the following incentive programs:
• Completing or updating an online Health Assessment: $50 per family, per year.
• Enrolling in and graduating from the Personal Health Coach program: $100 for enrolling and
$100 for graduating.
• Completing our Smoking Cessation Program: $50 per covered person, per lifetime.
• Completing our Weight Management Program: $50 per covered person, per lifetime
Lumenos Health Incentive Account (Lumenos HIA) provides traditional health coverage and Health
Incentive Account funded by specified dollar incentives members can earn if they use certain tools and
services to improve and maintain their health.
• 0% and 20% coinsurance options available • Individual/family deductible options (0% coinsurance): $1,000/$2,000, $2,500/$5,000,
• Individual/family deductible options (20% coinsurance): $1,000/$2,000, $2,500/$5,000
Healthy rewards incentives: Anthem contributions to the Health Incentive Account can be earned
by participating in the following incentive programs:
• Completing or updating an online Health Assessment: $50 per family, per year.
• Enrolling in and graduating from the Personal Health Coach program: $100 for enrolling and
$100 for graduating.
• Completing our Smoking Cessation Program: $50 per covered person, per lifetime.
• Completing our Weight Management Program: $50 per covered person, per lifetime
LUE PREFERRED TERM LIFE
Blue Preferred Term LifeTM offers consumers affordable life insurance coverage for a specified period of
time. It is available with most Anthem Individual medical plans. There are no additional forms to fill out.
• Benefit Options are: $15,000, $25,000 and $50,000
Note: Please refer to the Life section for enrollment guidelines.
D
Dental Blue helps cover the cost of maintaining good oral health, an important component of overall health and well being. Dental Blue pays the full cost of diagnostic and preventive care when a network provider is used. It can also help offset the cost of major dental care. The plan can be purchased in conjunction with a medical benefits plan, or as a stand-alone product. Plan highlights:
• Diagnostic and Preventive Care – no deductible and no waiting period when performed by a
network provider
• Basic Dental Care - $50 annual deductible and six (6) month waiting period
• Major Dental Care - $50 annual deductible and twelve (12) month waiting period
Note: Please refer to the Dental section for enrollment guidelines.
UNDER 65 GUIDELINES
Adding Benefits (Upgrades)
Members can upgrade or downgrade benefits twice per year: once at renewal and once more
within 12 months. To add benefits (upgrades) an application must be sent to Underwriting. In
order to secure an effective date, the application must be received by the requested effective
date. Otherwise, the effective date will be assigned by Underwriting for a future date.
Agent Tips - Members may qualify for a better rate tier if they were:
1. Previously issued as tobacco users and are now 12 months tobacco free. 2. Previously issued at a higher tier due to build, but have maintained a lower weight for 12
3. Previously issued at a higher rate due to a medical condition that has now been resolved
or has not required treatment for a specified period of time.
A Change of Coverage application must be filled out and is subject to complete Medical
Underwriting.
Adding Dependents
Any current member may add a "newly acquired" dependent due to birth, adoption, marriage, or
legal guardianship within 31 days of the qualifying event (i.e., date of birth, date of adoption,
date of marriage, or date of legal guardianship placement).
Newborns or Newly Adopted Children
Coverage is guarantee issue for the first 31 days for dependents who are newborns and newly
adopted children of the primary policyholder or spouse. In order to continue coverage past the
31st day, the policyholder must direct Anthem to add the dependent either by calling Customer
Service or submitting the request in writing. The newborn will be added at the existing family risk
tier. In the case of newly adopted children, a copy of the document awarding the policyholder or
spouse court-appointed custody must be provided. In addition, an affidavit attesting to the
adoption must be completed and accompany the application.
If notification is not received within 31 days, coverage will not be extended beyond the 31st day.
To obtain coverage after the 31st day, a new application, indicating "add dependent(s) to current
coverage," must be submitted and full underwriting will be required. In order to secure an
effective date, the application must be received by the effective date requested. When
completing the application, please take the following steps:
• In Section A, check the box: "add dependent (s) to current coverage" and provide the
current policy number
• Provide the member's name, social security number, and address in Section B
• Section D must be completed
• Complete Section K – answer all medical questions for all members being added
Moving a newborn to a ‘child only' policy requires submitting an application to Underwriting. In this case, unlike adding a newborn to an existing family policy, the first 31 days are not free. If approved, the newborn will receive the next available effective date following receipt of the application.
Other Dependents
Adding a dependent other than a newborn or newly adopted child (e.g., dependents as a result
of marriage or court-appointed legal guardianship) requires a new application. The dependent is
subject to full medical underwriting and the effective date will be assigned according to the
regulations set forth under the Effective Date Assignment section of this guide.
For dependents added as the result of marriage, the application must be received within 31
days of the qualifying event (i.e., date of marriage) in order for coverage to be effective as of the
date of the qualifying event. The dependents will be subject to full underwriting. The addition of
dependents as a result of marriage may result in a new policy risk tier.
For dependents added as a result of court-appointed legal guardianship (if the legal guardian is
someone other than the natural parent of the child(ren), proof of the guardianship will be
required, (i.e., court-appointed custody and affidavit) and must be submitted with the
application.
If the application and required proof are submitted within the first 31 days of
guardianship placement, adding the dependent is guarantee issue, and the dependent will be
added at the existing policy risk tier. Full medical underwriting will be required if the application
is submitted more than 31 days after the qualifying event.
Note: The affidavit required for adoptions and court-appointed guardianships can be
found in the Miscellaneous Forms section of this manual.
Address and Billing Changes
Members may make address, billing, and automatic bank draft changes verbally by contacting
Customer Service; by submitting a written request; or by contacting their agent. Automatic
deductions will begin on the next billing period after the receipt date of the request to use bank
draft.
Age Determination
The applicant's age on the effective date of coverage will determine the correct rate. If the
effective date is changed, the rate could also change. Premium due to age increases will be
effective at the member's annual renewal of the policy.
Attending Physician's Statement (APS)
Medical records and an APS may be requested by Underwriting to supplement the information
on the application. An APS may be requested if the application indicates a condition that
requires more detailed information or if medical conditions are not fully explained on the
application and/or medical questionnaires. An APS may also be requested based on internal
claims information.
A
mandatory APS will be requested if an applicant is over age 55 and
is not replacing prior
coverage. Underwriting will send the request to the applicant and notify the agent if medical
records are needed. It is the applicant's responsibility to have these records sent to Anthem.
The applicant is also responsible for any costs incurred in obtaining medical records.
Billing and Payment Options
The first month's initial premium is
required with the application. Once the underwriting process
is complete and the applicant's final rate has been determined, any remaining balance due will
be included in the next month's bill.
Billing Options: Members may choose paper billing or automatic bank drafts either monthly,
quarterly, semi-annually, or annually.
Payment Options:
Initial payments can be made by credit card (MasterCard, Visa, Discover, or American Express), a one-time automatic bank draft, or by check.
Subsequent/Ongoing payments can be made by automatic bank draft, paper check, or over the phone by calling Customer Service for a one-time credit card or bank draft. Members may also issue an electronic check through their bank's website.
Cancellation
All new policies may be cancelled by the applicant, back to the effective date of coverage, if the
cancellation request is submitted within 31 days after the applicant receives the contract or
certificate, or accesses it online, whichever is earlier. If no claims have been submitted, Anthem
will refund all premiums to the applicant.
A policy will be automatically cancelled when the member transfers to another Anthem
Individual plan. The cancellation will be effective at midnight on the day prior to the effective
date of the new coverage.
Note: Individual policies are not automatically cancelled when transferring to or from an Anthem
Group plan. In this case, the member must request cancellation of the Individual coverage. If a
member moves out of state, medical and dental coverage will be transferred to another Blue
plan; however Life coverage (if any) will continue.
All other cancellation requests must be received 30 days in advance of the cancellation date. If
proper notification is not given, the member will be asked to pay the final month's bill or have the
policy lapse for nonpayment if payment is not made. Customer Service will accept cancellation
requests verbally over the phone; the customer can also submit a written request to cancel
coverage.
Members with multiple policies (i.e., medical, dental, and/or life coverage) must specify which
policies are to be cancelled. The other policies will remain effective. If the member does not
specify which policies should be cancelled, all active coverage will be cancelled.
Life Policies only: Life coverage will be automatically cancelled on the last day of the month in
which a covered member turns age 65. Eligible spouses and dependents under age 65 may
continue their coverage under the Life Insurance policy.
Note: See "Death of a Policyholder" for policies related to death cancellations.
Certificate of Coverage or Policy Delivery
The member will receive, along with their ID cards, instructions on how to obtain their certificate
of coverage or policy via the internet. The member will also receive a postcard that can be
returned if a paper copy of the certificate is requested.
Child Only Policy
Coverage may be written for a child(ren) only. The parent and/or guardian must sign the
application and is considered to have contracted with Anthem Blue Cross and Blue Shield to
provide insurance to the covered child(ren). Applications may be submitted for a child(ren) only
if the child(ren) are under age 18. Newborns cannot be written on a Child Only Policy until they
have been released from the hospital. If approved by Underwriting, the youngest child will be
enrolled as the policyholder.
Completion of the Application
The most important source of underwriting information is the application. The underwriting
process can often be completed with a simple review of the application. Each question on the
application must be
specifically answered by each applicant and all responses must be
accurately and completely recorded on the application. All applications must be completed in
ink and the writing agent must verify that the applicant answered the questions, and signed and
dated the application. The applicant must initial any erasures or corrections. All "YES" answers
to medical questions
must be fully explained along with the name, address and telephone
number of all doctors consulted by the applicant.
Conditional Coverage
Coverage does not become effective until Underwriting approves the application. Therefore, an
applicant's current coverage should not be cancelled until they receive an approval from
Anthem Blue Cross and Blue Shield.
Note: See Effective Date Assignment section for information on available effective dates.
Counter Offers
Anthem Blue Cross and Blue Shield may decline one family member, but offer coverage to others. Or, the applicant may be extended a counter offer for coverage that may include a different rate, plan, or higher deductible level. Counter offer letters for a higher rate band only will offer alternatives for higher deductibles, along with the premiums for those deductibles. Counter offer letters will be mailed to the applicant for approval and signature. The agent will also be copied on the letter. The applicant must sign and return the counter offer letter to the Underwriting Department within 15 business days of the date on the letter. Some applicants may also accept the counter offer using voice signature capability. The applicant will be instructed in the letter to call a specific telephone number to accept the offer. Only applicants who receive this number in their letter have the option to use the voice signature. Applicants who wish to downgrade benefits or request a future effective date can indicate this on the counter offer letter and return it in writing to the Underwriting Department. All plans may be offered without drug coverage as a counter offer from Underwriting.
Death of a Certificate Holder
Written or telephone notification to Anthem Blue Cross and Blue Shield is required after the
death of a policyholder. Termination of the policy will be effective the day after the policyholder's
death; this is to ensure eligible benefits are paid up to the date of death and any unused
premiums will be refunded. If Anthem Blue Cross and Blue Shield is notified of the death of the
policyholder after 91 days following the date of death, a copy of the death certificate will be
required for a refund of any unused premiums.
Declination
If a health condition(s) or other underwriting criteria makes it impossible for coverage to be
offered on any basis, the application is declined, any initial payment submitted with the
application will not be processed. If the initial payment is submitted via check, the original check
will be destroyed and will not be returned to the applicant. The applicant will receive a letter from
Anthem Blue Cross and Blue Shield advising them of the reason for declination. Agents are sent
a copy of the declination letter as well.
Deleting Benefits (Downgrades)
Any deletion of benefits (including an increase in the deductible level or removal of an optional
rider) is considered a ‘downgrade' in benefits. Policyholders can upgrade or downgrade benefits
twice per year: once at renewal and once more within 12 months. Policyholders can make
changes by calling their agent, contacting Customer Service, or completing a
Downgrade/Policy Change Form. The change will be effective on the first day of the month after
notification is received by Anthem Blue Cross and Blue Shield, or on a specified future date if
requested by the policyholder.
Note: The Downgrade/Policy Change Form can be found in the Miscellaneous section of this
manual as well as on the Individual Producer Site.
Dental Coverage
Dental Bluesm, a dental PPO product, is available as a stand-alone product in addition to medical coverage. This product provides coverage for Diagnostic and Preventive Care, as well as Basic and Major Dental Care. There is no waiting period for Diagnostic and Preventive Care. There is a 6-month waiting period for Basic Dental Services, and a 12-month waiting period for Major Dental Care. The applicant must be covered for dental before a spouse or any dependents can be eligible for dental coverage. If dental coverage is requested for children, all of the dependents must be covered and a premium will be charged for each child. Each member with active dental coverage will be charged a premium. Members who cancel their medical coverage may keep dental coverage active, if they wish. For combined billing, dental must have the same renewal date as Medical. If both medical and dental coverage is requested, one application should be submitted for both plans rather than submitting separate medical and dental applications.
Dependent Coverage
Eligible dependents of the policyholder or spouse include unmarried children up to the end of
the calendar year in which they turn 19, or to the end of the calendar year in which they turn 24
if they qualify as full-time students. Premium is charged for up to 3 dependent children on a
medical policy. On the application, the primary applicant will be asked to list all dependents
beginning with the eldest.
Dependents Who Reach Age Limitation
A covered dependent who loses eligibility upon attaining the maximum age may apply for
his/her own coverage. A new application must be completed by the dependent and received
within 31 days of losing eligibility. If the application is received within the 31-day period, the
applicant will be guaranteed the same plan (or similar plan if the original plan is no longer
offered), with no lapse in coverage. Pre-existing credit and credit for any deductible amount met
under the original plan will be applied to the new plan.
If the application is received after the 31-day period, the applicant will be subject to Medical
Underwriting approval. Coverage will begin according to the regulations set forth under the
Effective Date Assignment section of this guide.
Divorce
When a covered person (including a dependent) loses coverage due to divorce, he or she may
apply for his or her own coverage. A new application must be completed and received within 31
days of losing eligibility. If the application is received within the 31-day period, the applicant will
be guaranteed the same plan (or similar plan if the same plan is no longer offered), with no
lapse in coverage. Pre-existing credit and credit for any deductible amount met under the
original plan will be applied to the new plan.
If the application is received after the 31-day period, the applicant will be subject to medical
underwriting approval. Coverage will begin according to the regulations set forth under the
Effective Date Assignment section of this guide.
Dual Coverage
If an Anthem Blue Cross and Blue Shield individual member has health coverage under another policy once his/her Anthem individual policy is effective, and the member stated that no other health coverage would be in effect on the effective date of the Anthem policy, Anthem reserves the right to terminate the Anthem coverage. Rescission of the Anthem individual coverage will be retroactive up to 90 days or the policy effective date, at Anthem's discretion.
Effective Date Assignment
Applications will be assigned an effective date of either the 1st or the 15th of the month following the application received date. Exceptions for other dates can be made for continuous coverage only. Continuous coverage is defined as no break in coverage from a policy in effect immediately prior. If the application is received by Anthem within 10 days of the signature date and the signature date was on or prior to the requested effective date, coverage will begin on the date requested. (This applies as long as the requested effective date is not more than 90 days after the application signature date.) If the application is received by Anthem after 10 days following the signature date, and the signature date was on or prior to the requested effective date, coverage will begin on the next available effective date.
Example:
Application received within
Requested effective date June 1st
Signature date May 27th
10 days of signature date
Anthem received June 6th
Member will receive June 1st effective date
Application received after
Requested effective date June 1st
10 days of signature date
Signature date May 27th
Anthem received June 9th
Member will receive June 15th effective date (the next available date)
NOTE: In cases where an application is closed because Anthem did not receive requested
information, and subsequently the information is received, the original requested effective date
cannot be honored and a new effective day will be assigned. The new effective date will be the
next available effective date (1st or 15th) after the information is received. The signature on the
application is only valid for 90 days.
Short-Term
The application must be received by the requested effective date. If no effective date is
requested, the coverage, if approved, will be effective on the received date. The effective date
cannot be more than 90 days after the application signature date. Short-term coverage can be
selected in daily increments, with a minimum of 30 days of coverage and a maximum of 180
days at one time.
Short-Term coverage is not renewable; however, individuals may purchase additional Short-
Term policies, up to a maximum of 360 days of total coverage within a 12-month period.
Applicants must be able to answer "NO" to the current medical questions on the application. A
new application must be completed and sent to Anthem for approval, along with the appropriate
premium.
Any condition that occurred during an earlier contract term will be treated as a pre-existing
condition under subsequent contracts.
Please refer to the pre-existing condition section for
additional information on.
Short-Term policies can be cancelled if the policyholder requests cancellation 30 days prior to
the cancellation date.
Applicants who meet the following criteria are eligible to apply for individual coverage:
; Cannot be eligible for Medicare.
; Must be between the ages of "newborn" and age 64. Persons over age 65
who are not
eligible for Part A of Medicare may be considered for an Individual under 65 policy and are subject to full medical underwriting. To be considered for coverage, the applicant must provide a reason for not being eligible for Medicare.
; Must be a resident of the state in which they are applying for coverage.
; Cannot currently pregnant or an expectant parent.
; Must be a legal U.S. resident
If an existing member moves out of state, he or she may lose eligibility and coverage may be
terminated.
Full-Time Students
Coverage for full-time students within the age limit (age 24) continues as long as they are
enrolled in an accredited educational facility and are classified as full-time students by the
school. Coverage ends when they no longer meet the eligibility guidelines for dependents;
however, they may be eligible for guaranteed acceptance for the same coverage (or similar
coverage if the same coverage is no longer offered), or lesser benefits if Anthem Blue Cross
and Blue Shield is notified within 31 days of the loss of eligibility. This applies only to
dependents coming off their parents' Individual policies. Pre-existing credit met under the
original plan will be applied to the new plan. Refer to the contract for specific eligibility
information.
ID Cards
New members will receive ID cards approximately 3 to 5 days after enrollment, along with
instructions on how to obtain a certificate of coverage. New members will also receive a
separate Welcome letter shortly thereafter.
Life Coverage
Health coverage applicants may apply for the Preferred Choice Term Life coverage. New
applicants must meet Anthem's medical underwriting guidelines to qualify. Term Life coverage
is not offered as a stand alone product.
The benefit options are: $15,000, $25,000, and $50,000. The $50,000 option is not available to
applicants under the age of 19. If the $50,000 option is selected by an approved applicant under
the age of 19, coverage will default to $25,000. Applicants under the age of one year are not
eligible for Life Insurance.
If Term Life coverage is selected for dependent children,
all of the dependent children must be
insured for the same benefit amount.
Active Term Life coverage will be automatically cancelled on the last day of the month of the
covered member's 65th birthday. Spouses and dependents may continue Term Life coverage, if
eligible.
List Bill
Criteria for List Billing
¾ List billing is a billing option for Individual coverage that allows premiums to be paid through
a third party (such as an employer) for a group of individuals. It is not intended for use by families. List bill arrangements must consist of a minimum of 2 members in order to be set up and maintained. Covered individuals must pay 100% of their own premium. The third party only facilitates payment of the individual health insurance premium.
Applying for Coverage
¾ The "Request for List Billing Arrangement" form must be completed and all individuals to be
enrolled in the List Bill arrangement must be listed.
¾ Each individual must then complete an individual application for coverage and sign the
Permission to Provide List Bill Arrangement form. A copy of the authorization form must be attached to each application. Failure to comply will result in delays in the enrollment process. The writing agent must sign the "Request for List Billing Arrangement."
¾ All individual applicants must request the same billing due date and bill cycle (monthly,
quarterly, semi-annual, annually).
¾ Please do not submit payment with application.
Adding to an Existing List Bill
¾ To add a new member to an existing List Billed account, the individual must complete an
individual application for coverage and attach a copy of the "Request for List Billing Arrangement" form (including the name of the new member), and the "Permission to Provide List Bill Arrangement" form (Disclaimer) and send the completed forms to the writing agent. This form must include the Parent Group Number found on the monthly bill summary. Please note that the billing date for a new member will be the same as the other Group members on the arrangement (i.e., 1st or the 15th of the month).
¾ In order to add a dependent to an existing individual policy, the policyholder must submit an
application to Anthem through his or her agent. The same effective date will apply: 1st or the 15th of the month.
Cancellation of List Bill Affiliation
¾ Cancellation of a List Bill account must be received by Anthem in writing from the list bill
administrator 30 days prior to the cancellation date requested. If the cancellation is due to a death, and the cancellation notice is received 90 days after the death, a copy of the death certificate Is required
¾ Upon cancellation of a List Billed account, all individual policyholders billed within that
arrangement will begin receiving monthly billings statements at their home address. Any refunds due will be issued directly to the policyholder.
Marriage
Current members who wish to add a spouse due to marriage must submit a new application. The spouse is subject to full medical underwriting. Both the current member and the spouse must sign the application. The new application must be received by Anthem Blue Cross and Blue Shield within 31 days of marriage in order for coverage to begin on the date of marriage. If the application is after 31 days of marriage and Underwriting approves the application, the effective date will be the next available effective date (1st or 15th of the month).
Medical Questionnaires
Medical questionnaires should be used to supplement "yes" answers indicated on the application. Questionnaires should be completed, signed and dated by the applicant; however, an agent may obtain the applicant's information over the telephone, sign and date the questionnaire, and indicate with whom they spoke. In most cases, an Attending Physician's Statement (APS) is not necessary if a questionnaire is fully completed and submitted. Agents may obtain the questionnaires listed below in the Medical Questionnaire section of this manual or from the Individual Producer website:
Abnormal Pap Smear
Seizure/Epilepsy
Attention Deficit Disorder
Heart Murmur/MVP
Colitis/Irritable Bowel
Member Self Serve
Members have the ability to manage their health benefits any time, day or night, through the anthem.com website. Members should select the member tab, and enter their home state. Members who log in to MyAnthem and select
MyServices will be able to:
• find a doctor or hospital
• order a new ID card
• view benefits
• check a claim status
• check the formulary
Plan Transfers
If a current Anthem Blue Cross and Blue Shield member moves outside the state of residence in which the policy is held, the Blue Cross and Blue Shield Association, an association of independently licensed Blue Cross and Blue Shield plans, requires the member to transfer to a local plan in the new state of residence. It is the policyholder's responsibility to apply for a new policy within that state. A letter will be sent to the member requesting permission to send a letter to the other plan. Medical and dental coverages may be transferred to another Blue plan; however, Term Life coverage can remain active with Anthem unless the policyholder requests cancellation. Dental policies will be cancelled and transferred to the new local plan.
Coverage is NOT available to any applicant if the applicant or spouse is currently pregnant
(whether or not they are to be covered on the policy), or
IF they are an expectant parent;
however, children of the expectant parent(s), or sibling of an expectant minor, may be written
independently.
Premium Requirements
The first month's premium must accompany the application. Initial payments can be made via
credit card (MasterCard, Visa, Discover, or American Express), check or authorization for a one-
time bank draft.
If the initial premium is submitted via check, we will convert that check to a one-time bank
draft/electronic transaction and destroy the original check; however the premium amount will not
be deducted from the applicant's bank account unless and until the application is approved. If
the application is declined, the applicant will receive a declination letter indicating the reason
coverage was denied.
For subsequent premium payments, applicants have two billing options – (1) automatic bank
draft and (2) paper billing. Members can choose to be billed monthly, quarterly, semi-annually or
annually. If premiums will be paid by a third-party administrator, a list bill arrangement may be a
third billing option. See the List Bill Section of this manual for additional information.
Automatic Bank Draft: Premium payments will be automatically deducted from a checking or
savings account. Applicants requesting Automatic Bank Draft must complete and sign the Automatic
Bank Draft Authorization section included on the application. If premium payments will be deducted
from a checking account, a voided check (not a deposit slip) must accompany the application. If
premium payments will be deducted from a savings account, a blank deposit slip showing the Routing
Number of the financial institution must accompany the application. Members can also request
Automatic Bank Draft for an existing policy by calling Customer Service and providing their bank
account information.
Although every effort is made to set up Automatic Bank Draft payments with the appropriate financial
institution as quickly as possible, processing delays sometimes occur. If Automatic Bank Draft is
requested on a new application and a processing delay prevents Anthem from collecting any initial
premium(s), the initial Automatic Bank Draft payment, once established, will include the current
premium and any back premiums owed as a result of the delay. In this event, members will receive a
letter notifying them of the total initial Bank Draft amount, and giving them the option of canceling the
withdrawal. Members who request Automatic Bank Draft on an existing policy may receive a direct bill
at their home address if the policy is not paid up through the current billing period at the time the
Automatic Bank Draft becomes effective.
Bill Direct: Billed at the member's home address monthly, quarterly, semi-annually or annually.
List Bill: If an individual applicant will be making premium payments through his or her employer (via
payroll deduction) Anthem can arrange to bill the employer directly each month via a list bill. The List
Bill option requires 2 or more employees to be set up.
See the List Bill section of this manual for
additional information. Short-Term
Advance Payment: Full premium for the entire term of coverage in the form of check, money order or
credit card.
Automatic Bank Draft for Monthly Billing: $10 additional monthly fee will be assessed (Short-Term
product only).
Monthly Billing: $10 additional monthly fee will be assessed (Short-Term product only). (At least one
month's premium is required with the application)
Pre-Existing Conditions
All Plans excluding Short Term and Blue Preferred HMO
A pre-existing condition is defined as any condition that was diagnosed or treated within 12
months prior to the effective date of coverage, or that produced symptoms within 12 months
prior to the effective date of coverage, that would have caused an ordinarily prudent person to
seek medical diagnosis or treatment.
Pre-existing conditions are only covered after the coverage has been in-force for 12 consecutive
months following the effective date of coverage. Credit for a prior carrier's coverage may be
given, if that coverage was continuous to a date not more than 63 days prior to Anthem's receipt
of a completed application.
Prior coverage can be from a group, individual, or short-term contract. (Medicaid qualifies as
prior coverage) but it must be a major medical type policy. To apply for pre-existing credit, the
applicant must complete the section for prior coverage information on the application. Credit is
not available if the prior coverage was an indemnity plan, hospital only plan, or supplemental
policy.
Short-Term
A pre-existing condition is defined as any condition that was diagnosed or treated within 24
months prior to the effective date of coverage, or that produced symptoms within 24 months
prior to the effective date of coverage, that would have caused an ordinarily prudent person to
seek medial diagnosis or treatment. For Short-Term policies only, a Pre-existing condition is
also defined as any condition that occurred during an earlier contract term.
Pregnancy on the effective date of coverage is also considered a pre-existing condition. Pre-
existing conditions are not covered for the term of the certificate.
Blue Preferred HMO
No waiting period for pre-existing conditions applies to members on this policy.
If a current member allows his/her contract to lapse and wishes reinstatement, he/she will be automatically eligible if the following guidelines are met: 1. Request for reinstatement is received within 90 days of the cancellation date and money is
received in full by the 90th day after the members paid to date.
2. No more than one previous cancellation for non-payment on current, continuous coverage
within the last 12 months.
3. No more than three bad checks in the past 12 months. If a member does not fall within above guidelines, a new application for coverage must be completed and Medical Underwriting will apply. If approved, a new effective date for coverage will be established.
Rate Increases/Renewals
Members are typically notified at least 30 days in advance of any intended rate increases.
Approximately 15 days prior to the customer notification, agents will receive a listing of their
client members who will be affected by the rate increase. Renewals occur approximately 12
months from the policy effective date. Renewal dates for all members will be the first of the
month in which the policies were originally effective. For example, a policy with a July 15th
effective date will have a July 1st annual renewal date. On the renewal date, the policyholder will
receive applicable age and product rate changes.
Signature Requirements
The primary applicant (and spouse, if applying), must sign and date the application. The
parent/guardian of a dependent child applying must sign and date the application. Failure to
obtain any of the above signatures will result in the return of the application. The application will
expire 90 days from the signature date if health coverage has not been approved by the end of
the 90-day period.
Surviving Spouse/Dependents
If a covered spouse or dependents (if any) lose coverage due to the death of the primary
policyholder, the spouse may continue the contract in his/her name. Anthem must receive
notification within 31 days following the primary policyholder's date of death.
If notification is received after the 31-day period, a new application must be submitted and the
applicant will be subject to Medical Underwriting approval. If approved, coverage will begin on
the next available effective date (1st or 15th), or a later date if requested.
Telephone Interviews
The applicant should be aware that the Underwriting Department may conduct a telephone
interview to verify information on the application, or to obtain additional details or missing
information for the purpose of underwriting.
Tier Rating
Anthem offers tier-rated coverage on all Under 65 Products, except Short-Term products. Super Preferred, Preferred, Standard 1, Standard 2, Modified 1 rates are available based upon health status, height/weight proportion, and tobacco usage. Generally, underwriters will permit tobacco users with no other ratable health history for any plan at a risk tier of Standard 1; however, approval and final rate tier placement is always determined by Medical Underwriting. Any changes to the rate quoted by the applicant's agent, will be communicated to the applicant and agent by the Underwriting Department. This will be a counteroffer letter, which must be signed by the applicant and returned to the Underwriting Department within 15 business days of the date on the letter. In order to qualify for the Super Preferred risk tier, the applicant and/or spouse must complete the Healthy Lifestyle section on the application. The Super Preferred rate is only available for an applicant and spouse 18 years of age or older. The applicant(s) must be able to answer "yes" to
all the questions and fall within a restricted build chart.
(This chart can be found in the
height;/weight section of this manual) The Healthy Lifestyle questions are in addition to the other
medical questions on the application. The Super Preferred Rate is a quotable rate. Children are
not eligible.
The tiers equate as follows:
decrease/
Please indicate on the application the tier you have quoted for all applicants dependents.
Tobacco/ Non-Tobacco Use Rate
Preferred rates may be available to any applicant, spouse or dependent that has not used ANY
form of tobacco products within the past twelve (12) months.
Generally, tobacco users (applicant and spouse) with no other ratable health history are eligible
for any plan at a risk of Standard 1.
Generally, non-tobacco users (applicant and spouse), with no other ongoing medical conditions
and no tobacco use for at least 3 years are eligible for any plan at a Super Preferred tier.
Note: Please refer to the section titled Tier Rating for all other rating tiers.
Underwriting Opinion Form
The Underwriting Opinion Form is designed to be used when agents face a difficult question
that may not be addressed in the Medical Condition Guide or if there is uncertainty as to
whether we would consider the application or decline coverage.
Underwriting will make a determination based only on the information provided on this form, and
then return the form to the agent. If an application is submitted following the return of an
Underwriting Opinion Form, please attach form to your completed application.
Withdraw Application
To withdraw an application, Anthem Blue Cross and Blue Shield must be notified by the applicant or agent. The request can be submitted in writing, by fax, or by calling Anthem.
MEDICAL CONDITIONS AND RATING GUIDE
Introduction
Medical Underwriting is the process of estimating the morbidity risk of an applicant for health coverage. Various sources are used for estimating this risk; however, the most important is the application. This guide is intended to help the writing agent solicit and write applications for coverage, and should not be interpreted as a guarantee of underwriting action on any one specific case. The agent and applicant must be aware that the final decision regarding insurability and possible effective dates is always made by the Medical Underwriting Department. This section includes some medical conditions and the probable underwriting action for applicants with such conditions. This is not an all-inclusive list and final decisions will be
determined by Medical Underwriting. Medical conditions preceded by a "#" designate that a Medical Questionnaire is required. These questionnaires should be completed and submitted with the application. Conditions are classified and rated as follows:
Super Preferred Rate Band
(Only available for applicant and
spouse/Healthy Lifestyle Questionnaire required)
Preferred Rate Band
(non-tobacco use)
Standard One Rate Band
(tobacco use)
Standard Two Rate Band
Modified Rate Band
Individual Consideration
Medical Records may be required
Cost of Medication
KEY POINTS TO REMEMBER • Decisions for applicants contemplating surgery will be postponed until surgery is completed.
• Applicants with several conditions may be declined due to the combination of conditions.
• Please refer to the Build Chart for applicants, spouses, and all dependents to determine the
"baseline" rate band
before factoring in any medical conditions.
• Decisions for expectant parents will be postponed until after delivery.
• All ratings will depend on the benefit plan and deductible selected.
• If health information is discovered that is not on the application, it will be referenced as PHI
(Protected Health Information) and cannot be released to the agent per HIPAA guidelines. Correspondence will be handled between the applicant and Underwriting.
• Prescription drug usage will be rated for dosage and cost. This could result in an offer of no
prescription coverage.
MEDICAL CONDITION RATINGS
Condition
On Accutane/Amnesteem/Claravis/Sotret. DEC Others, rate based on medications . STD 1/COM
Acquired Immune Deficiency Syndrome or Aids Related Complex . DEC
#
Alcohol / Drug Dependency
< 5 years since last treatment . DEC > 5 years since last treatment . IC/APS
#
Allergy
Mild (seasonal), minimal prescription usage . PREF Mild (seasonal), multiple medications . STD 1/COM Moderate year round and/or allergy shots . STD 1/STD 2/COM Severe (Allergy Shots/Multiple Medications) ER visits.IC/MOD 1/COM
Alzheimer's. DEC
Amputation (not caused by disease)
Fingers / toes . PREF Other limbs or with prosthesis .MOD1
Angina. DEC
#
Anxiety (Mental Health Questionnaire)
Current treatment with medication . STD1/COM Medication and/or current counseling sessions w/weekly, bi-weekly visits. DEC Hospitalization within 1 year. DEC Others . IC
#
Arthritis
Osteoarthritis, no med/OTC med, in hip, knee, shoulder .STD1 Osteoarthritis, no med/OTC, other sites. PREF Osteoarthritis, on prescription medication or no med/OTC in spine or neck . MOD1/COM Rheumatoid Arthritis. DEC With joint replacement done age 60-64 and over one year ago .MOD1 With joint replacement done under age 60 or under one year ago . DEC
Ascites, (all cases). DEC
Acute attack within 6 months . DEC Acute attack > 6 months, meds as needed or meds taken w/in one year.STD1 Acute attack > 6 months, meds taken daily . MOD1/COM No medication or treatment > one year. PREF
MEDICAL CONDITION RATINGS
Condition
#
Attention Deficit Disorder (ADD)
Rated based on medication .COM
#
Back Strain/Sprain
Single occurrence, < 1 year, full recovery .STD1 Recurrent episodes or with ongoing chiropractic care . IC/APS
#
Bronchitis (Allergy and/or Asthma Questionnaire)
Mild, Single Occurrence, Not Hospitalized, Full Recovery . PREF Moderate, recurrent episodes, infrequent attacks . IC/STD1 Severe, with hospitalization and/or numerous attacks/medications . DEC Chronic bronchitis within 2 years . DEC
Bursitis
Single occurrence <1 year .STD1 Unresolved, current treatment. DEC
#
Cancer (Tumor Questionnaire)
Metastatic Cancer . DEC Internal Cancer < 5 years last treatment . DEC Others .STD1
Carpel Tunnel Syndrome
Unoperated With Symptoms within 1 year . DEC Unoperated no symptoms within 1 year . PREF Operated, resolved. PREF
Cataracts
Unoperated .MOD1Operated, released from care . PREF
Cerebral Palsy
< age 20 . DEC > age 20 . IC/APS
Cholesterol (fasting)
Diet Controlled, < 200 .PRE No medication, reading 200 – 260 or with medication . MOD1/COM Reading > 260 or with or without medication . DEC
Cirrhosis of the liver . DEC
Chronic Fatigue Syndrome. IC
Chronic Obstructive Pulmonary Disease
(COPD, Emphysema) . DEC
MEDICAL CONDITION RATINGS
Condition
#
Colitis
Mild, Irritable Bowel Syndrome, normal weight .STD1 Moderate, recurrent episodes . IC/MOD1 Severe, chronic, underweight. DEC Ulcerative Colitis (Crohn's Disease). DEC
Coronary Insufficiency
Angina within 5 years . DEC Angioplasty within 5 years. DEC Bypass Grafting (CABG) within 5 years . DEC Myocardial Infarction (Heart Attack) within 5 years . DEC Any of above after 5 years . IC
Coronary Occlusion
Angina . DEC Angioplasty. DEC Bypass Grafting (CABG) . DEC Myocardial Infarction (Heart Attack) . DEC
Crohn's Disease . DEC
Cystic Fibrosis . DEC
Cystitis
Single episode, recovered. PREF Recurrent episodes .STD1
#
Depression, not Manic or Psychotic (Mental Health Questionnaire)
Current treatment with medication . STD1/COM Medication and/or current counseling sessions w/weekly, bi-weekly visits. DEC Hospitalization within 1 year. DEC Others . IC
Deviated Septum
Not Operated, with symptoms .MOD1 Operated, full recovery . PREF
#
Diabetes
Diet controlled, adult onset, excellent control, no other related conditions .STD 1/APS Oral medication, excellent control, no other related conditions. MOD 1/APS Diet/Oral/Insulin, Fair to Poor control or with other related conditions . DEC Juvenile Diabetes. DEC
Disc Disorders (see Spinal Disorders)
Diverticulitis / Diverticulosis . STD1 to MOD1
MEDICAL CONDITION RATINGS
Condition
Drug Treatment - See Alcohol/Drug Dependency
Emphysema. DEC
#
Endometriosis
No current symptoms or symptoms controlled .STD1 Current symptoms or laser treatment < 1 year. DEC Operated (hysterectomy) . PREF
#
Epilepsy (Seizure/Epilepsy Questionnaire)
Any Seizure < 3 Years . DEC Grand Mal, no seizure > 5 years .MOD1 Others, no seizure > 3 years .STD2
#
Fibrocystic Breast Disease (Tumor/Cyst Questionnaire)
Benign, definite diagnosis, treatment/testing < 1 year .STD1 Benign, definite diagnosis, treatment/testing > 1 year . PREF
#
Fibromyalgia
No medication or symptoms within the year . PREF Use of anti-depressant medication(s) . MOD 1/COM Chronic with pain/narcotic medication. DEC
Friedreich's ataxia . DEC
Gallbladder Disease
Unoperated, with Current Symptoms . DEC Operated, complete recovery . PREF
<5 years . DEC 5 – 8 years, no complications.MOD1 > 8 years, no complications.STD1
Gastric Reflux (GERD)
Single Episode, No Medication . PREF On maintenance medication .COM
Glaucoma
Mild, controlled by drops .STD2 With past surgery .MOD1
#
Gout
No attack/treatment within 2 years. PREF
With attack/treatment within 2 years…………………………………………. STD2/COM
MEDICAL CONDITION RATINGS
Condition
#
Graves Disease (see Thyroid Disorders)
Heart Attack (Myocardial Infarction) within 5 years . DEC
After 5 years. IC
#
Heart Murmur
Insignificant/asymptomatic, no treatment .STD1 Others . IC/APS
Heart Palpitations
Symptoms controlled, no surgery within 6 months.STD2 Symptoms uncontrolled or surgery in last 6 months . DEC
Hemophilia. DEC
Hemorrhoids
Unoperated, with symptoms < 2 years.STD1 Operated, full recovery . PREF
Hepatitis
A and B, within one year .IC/APS A and B, over one year . PREF C/Chronic or Alcoholic. DEC
Unoperated, with current symptoms . DEC Operated complete recovery . PREF1 Hiatal, unoperated, no medication in last year .STD1 Hiatal, unoperated, with medication in last year. MOD1/COM
Diagnosed within one year or on daily medication . MOD1/COM No medication or medication with outbreaks only . STD1/COM
#
High Blood Pressure (Hypertension Questionnaire)
Uncontrolled, Malignant, or over 3 medications . DEC Well controlled, 2-3 medications . STD2/ MOD1 Well controlled, one medication .STD1/ STD 2
Hodgkin's Disease
Within 10 years . DEC Over 10 years.STD1
Huntington's
Chorea . DEC
MEDICAL CONDITION RATINGS
Condition
#
Hyperthyroidism (see Thyroid Disorders)
Mild, controlled .STD1 Severe or uncontrolled . IC
Benign Cause. PREF Due to Cancer (non metastatic) < 10 years . DEC
Infertility Treatment (current). DEC
Interstitial Cystitis
Chronic. MOD1/COM No symptoms/treatment >1 year . PREF
#
Irritable Bowel Syndrome (See Colitis)
Joint Replacement
Done age 60-64 and over one year ago .MOD1 Done under age 60 or under one year ago . DEC
Kidney Failure or Dialysis . DEC
#
Kidney Stones
Multiple within one year. DEC Multiple > one year OR one episode within year.STD1 After one year. PREF
Leukemia
Within 10 years . DEC Over 10 years.STD1
Maintenance Medications for any condition
Will be underwritten based on number of medications and costs . IC/COM
#
Melanoma (Tumor/Cyst Questionnaire)
Within 10 years . DEC Over 10 years.STD1
Metastatic
Cancer . DEC
Meningitis (viral or bacterial)
MEDICAL CONDITION RATINGS
Condition
Menstrual Disorders . IC
#
Migraines
Infrequent, one per year or less often . PREF Moderate to severe with chronic medication . MOD 1/DEC
#
Mitral Valve Prolapse (MVP) (Heart Murmur / Mitral Valve Prolapse Questionnaire)
No Symptoms Or Treatment Required(except antibiotics with dental work) . PREF
No symptoms within last 2 years, controlled on medication.STD1
With symptoms within last 2 years . DEC
Motor or Sensory Aphasia . DEC
Multiple Sclerosis . DEC
Muscular Dystrophy . DEC
Myasthenia Gravis . DEC
Myotonia . DEC
Obesity (see Height/Weight Build Charts)
Obsessive Compulsive Disorder. DEC
Open Heart Surgery within 5 years . DEC
After 5 years. IC
Organ Transplant Recipient/Candidate . DEC
No history of fractures . STD1/COM With history of fractures . DEC
#
Otitis Media (Ear/Otitis Questionnaire)
Single Episode, Recovered . PREF Multiple episodes .STD1
Single episode, resolved . PREF Single episode, unresolved or recurrent episodes .MOD1
Pacemaker Implantation. DEC
Palpitations (see Heart Palpitations
Pancreatitis
Single episode, > 1 year, no residuals . IC/APS Recurrent/multiple episodes/alcoholic. DEC
MEDICAL CONDITION RATINGS
Condition
#
Pap Smears (Cervical Dysplasia, Cervicitis)
Class I or II - clean pap obtained . PREF Clean pap NOT obtained . DEC Class III or more .IC/DEC
Parkinson's Disease . DEC
#
Peptic Ulcer (Ulcer Questionnaire)
Unoperated, current symptoms . DEC Unoperated, no current symptoms, current treatment . STD2/COM Operated within one year, resolved .STD1 Operated more than one year, resolved . PREF
Phlebitis
Current symptoms or treatment . DEC No current symptoms/treatment but symptoms/treatment within 3 years .MOD1 No symptoms/treatment within past 3 years .STD1
Polycystic Kidney Disease. DEC
Polycystic Ovaries
Both ovaries removed . PREF No current symptoms on glucophage/hypoglycemic med.MOD1 No current symptoms on hormone replacement or BCP.STD1 With current symptoms . DEC
Pregnancy
Premature Infant
Birth to one year of age . IC/APS
Prostate Disorders (Benign)
Hypertrophy (BPH),unoperated, no symptoms on medication . STD1/COM Hypertrophy (BPH),unoperated, current symptoms . MOD1/COM Operated, complete recovery . PREF
Elevated PSA, no follow-up or repeat test . DEC
Elevated PSA, follow-up test normal .STD1 Prostate Disorders (Malignant) <5 years. DEC
Prostatitis
Acute within one year, resolved, no current symptoms or treatment .STD1 Acute within one year, unresolved or Chronic within 1 year.MOD1 Chronic after 1 year.STD2
MEDICAL CONDITION RATINGS
Condition
#
Psychotic Disorders (Mental Health Questionnaire)
Psychosis / Schizophrenia . DEC Manic Depression / Bipolar . DEC
All others, severe but not Psychotic or Manic…………………………………………. DEC
Quadriplegia (Paralysis) . DEC
#
Rheumatoid Arthritis (see Arthritis). DEC
Skin
Basal cell . PREF Squamous cell within 1 year .MOD1 Squamous cell, 1 to 5 years .STD1 Squamous cell, over 5 years . PREF
Skin Disorders (psoriasis, rosacea)
Infrequent attacks, no regular meds.STD1 Moderate/maintenance meds, not Methotrexate or Plaquenil. STD2/COM Severe/ultralight therapy or use of Methotrexate or Plaquenil . DEC
Sleep Apnea
Normal height/weight, controlled on CPAP .MOD1 Others .STD1
#
Spinal Disorders (Back Pain Questionnaire)
Mild Curvature (Scoliosis), No Symptoms Or Treatment .STD1 Moderate to severe curvature, unoperated or operated <1 year. DEC Operated to repair curvature, complete recovery,1-3 years.MOD1 Operated to repair curvature, complete recovery,>3 years.STD1 Disc disorder, unoperated, < 5 years . DEC Disc disorder, operated < 1 year . DEC Disc disorder, operated, full recovery, 1-3 years.MOD1 Disc disorder, operated, full recovery, >3 years.STD1
Stroke (Cerebral Infarction, Hemorrhage, Embolism, Thrombosis) witihin 5 years . DEC
After 5 years. IC
Syringomyelia . DEC
Temporomandibular Joint Syndrome (TMJ)
Unoperated . IC Operated, no residuals, recovered . PREF
Tendonitis
Current treatment . DEC Resolved < 1 year .STD1 Resolved > 1 year . PREF
MEDICAL CONDITION RATINGS
Condition
#
Thyroid Disorders
Hyperthyroidism, Adequately Controlled . PREF Graves Disease, I-131 or operated, recovered . PREF Goiter, present . IC
Tonsillitis
Single episode, fully recovered . PREF Chronic, requiring surgery . DEC
Varicose Veins
Operated < 2 years .STD1 Operated, > 2 years complete recovery . PREF Unoperated, current symptoms/treatment.MOD1
Wilson's Disease . DEC
MISSOURI DECLINES
• Connective Tissue Disease,
Poliomyelitis(current)
• Leukemia < 10 years
Leukoencephalopathy
AIDS/AIDS Related Complex
• Alcohol/Drug
attack, bypass, etc.)
• Within 5 years of treatment
• Mediterranean
• Cushing's Syndrome w/in 5
(Thalassemia Major)
Melanoma, within 10 years
Dermatomyositis
• Aneurysm (Cerebral or
Diabetes, Insulin dependent
Angina within 5 years
Drug Treatment w/in 5 years
Ankylosis(current)
• Neiman Pick Disease (Lipidosis)
Any condition for which
testing or surgery is
• Endocarditis
Neurofibromatosis
Occlusion of Cerebral Arteries
Epilepsy / any seizure < 3
• Aphasia, Motor or Sensory
• Open Heart Surgery within 5
• Arthritis - Rheumatoid
• Organ Transplant recipient
• Osteogenesis
• Gallbladder Disease /
Atresia(current)
Gastric Bypass w/in 5 years
Brain Damage (Organic)
• Glomerulonephritis
• Buerger's Disease
(Thromboangitis
Disease-coronary
• Burkett's Tumor (Malignant
• Pneumoconiosis
• Cancer-Most internal < 5
• Heart Attack within 5 years
• Pneumocystis
years last treatment
Pneumocystis carnii infections
• Cardiomyopathy
• Polyarteritis
Hemochromatosis
• Polycythemia
• Cerebral Palsy under age 20
• Hepatitis, chronic or C
• Polymyositis
Charcot-Marie Tooth Disease
• Post-Inflammatory
Hodgkin's Disease < 10
(COPD/Emphysema)
• Psychosis Organic Brain
Cirrhosis of Liver
• Huntington's
Pulmonary Heart Disease,
Cleft Lip / Palate Uncorrected
• Hydrocephalus
• Hydronephrosis, present or
Pulmonary Embolism, current
• Quadriplegia
• Congestive Heart Failure
Failure/dialysis
• Reyes Syndrome within one
• Rheumatoid Arthritis • Saracoma,
• Schizophrenia • Scleroderma • Senile, Pre-Senile Organic
• Shunts • Sickle Cell Anemia • Silicosis
• Spinocerebellar
• Stents • Stroke within 5 years • Syringomyelia • Tabes
(Cerebral Lipidosis)
• TIA – Transcient Ischemic
Attack within 5 years
• Transplanted
• Thalassemia,
• Thromboangitis
Thrombocytopenia Purpura
• Transient Organic Psychotic
• Transposition of the great
• Tuberculosis
Recklinghasusen's
Disease (Neurofibromatosis)
• Werlhof's Disease (Purpura,
Thrombocytopenia)
• Wilson's Disease
Medication Denials
Application is denied if any applicant is taking or has taken any of the following medications within the last twelve months*: Abacavir
Hydroxychloroquine
Lymphocyte Immune
* Any medication not on this list should be investigated in order to determine the underlying medical condition for which the medication was prescribed.
** Will consider after off medication for 3 months. *** Will consider after off medication for 6 months.
MISSOURI
BUILD CHART – MALES AGES 13 AND OVER
Preferred
Standard 1
Standard 2
Modified 1
BUILD CHART - FEMALES
AGES 13 AND OVER
Preferred
Standard 1
Standard 2
Modified 1
Super Preferred Healthy Lifestyle Questions and Build Chart
Online Capabilities Introduction
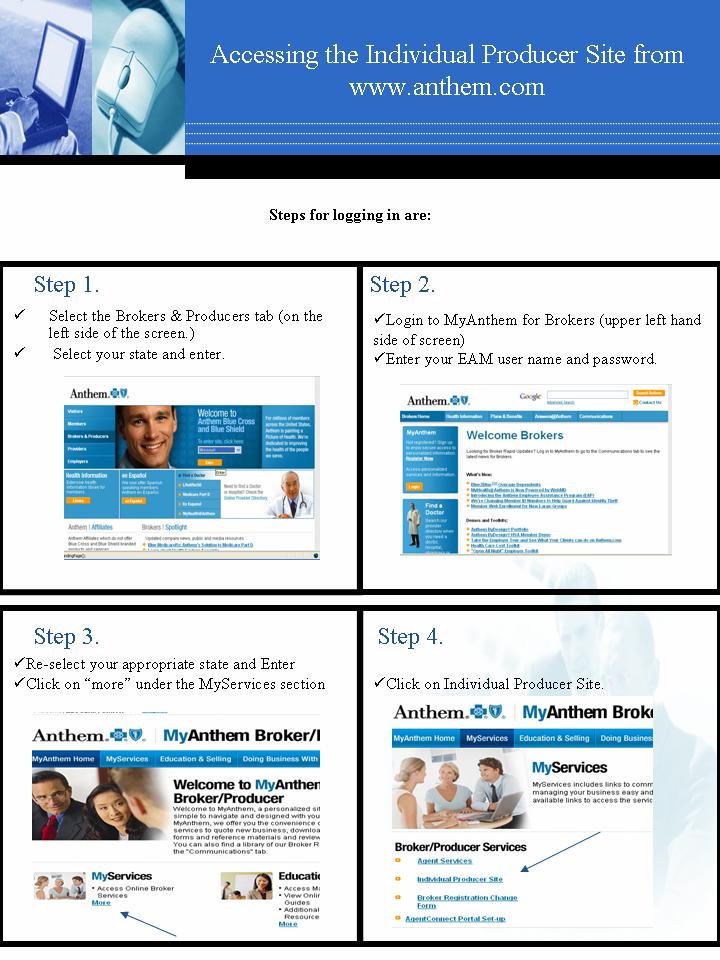
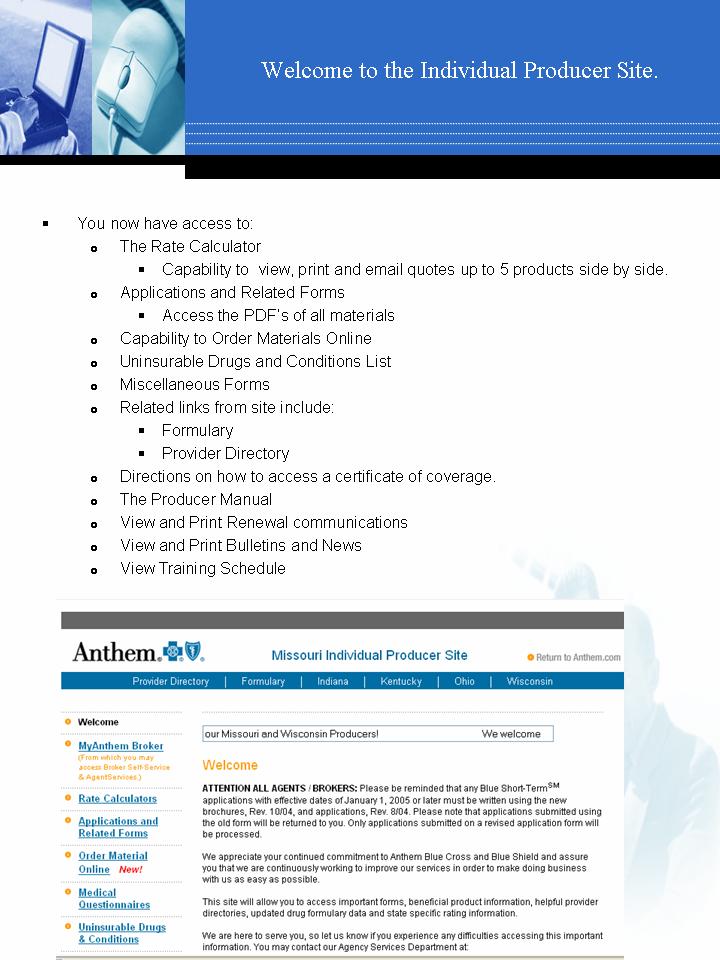
The purpose of this section is to guide you through the various online tools that are available to you, the agent/broker. These tools will assist you with:
• Helping you find a suitable plan for your clients and apply for coverage online
• Monitoring your business
• View and update member information
Overview of Rating Tools
The
Individual Producer Site can be accessed via and will allow you to
quote rates, order materials, view PDFs of all materials, read broker news, and access any
information needed to write Individual products. You can save and email quotes to your clients
as well. Utilizing this site does require that you have an internet connection at all times.
Refer to page 62-63 for steps to accessing this tool.
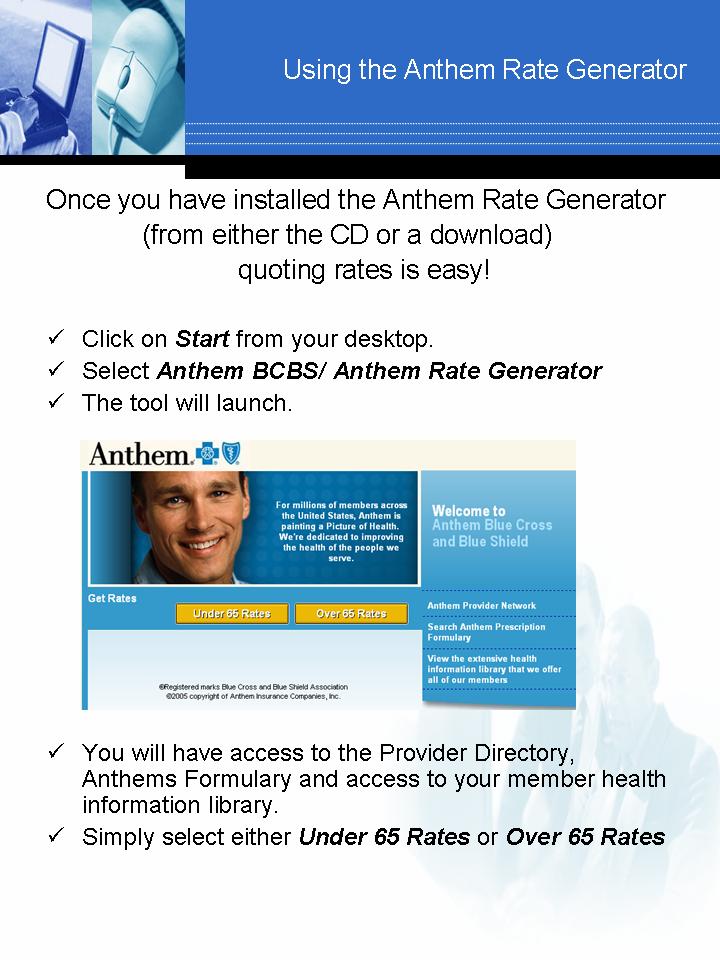
The
Anthem Rate Generator can be installed to your computer from a CD or a download.
(Please contact Producer Support for the link)Once this tool has been installed on your
computer, you have capability to quote products, save/store the quotes, and email them to your
clients. Updating the software is also easy. You will receive a communication when rates
change and when the new rates are available to be installed. Simply follow the instructions and
the new rates will be updated to your computer. Utilizing this rating tool requires only that you
have and internet connection; therefore this tool can be used from your laptop while in a client's
home to make sure you have the most up-to-date rates.
Refer to page 64-65 on steps to using this tool.
Overview of Other Tools
Help your clients find a plan and apply for coverage online via our
AgentConnect tool, a
co-branded website featuring your own personal information .66-67
Monitor your business and view your clients' applications, billing information etc., via our
AgentServices tool. 66-67
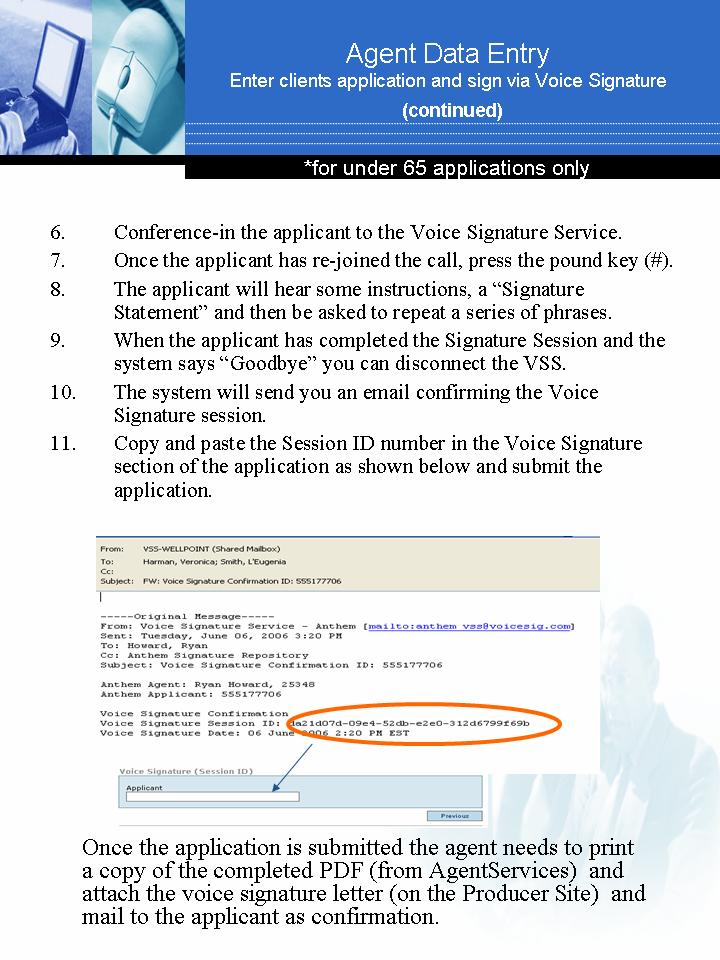
Instructions for
Voice Signature Agent Registration . 68
Enter and submit your clients' applications for them and
attach a voice signature……… .69-70
View your clients' certificates/contracts and order a new id with
VAMI… ………. 71
Order your own supplies through our
Anthem Online Order Entry System (OES) and receive
notification when materials are shipped. 72-73
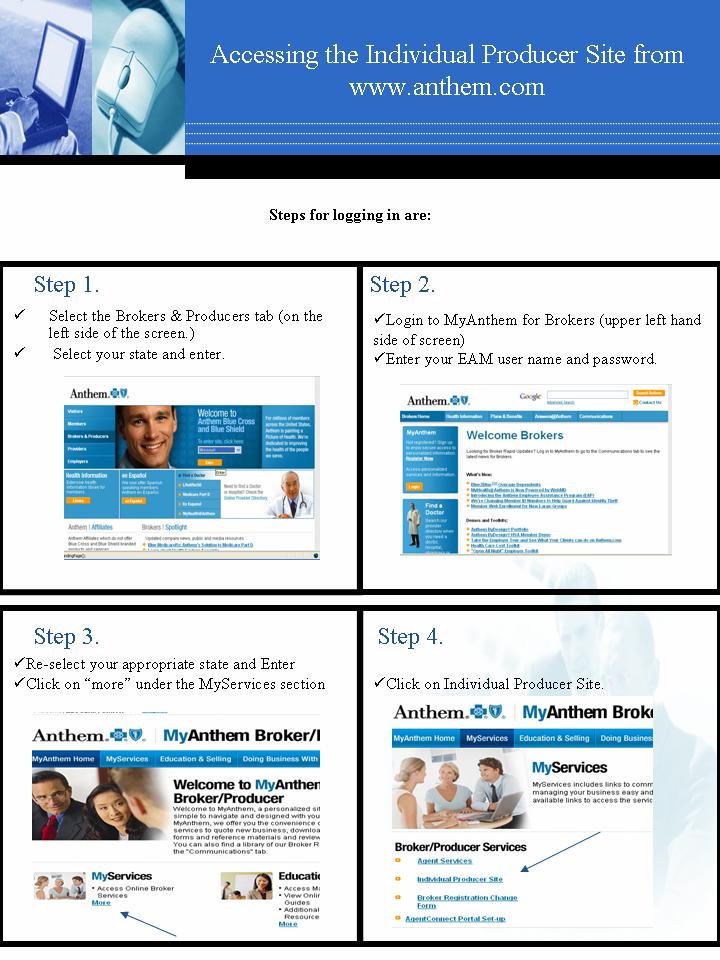
If you do not have a Username and Password, please select "Register Now" and follow instructions to
obtain access. Your Username and Password will be emailed to you within 7-10 business days.
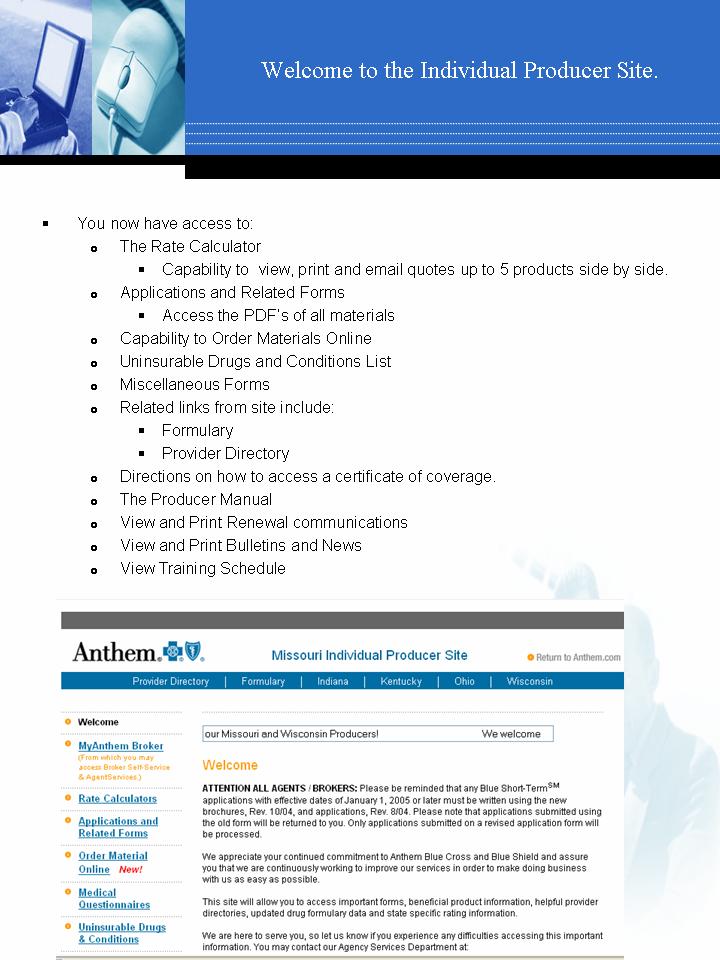
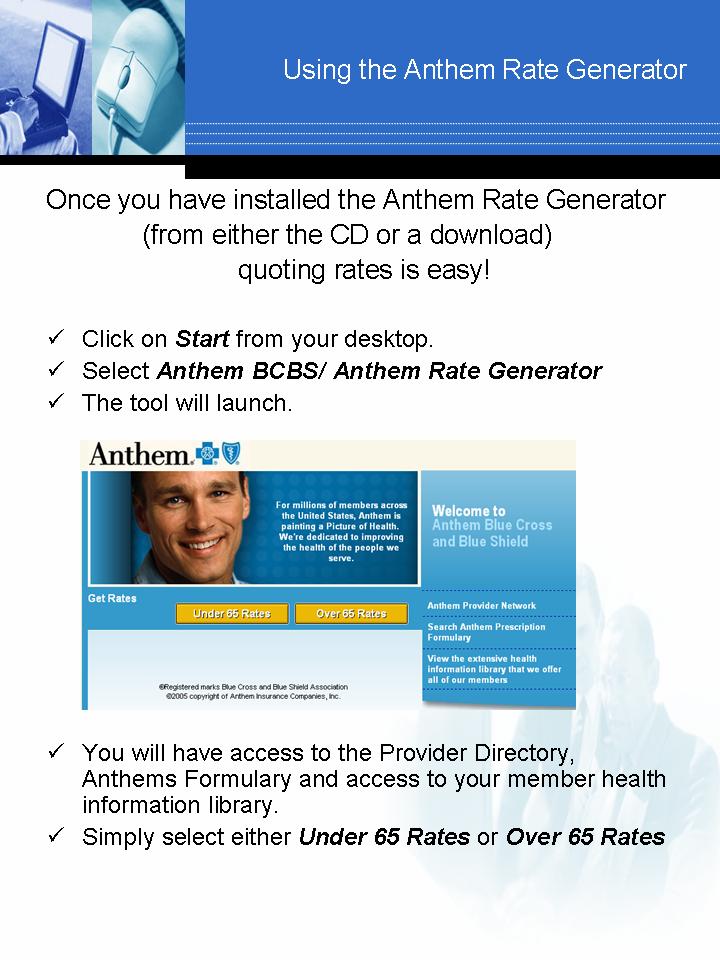
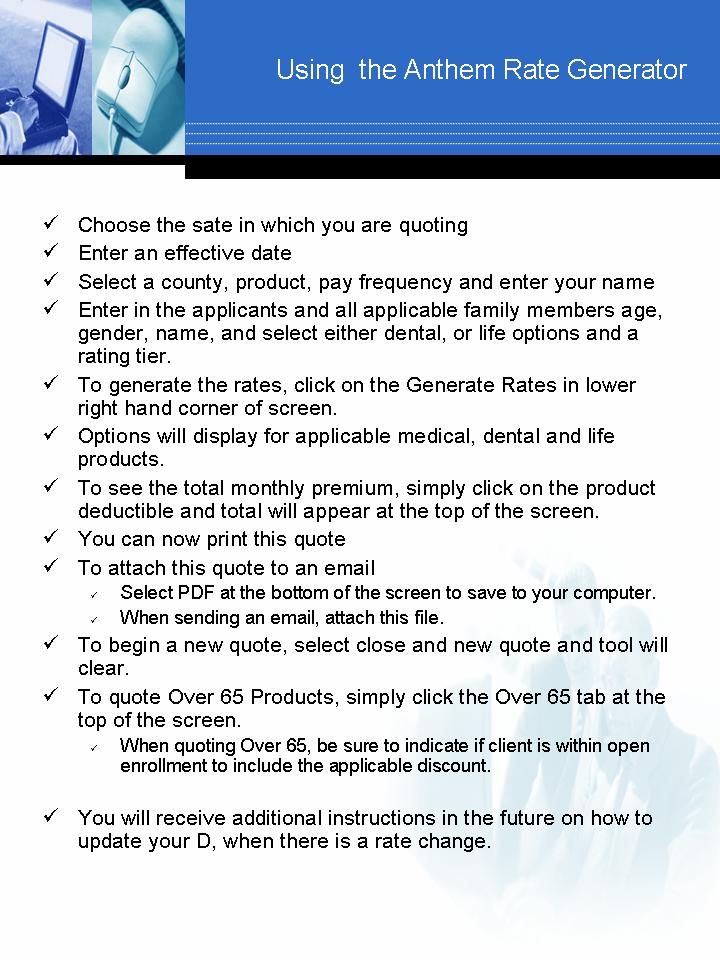
Instructions for Voice Signature ServiceSM Agent Registration
In order for Agents to use the Voice Signature Service to acquire Voice Signatures for
Anthem health insurance applications, they must first be provided a Voice Signature
Agent ID.
Agents are issued an Agent ID as a result of completing the online registration process
The registration process requires that the Agent enter their Anthem Agent Code.
Registration step-by-step:
1. Click on the following link, or copy and paste it into the address window of your
2. Enter your Anthem Agent Code in the field provided. 3. On the Agent Registration page – correct or add any missing information in the
required fields. Take special care to be sure that your email address is entered correctly. Create a secure password that is at least 8 characters; contains upper and lower case letters; contains at least one numerical character; and contains at least one special character.
4. Once your registration is complete, you will be provided an eight-digit Agent ID to
be used with the Voice Signature Service. The system will automatically send you a welcome email (at the email address you provided) that will include your Agent ID along with instructions for using the Voice Signature Service. Print out and save this email for future reference.
5. Call the Voice Signature Service and conduct a test transaction to confirm that
you are properly registered in the system. For the test transaction, use your Agent ID and the "test" Applicant information as follows - Phone Number: 1234567890 Last 4 digits of the SSN: 1234. Respond to the Voice Signature prompts as though you are the Applicant so you can experience the process. The Voice Signature Service will then send a Voice Signature confirmation email to your registered email address.
Congratulations, you are now ready to start using the Anthem Voice Signature
Service!
Once, you have completed you agent registration,you will be provided an Agent ID.
The Central Region telephone number you will always call to obtain a voice
signature for an application is: (877)-339-8092
For instructions on how to obtain a voice signature, please refer to the
following page in this manual; Agent Data Entry page.
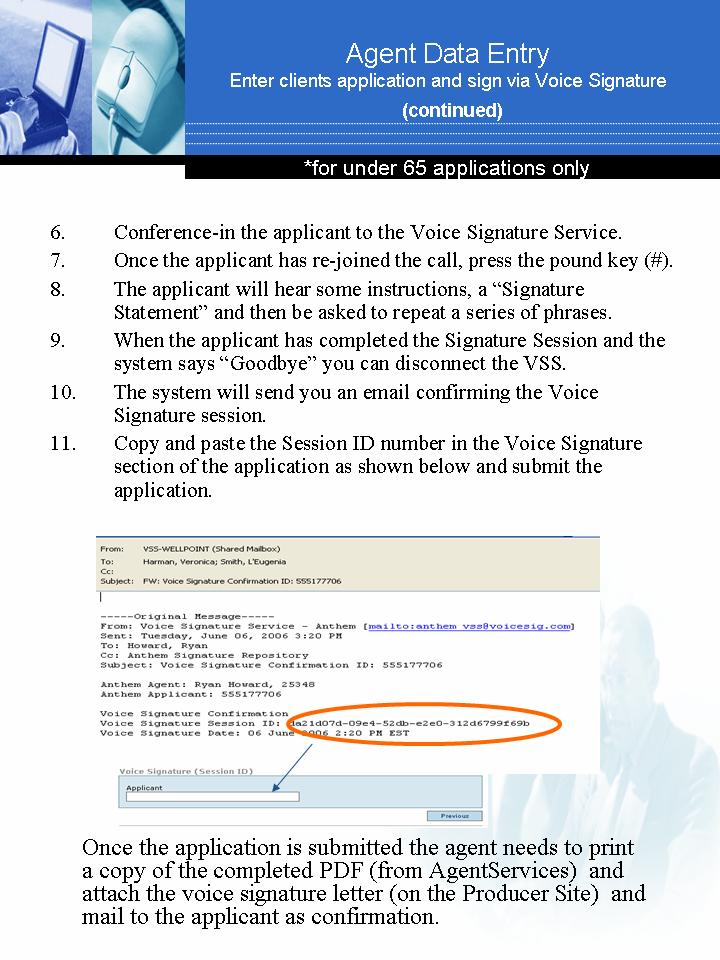
OES Common User Errors
Order Your Sales Materials Online
1. Received only one of the items ordered.
Please make sure you hit the UPDATE button after entering the quantity. The quantity amount defaults to one and you will not receive the expected quantity. Please make sure you confirm your order on the Confirmation Order screen prior to exiting the system.
2. Receiving multiple UPS emails.
UPS assigns tracking numbers per box, and not per order; therefore, you will receive as many UPS tracking numbers as the number of boxes they need to expect.
3. Shipped to the wrong address.
You need to confirm the default address in the account information section. You can add another address which will override the default.
4. Did not get e-mail confirmation.
You need to confirm the default email address in the account information section. At the time of order placement, you can add one additional e-mail address.
5. Items are not in OES/ I can't find item in OES.
1) To find the Kits category, click on the word "Anthem."
2) Type in part of the item description and the Quick Find
feature will pull a more narrowed list.
3) Only products authorized for the agent by state and/or
product certificate are visible.
6. I did not receive all the materials I ordered.
At the time of order placement, you are notified if the materials are on backorder.
A Good Reminder! You can review order content and shipping address on the last
screen before confirming the order. Changes can be made before confirmation.
MISSOURI A
PPLICATIO N CH
FORM NEEDED
COMMENTS
Downgrade/Policy
Policyholder can either call customer service
Add newborn within first 31 days of life to
and give information on child and request
parent(s) policy.
child be added permanently, or submit the
Individual Enrollment
Not guaranteed issue; if approved, next
Add newborn to sibling policy at anytime.
available effective date after app is received
Individual Enrollment
Underwriting applies; if approved, the next
Add newborn after 31st day.
available effective date after app is received
Individual Enrollment
Besides application, need Affidavit for Special
Add adopted child.
Dependent and a copy of the document
awarding court-appointed custody.
Individual Enrollment
Add any other dependent/spouse.
Individual Enrollment
Changing from HMO to non-HMO product
Downgrade/Policy
Policyholder can submit form or send signed
Delete dependent.
letter to Anthem. Will be deleted effective on
receipt date of letter.
Letter to Anthem signed by policyholder.
Delete policyholder and keep coverage on
Enrollment will set up coverage in spouse's or
spouse/dependents.
dependent's name, if requested.
Will accept verbally from the policyholder or
Downgrade/Policy
agent. The policyholder can also complete
the Downgrade/Policy Change Form or
submit a request in writing.
If policyholder does not want a rate review or
Policyholder wants to combine separate
Individual Enrollment
isn't requesting an upgrade, medical
policies into one.
questions don't have to be answered.
Claims and medical history are reviewed.
Rate review: Policyholder wants to remove
Change of Coverage
exclusion rider or try for better rate due to
change in medical history, lost weight, stopped using tobacco.
Change of Coverage
Upgrades, excluding HMO to non-HMO
product and vice versa.
PRODUCT TRANSITION CHART
The following information applies during the transition from Blue Cross Blue Shield of Missouri to Anthem Blue Cross
and Blue Shield.
CLIENT ACTION
FORM NEEDED
COMMENTS
Request move to new
Claims and medical history are
Anthem product prior to
reviewed. Clients moving to
Louisville, KY 40233-7810
"transition only" deductibles
cannot move to that product
Fax #: 800-884-9931
early—to keep that deductible they must wait until their renewal date. They can request to move early to another actively sold product/deductible.
Request an Anthem
Requested product/deductible
product other than the
must be actively sold; claims
product offered prior to
Louisville, KY 40233-7810
and medical history are
Fax #: 800-884-9931
Request upgrade to a new
Requested product/deductible
Anthem product on or after
must be actively sold; claims
Louisville, KY 40233-7810
and medical history are
Fax #: 800-884-9931
Request downgrade to
Downgrade/Policy
Will also accept verbal or
new Anthem product after
written request from the
Louisville, KY 40233-7810
policyholder or agent.
Fax #: 317-488-6969
Request an Anthem
Contact Producer
Producer Support (for product
Requested product/deductible
product other than product
transition issues):
must be actively sold; Internal
offered on 1/1/2007 if
Customer Service
process used to track and
benefits are downgraded
complete these changes before member receives new ID cards
Customer Service:
Customer Service numbers
Clients enrolled in current BCBSMO plans:
• For routine billing inquiries or address changes, your clients may call 800-344-8116.
• For questions regarding their notification letter/product transition, your clients may call
• For all other customer services inquiries, your clients may call 800-392-1104.
Client enrolled in new Anthem BCBS plans
• For routine billing inquiries or address changes, your clients may call 866-649-2034.
• For all other customer service inquiries, your clients may call 800-490-6217.
AFFIDAVIT
Member's Name
Area Code) Phone No.
Member's Address:
Spouse's Name and Address:
I hereby certify that as the court-appointed custodian or guardian of the dependent child(ren) listed below, such child(ren) is/are my legal and financial responsibility and will, to the best of my knowledge, reside in my home until age 19 or until the child(ren)'s marriage, whichever comes first. (Dependent children are defined as unmarried children under 19 years of age, including legally adopted or legally placed children, who are dependent upon the subscriber for support and live with the subscriber in a regular parent-child relationship.)
DATE OF BIRTH
Are you legally and financially responsible for the child? YES NO Please advise the date on which you assumed financial responsibility for the child.
Is the child claimed as an eligible dependent on your State or Federal Income Tax Return? YES NO If
Do you live in a regular parent-child relationship with the child? YES NO Please advise the date the Petition for Adoption or Application for Appointment of Guardianship was filed. _ Was custody or guardianship awarded by a court or an authorized governmental agency? YES NO Do you intend to adopt the child? YES NO Has a court already approved the adoption? YES NO Is the child covered by Medicaid? YES NO If yes, give Medicaid Number:
Is the child covered by Medicare? YES NO If yes, give Medicare Number:
Effective dates for Medicare (if applicable): Part A
Are the natural parents of the above listed child(ren) living? YES NO Does either of the child's natural parents live in your household? YES NO Mother's
Father's Current Address:
Does either natural parent have Blue Cross and Blue Shield or Option 2000 coverage YES NO If yes, which parent?
Certificate No.
NOTE: Please submit a copy of the Petition for Adoption or Application for Appointment of Guardianship or
the legal document awarding you custody or guardianship of the listed child(ren). If the child was placed for
adoption, please submit a letter from the attorney handling the adoption, including the name and date of
birth of the child, the name of the adoptive parent(s), and the date the child was placed. Custody or
guardianship awarded other than by a court of law or an authorized governmental agency will not be recognized in
the determination of eligibility for Blue Cross and Blue Shield coverage for the listed dependent child(ren). All
information requested must be furnished before coverage for the listed child(ren) will be considered.
(PLEASE SEE REVERSE SIDE)
I AGREE TO NOTIFY ANTHEM BLUE CROSS AND BLUE SHIELD IMMEDIATELY OF ANY
CHANGES, PRESENTLY UNFORSEEN BY ME, IN THE CHILD(REN)'S LIVING
ARRANGEMENTS WITH ME. I UNDERSTAND THAT AN ELIGIBLE CHILD(REN) WILL BE
REMOVED FROM MY MEMBERSHIP WHEN HE/SHE NO LONGER QUALIFIES AS A
DEPENDENT AS DEFINED IN MY CONTRACT.
Signature of Member
THIS FORM MUST BE NOTARIZED BY A NOTARY PUBLIC
STATE OF
The foregoing document was subscribed and sworn to before me on the
The following is to be completed if the member has coverage through an employer's group plan.
Signature of Authorized Official
Name of Company
In Missouri: Anthem Blue Cross and Blue Shield is the trade name RightCHOICE® Managed Care, Inc. (RIT) , Healthy Alliance® Life Insurance
Company (HALIC) and HMO Missouri, Inc. RIT and certain affiliates admisister administer non-HMO benefits
underwritten by HALIC and HMO benefits underwritten by HMO Missouri, Inc. Life and disability products are underwritten by Anthem Life Insurance
Company (ALIC). RIT and certain afiiliates only provide administrative services for self-funded plans and do not underwrite benefits. Independent
licesnees of the Blue Cross and Blue Shield Association. ®Anthem is a registered trademark. The Blue Cross and Blue Shield names and symbols are
registered marks of the Blue Cross and Blue Shield Association. licensees of the Blue Cross and Blue Shield Association.
Request for Underwriting Opinion
Send to: Underwriting Department
MISSOURI Request
Louisville KY 40233-7810
FAX: 502-889-3515
Complete a separate form for each applicant/dependent
Date: GA/Agent Name: GA/Agent Phone #: _
Send Response to GA/Agent Fax #: _ Client Name: _
Client Id#: _
AGE: _ SEX: _ HEIGHT: WEIGHT: SMOKER (Y/N): _
Blue Access/Choice
MEDICAL HISTORY – PLEASE LIST ALL MEDICAL HISTORY
Details of symptoms,
Treatment, tests performed,
Additional Comments:
THIS UNDERWRITING OPINION IS NOT BINDING IN ANY WAY AND ANY DECISION IS BASED SOLELY ON THE INFORMATION
FURNISHED ON THIS FORM AND IS SUBJECT TO REVIEW IF ADDITIONAL INFORMATION IS PROVIDED.
UNDERWRITER OPINION (BEST CASE OR CONSIDER FOR):
MEDICAL RECORDS ARE NEEDED
In Missouri: Anthem Blue Cross and Blue Shield is the trade name RightCHOICE® Managed Care, Inc. (RIT) , Healthy Alliance® Life Insurance
Company (HALIC) and HMO Missouri, Inc. RIT and certain affiliates admisister administer non-HMO benefits
underwritten by HALIC and HMO benefits underwritten by HMO Missouri, Inc. Life and disability products are underwritten by Anthem Life Insurance
Company (ALIC). RIT and certain afiiliates only provide administrative services for self-funded plans and do not underwrite benefits. Independent
licesnees of the Blue Cross and Blue Shield Association. ®Anthem is a registered trademark. The Blue Cross and Blue Shield names and symbols are
registered marks of the Blue Cross and Blue Shield Association. licensees of the Blue Cross and Blue Shield Association.
Products for Members Over Age65
Medicare Recipients
As a result of the Omnibus Budget Reconciliation Act of 1990 (OBRA-90), Congress
authorized the National Association of Insurance Commissions (NAIC) to develop 10
model Medicare supplement plans to replace the many varied plans on the market.
Since 1992, companies may sell only these identical plans. The plans are identified
with the letters A through J. Every participating company must sell Plan A, and then the
company can choose to sell other standard plans if they wish. Effective January 1,
2006, the Medicare Modernization Act of 2003, Public Law 108-173, provided two
additional voluntary plans, Plans K and L; however, Anthem Blue Cross and Blue Shield
does not currently offer these products.
Plans sold prior to 1992 were not impacted by standardization, and enrolled members
could choose to keep these plans.
Medicare Supplement Plans
Anthem offers Medicare Supplement plans that conform to the NAIC guidelines adopted
by the state of Missouri. To be eligible for Blue Horizons Medicare Supplement plans,
the applicant must live in Missouri in the Anthem Blue Cross and Blue Shield service
area and be enrolled in both Part A and Part B of Medicare.
We offer plans with two types of rates, issue-age rates and community rates. With
issue-age rates, the rate is established based on the person's age at the time he or she
enrolls in the plan. With community rating, the rate is the same for everyone enrolled in
the plan, regardless of age. The rates may change from time to time with both of these
rating methods, based on medical costs and the use of benefits by those enrolled in the
plans. The rates do not change based on the ages of the members.
We offer the following plans:
Issue-Age Plans: Plans A, B, C, D, F, and High-Deductible Plan F (SmartChoice and
SmartChoice Preferred). SmartChoice Preferred is a High-Deductible Plan F with a
copayment on select services. Like other Medicare Supplement plans, SmartChoice
pays the charges that Medicare doesn't pay, including Medicare deductibles and
coinsurance, after the member has met the annual deductible. The annual deductible is
determined by Medicare and subject to change annually.
Community Rated Plans: Plans A, B, C, D, and F.
Dental Plan
Dental Blue Senior Plan: Anthem also offers Dental Blue Senior, a dental plan
covering 100% of eligible expenses for preventive and diagnostic care from network
dentists. In addition, after members pay a $50 annual deductible, Dental Blue pays a set
amount for covered basic and major dental care from network dentists.
Medicare Advantage and Part D Plans
Medicare Advantage Private-Fee-for Service plans – SmartValue Classic and
SmartValue Plus are Medicare Advantage (MA) plans. Medicare Advantage plans
provide specific sets of health benefits offered at a uniform premium and uniform level
of cost-sharing to all Medicare beneficiaries residing in the service area for the MA plan.
MA plan members receive all of their Medicare-covered health care through the MA
plan, usually with more benefits and lower cost-sharing than original Medicare.
SmartValue Classic covers doctors' office visits, inpatient hospital services, emergency
care services, ambulance services, durable medical equipment and diagnostic tests,
including X-rays and laboratory services. SmartValue also covers routine physical
exams, vision services, including eyewear, and hearing services — all of which are not
covered by original Medicare.
SmartValue Plus provides the same benefits as SmartValue Classic, as well as Part D
prescription drug coverage.
Blue MedicareRx (Part D) – Anthem has contracted with the Centers for Medicare and
Medicaid Services (CMS) to offer Medicare Part D Prescription Drug plans to Medicare
beneficiaries. Anthem offers three plans: Blue MedicareRx Value, Plus and Premier.
Refer to the summary of benefits for the features of these plans. The summary of
benefits does not list every limitation or exclusion or the drugs Blue MedicareRx covers.
Limitations and exclusions are included in the Evidence of Coverage, and covered
drugs are listed in the formularies.
Note: Annual certification is required to market and sell the Medicare
Advantage and Blue MedicareRx (Part D) products.
Balanced Budget Act of 1997 (BBA)
Effective July 1, 1998, carriers offering traditional Medicare Supplement Policies must offer
some disenrolled members of a Medicare+Choice (or M+C) or Medicare Select Plans
guaranteed issue policies OR allow the member to enroll in their previous standardized
Medicare Supplement Plan if it is still available from the carrier. The product previously offered
as Medicare+Choice (or M+C) has been replaced with Medicare Advantage.
To qualify for guaranteed issue plans, the insured must meet one of the following qualifying events: 1. First time Medicare Advantage or Medicare Select member that disenrolls within the first 12
months of enrollment. The guarantee issue period begins 60 day before, and ends 63 days after, dis-enrollment.
2. A person involuntarily loses coverage under an employer sponsored health plan. (This
includes retirement from am employer sponsored plan.) The guarantee issue period begins upon receipt of notice and will end 63 days after termination.
3. Medicare Advantage or Medicare Select member moves out of the plan's service
area. (Does not apply to seasonal residents/snowbirds). The guarantee issue period begins upon receipt of notice and will end 63 days after termination.
4. Medicare Advantage Plan is terminated for cause (e.g. insolvency).
Individuals that meet any of these four qualifying events are candidates for
guaranteed issue Medicare Supplement Plans A, B, C or F from any carrier. (The
carrier must only guarantee issue a plan it already sells; for example if it does not
offer Plan C, it does not have to offer it to one of these candidates.) SmartChoice
(high deductible Plan F) and SmartValue (private fee for service) are also available
as options.
Notes:
• The rights of the member must be communicated by the insurer providing prior coverage.
• Application must be received by Anthem within 63 days of disenrollment.
• Proof of disenrollment from the applicant's prior carrier must be submitted.
The following chart indicates qualifying events and which plans are guaranteed issue.
CHART FOLLOWING THE FEDERAL REGULATIONS AND MO REGULATIONS
The product previously offered as Medicare+Choice (or M+C) has been replaced with Medicare
Advantage.
Qualifying Event
Plans Offered As Guaranteed Issue
Any age – enrollment under an employee welfare benefit plan
MO regulations require that all Medicare Supplement
(group health plan) ends, or plan stops providing benefits. Must
products be offered to Medicare recipients. The
be involuntary termination by member. This includes retirement
guarantee issue period will begin upon receipt of
from a group health plan.
notification and will end 63 days after termination.
Any age – enrollment in Medicare Advantage ends because plan
MO regulations require that all Medicare Supplement
ends; entity discontinues plan in service area; individual moves
products be offered to Medicare recipients. The
out of service area; plan misrepresented program to enrollee;
guarantee issue period will begin upon receipt of
"other exceptional conditions" occur.
notification and will end 63 days after termination
Any age – enrollment in Medicare Advantage, cost contract,
MO regulations require that all Medicare Supplement
demo project, prepayment plan, or Medicare Select ends
products be offered to Medicare recipients. The
because plan ends; entity discontinues plan in service area;
guarantee issue period will begin upon receipt of
individual moves out of service area; plan misrepresented
notification and will end 63 days after termination.
program; "other exceptional conditions" occur.
Any age – enrollment in Medicare Supplement ends because
MO regulations require that all Medicare Supplement
carrier becomes insolvent, bankrupt, or otherwise involuntarily
products be offered to Medicare recipients. The
terminates Med Supp. coverage; carrier or agent misrepresented
guarantee issue period will begin upon receipt of
policy provisions; carrier violated material policy provisions.
notification and will end 63 days after.
Any age – person was enrolled in a medicare supplement plan,
The same Medicare supplement plan in which the
then left it to enroll for the 1st time ever in a Medicare Advantage
person was most recently enrolled prior to the Medicare
or other such plan, OR a Medicare Select plan, and within 12
Advantage/Medicare Select dis-enrollment, if that plan is
months the enrollee dis-enrolls.
still available from the carrier they originally had; and if it is not still available, then Plan A, B, C or F from any insurer. The guarantee issue period will begin 60 days before, and end 63 days after, disenrollment.
Age 65 – Person enrolls in a Medicare Advantage plan upon first
ANY Medicare Supplement plan offered by ANY carrier.
becoming eligible for Medicare Part A benefits at age 65; then
The guarantee issue period will begin 60 days before,
disenrolls from the Medicare+Choice plan within 12 months after
and end 63 days after, disenrollment.
the effective date of enrollment.
MEDICARE PART D -- Open to anyone entitled to Medicare Part
There are three plans Anthem offers to Medicare
A or enrolled in Medicare Part B. Medicare beneficiaries who
recipients: Blue MedicareRx Value, Blue MedicareRx
are those individuals that are entitled to Medicare Part A or
Plus and Blue MedicareRx Premier. The annual open
enrolled in Part B. In addition, the individual, must reside in the
enrollment period when anyone may change plans is
service area of the PDP plan offering the Part D product.
11/15 thru 12/31.
Participation is voluntary. Part D members may not have the following drug coverage:
Medicare Supplement with drug coverage (ex. Plan H, I or J, & SmartChoice with Drugs)
Group Subsidy plan
Medicare-approved Drug Discount Plan
Late enrollment penalties apply – 1% of premium per month
Any age- Individuals applying for the same, or lesser, benefit
MO regulations require that all Medicare Supplement
prior to, or 30 days after, the anniversary date with another
products be offered to Medicare recipients.
carrier will be guaranteed issue.
Notes:
♦ The rights of the member must be communicated by the carrier providing prior coverage.
♦ Application must be received by Anthem in accordance with the qualifying event guidelines as outlined above
♦ Anthem Blue Cross and Blue Shield may as for proof of prior carrier information on an anniversary date change.
MISSOURI MEDICARE SUPPLEMENT GUIDE
SITUATION GUIDELINE
Pre-Existing Waiver
Waive Pre-Existing
Effective Dates
First of the month and odd dates only when matching to a client coming from a BCBSMo group
Guaranteed renewal. No open enrollment. Anniversary date is January 1st, regardless of effective
Plan Transfers
Guarantee Issue to any plan offered by Anthem Blue Cross and Blue Shield, regardless of plan enrolled in
with other Blue Plan.
GI/BBA eligible
SmartChoice is our high deductible Plan F. SmartValue is our private fee for service. Both are
available. In some situations, any plan offered by Anthem Blue Cross and Blue Shield may be an option.
Under 65 Disability
All programs are available to under 65 Medicare recipients and will follow the same guidelines as those
offered to 65+ Medicare recipients.
Updated 08/30/06
Guaranteed Acceptance
Acceptance to any Medicare Supplement or Medicare Select plan is guaranteed, if the applicant
applies within their 6-month open window period (the 6-month period following their Medicare
Part B effective date.)
Open Enrollment Period
If applying for a Medicare Supplement or Medicare Select Plan, coverage is guaranteed if the
applicant is at least 65 years old and applying for coverage within six months after enrolling in
Medicare Part B benefits. During this six-month "window," the applicant does not have to
answer medical questions or pass medical underwriting requirements.
To determine if an applicant is within their 6-month window, add 6 months to the effective date
of their Medicare Part B coverage. If the date is in the future and the applicant is at least 65,
he/she is eligible for open enrollment. Example: If applicant's Medicare Part B effective date is
June 1st, add 6 months (June, July, August, September, October, and November) making
his/her 6 month window period end November 30th.
Individuals applying for the same, or lesser, benefit prior to, or 30 days after, the anniversary
date with another carrier will be guaranteed issue.
Disabled Medicare recipients who are turning 65 will be given a new 6-month guarantee issue
window.
If Medicare Advantage coverage is interrupted during the 12-month trail period, the beneficiary
is granted another 12-month trial period, up to a 24-month lifetime limit.
ADDITIONAL INFORMATION REGARDING OPEN ENROLLMENT:
There are no guarantee issue provisions for an individual losing Medicaid benefits.
An individual living out of state who presently has a Medicare Supplement policy with Anthem
Blue Cross and Blue Shield may not make changes other than deleting drug coverage (if
applicable).
Missouri Important Contacts
Agency Services/ Sales Support:
Telephone: 1-888-800-1053, Option 3
Email:
1-888-800-1068 or 314-923-6852
Hours: 8am - 5pm, Monday – Thursday
Faxing Applications and Additional information to Underwriting:
1-800-884-9931
Faxing Underwriting Opinion Form Only:
502-889-3515
Mailing Applications:
PO BOX 37810
Louisville, KY 40233-7180
Customer Service: (Individual only)
1-800-490-6217
Individual Premium Payment Address: (including Med Supp)
Anthem BCBS
PO BOX 790351
St. Louis MO 63179-0351
Individual Billing Maintenance Address: (i.e. for sending cancellations etc)
(including Med Supp)
PO Box 34200
Louisville KY 40233-4200
Anthem Formulary Line: (to hear recent changes to the prescription drugs)
1-(877) 4MULARY/ 877-468-5279
Precision RX: (mail service pharmacy)
1-888-820-0285
Dental:
1-866-589-0582
Supplies:
Select "Order Material Online" from the Individual Producer Site
Refer to your Producer Manual on how to order materials via the Online Order Entry
System.
Source: http://www.gatewayinsurance.net/forms/Anthem%20BCBS%20Missouri/Individual/Underwriting/Anthem%20BCBS%20MO%20Producer%20Manual.pdf
January - March 2010 / # 1 2 hours ago our wandering female harrier from the west In this issue: coast flew straight into the heart of Lesotho! She is now close to a smal stream in a high altitude val ey, about 1 More travels by Lockie . . . . . . Rob Simmons 32 km from the Katse Dam. She has flown a straight line distance of 1173 km from her coastal "home" near
William E. Seidelman MDScience and Inhumanity: The Kaiser-Wilhelm/Max Planck Society First Published in: If Not Now an e-journal Volume 2, Winter 2000 Revised February 18, 2001. One hundred years ago this past December a German scientist by the name of Max Karl Ernst Ludwig Planck gave a lecture in Berlin to the German Physical