Portal.research.lu.se

Acute Confusional State in Elderly Patients with Hip Fracture. Identification of risk
factors and intervention using a prehospital and perioperative management program
Björkman Björkelund, Karin
Published: 01/01/2008
Citation for published version (APA):Björkman Björkelund, K. (2008). Acute Confusional State in Elderly Patients with Hip Fracture. Identification ofrisk factors and intervention using a prehospital and perioperative management program Karin BjörkmanBjörkelund
General rights
Copyright and moral rights for the publications made accessible in the public portal are retained by the authors
and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the
legal requirements associated with these rights.
• Users may download and print one copy of any publication from the public portal for the purpose of privatestudy or research.
• You may not further distribute the material or use it for any profit-making activity or commercial gain • You may freely distribute the URL identifying the publication in the public portal ?
Take down policy
If you believe that this document breaches copyright please contact us providing details, and we will remove
access to the work immediately and investigate your claim.
Download date: 08. Oct. 2016
Department of Anesthesiology and Intensive care, Clinical Sciences, Lund, Faculty
of Medicine, Lund University, Sweden, 2008
ACUTE CONFUSIONAL STATE IN ELDERLY PATIENTS
WITH HIP FRACTURE
Identification of risk factors and intervention using a prehospital
and perioperative management program
Karin Björkman Björkelund
Copyright Karin Björkman Björkelund
ISBN 978-91-85897-99-5
Printed in Sweden by
,Q�/RYLQJ�0HPRU �RI�0 �3DUHQWV�
ABBREVIATIONS . 8
ORIGINAL PAPERS. 9
INTRODUCTION . 10
Acute Confusional State (ACS) . 10
Definition of ACS. 12
Terms and symptom profiles . 12Etiology and underlying mechanisms of ACS. 13Postoperative cognitive dysfunction, POCD . 13Dementia . 14The aging brain . 14Cognition . 14
Elderly patients. 15
Elderly patients' experiences of having ACS. 15
Risk factors for ACS . 15Elderly patients with hip fracture . 16
Swedish National Hip Fracture Register . 17Fall and fracture type . 18ASA risk classification . 19Anesthesia . 20Timing of surgery . 21Pain . 21Hypoxemia. 22Anemia. 22Hypotension . 22Dehydration and malnutrition. 23Drugs. 23
Outcome after hip fracture . 24Intervention studies . 25Documentation . 26Cognitive tests . 26
RATIONALE FOR THE THESIS . 29
Design and study description . 31Study population . 31Data collection. 33
Study I and II . 33Study III. 34Study IV. 34
Assessments in study IV . 36
Intervention in study IV. 37
DATA ANALYSIS. 40
Study I, II and IV. 40Study III. 41
ETHICAL CONSIDERATIONS. 43
Study I, Factors at admission associated to 4-months outcome in elderly patientswith hip fracture . 46Study II, The influence of perioperative care and treatment on 4-months outcome in elderly patients with hip fracture. 46Study III, The Organic Brain Syndrome (OBS) Scale: a systematic review . 54Study IV, Reducing Acute Confusional State in elderly patients with hip fracture: a multi-factorial intervention study. 59
Methodological considerations . 64The findings of the studies . 69
Risk factors for ACS . 69Prevalence of ACS . 70Morbidity and mortality after ACS . 72ACS assessment. 73Reduction of ACS by a multi-factorial intervention program. 73
Clinical implications . 74
FUTURE RESEARCH . 76
POPULÄRVETENSKAPLIG SAMMANFATTNING . 77
ACKNOWLEDGEMENTS. 80
APPENDIX I - III
The overall aim of this thesis was to increase knowledge about underlying causes and perioperative risk factors of Acute Confusional State (ACS) in elderly patients with a hip fracture and to investigate the effect of a multi-factorial intervention program in order to decrease the number of patients who develop ACS. The aim in paper I was to describe elderly patients with a hip fracture on the basis of the American Society of Anesthesiologists' ASA classification system and to identify preoperative risk factors in relation to the postoperativeoutcome measured up to 4-months after surgery. The aim in paper II was to identifyperioperative risk factors in relation to postoperative outcome up to 4-months after surgery. In paper III the aim was to critically examine the Organic Brain Syndrome (OBS) Scale using the criteria and guidelines formulated by the Scientific Advisory Committee of the MedicalOutcomes Trusts (SAC) for the evaluation of assessment instruments; and to investigate its relevance and suitability for use in various clinical settings. In paper IV the aim was to investigate whether an implementation of a multi-factorial intervention program includingprehospital, pre-, intra- and postoperative treatment and care can reduce the incidence of acuteACS among elderly patients with a hip fracture, lucid at admission to hospital.
Design: In paper I and II a descriptive, cohort design was used, using data prospectively registered, and data retrospectively collected from medical records and nursing charts. The design used in study III was a two-stage strategy for identifying and reviewing scientific papers. In study IV a quasi-experimental, nonequivalent comparison group design was used. Results: In paper I risk factors for a poorer 4-month's survival after hip fracture found were ‘ASA-status 3 and 4', ‘more extensive fractures', ‘age 85', ‘male sex', and ‘dependency in living.' Mortality within 4-months was significantly associated with ‘ASA status 3 and 4', ‘age 85 years', ‘male sex', ‘dementia diagnosis', ‘Short Mental Status Questionnaire(SPMSQ) score <8 correct answers', ‘prescribed drugs 4', ‘hemoglobin <100 g/L',‘creatinine >100 micromol/L', ‘dependency in living', ‘unable to walk alone', and ‘fracture other than undisplaced intracapsular'. In paper II significant perioperative risk factors for a poorer recovery and survival after hip fracture were ‘oxygen saturation (SpO2) <90 %',‘fasting time 2 hours', and ‘blood transfusion 1 unit '. ‘SpO2<90 %', and ‘blood transfusion 1' unit were factors significantly associated with postoperative confusion, in-hospital complications and/or death within 4-months after hip fracture. A ‘postoperative hemoglobin <100 g/L' was also significantly associated with postoperative confusion and in-hospital complications. In paper III the result showed that the OBS Scale in many aspects satisfies the requirements formulated by the SAC, but there is a need for additional evaluation, especially with regard to different forms of reliability, and the translation and adaptation to other languages. In paper IV the incidence of ACS was reduced by 64 % in the intervention group (29 of 131) compared to the control group (45 of 132) (p=0.031). Patients developing ACS had significantly higher levels of serious complications and 30-day mortalitycompared to patients without ACS. Conclusion: The majority of elderly patients acutely admitted to hospital due to a fracture ofthe hip suffers from increased morbidity. The incidence of complications is high in thispatient group It is of great importance that patients at risk of developing postoperative complications such as ACS are identified and treated promptly in order to preventdevelopment of complications. Patient's baseline characteristics, such as high age, number of prescribed drugs, or functional status are not possible to have influence on. On the other hand, factors such as oxygen saturation in blood, anemia, fluid balance, pain, or the length of fasting time are possible to affect already at an early stage.
Acute Confusional States, Delirium
Acute and Emergency Unit
American Psychiatric Association
American Society of Anesthesiologists
Confusion Assessment Method
Case report form
Diagnostic and Statistical Manual of Mental Disorders
Functional Residual Capacity
General Anesthesia
Intervention Group
Mini-Mental State Examination
The Organic Brain Syndrome (OBS) Scale
Postoperative Cognitive Dysfunction
Spinal Anesthesia
Scientific Advisory Committee of the Medical Outcomes Trust's
Standardized Audit of Hip Fractures in Europe
Systolic Arterial Pressure
Short Portable Mental Status Questionnaire
Percentage of Oxygen in blood (Oxygen Saturation)
This thesis is based on the following papers referred to in the text by their Roman numerals:
Björkelund KB, Hommel A, Thorngren KG, Lundberg D, Larsson S. Factors at admission associated to 4-months outcome in elderly patients with hipfracture. AANA Journal (accepted).
Björkelund KB, Hommel A, Thorngren KG, Lundberg D, Larsson S. The influence of perioperative care and treatment on 4-months outcome elderly patients with hip fracture (in manuscript).
Björkelund, KB, Larsson S, Gustafson L, Andersson E. The Organic Brain
Syndrome (OBS) Scale: A Systematic Review. International Journal of
Geriatric Psychiatr 2006; 21(3):210-222.
Björkelund KB, Hommel A, Thorngren KG, Gustafson L, Lundberg D, Larsson S. Reducing Acute Confusional State in elderly patients with hip fracture: a multi-factorial intervention study (in manuscript).
The papers have been reprinted with the kind permission of the respective journals.
Old people in need of acute surgery and in connection with sickness are frequent in theanesthesiological setting. The cause for surgery in elderly patients is often preceded by a gradual decline in functional abilities or in medical illness leading to acute impairment or in a fall (1 - 4). Often the time perspective for the preoperative optimization and preparation is short and the patient may arrive at the operating department in a poor condition. The stressful events signified by the illness or trauma, pain, admittance to hospital, long waiting time, surgery and anesthesia, often including respiratory and circulatory loading and poly-pharmacy, may put the elderly patient in an even worse condition postoperatively. The increased strain on an already frail elderly person frequently results in different complications such as Acute ConfusionalState (ACS), leading to a delay in recovery, mobilization and rehabilitation, and alsoimplying a safety risk for the patient (5). Its physical and mental components are recognized as serious, painful and sometimes life-threatening problems. It is reasonable to assume that by implementation of preventive measures against ACSwould not only reduce the incidence of ACS but also the suffering for the individual,the amount of care needed, and the morbidity and mortality.
Acute Confusional State (ACS)
Acute Confusional State (ACS), delirium, in connection with acute illness in elderly patients undergoing orthopedic surgery or cardiac surgery, has been recognized as a serious and common care problem during the last decades. Despite a number of studies have been carried through in order to illuminate and prevent the phenomenon the number of elderly suffering is still high and is expected to increase as the number of elderly is increasing (6). Previous studies have estimated ACS to occur in 14 % to63 % of elderly, hospitalized patients (7 - 12) (Table 1). Variability in incidence could be due to differences in design, the quality of the studies, patient selection, sample size, and different diagnostic criteria (13 - 15). ACS is associated with more intense nursing care (15 - 18) increased rates of postoperative complications, such as pneumonia, urinary tract infection, and pressure ulcer, and longer and more costly hospitalizations (7, 19 - 22). Furthermore, ACS is associated with decreased functionalcapacity (23 - 27) and increased nursing home placements directly or after a few months following the acute care (28 - 32). Finally, ACS is connected with increased hospital mortality (20, 33, 34). Elderly patients with a hip fracture constitute a special group at risk of developing ACS postoperatively where factors as trauma, pain, operation and anesthesia as well as old age, the use of several drugs and infection are of importance (19).
Table 1. Incidence of Acute Confusional State in elderly patients with hip fracture (65 years)
Berggren et al, 1987
Dementia, not fully lucid at admission
Gustafson Y et al., 1988
Magaziner et al., 1990
Gustafson Y et al., 1991
Lundström et al., 1999
Strömberg et al., 1999
Pathological HF, communication
difficulties, history of mental detoriation
Brauer et al., 2000
Patients fractured in hospital/ previouslyfractured, bilateral HF, pathological HF
Dolan et al., 2000
Dementia, institutional living
Duppils et al., 2000
ACS at admission, aphasia
Marcantonio et al., 2000
Life expectancy <6 months, informedconsent not obtained within 24 h of surgery or 48 h of admission
Andersson et al., 2001
Mental disease, ACS at admission,communication difficulties
Edlund et al., 2001
Marcantonio et al., 2001
Metastatic cancer or life expectancy<6 months
Milisen et al., 2001
MT, brain concussion, pathological HF,
surgery <72 h after admission, aphasia, blindness, deafness,<9 years of education
Zakriya et al., 2002
Dementia or ACS on admission
Gruber-Baldini et al., 2003
Dementia, institutional living
Schuurmans et al., 2003
Edelstein et al., 2004
Patients with dementia unable to answer a simple questionnaire
Kagansky et al., 2003
Dementia, hearing loss, severe visual impairment, patients with postoperative ‘interval' ACS§)
Olofsson et al., 2005
RA, severe osteoarthritis of the hip, severe renal failure, pathological HF, bedridden patients
Lundström et al., 2007
RA, severe osteoarthritis of the hip,
severe renal failure, pathological HF, bedridden patients
Vidán et al., 2005
Inability to walk, ADL = 0, pathological
HF, life expectancy <12 months
*) Intervention sample
†) Usual care group
‡) Postoperative assessment only§) ‘Interval' ACS= ACS occurring between the second and the seventh postoperative days (Becker et al., 2003)HF = hip fracture, ACS = Acute Confusional state, ADL = Activity of Daily Living, MT = Multiple trauma, RA = Reumathoid arthritis
Definition of ACS
The definition of ACS according to the American Psychiatric Association (APA), Diagnostic and Statistical Manual of Mental Disorders, DSM-III, definition of Delirium goes back to the nineteenth century when Greiner (1817) introduced the term ‘clouding of consciousness'(49, 50). This term was dropped in the revised version ofDSM-III (DSM-III-R, 1987) on the grounds that it was difficult to make operational (51). The term ‘clouding of consciousness' has been replaced by ‘disturbance of consciousness' (reduced clarity of awareness of the environment) in the later revision, i.e. the DSM-IV definition of Delirium (52, 53). According to this definition ACS is an acute, transient, neuropsychiatric syndrome, with organic causality, characterized by disturbed attention and cognition which develops over a period of hours, or days, and fluctuates over the course of the day. Often there is also a disturbed sleep-wake cycle(49, 54, 55). As criteria for ACS, Delirium, at least four clinically important features are required (56) (Table 2).
Table 2. Diagnostic criteria for Acute Confusional State, ACS, according to the DSM-IV definition of
Delirium
Disturbance of consciousness with a reduced ability to focus, sustain, or shift attention
A change in cognition (such as memory deficit, disorientation, language disturbance) or the development of a perceptual disturbance
The disturbance develops over a short period of time (hours or days) often showing a fluctuating course
There is evidence from the history, physical examination or laboratory findings that the disturbance is caused by the direct physiological consequences of the general medicalcondition (substance intoxication or withdrawal, or not otherwise specified).
(Adapted from the American Psychiatric Association, APA, 1994)
Terms and symptom profiles
According to Lipowski (1992) the term Acute Confusional States, ACS, is the only synonym for delirium that can be accepted (19, 55, 57), although several terms exists in the literature for the same phenomenon, such as ‘Cognitive impairment' (58), ‘Acute confusion' (59), ‘Postoperative delirium' (60), or ‘Postoperative confusion' (7).
‘ICU psychosis' or the ‘ICU syndrome' are other labels for the same phenomenon (61).
There are different symptom profiles of ACS in different patients, the easiest to recognize is the hyperactive when the patient has both a psychological and motoricaldisturbance often showing hallucinations, and the hypoactive when the patient is silent and calm (62). This situation is often mistaken in the incorrect belief that the patient is suffering from dementia and instead suffers from a cognitive disturbance, even if ACS is often found in patients suffering from dementia (62, 64). ACS usually develops over
a short period of time and often occurs during the first postoperative days. After thefifth postoperative day the incidence of ACS has been estimated as low (64). In the majority of cases ACS has resolved before discharge from hospital without any focused intervention (65).
Etiology and underlying mechanisms of ACS
ACS is believed to be a multi-factorial disorder including aging, impairment of cerebral metabolism, polypharmacia as well as drug interaction, and surgical stress. Different patophysiological changes as hypoglycemia, hypotension, hypoxemia, andfactors related to intraoperative events such as greater blood loss, several postoperativeblood transfusions, and postoperative hematocrit below 30 % have been shown to be associated with an increased risk of postoperative ACS (6, 64 - 69).
Hypotheses of the mechanism behind the ACS
The mechanism behind ACS is based on two hypotheses (70). The first hypothesis is about hypoxemia in the brain leading to a disturbed oxidative metabolism and a disturbed synthesis of acetylcholine (71). The other hypothesis proposes that ACS ismediated by stress-hypercortisolism leading to a disturbed glucose metabolism and neural damage especially in the cholinergic neurons (70). Several studies indicate that disturbances in the cholinergic metabolism are of significance for the development of ACS. Both hypotheses are probably of importance in most cases of ACS developing inelderly persons (72).
Postoperative cognitive dysfunction, POCD
ACS seems to have the same etiological mechanisms as the milder condition, postoperative cognitive dysfunction (POCD). The term POCD was first presented during the late 1990-ies (73). The syndrome group Postoperative Cognitive Impairment /Disorders range from mild postoperative cognitive dysfunction to the more serious form ACS. Although ACS and POCD probably have similarpredisposing factors, POCD and ACS differ in several ways. POCD is defined as "a deterioration of intellectual function that presents as impaired memory or concentration" (74). It is looked upon as a mild neurocognitive disorder when thepatient generally/usually is fully alert and oriented with mild forgetfulness or concentration to affecting the full-range of cognitive functions resulting in loss of independence (73, 75). POCD has, at the time of discharge from hospital, been shownto appear in all ages (18 years) after major non-cardiac surgery but with increasing incidence in relation to age (76). At three months after surgery the incidence of POCDin patients 60 years and older were more than the double compared to younger age groups. Patients who suffered from POCD at both hospital discharge and at three months after surgery were more likely to die during the first year after surgery (a.a.).
The concept dementia comprises multiple cognitive deficits together with impairment in functional and social function. Dementia, in contrast to ACS, is a progressive and chronic brain disorder, which has a slow onset. Dementia as defined according to theDSM-IV criteria is a deterioration of the memory, impairment in long or short-term memory, followed by at least one (or more) cognitive disturbances such as aphasia, apraxia, agnosia, and detoriation in executive functioning as planning and organizing(52). Different subtypes of dementia are defined specifically in the DSM-IV. The prevalence of dementia is estimated to be about 5 % in persons over 65 years (77). The annual incidence rate for dementia in individuals of 75 and older, presented by theLeipzig Longitudinal Study in Aged (2001), is 47.4 (CI=36.1 - 61.2) per 1000 person-years (78).
The aged-associated structural and functional changes of the central nervous system (CNS) as a 15 percent decline in brain volume, attrition of neurons and decline in neural numbers of about 15 %, a decrease in neural size, and changes in dendrites treewith a reduction in the number of synapses. Moreover, the alteration or reduction innumerous neurotransmitter systems for example dopamine, serotonin, gamma-aminobutyric acid (GABA), and central cholinergic activity leads to a slowing in reaction time and cognitive processing (79, 80). Failure of cholinergic neurotransmission is a central feature of Alzheimer's disease. All the changes in the aged brain imply that the CNS has a reduced functional reserve and the assumption among researchers is that this reduction makes the elderly more vulnerable to thedevelopment of ACS or POCD (79).
Cognition refers to "the use and handling of knowledge" and "the overall functioning of mental abilities" (81). Cognition can be defined as the mental process of perception,memory, and information processing, by which the individual acquires knowledge, solves problems, and plans for the future (82). Cognition implies intellectual processes in the brain comprising activities of daily functioning: the mental process of perception as to focus, maintain and divide attention (concentration) to learn and remember new things, to think, reason and solve problems, to plan, carry out and monitor own activities, to understand and use language, to recognize objects and assemble thingstogether, and to judge distances (spatial skills). Cognition problems in elderly persons are about changes and manifestations of decline such as in recall of memory, in concentration, or reasoning, or in finding the right word (81).
The concept "elderly" is frequently used in the literature as referring to persons 65 years of age and older; however, it is many times not defined. Elderly patients in thisthesis refer to the definition of "old" based on chronological age as a person of the age of 65 and older (83). However, this definition does not take the biological,physiological and psychological ageing fully into consideration, as these aspects show a more gradual decline with age rather than that of a clear point (84). The age of80 - 85 years (the very elderly) could be considered as a risk of frailty as this age often is characterized by hearing and vision problems, causing functional dependency in the majority of people beyond this age (85). The very elderly persons often suffer from coexisting debilitating diseases, and are thus more vulnerable to surgery and anesthesia. Hence, in this thesis the concept "frail elderly patients" should beinterpreted as persons of about the age of 80, rather than that of 65 years.
Elderly patients' experiences of having ACS
Elderly patients´ memories and stories of their experiences of having ACS have been compared to being in a borderland between reality and imagination, past and present, and between being conscious and unconscious of external events (86, 87). Documentation from elderly's stories describe memories of knowing their experiences were unreal but they appeared real when they occurred (88), and how the environmentchanged into something else and the staff became total strangers (89). The experiences of strong emotional feelings of threat, insecurity, and anger were described but also of suspiciousness, hallucinations, and illusions (89, 90). Descriptions of being humiliated by the staff were expressed (90) and feelings of shame and guilt of having behavedbadly during the ACS (89, 90).
Risk factors for ACS
An overview of risk factors for ACS identified in 14 studies published between 1980 and 1995 provided independent risk factors for ACS among older patients identifiedthrough predictive models or stratification methods (6). The most common risk factor identified across studies was cognitive impairment. Other risk factors appearing were high age, psychoactive drug use, severe illness/comorbidity, azotemia/dehydration, male gender, alcohol abuse, infection/fever and metabolic abnormality. Among ‘Other' were found fracture on admission, hypotension, hypoxia, type of surgery (aortic aneurysm, thoracic), depression, low social interaction and low activity level (6). In two prospective studies precipitating and predisposing factors respectively forACS were identified (67, 68). A multifactorial model for ACS was proposed involving a complex interrelationship between baseline patient vulnerability and precipitatingfactors or noxious insults occurring during hospitalization (6) (Figure 1).
High vulnerability
Several psychoactive
Sleep deprivation
sleeping medication
Low vulnerability
Not noxious insult
Figure 1. Multifactorial model of Acute Confusional State.
(Modified after: Inouye & Charpentier, 1996 and Rolfson, 2002)
As an example of the interrelationship in this model a patient with a high vulnerability (as severe dementia, vision or hearing impairment) may develop ACS with a relativelybenign insult as one dose of sleeping medication. Conversely, a patient with low vulnerability would be relatively resistant and require multiple noxious insults as general anesthesia, major surgery or sleep deprivation of developing ACS. Olderpatients are generally more vulnerable than younger, depending on a number of predisposing factors as cognitive impairment, comorbidity and others (6).
Elderly patients with hip fracture
Hip fracture is a common cause of acute hospitalization in older people. Patients with hip fracture are one of the most resource consuming patient groups (91). In Sweden,with a population of nearly 9 million, approximately 18.000 persons yearly are treated due to a hip fracture, occupying around 25 percent of all bed days in orthopedicdepartments (91). By using Swedish data based on predicted mortality the lifetime risks of hip fracture at the age of 65 years are estimated to 30% in women and 13 % in men (92). During the last twenty years the incidence of hip fracture has doubled in persons above 80 years of age, and is the most frequent fracture for persons over this age (93). This increase in the risk of hip fractures is expected to continue due to an increasing number of elderly persons in the population and an increase, particularly in the oldest persons, those above 80 years (91, 94). Using Sweden as a reference country the expected number of patients with hip fractures has been estimated to increase by 28 % between 1990 and 2025 (92), although several recent reports suggest a decline in
the incidence of hip fractures (95, 96). The number of hip fracture occurring each year in the world has been estimated to increase from about 1.7 million in 1990 to 6.3 million by the year 2050 (97).
Three out of four of the patients with a fracture of the hip in Sweden are women butthe number of men is increasing, today reaching 30 % (98). The mean age of the patients at fracture is 82 years. Men tend to be younger (mean age 80 years) thanwomen (mean age 83 years), to have more comorbidities and a higher mortality 1-year post fracture. About 65 % of the patients lived in their own home before the fracture, while 29 % were dependent in living i.e. they lived in institutional care such as old peoples´ home or nursing home. The remaining patients were admitted from other living conditions such as rehabilitation unit (2 %), acute hospital (3 %) or other type of care (1 %) (98). Forty-eight percent of the patients lived by themselves before the fracture (a.a.).
Swedish National Hip Fracture Register
To characterize and organize the treatment outcome of hip fractures in the elderly inSweden the national register RIKSHÖFT was started in 1988 (91). Annual reports including analysed and synthesized medical, functional and patient perceived outcomedata are presented. RIKSHÖFT has been validated several times (98). Data registered in the RIKSHÖFT Primary registration form is filled in prospectively during thehospital stay and includes demographic data, data concerning the patient's background as place of residence, walking ability, and the use of walking aids. Furthermore, data on fracture, admission at hospital, date and time of surgery, type of surgery, ASA-grade (American Society of Anesthesiologists relative risk classification system (99),and date of discharge and where to, such as home, nursing home or other are included.
The patient is followed-up by the orthopedic department via the 4-months registration form with regard to pain, residence, walking ability and walking aids, and care continuum with various types of accommodations (98).
A project for quality improvements of care called Q-reg 99, initiated by The National Board of Health and Welfare and The Swedish Association of County Councils was started 1998 and included in the RIKSHÖFT the following year (100). The project was later implemented in the RIKSHÖFT. The Q-reg 99 includes details of the patient's mental status (The Short Portable Mental Status Questionnaire (SPMSQ)) (101),location of fall, cause of delay for surgery, registration of time of arrival to hospital, first analgesic medication given, X-ray, and time for start of operation. Moreover, any complication appearing during hospital stay and after discharge up to four months after surgery is registered (100). Complications as pressure ulcer, pneumonia, heart failure, deep vein thrombosis, superficial and deep wound infection, wound hematoma, urine tract infection, acute renal failure, gastrointestinal haemorrhage, myocardial infarction,and cerebrovascular lesion had each one a separate heading in the registration form.
Under the heading of ‘Other', complications as ACS, anemia or constipation were registered without any further specification (102).
International interest in the national audit resulted in the start of the project Standardized Audit of Hip Fractures in Europe (SAHFE) in 1996 in order to achieve comparative international audits (91, 103). Today several countries in Europe use theregister as well as countries outside Europe, as Japan, Australia and USA.
Fall and fracture type
Most hip fractures are a result of a fall or a stumble, only in about 2-5 % of the cases there are no history of an injury (2, 104, 105). There is often a multifactorial origin behind the fracture related to an increased tendency to fall, loss of protective reflexes,and reduced bone strength due to osteoporosis or osteopenia (105). Most accidents take place indoors (68 %) in familiar environments (2). The majority of hip fractures are diagnosed by a history of fall leading to a shortened and externally rotated leg, pain in the hip, inability to walk, and plain radiographs of the hip that confirms the diagnosis (105, 106).
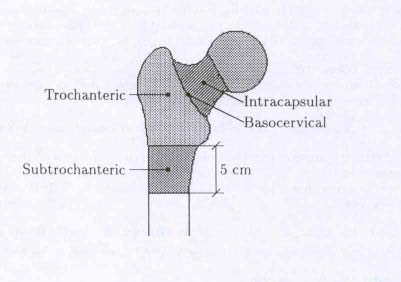
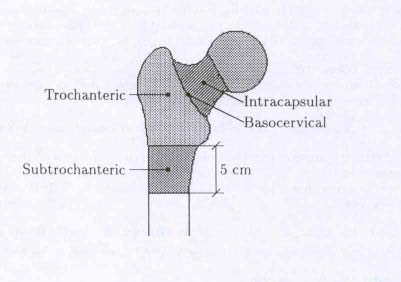
Figure 2 Types of hip fractures
(Source: RIKSHÖFT, form 1)
Hip fracture is the common name for two types of fractures of the proximal femur; the cervical and the trochanteric (91) (Figure 2). The fracture is cervical if it is located in the femoral neck. The cervical fracture can be undisplaced (about 33 % of the cases) or displaced (67 %). A trochanteric fracture is located through the muscle insertions distal to the femoral neck (38 % of the cases). If the fracture extends distally within 5 cm below the lesser trochanter it is called subtrochanteric. Basocervical fracture is an intermediate type of hip fracture. The incidence of cervical vs. trochanteric fractures is about the same, with a slight predominance of cervical fractures (91, 98).
Frail elderly patients often sustain more extensive fractures as the trochanteric (98),although most fractures of the hip in the elderly are the result of a low-energy fall (104). Extensive fractures, especially the unstable intertrochanteric ones often lead to an increased blood loss and more postoperative complications compared to lessextensive fractures, as the undisplaced intracapsular (107). As the aim is to rehabilitate the patient to the same functional level as before the fracture, the treatment of a hip fracture is therefore in most cases surgical, either as ostheosynthesis with hook pins (inabout 23 % of the cases, or screw and plate fixation (36 %), or as arthroplasty (hemi-arthroplasty (25 %) or total arthroplasty (5 %). The mean time spent in hospital in Sweden today is 11 days (98), which might seem rather long in relation to that many patients are mobilized already on the first postoperative day. On the other hand, thetime spent in the acute hospital many times depends on other causes such as clinical routines, access to rehabilitation units, or that the patients suffer from other medical problems.
ASA risk classification
According to general routines all patients undergoing surgery are preoperativelyexamined by an anesthesiologist. The patient's physical status should be assessed according to the American Society of Anesthesiologists classification of physical status (ASA) (99) (Table 3).
Table 3. ASA physical status classification
A normal healthy patient
A patient with mild systemic disease
A patient with severe systemic disease that limits activity, but is not incapacitating
A patient with an incapacitating systemic disease that is a constant threat to life
A moribund patient not expected to survive 24 hours with or without operation
(Adapted from the American Society of Anesthesiologists (ASA, 1963)
The ASA scoring system has been found to be a significant predictor of post-surgerysurvival in patients (age 65+) with hip fracture (n=114, age mean (SD) 82.4 (7.9) years). One year mortality rate has been shown to be almost nine times higher in ASA class 3 - 4 patients compared to ASA 1 - 2 patients (108). ASA physical statusclassification is a predictor of postoperative outcome and the risk of complication is influenced mainly by ASA class 3 and 4 (109). Patients in ASA class 3 - 4 more frequently sufferer from cardiovascular disorders, are more often disoriented, and already have some pre-fracture difficulty with ambulation compared to ASA 1 - 2patients (108). The ASA rating of operative risk counts on the severity of any systemic
diseases that may affect survival, whereas the number of medical comorbidities only is a reflection of the patient's general health status (110). On the other hand, the ASAphysical status classification suffers from lack of precision (111), and may be too insensitive and subjected to local variations (112, 113).
The choice of anesthetic technique in hip fracture surgery patients eventually dependson different factors as patient's desires, co-existing medical conditions, and risk ofanesthetic techniques (114). The two main anesthetic types used in hip fracture surgery are general anesthesia and spinal anesthesia. General anesthesia involves loss of consciousness, including intravenous and/or inhalation drugs. Spinal anesthesia refers to a neuraxial anesthesia, when local anesthetics are injected into the subaracnoidalspace and the lower part of the body is anesthetized (a.a.).
Previous randomized and quasi-randomized trials from 1978 to 2003 (n=22), reviewed by Parker et al, (115) have failed to establish a benefit of one form of anesthetic over another. Methodological flaws occurred in all trials, and many trials didn't reflect anesthetic practice of today. Author's conclusions were that regional anesthesia compared to general anesthesia may reduce acute postoperative confusion. There were also trends in a reduction of myocardial infarction and fatal pulmonary embolism, but an increase in the number of non-fatal pulmonary embolism and cerebrovascularaccidents. No conclusions, however, could be drawn with regard to mortality or other outcomes (115). No statistically significant differences in the incidence of confusionbetween two anesthetic groups (halothane and epidural) was found in a study by Berggren et al. (1987), even after correction for the use of anticholinergic drugs whichwas overrepresented in the epidural group. The most important predictor for postoperative mental confusion was a regular use of drugs with anticholinergic effects (p<0.005) (7).
One prospective study, in which the anesthetic method was decided by theanesthesiologist, no differences in short and long-term outcomes (ambulatory status at hospital discharge, recovery of ambulatory status, and functional ability at 3, 6 or 12 months) were found when evaluating general versus spinal anesthesia in patients undergoing hip fracture surgery (116). One of the studies in favor of regionalanesthesia was a prospective 2-year longitudinal observational study, part of theBaltimore Hip Studies during 1990-91. In this study the choice of anesthesia, general anesthesia or spinal anesthesia, was decided by the attending anesthesiologist (117). Cognitive functioning was assessed with the Mini-Mental State Examination (MMSE) (118). A small difference near to statistical significance was seen favoring spinal anesthesia for cognitive functioning through 2 years of postprocedure follow-up tests (5, 12 and 24 months) (117). There was no information presented about any form of medications for sedation administered to patients assigned to spinal anesthesia (a. a.). In later studies, as in one study using a randomized design, showed that the onlyimportant factor statistically significant for development of ACS, using the MMSE,
was preexisting cardiovascular disease irrespectively of anesthesia type which in this case was general or spinal anesthesia (p<0.025) (119).
Timing of surgery
Early surgery i.e. within 24 hours has been recommended to increase the chances of a favorable outcome after hip fracture (120), as it enables early mobilization the day after surgery (91). However, evidence supporting this approach is lacking and previous studies have reported contradictory and inconclusive data as to whether early surgery is beneficial or not (102, 121). A surgical delay of 24 hours or more have been reported to constitute a significant risk factor for the development of complicationssuch as ACS (39, 122), pneumonia including hypoxia (123), deep vein thrombosis,urine tract infection (124), an increased postoperative hospital stay (126), and increased mortality rates (125, 127, 128). However, several studies did not find early surgery associated with decreased mortality rates (129, 130; 131, 132), or with improved postoperative function (locomotion), but with fewer days of severe pain (130), and a reduction in pressure ulcers (100, 129). Early surgery is associated with fewer major complications if patients who are medically stable at admission are included in the study and therefore eligible for early surgery (130). Primary reasons fordelaying surgery more than 24 hours after arrival to hospital are factors as waiting for completion of medical evaluation, unavailability of the operating room or surgeon, waiting for laboratory results and waiting for medical stabilization (123). Living alone and being older may imply that hospital arrival could be delayed hours or even days,and by which time the patient can be both dehydrated and have developed ACS (104). The prevailing recommendation is therefore that the majority of patients should beoperated without delay before surgery, provided that any concomitant medicalconditions are not amenable to specific treatment (120). The mean waiting time from hospital admission to operation in Sweden today is 1.2 days (98).
A patient with a hip fracture is generally subjected to acute severe pain, especiallypatients who suffer from more extensive fractures. Acute pain involves an activation of the autonomic nervous system and an endocrine metabolic response, which couldlead to a greater strain in an already frail elderly person. Pain provokes a sympatheticreaction with tachycardia and increased myocardial oxygen demand, leading to cardiac ischemia (133). This sympathetic reaction is especially harmful in elderly persons as it may lead to cardiovascular instability (134). A reduced functional residual capacity (FRC), resulting in atelectases, is related to pain and a reflex-mediated reduction of the diaphragm (135, 136). Several studies have demonstrated that preoperative pain is an important predictor of the incidence and intensity of postoperative pain (137).
Postoperative pain in elderly is associated with increased hospital stay, delayed locomotion, and long-term functional impairment (138). Severe pain, untreated pain orinadequate analgesia significantly increases the risk of ACS in cognitively intact,
elderly patients following hip fracture (138, 139). Hence, management of acute pain is obviously a central issue in elderly patients with hip fracture; however, pain is often underassessed by the staff (140, 141).
Traumatized elderly run a high risk of developing clinically significant hypoxemia due to an increased mismatching of ventilation to perfusion in the lungs soon after being bedridden (142, 143). Arterial hypoxemia has been reported as frequent in elderly bedridden patients after hip fracture (7, 144 - 146). The supine positioning, surgery,and anesthesia, and immobilization, sometimes for several days, contribute to a reduction in FRC with hypoxemia, hypoventilation, and the development of atelectasis and pneumonia as a consequence (136, 147). Although hypoxemia was frequently seen in elderly patients in an international multicentre study of POCD (the ISPOCD1study), it was not found to be a significant risk factor of POCD (148). Hypoxemia inelderly, however, has been supposed by other researchers to contribute to thedevelopment of ACS (7, 64, 144, 145, 149, 150).
Anemia, defined by the World Health Organization (WHO) as a hemoglobin in bloodless than 120 g/L (women) and 130 g/L (men), respectively, is frequent in olderpersons and is associated with increased mortality risk, especially in patients 85 years and older (151 - 153). A hemoglobin level <100 g/L in blood (corresponding to a hematocrit of <30 %) indicating severe anemia (142, 151, 154) has been accepted in patients with hip fracture (155). Evidently, many elderly patients are often dehydrated with falsely high hemoglobin levels at admission that decrease clearly after the initial fluid hydration (153, 156, 157). This condition may further increase a decline in tissue oxygen and an inadequate oxygen delivery to the brain and consequently contribute to the development of ACS (64). Patients (65+ years) who are anemic at admission aremore prone to have an ASA rating of III or IV, have sustained an intertrochanteric fracture, and tend to have a longer length of hospital stay (LOS) (152). Even mild degrees of preoperative anemia have been found to increase the adjusted risk of 30-day postoperative mortality in elderly patients undergoing noncardiac surgery (158).
Higher average postoperative hemoglobin level in patients aged 60+ is independentlyassociated with better early functional recovery (159).
Age-related changes in autonomic reflex responses (baroreceptor response, vasoconstrictor response to cold stress, and beat-to-beat heart rate response after postural change) that maintain cardiovascular homeostasis progressively decrease in elderly persons (160). The changes in response presents as being less rapid in onset,
smaller in magnitude, and less effective in stabilizing blood pressure (a. a.). Age-related changes in the cerebral autoregulation implies that even minor fall in systolic blood pressure may precipitate a decrease in cerebral blood flow (161). Intraoperativehypotension have been thought to contribute to postoperative complications in elderly patients, however, reported data from previous studies give contradictory answers. In two studies hypotension, defined as a more than 30 % below preanesthetic noninvasivesystolic control levels and a systolic arterial pressure decline to <0.66 of preoperativebaseline or <90 mmHg, requiring vasopressors or fluid resuscitation, respectively, didnot show to contribute to the development of ACS (7, 64). In a later study perioperative blood pressure falls (mean (SD) 31.4 (± 16.5)) were revealed as an independent predictor for postoperative ACS together with male gender (21). In this study hypotension and male gender could correctly predict 82 % of the elderly patientswho developed postoperative ACS.
Dehydration and malnutrition
In older persons with increasing disability, dehydration is among the most common reasons for hospitalizations and an important cause of increased hospital-associatedmortality (156). Mortality was significantly increased in patients (mean age 80 years(range 17 - 101) with hip fracture admitted to hospital with a raised or low serumsodium, raised serum potassium and raised serum urea (162). Dehydration has beenidentified as both a predisposing and a precipitating factor for ACS (67, 68).
Furthermore, an inadequate fluid intake with dehydration and/or serum electrolyte imbalance has been shown to be a significant predictor for ACS (11, 163). Malnutrition was seen in one third of comparatively healthy patients (mean age 84 years) with hip fracture (164). Malnourished patients are less likely to recover their pre-fracture level and are more likely to die within 1-year post surgery (165). Aprolonged preoperative fasting time, frequently occurring in elderly patients with hipfracture may further deteriorate an already exhausted state (156, 165). On the otherhand, improvements in preoperative hydration and nutritional status in elderly has thepotential of improving outcome (164, 166).
Polypharmacia and a large number of medications in combination with frailty can cause ACS in elderly patients (90, 167). The use of four or more prescribed drugs haveshown to be a risk factor for falling in elderly persons (168), and independentlyassociated with ACS within 24 - 48 hours to its onset (68). Medications withanticholinergic effects or drugs that reduce brain cholinergic activity are known to increase the risk of ACS in elderly people (7, 60, 167, 169) (Table 4).
Table 4. Medication that may cause ACS
Drugs that reduce brain cholinergic activity
Other drugs associated with ACS
H2 antagonists (eg. Cimetidine, Ranitidine)
Steroids (eg. Prednisolone)
Neuroleptics (eg. Haloperidol)
Tricyclic antidepressants (eg. Amitryptyline) ,
Antiparkinsonian agents (eg. L-dopa)
Antipsychotics (Neuroleptics eg. Chlorpromazine)
NSAID (eg. Celecoxib, Ibuprofen)
ACS-inhibitors (eg. Captopril
Calcium-channel blockers (eg. Nifedipine)
Diuretics (eg. Furosemide, Triamterene with thiazide)
Beta blockers (eg. Isosorbide dinitrate)
Antiarrythmics (eg. Disopyramide)
Anticoagulant (eg. Warfarin, Dipyridamole)
Methylmorphine (eg. Codeine)
Anticholinergics (Oxybutynin, Tolterodine)
Antihistamines (Diphenhydramine, Promethazine)
Anti-diarrhoeal agents (containing belladonna)
Gastro-intestinal antispamodics (Hyoscyamine)
NSAID = Non-steriodal anti-inflammatory drugs
(Modified after Tune et al., 1994, Mintzer and Burns, 2000, and Rolfson, 2002)
Outcome after hip fracture
Outcomes after hip fracture surgery are associated with complications in up to one third of the patients (104). Postoperative complications were found to be more frequent in patients with unstable intertrochanteric fractures (38 %) than in patientswith nondisplaced (17 %) or displaced fractures (25 %) of the hip. There were no differences, however, among the fracture groups in the incidence of majorcomplications (107).
Six months after hospital stay only about 60 % of hip fracture patients (age > 50) haverecovered their pre-fracture walking ability (170), and less than 50 % of the patientsreturn to their pre-fracture level of functioning (171). Increased age, living in an institution at time of injury, and poor functional status at discharge have been found to be the most significant predictors of poor functional status 1 year after the hip fracture (172).
A hip fracture is associated with significant perioperative mortality and morbidity (173 - 175) and the highest risk of mortality occurs within the first 2 - 6 months after fracture (120). It is the very elderly patients, 80 years and over, who have the highest
1-year mortality (176). In-hospital mortality rates show that mortality is much higher in patients after hip fracture than in the general population of comparable age, and itremains raised for several months after the fracture (174). Death during primary hospitalization in elderly patients (age 50+) with hip fracture varies from 1.6 % to 4 % (110-171). Four-months and 1-year mortality varies from 15 % to 17 %, and 13 % to 26 %, respectively (110, 173, 177). One year mortality was shown to be twice as high for men (21 %) as it was for women (11 %), while the mortality rate of patients whowere 85 years and older (21 %) was more than twice that of the younger age group (9 %) (110). Cognitive dysfunction and reduced pre-fracture mobility have shown to be reliable prognostic indicators of increased mortality within the first postoperative year (age, range 53 - 100 years) (131). Three-year follow-up survival in elderly hospitalized patients (age 65+) was 75 % for patients with ACS and 51 % for non-ACS patients (34). Recent results suggest, presenting mortality analysis in a group ofunselected hip fracture patients, that about half of the total mortality would be possible to avoid (175). Therefore it would be reasonable to assume that by implementingdifferent preventive measures against ACS this may not only reduce the incidence ofACS, but also the morbidity and mortality.
Intervention studies
A number of intervention studies have been carried through with the aim to reduce the development of ACS in elderly patients connected with acute illness (Figure 3). The interventions have been focused on four types of intervention: general geriatric approaches, nursing care, family interventions, and anesthesia (178). Despite methodological limitations in some of these studies, such as small samples, use of non-targeted interventions or relatively insensitive outcome measures, all of them have shown positive effects (13, 27, 41, 179 - 181).
Interventions have involved actions to make the surroundings as familiar as possible, strategies to avoid changes (182), environmental changes for noise reduction, orientating objects, sensory support through improving the patients possibility to see and hear, and psychological support as cognitively stimulating activities (178) as well as early mobilization and increased physical activity (18, 178). Consultation by a geriatric internist or psychiatrist and/or with daily follow-up by a liaison nurse who assessed the patient's condition, treatment and contacts has been performed (13, 183). A multi-disciplinary geriatric intervention program to identify and quantify medical and psychosocial problems and functional capability was introduced by Vidan andcolleagues (48). A joint geriatric-anesthetic approach was carried out by Gustafson, Y. et al. (1991) (35). The intervention included a preoperative and postoperative geriatric assessment, oxygen therapy (1 litre/min) administered at admission, during surgeryand for the first postoperative day, early surgery, prevention and treatment of perioperative hypotension, and early detection and treatment of postoperative complications (35). Other forms of interventions have included stabilizing physiological functions as early recognition of dehydration, encouragement of oral intake of fluids, and pharmacological intervention through strategies for pain relief
(178, 184). Interventions by nurses alone have been as effective as interventions by physicians (13). Many studies, however, have focused on the treatment of ACS rather than early prevention (178). The programs have also been heavy and difficult to carry through in the clinical settings including regiments designed to manage pre-existingcognitive impairment, sleep deprivation and sleep-apnea syndrom, patient-focusing environment, immobility, visual and hearing impairment, low saturation, and dehydration (181, 185). Despite methodological limitations in some of these studies, all of them have shown positive effects (186). Only two multi-factorial interventions for preventing ACS have been carried through using a randomized design (40, 47,187), which points at some difficulties in applying the randomized design into clinical settings and practice. However, the results of earlier interventions made indicate that a multi-factorial program, adapted to the prehospital and the perioperative clinical practice, would be possible to implement in order to reduce the incidence of ACS.
In the literature the importance of assessing cognitive status is frequently discussed, however, the knowledge among nurses regarding cognitive impairment is often insufficient (57, 188, 189). Although nurses' clinical notes contain information aboutthe patient's cognitive status, the documentation of mental status in the nursing records is seldom accurate and ACS is often under-diagnosed (190). In the study of Souder &O'Sullivan (2000) no documentation in the nursing chart of impaired cognitive status was revealed, although impaired performance was identified in 24 % to 67 % of thecognitive measures in this population. The authors came to the conclusion that nurses often limit their assessments to the patients' capability to orientate themselves (time and place) and don't identify cases where a cognitive problem exists (188).
Many times nurses and physicians don't recognize the symptoms of ACS. This couldlead to the patient being mistakenly assessed as suffering from cognitive impairmentor dementia, and the underlying causes not being investigated (16, 146, 191 - 193). In clinical practice 32 % to 67 % non-identified cases of ACS have been reported (16).
The agreement between nurses' opinion about patient's symptoms and the patients cognitive orientation according to the result of the SPMSQ was only 58 % amongpatients who were cognitively impaired (189). Failure to diagnose i.e. to recognize and treat ACS in a correct way is in turn connected with a poorer treatment outcome (194).
Cognitive tests
Precise and reliable assessment of the mental status in elderly patients within the field of emergency care is essential as changes in cognition and behavior often are the first symptom of an underlying psycho-physiologic disturbance (195). A large number ofmental tests have been designed for clinical assessment and diagnosis of organicmental disease. There is a recommendation in the literature of using a combination of two or more instruments for assessing ACS in clinical practice as well as in research.
A brief cognitive test, a diagnostic tool, and a severity scale should supply these demands (196). With regard to an existence of decline in cognitive function from a previously high functional level a measurement scale should record alterations in mental state rather than only current state (81).
The brief cognitive tests as the Mini-Mental State Examination (MMSE) (118) and theShort Portable Mental Status Questionnaire (SPMSQ) (101) have been frequently used as screening tests for cognitive impairment. The instruments assess different aspects of cognitive function, generating scores that are considered as markers for cognitive impairment. The symptoms of cognitive impairment may be symptoms of dementia or any other mental disorder influencing cognitive function and not only ACS (196). The MMSE has been widely used in clinical practice and has been shown by several authors to demonstrate adequate sensitivity and specificity in the detection of cognitive loss, delirium and/or dementia in various populations (81). However, various limitations to the MMSE have been identified. One reported deals with that people with low education tend to give false-positive responses (197). Furthermore, the MMSE includes items with writing and drawing which could be difficult tasks to standardize for elderly bedridden or otherwise disabled patients (198).
The SPMSQ have been validated with similar rates of sensitivity and specificity to that of MMSE (81, 199, 200), and with regard to dementia and acute confusional state (ACS) and Scandinavian conditions (201). The SPMSQ, judged as quick and easy to administer, includes 10 items in which the patient is assessed according to a nominal scale (right/wrong answer). A cut-off score of <8 SPMSQ points out of 10 correct answers has been considered to indicate cognitive impairment (8, 189, 202)(Appendix 1).
A screening and diagnostic tool as the Confusion Assessment Method (CAM) (202) was developed on the basis of the DSM III (49) (196). It consists of nine questions to be answered by the examiner after a structured interview with the patient (202). TheCAM has been used in research to study the occurrence of ACS and to diagnose ACSin various different settings, by nurses as well as by physicians (203). Several researchers have recommended that there is a need of training for those who use theCAM, especially when it is administered by non-physicians (196).
A severity scale as The Memorial Delirium Assessment Scale (MDAS) (204) has 10 items rating awareness, orientation, short term memory, digit span, attention, thinking, perception, delusion, psychomotor activity, and sleep-wake cycle. Each item has four well-defined scale points from zero to three indicating none, mild, moderate and severe disturbance. Three items are test items including orientation, short-term-memory, and digit-span, while the remainder is based on the rater's observations of thepatients' behavior. The scale has primarily been used by experienced psychiatrists(196)
A scale developed for clinical evaluation of disturbances of awareness and orientation together with other signs of confusion in elderly patients is the Organic Brain
Syndrome Scale (OBS Scale) (205 - 207) (Appendix 2). The OBS scale consists oftwo subscales: ‘OBS 1 – The disorientation subscale' and ‘OBS 2 – The confusion subscale'. OBS 1 is an interview scale with 16 questions and describes the patients´awareness of and orientation to own identity, time, place, and knowledge about some general topics. The patient is assessed according to a four-point ordinal scale with a detailed description given for each level (0 – 3) where zero indicates a correct response, while 1, 2 and 3 indicate slightly, moderately or completely wrong answers(205 - 207). OBS 2 is an observation scale with 39 clinical items and with a longertime perspective (a seven day period), covering different cognitive, perceptual, emotional, social interactions and personality changes and fluctuations in clinical condition. The severity of the symptoms is ranked in a four point ordinal scale (Jensen et al., 1993, Gustafson L et al., 1985, 1995). The assessment procedure with the OBSScale is always started with three questions concerning the patients' hearing, vision and speech (206, 207).
The OBS scale has been used in a number of Swedish studies for assessing mentalstatus in elderly both in the original form (62, 208 - 214) and in a modified version were OBS 1 has been reduced to 12 items and the OBS 2 to 21 items as variables affected by the hip fracture per se were excluded (7, 10, 19, 23, 33, 37, 46, 146). Atotal score of six points when a maximum of three variables have been added togetherhas been used by a majority of the researchers as representing normal mental functioning (7, 10, 19).
The OBS scale has been compared with the CAM (202) showing a 100 % agreementregarding the diagnosis of postoperative ACS as classified in the DSM-IV (215) and referred to as a standardized mental test similar to the CAM (216, 217). The agreement between clinical assessments based on the criteria stated in DSM-IV, and the scores on the OBS scale 1 showed an exact agreement of 96.2 % (Kappa-coefficient 0.77 (95 %CI, 0.71 – 0.83)) (10). Comparisons between the OBS scale and the MMSE based upon correlations between the patients´ scores in the assessments scales showed satisfactory concurrent validity (OBS 1: r=0.56, OBS 2: r=0.75) (207). Another strong correlation (r=0.90) between the OBS 1 and the MMSE gave evidence of a satisfactory criterion-related validity (63). In several studies, carried out by experiencedresearchers and clinicians, the OBS scale has shown satisfactory inter-reliability(rs = 0.7 – 1.0), and more than 90 % identical scores (7, 19, 23, 24, 35, 146).
RATIONALE FOR THE THESIS
Previous research has enabled the identification of frail elderly patients who are at increased risk of developing ACS in connection with hip fracture and acutehospitalization. The overall knowledge concerning important factors that can precipitate and accelerate the development of ACS is increasing, as well as the knowledge of how to prevent the development of ACS. By baseline assessments of the patient's cognitive and physical condition elderly patients at risk can be identified and preventive treatment can be started. By early identification the treatment and care could be directed towards those elderly patients in best need. Consequently, this wouldmake it possible to avoid a prolonged length of hospital stay, including the risk of anextended suffering for the elderly patient, and also the increased costs for the society. Furthermore, the possibility for the patients to return to earlier functional level would be possible to improve.
Due to decreasing resources in the public medical care and service, decreased time in hospital stay and an increasing number of elderly people, constitute a growing clinical problem regarding the rehabilitation of the elderly patients with hip fracture. This is a problem of concern for the society, as the elderly patients shall return to their own home, if possible to the same functional level as before the fracture.
The overall aim of this thesis was to increase knowledge about underlying causes andperioperative risk factors of Acute Confusional States, ACS, in elderly patients withhip fracture and to investigate the effect of a multi-factorial intervention program in order to decrease the number of patients who develop ACS.
The specific aims were:
Study I: To describe elderly patients with a hip fracture on the basis of the ASAclassification system and to identify preoperative risk factors in relation to the postoperative outcome measured up to four months after surgery.
Study II: To identify perioperative risk factors in relation to postoperative outcome up to four months after surgery in elderly patients with a hip fracture, described on thebasis of the ASA physical classification system.
Study III: (1) To examine critically the OBS Scale using the criteria and guidelinesformulated by the SAC for the evaluation of assessment instruments; and (2) to investigate its relevance and suitability for use in various clinical settings.
Study IV: To investigate whether an implementation of a multi-factorial intervention program including prehospital, pre-, intra- and postoperative treatment and care can reduce the incidence of acute confusional state (ACS) among elderly patients with a hip fracture, lucid at admission to hospital.
Design and study description
In study I and II a descriptive, cohort design was used, using data prospectivelyregistered and data retrospectively collected from medical records and nursing charts.
The design used in study III was a two-stage strategy for identifying and reviewing scientific papers. The first stage involved systematic research from scientific databases (PuBMed and Cinahl), the second stage included analyses of papers selected in relation to the Scientific Advisory Committee of the Medical Outcomes Trust's (SAC) eight criteria for instrument assessments (218). In study IV a quasi-experimental, nonequivalent comparison group design was used (219).
In study I, II and IV the studies were based on data collection from the national quality register RIKSHÖFT. The studies were conducted at the Lund University Hospital,having a total of 1.150 beds, and a local catchment area of approximately 240 000inhabitants of the nine million inhabitants living in Sweden. In study IV the study was also conducted in the Prehospital-Ambulance care, represented by five ambulancestations in the same catchment area. Study IV was preceded by a detailed registration of the logistics of the patient's procedures from where the injury took place to admission at the A&E and throughout the hospital care period, regarding nursing care and medical treatment. This registration was repeated in six patients.
The sample for study I and II derives from patients treated for a hip fracture during theperiod September 1st – December 31st, in the years 1999, 2000 and 2001. The sampleincluded 436 consecutive patients with a hip fracture, aged 65 years or older, living inthe local catchment area of Lund University Hospital, and admitted to the Department of Orthopedics. Of these patients eight were excluded; five patients fractured whileabroad, one had bilateral hip fractures, one was moribund and one patient had died before surgery. Of the remaining patients (n=428) were 73 % women (mean (SD) age 82.9 (7.5) years) and 27 % men (mean (SD) age 81.6 (7.3) years) (Figure 3).
Eligible patients
2 fractured abroad
3 fractured abroad
1 bilateral fractures
1 moribund, no operation
Included in primary analysis
Figure 3. Flow-chart of the patients in study I and II.
In study III the sample consisted of 30 scientific papers selected using the following MESH terms and keywords: confusion, delirium, acute confusional state, hip fractures, aged 65+, elderly, organic brain syndrome, and OBS Scale. Only original papers in English language publications were included. Through systematic database search (PubMed and Cinahl) from 1966 to January 2005, 453 scientific papers were found. Through manual searches from literature citations and reference lists 8 papers were found. Of the 453 papers found in databases, 431 were excluded as the OBS scale was not used (Figure 4).
Internet database search: 453 papers
Excluded: not including the OBS scale: 431 papers
Result of data collection: 22 papers
Result of literature citations: 8 papers
Final result of data collection: 30 papers
Figure 4. Flow-chart of the literature search from databases and literature citations.
The sample for study IV derives from 276 patients, consecutively included, aged 65 years or older, and lucid at admission to hospital, treated for a hip fracture at the Department of Orthopedics, Lund University Hospital, during the period April 1st,2003 - April 5th, 2004. On October 1st 2003 a new evidence based program including prehospital and perioperative hospital treatment and care was introduced. One patient denied participation in the study and was not included. History of previous cognitive impairment, severe neuropsychiatric illness, difficulties to communicate, multi-trauma and no operation resulted in exclusion of twelve patients initially included; three patients had no operation (one was moribund, and died before surgery, two were treated conservatively), nine patients showed to have a diagnose of senile or vascular (n=2) dementia, or a history or treatment of previous psychosis (n=2), or ACS (n=5).
Thereby 132 patients remained in the control group (CG) and 131 patients in theintervention group (IG) (Figure 5).
Patients assessed for eligibility
(SPMSQ 8 correct answers)
1 patient in Control groupdenied participation
Included in Control group
Included in Intervention group
1 had no operation
2 had no operation
3 had history/treatment of
6 had history/treatment of
previous ACS, dementia
previous ACS, dementia
Included in primary analysis
Included in primary analysis
Figure 5. Flow-chart of the patients in study IV.
Data collection
Study I and II
In study I and II the majority of data were collected prospectively within the national
quality register RIKSHÖFT (Primary registration form, Q-reg 99 form, and 4-months
follow up form). Most of the registrations of the RIKSHÖFT were made by the
coordinator of the study (AH). The coordinator also interviewed the patients and
assessed their mental status (SPMSQ) within 24 hours after admission and before surgery. Follow-up registration was completed at the patients' 4-months follow-upvisit by the responsible orthopedic surgeon or if hospital visit was not needed, by thecoordinator over the telephone. If at this time a patient was unable to answer, a next of kin or a caregiver was interviewed. ASA-classification was collected prospectivelyfrom the Anesthesia register (database).
A chart review based on manual collection of data from the patient's medical record and nursing chart was performed retrospectively by the author (KBB). In study I collected data included baseline information (admission data) concerning prescribedmedications, presence of any neuropsychiatric illness and/or confusion, laboratory results (blood levels of hemoglobin, plasma levels of sodium, potassium and creatinine), oxygen saturation (SpO2, pulsoximetry), and systolic blood-pressure (SAP).
In study II collected data included all the data collected in study I together with dataconcerning the perioperative period including SpO2, SAP, intravenous (i.v.) infusions, analgesics and sedatives, anesthetic technique, blood-losses, and blood transfusions.
Data collected from the Anesthesia register included anesthetic technique and clock hours. Data collected from the A&E register included time for admission anddischarge calculated for a subsample of 249 (58 %) patients, admitted to hospital during September 1st to December 31st the years 2000 and 2001. No informationregarding clock-hours at the A&E was available for patients admitted during the samemonths in 1999. Information concerning deceased patients was obtained from theSwedish official death certificates.
Study III
In study III all data were collected from 30 scientific papers referring to the OBS scale
and in relation to the SAC's eight criteria for instrument assessments i.e. Conceptual
and measurement model, Reliability, Validity, Responsiveness, Interpretability,
Respondent and administrative burden, Alternative forms of administration, and
Cultural and language adaptations (translations) (218, 220). All data were also
collected in relation to clinical suitability.
Study IV
In study IV all data at hospital admission were collected by the two researchers
managing the study (KBB and AH). Throughout the year the patients with a suspected
hip fracture (shortened and externally rotated leg or history of a fall with subsequent
pain) were admitted to the hospital, one of the researchers was always available, day
and night, when called on, to appear within 30 minutes at the A&E. Patients were
informed orally and in written about the study and thereafter asked about participating
in the study. Written informed consent was obtained from the patients. The researcher
included the patient into the study, accompanied the patient to the ward and informed
the staff that the patient was included. The majority of patients were transferred and
treated in one of three orthopedic wards. In case of no beds available, the patients were treated in another hospital ward (24 patients).
All patients were visited daily at similar hours by one of the researchers, irrespectively of ward. Assessments for ACS, SpO2, physical status and pain were performed daily for eight days or shorter if the patient was discharged earlier (Figure 6). Onpostoperative day five, blood samples (hemoglobin, hematocrit, sodium and potassium) were carried through.
A standardized case report form (CRF) followed the patient throughout every unit; prehospitally, at the A&E including the X-ray department, the orthopedic ward preoperatively, anesthesia/operating department, recovery-room/postoperative unit,and postoperatively in the orthopedic ward. Besides an initial brief information about the study the CRF included clock-hours for arrival/departure, SPMSQ, assessments of pain (measured as pain: yes/no, and as intensity of pain: 1 to 10) (221), SpO2, blood pressure, heart-rate, body temperature, laboratory tests (blood/urine), fasting periods, oxygen supplementation, intravenous (i.v.) infusions, analgesics and sedatives, anesthetic technique, blood-losses, and blood transfusions. All nurses working in theambulances or in the different wards had been informed how to use the CRF and howto evaluate the patient clinically, assisted by the researchers.
Data collection/
Oxygen saturation
Oxygen supplement
Intravenous infusion
Blood transfusions
Prehosp=Prehospitally, A&E=Acute and Emergency department, Periop=Pre, intra, and postoperatively, SPMSQ = Short Portable Mental Test, OBS 1=Organic Brain Syndrome Scale 1, DSM-IV=Diagnostic Statistical Manual 4thEd
Figure 6. Flow chart of the data collection and assessments during study IV.
Assessments in study IV
Cognitive status All patients with a suspected hip fracture were interviewed and screened by one of the researchers for lucidity using the SPMSQ within 30 min after admission to the A&E. Inclusion criteria for participating in the study were 8 correct answers, indicating normal mental functioning.
Screening for ACS Patients giving their informed consent to participate in the ACS study were assessed with the OBS 1 scale within four hours after admittance to hospital. The patients were thereafter tested with the OBS 1 scale on a daily basis by one of the researchers during the first eight days, or until the patient was transferred to another hospital or rehabilitation unit, or was not fit to be tested due to medical complications. Patients transferred to a nearby hospital in near connection to surgery (day 1 - 4) were followedup through a visit on the fifth day by one of the researchers and tested with the OBSscale. Postoperatively the patients were tested a minimum of eight hours after anesthesia was completed avoiding possible effects ascribed to premedication and/oranesthetic agents (Berggren et al., 1987). The tests took place under as calm and quiet circumstances as possible, and at similar hours every day. Patients showing sign ofACS when tested with the OBS scale, or reported by the nurse as having a confusionalstate were evaluated in relation to the DSM-IV criteria of delirium (52) on a later occasion by a psychogeriatrician. One patient in the study with deaf-mutenesscompleted both questionnaires in writing. For another patient not native to Sweden, thequestionnaires were translated by an orthopedic surgeon speaking the same languageas the patient. Both patients only presented test results indicating normal mentalfunction.
Demographic data Information regarding patients' demographic data was registered in the Swedishnational quality hip fracture register RIKSHÖFT, in which ASA-classification andSPMSQ were also included. Information regarding deceased patients was obtainedfrom the Swedish official death certificates.
ASA-classificationAll patients undergoing surgery were routinely examined preoperatively by the anesthesiologist in charge. Patient's physical status was assessed according to the American Society of Anesthesiologists classification of physical status (99). Theassessment was registered in the anesthesia journal by the anesthesiologist or the nurse anesthetist, primary responsible for the patient in the operation department.
PainAssessments of pain were made prehospitally, at admission to hospital, before and after pain treatment. Thereafter pain assessments were made at least twice a day until the eighth day. In connection with surgery, anesthesia and the direct postoperativecare, pain was assessed at arrival at the departments and after pain treatment. Pain wasmeasured as pain: yes or no, and as intensity of pain according to a numerical rating scale (NRS) from 1 to 10 either verbally or marked manually on a ruler (221).
Oxygen saturation Oxygen saturation (SpO2) was measured prehospitally, at admission to hospital, before and after five minutes of oxygen treatment (intervention group). Thereafter SpO2 wasmeasured at least twice a day until the eighth day. In connection with surgery, anesthesia and the direct postoperative care, SpO2 was assessed at arrival at thedepartments and thereafter continuously. SpO2 was assessed by using pulse oximetry(Tuffsat®). Every patient was connected to a portable pulse-oximeter at the A&E untilthe fifth day. In the operating room the pulsoximetry was part of the anesthesiaequipment, while in the recovery room part of the standard monitoring. All patients irrespective of group showing SpO2<90 % after arrival to the A&E were reported bythe researchers and treated with supplemental oxygen SpO2.
Body temperaturePatient's body temperature was measured with an ear thermometer with infra-red light (First temp Genius®) at admittance to hospital and thereafter twice daily. Extra measurements were made during anesthesia and postoperatively in the recovery room,or if the patient was hypo- or hypertherm. During surgery treatment with forced-air warming and warm i.v. solutions to prevent unintended hypothermia/ maintainintraoperative normothermia was included in the intervention program (222 - 224).
Blood samplesFor all biochemical tests at admission and postoperatively on day five the standard laboratory SS-EN ISO/IEC 17025 was used. Test routines were kept according to theinstructions given by the Department of Clinical Chemistry and Pharmacology,University Hospital, Lund.
Intervention in study IV
The intervention including prehospital and perioperative hospital treatment and care of patients with hip fracture, introduced in October, 2003, was based on clinical evidence and current knowledge about risk factors associated with ACS in elderly hip fracturepatients (6, 7, 10, 39, 64, 122, 138, 139, 144, 145, 150, 163, 214, 224 - 228). TheIntervention Group (IG) was treated according to the new evidence based program (6, 7, 19, 35, 39, 64, 122, 125, 127, 138, 139, 142, 144, 145, 149, 150, 156, 157, 159, 163,
165, 166, 178, 188, 205, 207, 223, 226, 227, 229, 230 - 235) (Appendix III), while the Control Group (CG) admitted before October 1st 2003, received care according to standard clinical practice for patients with a hip fracture (91). According to current care treatment principles of the Orthopedic department before October 1st all patientshad surgery within 24 hours if possible, were treated with a permanent urine bladdercatheter during surgery and the first postoperative day, had antibiotic prophylaxis,anticoagulation prophylaxis with low-molecular-weight heparin for approximately 10 days postoperatively, and when possible, were mobilized within the first postoperative day (a.a.).
Standard care vs. Intervention
Supplemental oxygen was not a standard treatment in elderly patients with a suspected hip fracture either prehospitally nor at the A&E or the orthopedic ward at Lund University Hospital, even if the time spent on a trolley before entering the orthopedic ward many times could be more than six hours. Supplemental oxygen started normally first immediately before the introduction of anesthesia. In the intervention program supplemental oxygen 3 - 4 L/min started already prehospitally (225, 226).
Standard supplemental nutrition or intravenous (i.v.) liquid for elderly patients withhip fracture at the Lund University Hospital was, often after several hours as the diagnosis was settled through X-ray examination, one liter of i.v. saline/glucose preoperatively. If surgery was not close at hand the patient was offered a glass of milkand a sandwich. Extra nutrition was only given in special cases or in cancer patients.
Intravenous fluid supplementation already in the ambulance or directly after arrival at the A&E together with extra nutrition (nutritional drinks given postoperatively) was a second part of the intervention program (225).
According to standard clinical practice the patient's oxygen saturation was not checked either prehospitally nor preoperatively. The regimen of the Orthopedicdepartment of Lund University Hospital regarding treatment with blood transfusion inelderly patients with hip fracture was restrictive even if the hemoglobin level in bloodindicated severe anemia (100 g/L or lower). Patients with cancer or specific anemic diagnosis were excluded. Increased monitoring of vital physiological parametersespecially oxygen saturation, hemoglobin in blood, blood pressure, and temperaturewas a third part of the intervention program. The patient's saturation of oxygen was monitored continually and registered at least twice a day (225, 226).
Standard prehospital care and treatment of elderly patients with a suspected hip fracture in the local catchments area of Lund University Hospital did not include any analgesic drug administered before moving the patient or prior to admittance to hospital (236). After arrival at the A&E the patient was usually offered some treatmentfor pain (opioids and/or paracetamol) even if the administration of the drug was accomplished depending on organizational factors, such as a room or nurse available,
or an orthopedic surgeon available for prescription. Adequate pain relief directly after arrival in the A&E was as a fourth part of the intervention program (100).
All patients with a hip fracture at the A&E were, after the initial assessment by the orthopedic surgeon in charge, transmitted to the X-ray department according to the standard routines. After X-ray the patient had to return at the A&E for laboratory testsand further assessment before transfer to the orthopedic ward, often several hours later. Avoidance of delay in assessment and treatment routines and transfer logistics by direct referral to orthopedic ward after X-ray was a fifth part of the new program(100, 226).
All patients with a hip fracture were screened for lucidity within 24 hours afteradmittance to hospital by using the SPMSQ test. No further screening or testing was accomplished thereafter. Screening for ACS through daily testing with the OBS scalewas a sixth part introduced in the new program (206 - 208, 225, 226, 237).
No special guidelines were used regarding polypharmacia in elderly patients besides basic principles for drug interaction. Avoidance of polypharmacia especially sedatives and hypnotics and drugs with anticholinergic properties was a seventh part of the intervention program (7, 19, 225, 226).
The administration of i.v. analgesic prior to patient's transfer to the operation was not regulated by guidelines in the Anesthesiological department. Instead, this was up to every single nurse anesthetist to decide. As anesthetic technique spinal as well as general anesthesia was used frequently. Sedation during spinal anesthesia with i.v. propofol and/or midazolam was common. Intravenous opioids as postoperative analgesia were used as routine. In the eight and final part of the intervention programparacetamol as premedication, and spinal anesthesia preceded by 0.5 L of i.v. saline-acetate was recommended as first choice. Administration of i.v. propofol and/oralfentanil was recommended before patient's transfer to the operation table. Blood pressure and hemoglobin should be kept at normal levels, and red blood celltransfusion given if tendency of increased blood loss. Paracetamol should be includedas first choice postoperatively, or in combination with an i.v. opioid (100, 226)
Study I, II and IV
In study I, II and IV significant differences between groups including categoricalvariables were established using the Chi-square test and, when appropriate, Fisher's exact test (238). For continuous variables judged as normally distributed, Student's t-test was used, and for ordinal data or variables with skewed distributions, the Mann-Whitney U-test was used. Most of the data were not normally distributed and were therefore expressed with Median and Percentiles (q1 - q3) or Range. For parametric data Mean and Standard Deviation (SD) were used. For analyses between more thantwo independent groups One-way ANOVA with Bonferroni Post Hoc test for multiple comparisons to reduce the risk for mass-significance was applied (Study II) (238). For analyses of differences regarding physiological variables monitored at different occasions, Paired samples t-test and Wilcoxon's signed rank test were used (Study II) (238). P-values of <0.05 were considered statistically significant (Study I, II, and IV). Due to multiple comparisons in study II a reduced p-value (p<0.003) was used to control for the risk of mass-significance (239).
In study I, II and IV and due to the small number of patients in the ASA 1 and theASA 4 classes, patients were lumped and divided into two categories: ASA 1 and 2,and ASA 3 and 4.
In study I and II multiple logistic regression analyses (backward, likelihood ratio) were performed to identify factors predicting each of four outcome variables (‘Deceased within four months', ‘Postoperative confusion', ‘Registered in-hospital complication' and ‘Length of hospital stay'). One set of baseline variables was tested as independent variables in these analyses in paper I. In study II independent variables were entered in two steps. Firstly, baseline variables were entered, and those showing significant association with the respective outcome variable were kept in the next step, whenperioperative variables were added as predictor variables. Variables that in bivariate analyses were associated with the outcome variable with a p-value <0.2 or being clinically significant were included in the model. Dependent variables were dichotomized 0 = no/ best outcome and 1 = yes/worst outcome. Independent variableswere categorized according to clinically accepted cut-off values, based on previous studies or according to the median/mean values of the sample. They were either dichotomized into 0 = as less risk/better and 1 = as increased risk/worse, or dummy coded with the best item as reference e.g. undisplaced cervical fracture. The variables used for selection were age at fracture, gender, admitted from/living condition, walking ability, prescribed drugs, ASA score, dementia diagnosis, SPMSQ, fracture type, hemoglobin, potassium, blood creatinine, SpO2, waiting time for operation, hypotension during anesthesia, fasting time, anesthetic time, and blood transfusion.
Due to multicollinearity with dementia diagnosis, SPMSQ score was not entered in three of these analyses. In 90 patients preoperative SpO2 values monitored at admission in the operating department were missing. In order to get enough number of SpO2values in the analyses, SpO2 values for 44 patients registered in the A&E, and the
lowest SpO2 values registered on 40 patients during anesthesia (100 % received oxygen) were imputed. The relative importance of various predictors of outcome was presented as odds ratios (OR) with 95 % confidence intervals (CI). The model was tested with the Hosmer and Lemeshow goodness-of-fit test (240). Good model fit is indicated by non-significant chi-square value. The fit of the logistic regression modelfor every outcome indicated good model fit. Data were analysed using SPSS for Windows (version 11.5 and 14.0, SPSS Inc., Chicago).
In study IV, before the study was started, the required sample size was calculated. This was done in order to estimate the chance of detecting a statistically significant difference in incidence of ACS in the intervention group compared to the controlgroup (238). We had estimated a clinical effect of 50 % to be of clinical significance due to the results in incidence of previous studies in the special field (7, 8, 10). A power of at least 80 % was required with a p-value of less than 0.05. A sample size of300 patients was calculated to detect a 50 % reduction of ACS in the interventiongroup compared with the control group given the usual care.
Study III
The analyses in study III followed the SAC's eight attributes and review criteria which are based on current norms and principles of modern test theory as guidelines for evaluation of instruments (218, 241, 242). These guidelines were chosen due to the fact that SAC was created as a non-profit, international and independently operating entity with a commission to identify and review health status, functioning and quality of life instruments (220). Hence, the OBS scale was analysed and evaluated in relationto how the OBS scale had been performed, tested and used, presented in the 30scientific papers and in relation to the eight criteria of the SAC; the conceptual andmeasurement model i.e. its underlying rationale for and description of concepts and thepopulation that the OBS scale was intending to assess. Furthermore, the reliability ofthe OBS scale i.e. the degree to which the instrument is free from random error including the internal consistency and reproducibility, and its validity i.e. the degree to which the OBS scale measures what it is intended to measure covering content-related,construct-related and criteria-related validity. Moreover, the responsiveness of the OBS scale referring to its ability to discern change over time, and the interpretabilityreferring to the degree to which the data and meaning of the OBS scale's quantitative scores can be easily understood. Other criteria were respondent and administrativeburden aiming at the time, efforts and other demands that are put on the respondentand the administrator of the scale, alternative forms of administration, referring to other ways in which the scale might be used, and cultural and language adaptations(translations) including assessment of conceptual and linguistic equivalence and evaluation of measurement characters (218). Furthermore all data in the scientific papers were analysed and evaluated in relation to clinical suitability with regard to different clinical settings and patient populations in which the OBS scale had been administered or used.
In the analyses presentations of concept dimensions (factor analysis), modifications ofthe OBS scale, scale levels and steps, scores and target populations were looked for. Furthermore, presentations of inter-rater reliability (Spearman rank correlation), exact agreement between raters (Cohen's Kappa), overall reliability measured as internal consistency (Cronbach's alpha), test-retest or intra-class correlations (Spearman rank correlation). Moreover, the exact agreement with other scales, concurrent and discriminant validity, sensitivity to changes, prediction of illness, diagnostic criteria and evaluation of treatment were also looked for in the analyses (241, 242).
In this thesis the ethical principles for research in human subjects according to the Declaration of Helsinki (1989) and outlined by the World Medical Organization (WMA) 1996 have been followed (WMA, 2002) (243).
The projects in this thesis involved elderly person who earlier or just previously hadbeen affected by acute illness, signifying several different moments of stress, experienced as very trying and with the effect that the elderly person was not always able to assert her or his rights, will or wishes. The basic ethical principles of clinical research as respect for autonomy, beneficence, non-maleficence and the principle of justice were therefore taken into account (243). The research projects were alsoobliged to follow the Ethical Code for Nurses, outlined by the International Council of Nurses (ICN) including four basic areas of responsibility: to promote health, to prevent illness, to re-establish health and to alleviate suffering (244). Before the studies (I, II and IV) were started, potential ethical considerations were highlighted.
A consequence of the principles of non-maleficence (doing no harm) and beneficence(doing good) as far as it is possible was for this project to search for new knowledgewith the aim to be able to improve methods for diagnosis and treatment as well as prevention in relation to the risk of developing ACS in connection with a hip fracture (242). Potential risks of doing somebody harm should be redeemed by the benefit of possible improvements and a reduction of the suffering that may exist for those elderly in the future being in the same situation. Besides, the result of the projects might gain the society in the future through a possible reduction in healthcare costs. The benefits for the closely related could consist of getting more familiar with and a better comprehension of the underlying factors of the elderly reactions connected to acuteillness.
All patients with a hip fracture admitted to Lund University Hospital are registered in the RIKSHÖFT quality register. Before registration the patients are informed verbally and in writing. The RIKSHÖFT was approved by the National Bureau forComputerized Registration (87-3278) in 1988. The responsibility of the register has since 2003 been transferred to the Region Skåne (98).
In study I and II a major ethical dilemma existed as none of the persons in the population had been informed in advance and asked about participating in the study.
Consequently none of the persons involved had had the possibility to deny any participation in the research project. There were two ways of solving this dilemma; either to contact every person individually or to inform the patients through an advertisement. The latter was chosen and in line with the recommendations of TheEthics Committee of Lund University. This was accomplished through extendedinformation about the study and its purpose, including the possibility to denyparticipation through contact with the researcher, and presented in the largest daily newspaper of the South Region of Sweden. No patient denied participation. In study I and II the included data prospectively collected from the RIKSHÖFT and data
retrospectively collected from medical records and nursing charts were coded and handled with confidentiality. Consequently with regard to every person's right of autonomy, integrity and a private life, it was not possible to identify any individual inrelation to the results presented (245).
In study III no major ethical dilemmas were of hand as the study object solely comprised scientific results already published.
In study IV several ethical considerations were of hand. Firstly, the principle of justice as only patients 65 years and lucid at arrival to hospital (SPMSQ 8 correct answers) were consecutively included in the study. The remaining patients (<65 years, SPMSQ<8 correct answers, history of previous cognitive impairment, severe neuropsychiatric illness, difficulties to communicate, or multi-trauma) were not included. Due to the fact that persons 65 years of age or older, without early history of cognitive impairment or confusion were at risk, or increased risk of developing ACS while in hospital, and with regard to the aim of the study, we chose to exclude those notfulfilling the inclusion criteria. The included patients were all treated equally and asked to participate regardless of gender, nationality, race and social status. However, all patients with hip fracture living in the local catchment area of Lund UniversityHospital and admitted to the Department of Orthopedics during the study period wereconsecutively included in the larger population-based study (n = 478) with the aim to reduce the incidence of pressure ulcer and other complications, reported elsewhere (22).
Consequently all the patients throughout the year took part in the increased monitoringand daily visits by the researchers including other assessments besides the rating with the OBS scale. For any reason a patient or staff wished to encounter the two researches (KBB and AH), there was always one available 24 hours a day, and every day the year around. As the researchers were not involved in the care of the patients, nodependency was considered to exist between the researchers and the patients.
For ethical reasons and the principle of doing good and no harm, no blood testsperformed in the study, irrespectively of if the patient belonged to the control group or the intervention group, were hidden for the staff involved. Furthermore, all patients in both groups showing SpO2 <90 % were reported by the researchers and treated with supplemental oxygen. Whenever a patient showed sign of ACS this was reported to the responsible nurse.
Secondly, the principle of autonomy was considered. Prior to entering the ACS study, after being informed about the registration in the RIKSHÖFT and tested with the SPMSQ test, the patients were given oral and written information about the ACS study. Information was given to the patient and her/his next-of-kin that the participation in the study was voluntarily and possible to interrupt at any time. Any person, when asked about participation, finding it difficult to use her/his right of self determination was encouraged by the researcher to get support by the next-of-kin. Thenext of kin was given separate written information but with the same content. If absent at the patient's admittance, written information was send by mail to the next-of-kin.
Written informed consent was obtained from all patients, except one who denied participating.
Every assessment with the OBS scale was carried through during as calm and quiet circumstances as possible. Before the test started the patient's hearing and seeing was investigated. If the patient showed any signs of distress or being tired, the researcher made a short break before continuing the questions. The researcher always tried to becareful and sensitive with regard to the patient's physical and mental condition, and assupportive as possible if the patient showed any sign of being confused (10). If a patient was in need of support or to talk, the researcher stayed by the patient for a while. All assessment data including the OBS scale were made anonymous by coding and kept separately and confidential. Every patient and her/his next-of-kin were informed explicitly in the written information sheet how to get in contact with the researcher in case any questions were of hand after the study had finished.
Study I, Factors at admission associated to 4-months outcome in
elderly patients with hip fracture
Study II, The influence of perioperative care and treatment on 4-
months outcome in elderly patients with hip fracture
Patient characteristics in Study I and II are summarized in Table 5 and 6.
Table 5. Demographics and functional status in relation to ASA 1+2 and ASA 3+4 in Study I
and II.
201 (77.9)/57 (22.1)
111 (65.3)/59 (34.7)
Age (years) Mean (SD)
Sheltered/Institutional care
No mental illness
Post stroke/others
8 correct answers
<8 correct answers
Comparisons are between ASA 1+2 and ASA 3+4. Results are presented as number of patients(percentage). Concerning age Mean (SD) is used. ASA = American Society of Anesthesiologists'classification of physical status*)Pearson Chi-squared test or Fisher's Exact test†)Student's t-test‡) Missing patients: ASA 1+2: 35 (13.6)/ASA 3+4: 28(16.5)
About 60 % of the patients included in Study I and II were classified as ASA 1 and 2 and 40 % as ASA 3 and 4. Men compared to women were more commonly classifiedas ASA 3 and 4 than ASA 1 and 2 (p=0.005), lived significantly more often together with someone (42.2 % vs. 23 %, p<0.001), and got their fracture more often outdoors(18.3 % vs. 9.0 %, p=0.010). Of the 272 patients (64 %) who were able to walk alone
outdoors or indoors, 69 % and 56 % belonged to ASA 1 and 2 and ASA 3 and 4 groups, respectively (p=0.012).
Table 6. Biochemical and physiological variables at baseline and perioperatively in relation to
ASA 1+2 and ASA 3+4 in Study I and II.
Hemoglobin (blood)
Mean (SD) g/L (255 vs. 165)
<100 g/L (%) (255 vs. 165)
Sodium (serum)
Median (q1-q3) mmol/L (248 vs. 160)
139 (137.0 - 141.0)
Median (q1-q3) mmol/L (243 vs. 159)
Median (q1-q3) mmol/L (239 vs. 151)
69.0 (56.0 - 87.0)
71.0 (59.9 - 96.0)
> 100 micromol/L (%)
Oxygen saturation (SpO2) at A&E
Median (q1-q3) mmol/L (110 vs. 85)
96.0 (93.0 - 97.0)
95.0 (92.0 - 97.0)
Oxygen saturation (SpO2) at OD
Median (q1-q3) mmol/L (200 vs. 138)
94.0 (92.0 - 96.0)
93.5 (90.0 - 95.0)
Systolic blood pressure (SAP) at OD
Median (q1-q3) mmol/L (248 vs. 161)
Comparisons are between ASA 1+2 and ASA 3+4. Results are presented as Mean (SD), Median (q1-q3), or as number of patients (percentage). ASA = American Society of Anesthesiologists' classification of physicalstatus.
*) Student's t-test†) Pearson Chi-squared test or Fisher's Exact test ‡) Mann-Whitney U test A&E = Acute & Emergency Department, OD = Operating Department
A SPMSQ score of less than 8 correct answers was found in 99 % of the patients with a dementia diagnosis, and in 18.3 % of the patients without any previousneuropsychiatric diagnose (p<0.001). Confusion present at time of admission orappearing later preoperatively was registered in 18.6 % of the patients. Compared to other patients, patients with preoperative confusion were significantly more often 85years (59.5 % vs. 38.0 %) (p = 0.001), had a dementia diagnosis (57.0 % vs. 17.1 %)(p<0 .001), and/or a SPMSQ score of <8 correct answers more often (78.3 % vs. 32.7 %) (p<0 .001), and also lived in institutional care more frequently (67.1 % vs. 31.0 %)(p<0 .001).
Sixty-three percent of the patients had four or more prescribed medications. The use ofprescribed drugs 4 was significantly more frequent among ASA 3 and 4 groupcompared to ASA 1 and 2 (72.6 % vs. 61.6 %) (p<0.001), among patients 85 years compared to younger patients (72.6 % vs. 61.6 %) (p = 0 .022), and in patients admitted from any dependent living compared to patients living in their own homes (87.2 % vs. 51.0 %) (p<0 .001). Prescribed medications 4 was significantly morecommon among patients with a neuropsychiatric condition compared to other patients(86.7 % vs. 65.0 %) (p<0 .001), and in patients with a hemoglobin <100 g/L compared to other patients (80.6 % vs. 57.8 %) (p = 0 .015). Abnormal levels of hemoglobin,creatinine, potassium (slight increase) and SpO2 were more frequently found in the ASA 3 and 4 group (Table 6).
Fracture type did not differ significantly between the two ASA groups. The mostfrequent types of fractures were the displaced intracapsular (34.1 %), the trochantericwith two fragments (31.8 %), and the undisplaced intracapsular (18.0 %). Patients 85years suffered more often from basocervical fractures and trochanteric with twofragments fractures (46.4 % vs. 29.3 %) (p = 0 .004) compared to younger patients. Screw and plate fixation was the most common surgical method carried out in 48 % of the patients, whereas hemiarthroplasty was performed in 28 %, two screws or pins in 22 %, and total hip arthroplasty in 3 % of the patients.
Delay of surgery, defined as > 24 h, was registered in 45 % of the patients. In the majority of cases the causes of delay were reported to be due to late arrival to hospitalor delayed transport to operating department (23 %) or lack of available operating theatre space, surgeons and anesthesiologists or hospital beds in the recovery unit or the orthopedic ward (57 %). In 14 % of the delays operation was postponed because the patient was considered in medical need of treatment due to fluid imbalance,myocardial infarction, arrhythmia, gastrointestinal bleeding, or adjustment of anticoagulant treatment.
The median time spent in the A&E, including the transport to and fro the X-raydepartment, was for a sub-sample of patients (n=249, 58 %) 3.6 h (range, 0.6 - 9.6 h).
The median intra-hospital waiting time for surgery was 19.4 h (range, 4.3 - 219.0 h). Patients waiting 24 h after arrival (n=134, 33 %) belonged significantly more often to ASA group 3+4 (46 % vs. 35 %) (p = 0.031), and had more often a fasting time of 12h (73 % vs. 52 %), (p<0.001). About 40 % of the patients waiting 24 h had received 1 L i.v. fluid preoperatively.
The median fasting time was 12 h (range, 2 - 56 h). Patients fasting 12 h (n=249, 59 %) belonged significantly more often to ASA group 3+4 (43 % vs. 33 %)(p = 0.026), had more often a waiting time for surgery of 24 h (41 % vs. 21 %), (p<0.001), suffered more often from confusion at arrival or later preoperatively (n=77)(22 % vs. 13 %) (p<0.015). About 55 % of the patients fasting 12 h had received 1 L i.v. fluid preoperatively.
Anesthesia method was either spinal anesthesia (SA) or general anesthesia (GA). The majority of patients (64 %) had SA, of these 70 % had some kind of adjunctivesedation (benzodiazepines (n=56), propofol (n=120), another sedative or ketamine (n=8). About 36 % of the patients received general anesthesia (GA). Peroperative hypotension occurring in 275 (64 %) patients was more frequent in the GA group thanin the SA group (82 % vs. 58 %) (p<0.001). The incidence of hypotension, however,did not differ between the ASA groups. About 95 % of the patients were given analgesics preoperatively, and all patients received postoperative analgesia by meansof morphine, paracetamol, and tramadol hydrochloride. There were no significant differences in pain treatment between the ASA groups.
The median length of stay (LOS) was 10.0 (8.0 - 14.2) days. LOS did not differ between the ASA groups (median (q1-q3), ASA 1+2: 10 (7.0 – 14.0), ASA 3+4: 11 (8.0 – 14.0) (ns)). A significantly shorter LOS was found in patients with undisplacedintracapsular fracture (n=77), median (range) days 11 (2 - 43) vs. 8 (1 - 29) (p<0.05), in patients living in a more dependent living situation (n=157), 12 (1 - 40) vs.
8 (2 - 43) (p<0.001), in patients suffering from a neuropsychiatric diagnosis (n=160), 12 (1 - 43) vs. 8 (1 - 34) (p<0.001), and in patients with postoperative confusion (n=223), 11 (1 - 33) vs. 10 (1 - 43) (p<0 .041).
Measurements and treatments during the care period showed that only 15 of the 31 patients found to have hemoglobin <100 g/L at arrival were treated with one or moreunits of blood transfusions preoperatively. Only 16 of the 58 patients with a SpO2<90% measured at arrival at the operating department had been treated preoperatively with oxygen. In both ASA groups a significant decrease was found in SpO2 between themeasurements performed at the A&E, the operating department, and postoperatively in the orthopedic ward, respectively (Table 7). A significant decrease in hemoglobin wasalso found postoperatively in both ASA groups (Table 7). A blood loss of 0.3 L was present in 121 (29 %) of all patients. A vast majority of these patients had a more complicated fracture, either a displaced intracapsular or a trochanteric two fragmentsfracture. Sixty-five percent of the patients with a postoperative hemoglobin <100 g/L(n=213) were substituted with blood transfusion postoperatively. Of all the patients with a postoperative hemoglobin <100
g/L, 64 % had either a basocervical,
trochanteric, or a subtrochanteric fracture (p<0.001), and 63 % were operated with a screw and plate fixation (p<0.001).
Postoperative outcome presented as ‘4-months mortality', ‘postoperative confusion', and ‘in-hospital complications' showed to be significantly associated with a number of different baseline factors and a number of different perioperative factors as presented in Table 8. Four (1.6 %) patients in ASA 1+2 and eight (4.7 %) patients in ASA 3+4died while in hospital (ns). These patients suffered from respiratory, cardiac, or renal insufficiency, or cancer metastases. The 30-days mortality was eight percent (34 patients) and did not differ between the ASA 1+2 and ASA 3+4 groups. At four months follow-up 68 (16 %) patients had died; 27 (10.5 %) patients in ASA 1+2 and 41 (24.1 %) patients in ASA 3+4 (p<0.001).
Table 7. Differences in SpO2 and Hemoglobin pre- and postoperatively in relation to ASA groups in Study
I and II.
Orthopedic ward
96.0 (94.0 - 98.0)
94.0 (92.0 - 96.0)
93.0 (89.5 - 94.0)
95.0 (92.0 - 97.0)
93.5 (90.0 - 95.0)
92.0 (88.0 - 94.0)
Hemoglobin,
Mean (SD)
Hemoglobin,
Mean (SD)
*) Comparisons are between Acute & Emergency Department and Operation Department preoperatively (ASA 1+2,
n=77, ASA 3+4, n=74)
†) Comparisons are between Acute & Emergency Department and Orthopedic ward postoperatively (ASA 1+2, n=57,
ASA 3+4, n=49)
‡) Wilcoxon´s signed rank test
§) Paired samples t-test
) Comparisons are between Acute & Emergency Department and Orthopedic ward postoperatively (ASA 1+2, n=245,
ASA 3+4, n=156)
Altogether, 223 (52 %) patients suffered from postoperative confusion. Of those, 76 patients already showed signs of confusion preoperatively. Thus, as many as 43 % ofthe patients developed confusion after the operation. Patients who died within 4-months after surgery suffered significantly more often from postoperative confusioncompared to survivors (62.5 % vs. 39.4 %) (p=0 .004), whereas the incidence of postoperative confusion did not differ between the ASA groups (n=345), (ASA 1+2:40 %, ASA 3+4: 47 %), (p=0.197).
Fifty-one percent of the patients experienced in-hospital complications. The incidenceof complications did not differ significantly between the ASA 1 and 2 and 3 and 4 groups. Women had a significantly higher frequency of in-hospital complications than men (56 % vs. 37 %) (p=0.001). The most frequent complication, urine tract infection,was diagnosed in 33 % of the women and 13 % of the men (p<0 .001). The incidence of serious complications such as pneumonia and cardiac or renal failure was 19 %. Patients who died within four months after discharge were more often affected by in-hospital complications than survivors (70 % vs. 47 %) (p=0 .001).
The result of the multiple logistic regression analyses (backward, likelihood ratio), performed to identify factors predicting each of four outcome variables (‘4-monthsmortality', ‘postoperative confusion', ‘in-hospital complications' and ‘LOS'), are presented in Table 9.
Table 8. Postoperative outcome associated with various baseline and perioperative factors. Bivariate
analyses of significance (p<0.05*)), (n=428).
Study I: Baseline factors
Study II: Perioperative factors
Mortality within 4-months
Fasting 12 hours‡)
Peroperative transfusion 1§)
Postoperative SpO2<90 %
Dependency in living
Postoperative transfusion 1§)
Dementia diagnosis§)
SPMSQ <8 correct answer )
Hemoglobin <100 g/L¶)
Creatinine > 100 micromol/L**)
Other fracture than undisplaced
Dependency in living
Postoperative SpO2<90 %
Unable to walk alone/bedbound
Postoperative transfusion 1§)
Dementia diagnosis§)
Postoperative hemoglobin<100
SPMSQ <8 correct answer )
Prescribed drugs 4§)
In-hospital complications
Preoperative SpO2<90 %‡‡)
Dependency in living
Postoperative hemoglobin<100
Unable to walk alone/bedbound
SPMSQ<8 correct answer )
Prescribed drugs 4§)
SpO2<90 % at arrival§§)
Results are presented as percentage of patients. Comparisons are made between following groups: Deceased at 4 -months vs. Alive at 4-months, Postoperative confusion vs. No postoperative confusion, In-hospital complications vs. No in-hospital complications. ASA = American Society of Anesthesiologists' classification of physical status, SpO2 = oxygen saturation, Dependency in living = partially dependent/dependent living, SPMSQ = Short Portable Mental Status Questionnaire. *) Pearson Chi-squared test or Fisher´s Exact Test †) Patients with preoperative confusion excluded (n=76) ‡) n=421 §) n=424 ) n=365 ¶) n=420 **) n=390 ††) n=403 ‡‡) n=422 §§) n=195
+ trochanteric two
eoperative SpO2<90 %
Study II: Risk factors
Displaced intracapsular
Blood transfusion > 1 unit
Dementia diagnosis
Postoperative SpO2<90 %
Blood transfusion
subtrochanteric fracture
subtrochanteric fracture
Blood transfusion
er Hip Fracture in Study I and Study
ses of factors predicting outcom
+ trochanteric two
Study I: Risk factors
Displaced intracapsular
Dementia diagnosis
subtrochanteric fracture
Prescribed drugs
Displaced intracapsular
subtrochanteric fracture
Multiple logistic
Dead within
tive confu-
Length of
>10 days
mi-, and total hip
+ 2 vs. 3 + 4), Prescribed 1
on), Anesthetic tim
walk alone), Anesthetic method
), Walking abilit
mmol/L), Peroperative
ale vs. male), Prescribed drugs
dependent/dependent living
8 vs. <8 correct answers), Walking
100 vs. > 100 m
ble to walk alone), Postope
ears), ASA group (
ears), Prescribed drugs
otension vs. hypotensi
eshow Test > 0.374 in all analy
4 drugs), Dementia diagnosis, Hem
ble to walk alone), Creatinine (
= oxygen saturation.
(able to walk alone vs. unable to
(able to walk alone vs. unable to
4 drugs), SPMSQ score (
Age (<85 vs.
Age (<85 vs.
Age (<85 vs.
OR = Odds Ratio, CI = Confidence interval
Variables not in the final
(able to walk alone vs. una
arthroplasty vs. screws/pins with or without side plate).
(spinal vs general anesthesia), Total blood transfusion
y (able to walk alone vs.
walk alone vs. unable t
+ 2 vs. 3 + 4), Prescribed drugs1
dependent/dependent living
Anesthesiologists' classification of physical
4 drugs), Dementia diagnosis, Hem
swers), Walking abilit
walk alone vs. unable to w
ears), ASA group (
ears), Prescribed drugs
eshow Test > 0.424 in all analy
Dementia diagnosis
ty (able to walk alone vs. unable to walk alone).
ugs), Walking abilit
8 vs. <8 correct an
100 vs. <100 gram
Age (<85 vs.
Age (<85 vs.
OR = Odds Ratio, CI = Confidence interval
Variables not in the final *)
Walking abili †)
unable to walk alone).
Study III, The Organic Brain Syndrome (OBS) Scale: a systematic
review
The result of the analysis showed that in 18 of the 30 papers the criteria stated by the SAC - Conceptual and measurement model, Reliability, Validity, Interpretability, Responsiveness, Respondent and administrative burden, Alternative forms of administration, and Cultural and language adaptations (translations) - were considered(see Table 10). The conformity of the scale with the criteria stated in DSM-III, DSM-III-R and DSM-IV (49, 52, 55) was supported by several studies (7, 10, 210). The tests and cross-evaluations carried out in these studies strongly confirmed the reliability of the diagnosis of ACS thus a confirmation of the usefulness in the populations forwhich the OBS Scale was intended; a conclusion further supported by the literature which has been examined and studied.
In relation to Responsiveness the OBS 1 scale showed to be sufficiently sensitive to recognize, at an early stage, those patients who are at risk of developing an ACS (10). The same author had found significantly higher OBS 1 scores at admission to hospitalin patients who later developed ACS. In several studies the OBS 1 and 2 had been used to detect and follow the clinical course of ACS (7, 19, 21, 35, 37, 63). All patients in the study by Gustafson L et al. (1985) could be described by standardized factor scores in the different symptom clusters, based on factor analysis, and thesymptom profile could be followed during treatment of the confusional state (206-208).
Concerning Respondent and administrative burden the assessment using the OBS 1took approximately 5 - 10 minutes and was possible to integrate into ordinary nursing assessment (10). The assessment with both subscales took about 30 to 60 minutes and the patients never complained of feeling tired during the actual investigation (207, 211).
Regarding Alternative forms of administration two authors suggested that the patients' mental status before the fracture could be judged by interviews with relatives and care staff (21, 212). The observational schedule of the confusion scale, OBS 2, could be grounded on information given by nurses and other staff members, well acquaintedwith the patient's condition and behavioural patterns, and with special training of patients with organic mental disease (206, 207).
In relation to Cultural and language adaptations (translations) the selection and formulation of the items in the OBS Scale were based on a comprehensive review of literature concerning psychogeriatric assessment scales, using Scandinavian research traditions and approaches. The questions in the orientation subscale fulfilled those commonly used to establish the clinical assessment of patients suffering of organicbrain failure (207). Although the OBS Scale was originally founded on Swedish clinical concepts and tradition, it had shown a satisfactory concordance with otherrating scales in the field of organic mental disease.
The structure of the OBS Scale and its clinical applicability has been studied in different clinical settings and patient populations with a wide range of age from 23 years to 102 years and at different departments and hospitals (Table 6). In several studies the OBS Scale had been used to investigate the incidence of ACS and to follow the development of this condition, dementia, different psychiatric profiles and behavioural as well as cognitive symptoms in the elderly population. It has been applied on orthopedic patients, stroke patients, patients in coronary heart and intensive care units (ICU), showing good responsiveness, and comprehensibility in a number of clinical conditions. Compared to other mental tests, in which the patient has been assessed according to a nominal scale (right/wrong answer), the OBS Scale offered several well defined scoring steps which should make it more sensitive to changes in the patient's mental condition.
The OBS Scale in many aspects satisfied the requirements of a valid clinical instrument, though with respect to the eight attributes suggested by the SAC (2002) there is a need for further evaluation of the OBS Scale, especially with regard to reliability such as test-retest reliability and intra-class correlations, and the translation and adaptation to other languages (217).
Cut-off: 6 points
related, Factor analysis
Acute Confusional State (ACS) or ps
30 studies concerning
Identification. ADL-
ACS diagnose test
Identification of
intervention program
Investigating activity of
ogical order from
. Data in chronol
Cut-off: 6 points
10 patients tested
Internal consistency:
Analyzing if CFS
levels r/t clin.
investigation of
with MMSE-scores
n Assessment Method
variables / CAM /
e r/t intervention
entia incidence a
rtality rate r/t ACS o
Investigating psychiatric
Investig. prescript.of
Investigation of
Investigating patient´
obal Detoriation
Study IV, Reducing Acute Confusional State in elderly patients with
hip fracture: a multi-factorial intervention study
Only minor differences in patient characteristics were found in study IV between the intervention group (IG) (n=131) and the control group (CG) (n=132) (Table 11 and 12). Thus, patients of the IG had a significantly poorer ability to walk. The number of prescribed drugs and their use did not differ between the groups, except for the use of diuretics which was significantly more common in the CG (47 % vs. 31 %). There
Table 11. Patient characteristics and medical data at baseline.
Gender Female/Male
92 (69.7)/40 (30.3)
93 (71.0)/38 (29.0)
Impaired hearing
Residence/admitted from
Institutional care
Able to walk alone
Walks with assistance
Comparisons are between Control group and Intervention group. Results are presented as number ofpatients (percentage) or as Mean (SD) or Median (q1-q3). Significances tested with Pearson Chi-squared test or Fisher's exact test, Student's T-test or Mann-Whitney U test. SPMSQ = ShortPortable Mental Status Questionnaire, and OBS scale = Organic Brain Syndrome Scale.
were statistically significant differences in levels of sodium (IG > CG) and potassium(IG <CG) in serum between the two groups. Furthermore the patients in the IG had asignificantly higher pulse rate at admission. However, all these differences were small and insignificant from a clinical standpoint.
Table 12. Biochemical and physiological variables at baseline.
141 (138.0 - 143.0)
142 (139.0 - 144.0)
Potassium (mmol/L)
Creatinine (micromol/L)
72.0 (57.0 - 94.0)
71.5 (55.6 - 87.3)
96.0 (94.8 - 98.0)
95.6 (94.0 - 98.0)
SAP (A&E) (mmHg)
Heart rate (A&E) (/min)
Body temperature (ear) (ºC)
Comparisons are between Control group and Intervention group. Results are presented as Mean (SD) or Median (q1-q3). Significances tested with Student's t-test or Mann-Whitney U test. Oxygen saturation (SpO2) (pulsoximetry),systolic arterial pressure (SAP), Ambulance (AMB), and Acute & Emergency department (A&E).
Of the 131 patients in the IG 29 (22 %) patients developed ACS, whereas of the 132 patients in the CG, 45 (34 %) developed ACS (p=0.031). Eight patients in the IG and 11 in the CG developed ACS already preoperatively (n.s.). Two of these patients had confusion only preoperatively (IG: 1, CG: 1). Altogether 74 (28 %) patients developedACS, a 64 % reduction compared to the control group.
All but thirteen of the patients suffering from ACS presented OBS max scores of seven points or more in one or several tests. Twelve patients (IG: 2, CG: 10) suffered onlyfrom nocturnal confusion and presented, when tested daytime, OBS scores of six points or below. One patient in every group presented OBS scores of six points in four variables. These patients had no knowledge whatsoever of being in a hospital at the time. One patient in each group developed ACS after being transported to a nearby hospital. According to the clinical evaluations of the nurse in charge and the nurse's records all patients with ACS fulfilled the criteria for ACS in relation to DSM-IV showing a Kappa-coefficient 0.87, (95% C I, 0.80 – 0.94).
Supplemental oxygen was administered prehospitally and preoperatively in 76 % and 95 % of the patients in the IG, respectively. The corresponding percentages in the CG was only 12 and 18 (p<0.0001). During surgery/anesthesia and in the recovery roomthe majority of patients in both groups were treated with oxygen. Postoperatively,however, in the orthopedic ward, the number of patients receiving supplemental
oxygen differed significantly (IG: 95 % vs. CG: 55 %) (p<0.0001). Consequently, wefound significantly higher median (q1-q3) levels of SpO2 in the IG compared to in the CG measured both prehospitally (97 (94.0 - 98.0) vs. 96 (94.0 - 98.0)), and during the hospital stay, including the second day after surgery (96.0 (94.0 - 97.0) vs. 94.0 (92.0 - 96.0), (p<0.0001)). The mean (SD) body temperature during anesthesia was significantly higher in the IG (37.1 (0.7) vs. 36.8 (0.6), indicating that the efforts to avoid hypothermia were successful. Moreover, the total volume of i.v. fluids (L) given was significantly higher in the IG than in the CG (median (q1-q3), 5 (3.5 - 5.5) vs. 4 (3.0-5.0) (p=0.001)).
The time lapsed between the arrival in the A&E, including X-ray examination, and the arrival in the orthopedic ward was significantly shorter in the IG group (median (q1-q3)2.7 (1.9 - 3.8) vs. 4.6 (3.3 - 5.7), p<0.0001). The fasting time was about the same inboth groups, whereas the waiting time for surgery did not decrease as could have been expected.
There were no significant differences between the two groups with regard to premedication, anesthesia method, anesthesia time, surgical method, the amount ofblood loss, units of blood given or pain assessed prehospitally, at arrival in the A&E, in the orthopedic ward, or in the operating department. More patients in the CG hadprophylactic antiemetics (ondanzetron or droperidol) (p<0.0001), while more patients in the IG were treated with opioids postoperatively in the recovery room (p=0.009).
The lowest heart-rate registered during anesthesia was significantly higher in the IG (p=0.043), while the lowest SAP monitored during anesthesia did not differ between the two groups.
Patients who developed ACS were significantly older (mean (SD) 85.3 (6.4) vs. 80.1(7.5), p<0.0001), more often male (41 % vs. 23 %), suffered more often from impaired hearing (76 % vs. 65 %), and lived more often in institutional care (18 % vs. 5 %). Patients with ACS were significantly more often classified as ASA 3 or 4 (53% vs.
32%), had a significantly lower median (q1-q3) SPMSQ score at admission to the A&E (9 (8.0 - 9.0) vs. 10 (9.0 - 10.0), a higher initial OBS score in an increased number of variables (1 (0 - 4.0) vs. 0 (0 - 1.0), and a significantly higher maximum OBS scorealso in an increased number of variables (4.5 (4.0 - 6.3) vs. 1.0 (0 - 2.0), p<0.0001).
Furthermore, they had a significantly higher number (> 3) of diagnosed diseases (28 % vs. 17 %), were more often affected by a neurological disease (Mb Parkinson, cerebral vascular lesion, or myasthenia gravis) (34 % vs. 21 %), and were more frequentlyprescribed drugs 4 (68 % vs. 51 %) of which the number of diuretics (53 % vs. 34 %), nitroglycerine (14 % vs. 4 %), and drugs with anticholinergic effect (53 % vs. 26 %) were significantly increased in the ACS group.
The patients with ACS compared to non-ACS had significantly lower levels of hemoglobin (mean (SD) 119.1 (19.8) vs. 123.8 (14.3)) and sodium (median (q1-q3) 140 (137.0-143.0) vs. 142 (139.3-143)), and increased (median (q1-q3) levels of potassium 4.0 (3.8-4.3) vs. 3.8 (3.6-4.1)), and creatinine 82.0 (62.5-106.0) vs. 69.5 (56.0-85.0)), at admission. They also had significantly lower median (q1-q3) SpO2 levels, both
preoperatively (95 (93.0 - 96.3) vs. 96 (94.0 - 97.0)), and postoperatively (94(92.5 - 96.0) vs. 96 (93.0 - 97.0)). The fasting time (h) was significantly longer in the ACS group (median (q1-q3), 15 (11.0 - 24.3) vs. 13 (9.0 - 20.0)). The median (q1-q3)volume of i.v. fluids (L) (1 (0.4 - 1.0) vs. 1 (0 - 1.0), p=0.018) and number of units ofblood transfused postoperatively (0 (0-2.0) vs. (0 (0-2.0), p=0.029) were significantly higher in the ACS group. Type of fracture and the surgical method did not differ significantly between the ACS and non-ACS group.
Of all studied patients 11 (4 %) died within 30 days postoperatively (mean: 12, range3 - 24 days). Five patients were 85 years, four patients had 3 diagnoses at admission, five were classified as ASA 2, four as ASA 3, and two as ASA 4. Ninepatients had cardiovascular diseases, four had cancer, two had chronic respiratorydisease, five had neurological disease, two had diabetes, and one patient suffered from renal insufficiency. Since a significant majority (7 out of 11) of the deceased patientsdeveloped ACS during the observation period, development of ACS seemed to beassociated with increased mortality. Moreover, the patients who developed ACS weresignificantly more often stricken with other complications, such as cardiac failure and myocardial infarction. However, the incidence of any other complication duringhospital stay nor death within 30 days of surgery did not differ significantly between the intervention group and the control group.
A number of intervention studies throughout the world concerning the acuteorthopedic treatment and care of elderly patients with hip fracture have beenintroduced and carried through. The majority of these studies performed in the hospital setting have shown positive effects concerning reducing incidence of ACS. The intervention program of the present thesis includes also the prehospital treatment and care.
The standard clinical practice of the care and treatment of elderly patients with hipfracture has too seldom taken advantage of new clinical knowledge. This also indicates that introducing new knowledge into clinical practice is a strenuous process in itself. The multi-factorial intervention program effectuated in the present study combined previous findings and our own recent results about common perioperative risk factors linked to the development of ACS. It would be reasonable to assume that reducing the incidence of ACS also would affect mortality and morbidity in this frail patient group. However, the design of the studies of the present thesis does not yet allow an evaluation concerning long term effects on morbidity and mortality.
The majority of elderly patients acutely admitted to hospital due to a fracture of the hip suffers from increased morbidity. The incidence of complications is high in this patient group. Consequently, it is of great importance that patients at risk of developingpostoperative complications such as ACS are identified and treated promptly in orderto prevent development complications. Basic factors related to the patient, such as high age, number of prescribed drugs, or functional status are not possible to have influence on. On the other hand factors such as oxygen saturation in blood, anemia, fluid balance, pain, or the length of fasting time are possible to affect already at an early stage.
The present thesis includes two studies intended to describe elderly patients with hipfracture and to identify some important aspects regarding risk factors for a poorer survival and a rehabilitation process being affected by ACS or other complications, as well as for a prolonged hospital stay. A third study, which was based on a literature review, evaluated the sensitivity and clinically applicability of a psychometric scale (the OBS scale) through investigating how other studies had used and compared it with of other known scales used to assess the varying signs of acute confusion inelderly geriatric patients. The results of these three studies together with a detailed registration of the logistics of hip fracture patients formed the basis of the fourth studywhich was aimed to find out if a prehospital and perioperative multi-factorial programcan reduce the incidence of ACS in elderly patients with hip fracture.
Methodological considerations
In study I and II a descriptive, cohort study was performed using data prospectivelyregistered in the RIKSHÖFT, and the Anesthesia register, and data retrospectivelycollected from medical records and nursing charts. In order to obtain a sufficient number of patients (n=428) for analyses of outcome such as in-hospital complications, registered in the Q-reg-99, the same three consecutive yearly periods of four monthseach were chosen. The four months in question, September until December, was the only time period when the Q-reg-99 was in use during these years. The majority of registrations were made by one single, experienced research nurse, (AH) who was also the coordinator of the RIKSHÖFT and followed the standardization of the RIKSHÖFTformulas which should be satisfactory in most of the cases. The ASA classification of the patients registered in the RIKSHÖFT was possible to double-check through the Anesthesia register.
The retrospective collection of data in medical records and nursing charts has limitations. The documents screened may be more or less incomplete which couldbring some uncertainties to the result. The documentation made by physicians in medical records might not always be totally satisfactory (93), and nurses´ documentation of mental status is seldom accurate (59, 188, 190). This implies that the number of patients suffering from ACS could have been higher than that found in therecords. It was not possible to control the number of patients suffering from ACS in the Q-reg-99 as "confusion" was not specified as a complication. Instead it was registered as "Other complication" together with e.g. anemia or obstipation.
Another limitation in study I and II was the use of variables with a high internal drop-out such as the SPMSQ and the SpO2 bringing some uncertainties to the result. On the other hand, the relatively high number of patients tested with the SPMSQ should beconsidered satisfactory with regard to reliability and responsiveness. The lacking SpO2values (n=90) monitored before the start of anesthesia were all except six valuesreplaced by SpO2 values registered in the A&E (n=44) or the lowest SpO2 values,registered during anesthesia (n=40). This might indicate that the actual SpO2 valuesregarding 84 patients, after 24 hours in a supine position, could have been even lower than those values replaced by us, and the figures should consequently be interpreted with caution.
A comparative and correlational design, i.e. to study relationships among variables as in study I and II, has often a week internal validity due to lack of control over the independent variable (250, 251). The effect on the outcome dependent variable fromthe different independent variables may not be predicted with certainty, and no causal relationship can be established. However, the results of the multiple logistic regression analyses were clinically consistent and comprehensible. Even if the risk analyses concerning outcome of ACS were partially based on data retrospectively collected from medical journals and nursing charts, and not regarded as satisfactory in relationto risk analyses, all the data collected in the RIKSHÖFT register concerning patient descriptives, dementia diagnosis, fracture type, number of prescribed drugs, and
SPMSQ score were collected prospectively. Registration in medical journals and nursing charts regarding laboratory values as hemoglobin or SpO2 was done during thepatients´ hospital visit and should therefore be regarded as being correct in the majority of cases.
During the three year periods (1999, 2000, and 2001) of inclusion of patients in study I and II some changes in clinical routines in the Orthopedic department could haveinfluenced the results. In 1998 and 1999 actions to improve the care had been taken inorder to reduce the number of pressure ulcers (100). A new waiting room for bedridden patients in the A&E, better mattresses in orthopedic beds, and increasedpain treatment were introduced. However, the new routines were already in use as the inclusion of patients in study I and II started and should not have influenced the result over time. The patients who were included in study I and II were all included according to the same criteria. No systematic drop-out was of hand. Consequently no biases with regard to history, maturation, or attrition are known.
In study IV a quasi-experimental, non-equivalent comparison group design with a treatment group and an untreated comparison group, with dependent pretest and posttest samples was used. This design is thought to be the most common of all quasi-experiments (219). The quasi-experimental design lacks the strength of a true experimental and randomized design when the sample in each group is selected at random. In this design (referred to as the gold standard for treatment outcomeresearch) any outcome differences that are observed between the groups at the end of the study are likely to be due to treatment and not to differences between the groupsthat existed before the start of the study (219). The quasi-experimental design includes at least two groups; one treatment group (IG) and one untreated comparison group (CG), getting the treatment as usual. In the quasi-experimental design it can not be assumed that the treatment group and the comparison group are equivalent at the outset, which could imply a selection bias and a threat to internal validity if any pre-existing differences are at hand (250). The strength of the quasi-experimental design depends strictly upon the similarity of the treatment group and the untreated group (219, 251). Through pretest gathered in both groups giving the similar results, the result of the posttest should confidently be accepted to be due to the experimentaltreatment (250).
In this study (IV) the treatment group (IG) was matched with the non-treatment group(CG) with regard to the following inclusion criteria: fracture of the hip, age 65 years, the same catchment area, and lucidity (SPMSQ 8 correct answers) on admission to hospital. The groups were comparable in most respects and with regard to gender, age, hearing and vision, smoking, pre-fracture living conditions, hip fracture type, ASA-classification, medical diagnoses and number of diagnoses, number of prescribed drugs, OBS scale score within four hours after admission, and the majority of biochemical and physiological variables at baseline. Moreover, no significant differences were found between the groups regarding waiting time for surgery, fasting time before surgery, anesthesia method and anesthesia time, type of surgery, amount
of blood loss, number of blood transfusions, any complications in hospital except for ACS, nor death within 30 days postoperatively.
The choice to use a quasi-experimental rather than a randomized design had several reasons. Firstly, due to the organization of the prehospital care including five ambulance stations within the catchment area, the researchers could not control and effectuate a proper randomization. Secondly, due to the organization of hospital beds at Lund University Hospital it was not possible to change the way the patients were located; primarily in one of the three orthopaedic wards, but in case of no beds available, the patients were transmitted to other departments such as acute surgery, medical, infectious disease or neurology. If a randomization had been conductedconfounding factors would probably have occurred due to that it would have beenimpossible to separate the patients of both groups from each other and the samepersonnel had to take care of patients of both the IG and the CG at the same time. The information sharing among patients in the same unit would have contaminated thetreatment conditions. These situations would have been impossible to control for and involve threats to internal validity (250). A randomized design including patients from each group in the same ward at the same time would also have been unethical with regard to the possibility for the patient in the CG to get the best treatment and care.
After the start of the intervention program there was a minor delay in implementation of the new program prehospitally since the organization of the prehospital care was outside the hospital and difficult for the researcher to reach fast enough. This wascompensated for by a prolongation of the study period by one week. Another effect ofthe difficulty to work with an organization outside the hospital was that only 58 % of the prehospital case report forms following each patient were handed in at the A&E.
Some of the lacking information regarding the early patient assessment was registeredin the ordinary prehospital journal, and thus the information was almost complete.
New guidelines were introduced by the Prehospital-Ambulance care (252) shortly after that the intervention was introduced. This evidently improved the compliance of theintervention program. Other changes in health care practice inside the hospital during the study period were not present to our knowledge.
There were only minor differences with regard to patient demographic characteristics between the IG and the CG. Thus patients in the IG had a significantly poorer ability to walk while the use of diuretics was significantly more common in the CG. Levels of sodium (IG>CG) and potassium (IG<CG) in serum differed significantly between the groups, and the patients in the IG had a significantly higher pulse rate at admission. From a clinical standpoint these differences are small, but could imply selection biases to the result and a threat to internal validity. In case of a skewed distribution of the sample it would imply a systematic bias and a threat also to external validity. In thisstudy no patient was excluded for physical reasons in order to minimize these threats and to optimize the demands of generalizability concerning elderly patients with hip fracture, age 65 years, lucid at admission to hospital, and with no history of cognitive impairment, psychosis or multitrauma. Only one patient denied participation in the study. This implies that the results could be generalized to other people, settings, time,
measures, and characteristics outside the study group referred to, and should be a strength to external validity (251). Eight patients primarily included in the study were later excluded because of not fulfilling the criteria for inclusion. This was due to lack of information in medical records regarding earlier diagnosis and treatment, or due tolack of the patient's or next of kin's report regarding history of psychosis treatment.
In study I and II all eligible patients except eight were included. The patients excluded had fractured abroad (n=5), had bilateral hip fractures (n=1), or were moribund or died before surgery (n=2). These patients did not differ with regard to age, gender, living conditions, number of prescribed drugs, ASA classification, length of hospital stay, or mortality compared to the patients included in the study.
All studies (n=30) found through literature search using the OBS scale were included in study III and presented in the result. No exclusion criterion was otherwise used. Themajority of studies had been carried through in a population of elderly patients (n=20),with hip fracture (n=11), dementia (n=7), or other diagnoses, such as neurological,medical or psychiatric (n=6), and with the focus on incidence of ACS, the clinical profile of psychiatric symptoms, evaluation of an intervention program, or comparison with other psychiatric scales.
With regard to a high percentage of patients and the consecutively way of inclusion in study I, II, and IV, and all studies included in study III, the studies in this thesis could be said to have fulfilled the demands of generalizability.
The instruments used in the studies were chosen with regard to the focus of the research; elderly patients with hip fracture, acute confusion (ACS), and psychometricproperties of the instrument (241, 242). In study I, II and IV the psychometric instrument for screening for lucidity used was the SPMSQ (101, 253). The SPMSQwas included in the RIKSHÖFT and the Q-reg99 project in the late 1990-ies (91). The construction of the RIKSHÖFT formulas have been validated several times (98), butlack the separate alternative of registration of ACS. The RIKSHÖFT was not developed especially for patients 65 years even if the majority of patients registeredare elderly. However, the SPMSQ was developed to offer a rapid screening forcognitive deficit in the community-dwelling elderly (254). The instrument has been extensively used as a screening test for lucidity or to measure cognitive function in elderly patients (81, 254), and with hip fracture (8, 189, 255). The SPMSQ has been tested in a number of studies showing adequate reliability and validity in clinical samples (202). However, the validity results in community samples have shown to belower, suggesting that the SPMSQ may not correctly classify elderly with mild levels of impairment (81). On the other hand, used as a screening test for cognitive impairment the SPMSQ has been evaluated as very good and as one of the best knownand easy to administer (196, 200). The inter-rater reliability test for the SPMSQ presented in study IV, showed a Kappa-coefficient (Linear Weighting) of 1.00 (95 % CI, 1.00 – 1.00), indicating a total agreement between the two researchers (238).
The OBS scale was developed especially for clinical evaluation of disturbances ofawareness and orientation together with other signs of confusion in elderly patients (205 - 207). The scale has been used in several Swedish studies with the aim, like in study IV, to detect and follow ACS. It has been claimed in the literature that psychometric properties of the OBS scale are unknown (201), and that the validity and inter-rater reliability have not been reported (196). These statements are not in accordance with the results of study III. The evaluation of the OBS scale in relation tothe SAC's eight criteria for psychometric instruments showed that the OBS scale fulfils most of the requirements for a valid instrument but needs to be further evaluated with regard to reliability (test-retest and internal consistency) and translation and adaptation to other languages. The construct of the OBS scale has been described in similar ways by two independent factor analyses (206 – 207, 210) and the strength andstability of the factor structure have been documented (208). In study IV the internal consistency of the OBS scale 1 as measured by Cronbach's alpha showed an overall reliability of 0.82 - 0.90 for the second to the sixth OBS test, indicating a satisfactory concordance (256). The initial OBS test (within four hours after admittance) showed a non-satisfactory value of 0.39. This could be interpreted as due to the fact that the test was made in a selected group of patients, just previously assessed as lucid and without any symptoms of ACS, a manifestation the OBS scale in fact is supposed to assess.
The inter-rater reliability test for the OBS scale showed a Kappa-coefficient (Linear Weighting) of 0.98 (95 % CI, 0.94 - 1.00) between the two researchers, indicating asatisfactory result (238).
For practical reasons it was not possible for only one of the researchers in study IV to accomplish all the patient ratings, a condition otherwise preferred. However, the high inter-reliability agreements between the two researchers may have minimized biases to the result. The use of the OBS scale was not possible to blind to the researchers which may imply a bias. On the other hand, the assessments with the OBS scale were madein relation to several score steps (4 steps), the continuing dialogue with the staff, and the confirmation of the diagnose according to the DSM-IV should have increased the trustworthiness of the assessments (52). Although it was not possible for the researchers to watch all the patients 24 hours per day, the information anddocumentation concerning nocturnal confusion given by the personnel, affected boththe control and the intervention group, a fact supporting the trustworthiness. Daily tests and assessments of the patients solely made by the two researchers consolidate the trustworthiness of the study. The achieved differences in effects e.g. in SpO2 andi.v. fluid given preoperatively would further confirm that there was a good adherence to the program by the personnel.
Due to a relatively small number of patients in the ASA 1 and 4 classes, the patients in study I, II and III were lumped into two categories: ASA 1 and 2, and ASA 3 and 4. This was done in order to increase statistical power in the analyses, and to minimize the risk of Type I error i.e. the risk of rejecting the null hypothesis when the null hypothesis is in fact true (238). In study II a reduced p-value (p<0.003) instead of p<0.05 was used due to multiple comparisons across six different fracture groups to control for the risk of mass significance, and to minimize the risk of Type I error
(239). However, in study II in three of the fracture groups analysed, the number of patients were rather small (n = 16, 20, and 32) and therefore the result of these analyses should be interpreted with caution. Another way to reduce the risk of Type I error in study I and II was by dichotomization of the independent variables in the multiple logistic regression analyses such as walking ability: able to walk alone vs. unable to walk alone, and thereby increasing the number of patients in each group. Therisk of multicollinearity in study I and II between dementia diagnosis and the SPMSQ score was reduced by not entering SPMSQ score in three of the multiple logistic regression analyses. In study IV a power analysis was made in order to reduce the riskof Type II error, i.e. the risk of not rejecting the null hypothesis when the null hypothesis in fact is false, equal to conclude that no relationship exists when there is a relationship. This was done by calculating the required sample size (238). A power of at least 80 % was required with a p-value <0.05, and 150 patients in each group wereneeded to detect a reduction in ACS of 50 % in the intervention group compared to the control group. Although the required number of patients in each group only reached131 and 132 respectively, the result ought to be sufficient, but should as in all statistical analyses be interpreted with caution. Even if the effect of a 64 % reduction of ACS as a result of the new evidence based program was satisfying, there is a chance that the precision of the effect shown could have been even better if the study samplehad been larger than that of this study. Thus, the risk of false conclusions andstatistical conclusion validity has been regarded in study I, II, and IV (251).
The findings of the studies
Risk factors for ACS
Multiple logistic regression analyses accomplished in study I and II identified several statistically significant risk factors for the development of postoperative ACS. In study I, based on patient's preoperative baseline characteristics, dementia diagnosis and dependency in living were identified as strong independent predictors for the development of postoperative ACS. These baseline factors were still strong as riskfactors in study II when analyzed together with factors from the perioperative period. Thus, out of baseline- and perioperative factors affecting outcome, low postoperativeoxygen saturation (<90 %), was identified as a strong independent risk factor for the development of postoperative ACS. A prolonged fasting time of 12 hours or more was identified as another risk factor for postoperative ACS, but did not show a p-value of significance (0.086).
These findings are illustrated by the fact that 25 % of the patients had a significant decrease in oxygen saturation during the time period between the visit at the A&E and the postoperative stay at the orthopedic ward, and that almost 20 % of the patients, monitored at arrival in the operating department before anesthesia started, had aoxygen saturation of less than 90 percent. Only one fourth of these patients had beentreated with oxygen preoperatively. This is quite remarkably since the majority of nurses and physicians working in acute settings should be well acquainted with the
fact that, soon after being bedridden, traumatized elderly patients run a high risk of developing clinically significant hypoxemia (135-137,144, 145, 150) due to an increased mismatching of ventilation to perfusion in the lungs and that this situation in most cases can be prevented by oxygen treatment (142, 143). In fact, the lack of oxygen supplementation may be one of the causes of the development of ACS (7, 64,144, 145, 150).
Prevalence of ACS
Of all patients included in study I and II (n=428) 52 % suffered from postoperative ACS. Seventy-six patients already showed signs of confusion preoperatively. Thesepatients were more often 85 years, had a dementia diagnosis, and/or a SPMSQ score less than eight correct answers, and dependency in living. According to the retrospective collection of data, as many as 43 % of the patients, not registered as being confused preoperatively, developed ACS after the operation. However, one thirdof the patients regarded as lucid at arrival to hospital by means of the SPMSQ (8correct answers), were affected by ACS postoperatively. The retrospective collection of data in medical journals and nursing charts concerning incidence of ACS are known to be biased and is likely to be underestimated, due to the low awareness of this condition in elderly patients by medical and nursing staff (26, 185, 188, 189, 234). Consequently, the real incidence of ACS in study I and II is probably higher than presented.
Although the sample in study IV only included patients who were assessed as lucid at admission to hospital and with no history of previous cognitive impairment or severe neuropsychiatric illness, the incidence of ACS was as high as 34 % in the control group, which received routine treatment and care. This rather high incidence of ACS could be a result of the daily and repeated use of the OBS scale, since standardizedassessments by means of a psychometric instrument as the OBS scale, should be moresensitive in detecting the varying and early signs of ACS. The longer the interval between the assessments, the more likely fluctuating periods of ACS would have been missed (53). In a study similar to ours, but randomized and including both lucid and not lucid patients and patients with higher age (70+ years), the OBS scale test was accomplished only once in every patient during the hospital stay (47). Thus, incidence of ACS (usual care group: 76 %, intervention group: 58 %) was mainly confirmed based on the nurses´ documentation of the clinical symptoms of the patients. Even if these assessments could have been adequately registered, one could call the result in question, according to previous studies of active case-findings strategy and repeated assessment procedures (53).
The increased attention and information which was also given to patients in the controlgroup of our study (IV) might have reduced the incidence of ACS (34 %) in that group. Nonetheless, 22 % of the patients included in the intervention group, receivingcare and treatment according to the new evidence-based program, developed ACS.
Previous studies have reported an incidence of ACS of 13 % - 44 % in similar
selections of patients with hip fracture, i.e. tested as cognitively intact at admission (7,8, 9, 10). However, one of these studies of an earlier date included halothane, ananesthetic not frequently used today (7). Neither had these studies the purpose of reducing the incidence of ACS, making the results not fully comparable to ours.
It was shown in study I and II, that confusion starting in the postoperative period was significantly associated with dementia diagnosis, SPMSQ<8 correct answers, four or more prescribed drugs, dependency in living, and being unable to walk alone; factors indicating that this group of elderly patients are being more or less frail and suffering from different serious concomitant diseases. In study IV, patients who developed ACS,compared to non-ACS patients, were significantly older (mean (years): 85 vs. 80), more often male (41 % vs. 23 %), suffered more often from impaired hearing, and were more often dependent in living. They also used prescribed drugs with anticholinergic properties more frequently, such as neuroleptics and drugs againstincontinence, i.e. drugs well known as risk factors for the development of ACS (7,228). Surprisingly enough, in study I and II, the incidence of ACS in patients belonging to ASA group 3+4 did not differ significantly from that of the patients in ASA group 1+2. In study IV, however, the patients who developed ACS were significantly more often classified as ASA 3 and 4 (53 %), proposing that they weregenerally sicker, compared with patients without ACS (32 %). This result could be due to the use of a prospective design in study IV with an increased control of inclusioncriteria, measurements and registrations. However, the proportion of patients classified as ASA 3 and 4 in the whole population studied was only 38 %. This proportion seemsrather small when compared with that reported from a similar prospective study ofelderly patients with hip fracture, lucid at admission, in which as many as 65 % were classified as ASA 3 and 4 (11). Unfortunately, other Swedish studies using the samecriteria for inclusion as ours, did not present any ASA categorization (7, 8, 10). In our first sample (Study I and II), in which also non-lucid patients were included, the proportion of ASA 3 and 4 patients was about 40 %. This figure is clearly lower compared to that presented in similar studies (49 % to 83 %) (110, 116, 117,173, 175).
The discrepancy noted could be due to different local traditions in using the ASA scoring system. In our settings the patients may have been judged as being healthier than they really were. This in turn suggests that the ASA classification system may betoo insensitive (112, 113). Consequently, there seems to be a need for a more relevantand comparable preoperative classification system for elderly patients, like patients with hip fracture, to facilitate the optimization of the care an early stage.
Patients in study IV who developed ACS had a significantly longer fasting time(median (hours): 15 vs. 13) than non-ACS patients. In study II a prolonged fasting time of 12 hours or more was identified as a significant predictor of being inflicted by in-hospital complications, and with death within four months, and it is also likely to be a predictor of developing ACS. The result suggests that a further increased fasting timeof 15 hours or more might have worsened the condition of this already frail patient group even more. A prolonged fasting time is very likely associated with inadequate fluid intake causing dehydration and serum electrolyte imbalance, aberrations shownto be significant predictors for ACS (163). Obviously, elderly hip fracture patients
should in general be considered medically less fit with a need for improved circulatorystabilisation before surgery (128).
In study II postoperative ACS was shown to be associated with a low postoperative oxygen saturation (SpO2<90 %), transfusion of one or more units of blood postoperatively, and a postoperative hemoglobin less than 100 g/L; all factors suggesting that patients suffered from more complicated fractures, had an increasedblood loss or severe anemia, a prolonged bedridden period, and did not receive any oxygen treatment at all, or had insufficient oxygen supplementation. Compared to non-ACS patients in study IV, patients suffering from ACS had significantly lower SpO2levels, both preoperatively and postoperatively, lower baseline levels of hemoglobin,and larger volumes of i.v. fluids and more units of blood transfused postoperatively.
This indicate that the patients suffering from ACS had probably been exposed to a substantial prolonged decline in tissue oxygen and hemoglobin, given repeated bloodtransfusions postoperatively, conditions that may well contribute to the developmentof ACS (64). Since a low hemoglobin level further reduces the oxygen transport capacity in patients with a decreased oxygen saturation it seems quite plausible that anemia would also increase the risk of developing ACS. Significantly higher volumesof i.v. fluids were given during the postoperative period to the patients in the control group and those who developed ACS. This may have caused a fluid excess in patients with latent heart failure and thus contributed to the increased number of heart complications among the control- and ACS patients (257).
Morbidity and mortality after ACS
Patients deceased within 4-months after surgery (Study I and II) suffered significantly more often from postoperative ACS compared to survivors (62.5 % vs. 39.4 %)(p=0.004). However, postoperative ACS was not tested in the multiple logistic regression analyze as a risk factor (independent variable) in relation to death within 4-months after surgery (dependent variable). The reason was that postoperative ACS in itself was looked upon as an outcome. Instead, the variable dementia diagnosis was used in the analysis as a probable risk factor to death within 4-months after surgery.
However, this was not shown to be the case. With an aftermath perspective it would have been of interest to have investigated if postoperative ACS was a significant predictor to death within 4-months after surgery. On the other hand, for such a purposea study with an entirely prospective design would probably be more valid.
The number of patients in study IV who died within 30 days of surgery was significantly higher in the patient group suffering from ACS (9.5 %) compared to in the non-ACS group (2.1 %). There was also a significantly higher incidence of thetotal number of in-hospital complications, as well as serious complications, such as cardiac failure and myocardial infarction, in the patient group who suffered from ACS compared with the non-ACS group. In the current literature ACS has been presented as independently associated with mortality during the hospital stay but not so at a 90-dayfollow-up (20). The evidence with regard to the extent that ACS make an independent
contribution to mortality is not consistent, at least not in the short- and medium-term outcome perspective (53). Lundström et al. (2005) studied a sample of general internal medicine patients, (70+years, lucid and not lucid), using a prospective multi-factorialintervention program (33). They showed a significant reduction in in-hospitalmortality in patients with ACS in the intervention group compared to the control group. However, in a sample of hip fracture patients (70+years, lucid and not lucid), now using a postoperative, randomized multi-factorial intervention program, the sameresearch group did not find any differences in neither in-hospital mortality, nor at the 4- and 12-months follow-ups between intervention and control samples (47).
Nonetheless, there are reasons to assume that a similar intervention in patients with hipfracture based on a multi-factorial program in the long term could reduce not only theincidence of ACS, but also the incidence of mortality and morbidity.
ACS assessment
The patients in our study who developed ACS after admission showed a significantly lower SPMSQ score as well as a higher initial OBS score in an increased number of variables compared to other patients. This result is in accordance with a recent study showing a higher OBS score on admission in lucid patients to be predictive of the development of ACS (10). Patients who developed ACS presented a significantlyhigher maximum OBS score in a higher number of variables, compared to non-ACSpatients. The majority of the patients diagnosed as having ACS were disoriented to time, place, to own person and current situation as well as knowledge regarding some general topics. Eight patients were agitated or paranoid and having hallucinations.
Patients were tested on a daily basis, in line with recommendations for active case findings (258), and with other studies using the OBS scale or scales in previous studiessuccessfully validated with the OBS scale, such as the SPMSQ, the MMSE, or the CAM (8 - 10, 12, 118, 202, 215, 216). By daily testing and by keeping focus on the patient, the researcher easily got a thorough picture of any fluctuations or changes in the patient's mental and physical condition. The patients in our study, who suffered nocturnal confusion or was transmitted to another nearby hospital before developing ACS, and not at that moment were tested by the researchers, were observed by theregistered nurses who registered the clinical symptoms in the nursing chart. Thecriteria for ACS based on the clinical symptoms were later fulfilled in relation to DSM-IV (52).
Reduction of ACS by a multi-factorial intervention program
The observation of an increased incidence of ACS in elderly patients with hip fracture was an important contributing reason for us to undertake preventive measures, formulated in the new evidence based program, against risk factors and other factors shown to be associated with the development of ACS, and to bring the personnel's attention to this sometimes life-threatening condition. The increased suffering for frail,
elderly patients and the consequences of ACS and other complications together with the hip fracture itself have motivated the introduction of a clinically adaptable program; a program not being too demanding or requiring too much efforts for thepersonnel in the different departments.
The medical profiles of the intervention and the control group were similar with only a few statistically significant differences between the two groups. The number of patients in need of assistance when walking was higher in the intervention group indicating a higher degree of disability. A more frequent use of diuretics and a lower heart-rate at admission as well as during anesthesia was found in the control group.
This finding might be ascribed a tendency towards but statistically not significant an increased use of beta-blockers, possibly indicating an increased number of patientssuffering from more serious cardiovascular diseases among control patients comparedto those of the intervention group. Furthermore, there were minor but statisticallysignificant differences in the serum electrolyte levels. The clinical relevance isquestionable and perhaps related to the more frequent use of diuretics. Considering these differences were only small it seems reasonable to assume that they did notaffect the outcome of the study.
After the implementation of the program, treatment with supplemental oxygen prehospitally and perioperatively increased significantly to reach 95 % of all patients, indicating a fairly good compliance to the program of the personnel involved. Consequently, we found significantly higher levels of SpO2 in the intervention group already in the ambulance, consistently lasting during the hospital stay until the second day after surgery. Avoiding arterial hypoxemia and increasing the oxygen delivery to the brain and other body tissues seems to be of great importance especially in elderly patients prone to be bedridden in an uncertain lapse of time (7, 35, 144, 145, 149, 150,226). The significantly lower levels in SpO2, pre- and postoperatively, seen in patients suffering from ACS support the hypothesis, that arterial hypoxemia disturbing theoxidative metabolism in the brain and its cholinergic system contributes to the development of ACS (35, 71).
The program was implemented after the study was finished and has since then beenimproved and further refined. The value has later been confirmed (259).
Clinical implications
Due to an increased risk of development of ACS in elderly patients with hip fracture early management should include standardized methods for assessment of mentalstatus, increased monitoring of physiological parameters, especially oxygen saturation,hemoglobin, dehydration and/or electrolyte balance, and temperature. Supplementaloxygen should be administered prehospitally and continuously until patient's SpO2 is95 % without supplemental oxygen. Early supplementation of blood loss to keep hemoglobin > 100 g/L, especially in patients suffering from more extensive fractures. Intravenous fluid supplementation and extra nutrition should be administered at an
early state, and delay in transfer logistics should be kept at a minimum. Adequate painrelief should be given early as well as intra- and postoperatively, but polypharmaciashould be avoided especially simultaneously giving sedatives, hypnotics and/or drugswith anticholinergic properties. Spinal anesthesia is recommended as first choice with 0.5 L saline-acetate administered before introduction. Hypotension should be avoided.
The present studies show:
¾ Dementia diagnosis, dependency in living, and low postoperative oxygen
saturation (<90 %) are independent risk factor (predictors) for the developmentof postoperative ACS in elderly patients with hip fracture.
¾ Postoperative ACS in elderly patients with hip fracture is significantly
associated with dementia diagnosis, SPMSQ<8 correct answers, four or more prescribed drugs, dependency in living, and inability to walk without assistance. All these factors in this group of elderly patients indicate that they are more or less frail and suffering from different concomitant diseases.
¾ The OBS Scale in many aspects satisfies the requirements of a valid clinical
instrument, but there is a need for further evaluation especially with regard toreliability such as test-retest reliability and intra-class correlations, as well as the translation and adaptation to other languages
¾ Hip fracture patients at risk of developing ACS could be identified at an early
stage by their baseline characteristics such as high age (85 years), impairmentin hearing, dependency in living, inability in walking without assistance, having one or several severe systemic diseases that limit their activity (ASA 3 and 4 classification), and being prescribed four or more drugs, especially drugs withanticholinergic properties, such as neuroleptics and drugs used against incontinence.
¾ Elderly patients with hip fracture presenting low arterial oxygen saturation
(SpO2<90 %) prehospitally or at admission to hospital, lower score on the SPMSQ test, higher score on the OBS scale, an increased fasting time (12hours), and in need of more than one unit of blood transfusions indicating severe anemia (Hb<100 g/L), could be at risk of developing ACS.
¾ The use of an evidence based, multi-factorial intervention program based on an
early started and intensified and supporting treatment, and implemented in the daily routines can reduce the incidence of ACS in elderly patients with hip fracture.
FUTURE RESEARCH
A selection of research areas that need to be further highlighted are as follow:
¾ Evaluation of staff-compliance with regard to an intervention program.
¾ Further validation of the OBS scale with other scales. ¾ The effects of perioperative hypotension with regard to ACS in frail elderly
¾ Development and validation of an instrument for risk-identification for ACS in
elderly patients.
¾ Five-years follow up concerning mortality in elderly hip fracture patients. Did
we reduce morbidity and mortality in a longer perspective by intervention against ACS.
Akut förvirringstillstånd hos äldre patienter med höftfraktur. Identifiering av
riskfaktorer och intervention utifrån ett prehospitalt och perioperativt
vårdprogram
Akuta förvirringstillstånd eller akut konfusion (Acute Confusional State, ACS) uppträder hos 14-63 % av äldre patienter som vårdas på sjukhus. Akut konfusion har samband med en ökad risk för komplikationer efter operationen, (postoperativt), längre och mer kostsamma vårdtider samt en ökad dödlighet. Äldre patienter med höftfraktur är särskilt benägna att utveckla akut förvirring under perioden efter operation. Detta hör till stor del samman med att vid en höftfraktur drabbas patienten av flera trauman samtidigt: själva olyckan, smärtan, att flyttas till sjukhus, undersökning, väntan på operation, bedövning och operation. Ett akut förvirringstillstånd i samband med höftkirurgi fördröjer eller minskar patientens möjlighet att återhämta sig och återvända till sitt hem eller tidigare boende.
Äldre som drabbas av höftfraktur är en av sjukvårdens mest resurskrävande patientkategorier. Varje år drabbas cirka 18 000 personer. Antalet höftfrakturer har nästan fördubblats för personer över 80 års ålder under de senaste tjugo åren. Genomtidig bedömning av den äldre patientens kognitiva/mentala tillstånd med hjälp av ett standardiserat instrument som är ett sorts frågeformulär, som är lätt att använda, skulle vårdpersonalen snabbt kunna identifiera förändringar i patientens tillstånd och sätta in riktad och ändamålsenlig behandling och omvårdnad. Härigenom skulle risken för allvarliga komplikationer och ett förlängt lidande för patienten kunna minskas.
Dessutom torde vårdtid och sjukvårdskostnader kunna reduceras.
Avhandlingens delarbeten I och II baseras på uppgifter registrerade i det nationella kvalitetsregistret RIKSHÖFT samt granskning av medicinska journaler och omvårdnadsjournaler. Totalt omfattar materialet 428 patienter med höftfraktur somvårdades under tidsperioden 1 september till 31 december under åren 1999, 2000 och 2001. Ur RIKSHÖFT inhämtades uppgifter om patienternas boendeform och gångförmåga före olyckan, mentalt status vid ankomst till sjukhus, frakturtyp, riskbedömning i samband med anestesi/bedövning, operationsmetod, komplikationer i samband med sjukhusvistelsen samt boendeform, gångförmåga och komplikationerefter vårdtiden upp till fyra månader. Uppgifter som hämtades ur journaler omfattade antalet läkemedel som patienten stod på, förekomst av demenssjukdom eller förvirring, blodprover samt mätning av syremättnad i blodet vid ankomst till sjukhus och under vårdtiden, smärtbehandling samt uppgifter i anslutning till operation och bedövning.
Delarbete III är en systematisk litteraturöversikt som värderar och beskriver OBS skalan som är ett testformulaär för bedömning av mentalt status/förvirring. OBS skalan används senare som testinstrument i delarbete IV.
I delarbete IV ingick patienter med höftfraktur som testades vid ankomst till sjukhus och bedömts som mentalt friska, under tidsperioden 1 april, 2003 till 5 april, 2004.
Data insamlades under två tidsperioder där den första tidsperioden utgjordekontrollperiod, som beskriver rutin förfarandet avseende omvårdnad och behandlingföre interventionen. Nästa tidsperiod utgjorde behandlingsperiod enligt nya rutiner, interventionen. Totalt ingick 263 patienter i studien varav 132 patienter i kontrollgruppen och 131 patienter i behandlingsgruppen. De nya rutinerna sominfördes omfattade syrgasbehandling, och vätsketillförsel som dropp redan i ambulans samt ökad kontroll och upprätthållande av normala värden för olika kroppsfunktionersom syremättnad i blod, blodvärde, blodtryck och temperatur. På akutmottagningeninnebar de nya riktlinjerna att patienten skulle smärtlindras direkt efter ankomst och därefter hållas smärtfri. Tidigare kunde patienterna få ligga och vänta på smärtstillande under varierande tidslängd. Vidare skulle tidsförloppet på akutmottagningen minskasgenom att patienten skulle röntgas så fort som möjligt och därefter transporteras direkt till vårdavdelningen utan att återvända till akutmottagningen som tidigare var brukligt. Nytt var också att samtliga patienter testades med OBS skalan i anslutning till ankomst till sjukhus samt därefter dagligen för att undersöka förekomst av konfusion. Målet var också att undvika att patienten behandlades med för mycket lugnande medel eller sömnmedel och andra läkemedel som kan orsaka förvirring. I anslutning till operation och bedövning gällde nya riktlinjer för smärtlindring i samband med överflyttning till operationsbordet, rekommendation om extra vätsketillförsel som dropp, ersättning av blodförlust samt att ryggbedövning skulle användas i första hand. Delvis nya postoperativa smärtbehandlingsrutiner infördes. All personal fortbildades och instruerades att vara uppmärksam på tecken på förvirring hos patienterna.
Delarbete I Syftet med detta delarbete var att beskriva äldre patienter med höftfraktur utifrån en speciell riskbedömning samt att identifiera riskfaktorer hos patienterna som fanns före och i samband med ankomst till sjukhus och som var signifikant (statistiskt säkerställt samband) kopplade till patientens återhämtning efter operation och upp till fyra månader. Resultatet visade att riskfaktorer för en sämre 4-månadersöverlevnad efter höftfraktur var manligt kön, ålder 85 år och över, mer komplicerad höftfraktur samt att bo i särskilt boende/institution och att ha komplicerande sjukdomar det vill säga att ha en högre risk vid bedövning/operation. Ökad dödlighet visade sig dessutom ha signifikant samband med demenssjukdom eller sämre resultat på det mentala testet, att stå på fyra eller fler läkemedel, lägre blodvärde vid ankomst, tecken på sämrenjurfunktion samt att ej kunna gå utan assistans. Det sammantagna resultatet visar att det är viktigt att direkt efter ankomst till sjukhus identifiera de äldre patienter med höftfraktur som har en högre risk för en sämre överlevnad samt risk för att utveckla komplikationer som akut förvirringstillstånd.
Delarbete II Syftet med detta delarbete var att identifiera riskfaktorer som uppträder före, under och efter operation hos äldre patienter med höftfraktur och som är signifikant kopplade till patientens återhämtning efter operation och upp till fyra månader. Resultatet visade att riskfaktorer för en sämre 4-månadersöverlevnad efter höftfraktur var fortfarande manligt kön, mer komplicerad höftfraktur och att bo i särskilt boende/institution, men också längre fastetid före operation (12 timmar eller mer) samt att vara i behov av och
därmed bli behandlad med flera blodtransfusioner. Ökad dödlighet hade dessutomsignifikant samband med att ha för låg syrgasmättnad i blodet efter operation. Resultatet visar att det är av stor vikt att optimera patientens syrgasmättnad och blodvärde samt att minska fastetid men också väntetid inför operation i syfte att minimera risken för ökade komplikationer och dödlighet.
Delarbete III Syftet med detta delarbete var att systematiskt granska OBS skalan utifrån åtta specifika kvalitetskriterier som används för utvärdering av bedömningsinstrument,samt att undersöka OBS skalans användbarhet i olika typer av kliniska sammanhang.
Resultatet visade att OBS skalan uppfyller de flesta av dessa kvalitetskriterier, t.ex. att skalan mäter vad den är avsedd för att mäta och att mätmetoden är tillförlitlig, skalan behöver dock testas ytterligare. OBS skalan visade sig tillräckligt känslig och kliniskt användbar för att upptäcka tidiga tecken på förvirring hos äldre personer.
Delarbete IV Syftet med detta delarbete var att undersöka om införandet av ett multifaktorielltvårdprogram omfattande behandling och vård i ambulans, före, under och efter operation och bedövning, kunde minska förekomsten av akut förvirringstillstånd hos äldre patienter med höftfraktur som var mentalt/kognitivt friska vid ankomst till sjukhus. Resultatet av studien visade att andelen patienter som drabbades av akut förvirringstillstånd minskade signifikant. I gruppen som vårdades enligt rutinerna före interventionen drabbades 45 av 132 patienter av ACS, medan 29 av 131 patienter drabbades i den grupp som fick vård och behandling enligt det nya vårdprogrammet.
Patienter som insjuknade i akut förvirringstillstånd, oavsett grupp, drabbades av signifikant fler allvarliga komplikationer som t.ex. hjärtinfarkt och hade också en signifikant högre dödlighet 30 dagar efter operation jämfört med de patienter som inte blev förvirrade. Resultatet av studien visar att införandet av ett multifaktoriellt vårdprogram omfattande tidigt insatt syrgasbehandling, vätskebehandling och blodersättning, adekvat och tidigt insatt behandling av smärta samt förbättrade rutiner för överflyttning av patienter mellan avdelningarna bidrog till att minska insjuknandet i akut förvirringstillstånd med 64 %.
This thesis for the doctoral degree was carried out at the Department ofAnesthesiology and Intensive care, Clinical Sciences, Lund University. I wish to express my sincere gratitude to all those who have contributed to this thesis:
All participants in the studies, the patients as well as the staff in the different facilities, for their kind and generous participation and co-operation, allowing me to conduct this thesis.
Dag Lundberg, my supervisor and mentor, who throughout the study has advised,supported and encouraged me with never ending energy, interest, knowledge and patience.
Sylvia Larsson, my co-supervisor, for friendship, engagement, support and constructive criticism during all these years.
Ami Hommel, my co-author and research colleague, for friendship, collaboration, andfor all stimulating and valuable discussions.
Lars Gustafson, my-co-author and supervisor in the psychogeriatric field, for professional guidance and stimulating discussions.
Edith Andersson, my co-author and co-supervisor in the psychometric domains, for constructive advice and valuable discussions.
Karl-Göran Thorngren, my co-author, for kindly putting the facilities of the Orthopedic Department at my disposal, thanks for your support during these years.
Ingalill Rahm Hallberg, for excellent guiding at seminars.
Per Nyberg, my supervisor in statistics, thank you for all invaluable help.
Margareta Bergman, my colleague and tutor, thank you for friendship, encouragement, and support throughout the years.
Bibbi Thomé, for help in discovering the "research domains".
Amir Baigi, for guidance in power calculation and other statistical problems.
Ulf Jakobsson, for further statistical advice.
My colleagues and friends at the Department of Health Sciences, Lund University for your interest, encouragement, support and friendship.
My colleagues and friends at the Department of Anesthesiology and Intensive Care, Lund University Hospital, for your interest, support and for taking part in the study.
My colleagues in the Prehospital care, Region Skåne, for your interest, support and for taking part in the study.
My colleagues at the Acute & Emergency unit, the Department of Orthopedics, and the X-ray-unit, Lund University Hospital, for your interest and for taking part in the study.
Håkan Mejstad and his colleagues at the IT-Services, Department of Health Sciences, Lund University, for invaluable help.
The staff at the Medical Faculty Library, Lund University, for excellent help and assistance.
Staff at the Department of Health Sciences, Lund University, especially ChristinaLinde, Anna Blomgren and Göran Jönsson, for invaluable help.
My colleagues in the Swedish Association of Nurse Anesthetist and Intensive Care Nurses, for friendship, collaboration, support and interest in my work.
My colleagues in the International Federation of Nurse Anesthetists, IFNA, for
friendship, collaboration, and interest in my research.
All my relatives and friends, for their interest in my work and their patience with me during the different phases of my research work.
Elin och Sven-Arne for all assistance throughout the years.
Cecilia Björkelund, for being my sister, and for all your wise and sensible support in different matters.
And last but not least, my family, my husband Tommy, for your love, being with me all the time with never-ending support and endurance, our sons Hampus and Christopher,for love, patience and support, and for being my reality, Linda and Henrik, Vilde andOscar for giving me joy at a far distance.
This thesis was supported by grants from The Cornell Foundation, Sweden, The HSF, Council for Medical Health Care Research in Southern Sweden, The Swedish Association of Nurse Anesthetist and Intensive Care Nurses, and The Medical Faculty, Department of Health Sciences, Lund University.
Tinetti MJ, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med 1988; 319:1701-1707.
Nyberg L, Gustafson Y, Berggren D, Brännström B, Bucht G. 1996. Falls leading to femoral neck fractures in lucid older people. J Am Geriatr Soc 44:156-160.
Gillespie LD, Gillespie WJ, Robertson MC, Lamb SE, Cumming RG, Rowe BH. Interventions for preventing fall in elderly people. Cochrane Database ofSystematic Reviews 2003 Issue 4. Art. No.: CD000340.
Lawlor DA, Patel R, Ebrahim S. Association between falls in elderly women and chronic diseases and drug use: cross sectional studie. BMJ 2003; 327:712-719.
Jagmin MG. Postoperative mental status in elderly hip surgery patients. Orthop Nurs 1998; Nov/Dec:32-42.
Inouye SK Predisposing and precipitating factors for delirium in hospitalized older patients. Dement Geriatr Cogn Disord 1999a; 10:393-400.
Berggren D, Gustafson Y, Eriksson B, Bucht G, Hansson LI, Reiz S, Winblad B. Postoperative Confusion after Anesthesia in Elderly Patients with Femoral Neck Fractures. Anesth Analg 1987; 66: 497-504.
Strömberg L, Ohle'n G, Nordin C, Lindgren U, Svensson O. Postoperativemental impairment in hip fracture patients. Acta Orthop Sacnd 1999; 70:250-255.
Marcantonio ER, Flacker JM, Wright RJ, Michaels M, Resnick NM. Delirium is independently associated with poor functional recovery after hip fracture. J AmGeriatr Soc 2000; 48:618-624.
Andersson E, Gustafson L, Hallberg I-R. Acute confusional state in elderlyorthopedic patients: Factors of importance for detection in nursing care. Int J Ger Psychiatry 2001; 16:7-17.
Zakriya KJ, Christmas C, Wenz JF, Franckowiak S, Anderson R, Sieber FE.
Preoperative factors associated with postoperative change in confusionassessment method score in hip fracture patients. Anesth Analg 2002;4:1628-1632.
Bitsch MS, Foss NB, Kristensen BB, Kehlet H. Acute cognitive dysfunction after hip fracture: frequency and risk factors in an optimized, multimodal, rehabilitation program. Acta Anaesthiol Scand 2006; 50:428-436.
Cole MG, Primeau F, McCusker J. Effectiveness of interventions to prevent delirium in hospitalized patients: A systematic review. Can Med Assoc J 1996;155:1263-1268.
Jin F, Chung F. Minimizing perioperative adverse events in the elderly. Br J Anaesth. 2001; 87:608-624.
Cole MG, Primeau F. Prognosis of delirium in elderly hospital patients. Can Med Assoc J 1993; 149:41-46.
Inouye SK. The dilemma of dilirium: Clinical and research controversies regarding diagnosis and evaluation of delirium in hospitalized elderly medicalpatients. Am J Med 1994; 97:278-288.
Murray AM, Levkoff SE, Wetle L, Cleary PD, Schor JD, Lipsitz LA, Rowe JW, Evans D. A. Acute delirium and functional decline in the hospitalized elderly patient. J Gerontol Med Sciences 1993; 48:M181-M186.
Williams MA, Campbell EB, Raynor WJ Jr, Mlynarczyk SM, Ward SE. Reducing acute confusional states in elderly patients with hip fractures. Res Nurs Health 1985b; 8:329-337.
Gustafson Y, Berggren D, Brännström B, Bucht G, Norberg A, Hansson L-I, Winblad B. Acute confusional states in elderly patients treated for femoral neck fractures. J Am Geriatr Soc 1988; 36:525-530.
Pompei P, Foreman M, Rudberg MA, Inouye SK, Braund V, Cassel C. Deliriumin hospitalized older persons: Outcomes and predictors. J Am Geriatr Soc 1994; 42:809-815.
Edlund A, Lundström M, Brännström B, Bucht G, Gustafson Y. Delirium before and after operation for femoral neck fracture. J Am Geriatr Soc 2001; 49:1335-1340.
Hommel A, Bjorkelund KB, Thorngren KG, Ulander K. Nutritional status among patients with hip fracture in relation to pressure ulcers. Clin Nutr 2007;26:589-596.
Brännström B, Gustafson Y, Norberg A, Winblad B. Problems of basic nursing care in acutely confused and non-confused hip-fracture patients. Scand J Caring Sci 1989; 3:27-34.
Brännström B, Gustafson Y, Norberg A, Winblad B. ADL performance and dependency on nursing care in patients with hip fractures and acute confusion in a task allocation care system. Scand J Caring Sci 1991; 5:3-11.
Dolan MM, Hawkes WG, Zimmerman SI, Morrison RS, Gruber-Baldini AL, Hebel JR, Magaziner J. Delirium on hospital admission in aged hip fracturepatients: prediction of mortality and 2-year functional outcomes. J Geront Med Sciences 2000; 55:M527-34.
Milisen K, Foreman MD, Godderis J, Abraham IL, Broos PL. Delirium in the hospitalized elderly. Geriatr Nurs 1998; 33: 417-437.
Milisen K, Foreman MD, Abraham IL, De Geest S, Godderis J, Vandermeulen E, Fischler B, Delooz HH, Siessens B, Bross PLO. A nurse-led interdisciplinary intervention program for delirium in elderly hip-fracture patients. J Am Geriatr Soc 2001; 49:523-32.
Francis J, Martin D, Kapoor WN. A prospective study of delirium in hospitalizedelderly. JAMA 1990; 263: 1097-1101.
Inouye SK, Rusing JT, Foreman MD, Palmer R, Pompei P. Does deliriumcontribute to poor hospital outcomes? A three-site epidemiologic study. J Gen Int Med 1998; 13: 234-242.
Levkoff SE, Evans DA, Liptzin B, Cleary PD, Lipsitz LA, Wetle TT, Reilly CH, Pilgrim DM, Shor J, Rowe J. Delirium. The occurence and persistence ofsymptoms among elderly hospitalized patients. Arch Internal Med 1992;152:334-40.
Magaziner J, Simonsick EM, Kashner TM, Hebel JR, Kenzora JE. Predictors offunctional recovery one year following hospital discharge for hip fracture: a prospective study. J Gerontol Med Science 1990; 13:234-242.
O'Keeffe S, Lavan J. The prognostic significance of delirium in older hospital patients. J Am Geriatr Society 1997; 45:174-178.
Lundström M, Edlund A, Karlsson S, Brännström B, Bucht G, Gustafson Y. Amultifactorial intervention program reduces the duration of delirium, length of hospitalization, and mortality in delirious patients. J Am Geriatr Soc 2005; 53:622-628.
Curyto KJ, Johnson J, Tenhave T, Mossey J, Knott K, Katz IR. Survival of hospitaized elderly patients with delirium. A prospective study. Am J Geriatr Psychiatry 2001; 9:141-7.
Gustafson Y, Brännström B, Berggren D, Ragnarsson I, Sigaard J, Bucht G, Reiz S, Norberg A, Winblad B. A geriatric-anestesiologic program to reduce acuteconfusional states in the elderly patients treated for femoral neck fractures. J Am Geriatr Society 1991a; 39:655-662.
Bowman AM. Sleep satisfaction, perceived pain and acute confusion in elderlyclients undergoing orthopaedic procedures J Adv Nurs 1997; 26:550-564.
Lundström M, Edlund A, Lundström G, Gustafson Y. Reorganization of nursing and medical care to reduce the incidence of postoperative delirium and improverehabilitation outcome in elderly patients treated for femoral neck fractures. Scand J Caring Sciences 1999; 13:193-200.
Brauer C, Morrison RS, Silberzweig SB, Siu AL. The cause of delirium in patients with hip fracture. Arch Intern Med 2000; 160:1856-1860.
Duppils GS, Wikblad K. Acute confusional states in patients undergoing hip surgery. A prospective observation study. Geront 2000; 46:36-43.
Marcantonio ER, Flacker JM, Wright RJ, Resnick NM. Reducing delirium after hip fracture: a randomized trial. J Am Geriatr Society 2001; 49:516-522.
Zakriya KJ, Christmas C, Wenz JF Sr, Franckowiak S, Anderson R, Sieber FE.
Preoperative factors associated with postoperative change in confusionassessment method score in hip fracture patients. Anesth Analg 2002; 6:1628-1632.
Gruber-Baldini AL, Zimmerman S, Morrison S, Grattan LM, Hebel JR, Dolan MM, Hawkes W, Magaziner J. Cognitive Impairment in hip fracture patients: Timing of detection and longitudinal follow-up. J Am Geriatr Soc 2003; 51:1227-1236.
Schurmans MJ, Duursma SA, Shortridge-Bagett LM. Elderly patients with hip fracture: The risk for delirium. Appl Nurs Res 2003; 16:75-84.
Edelstein DM, Aharonoff GB, Karp A, Kapla EL, Zuckerman JD, Koval KJ. Effect of postoperative delirium on outcome after hip fracture. Clin Orthop Relat Res 2004; 422:195-200.
Kagansky N, Rimon E, Naor S, Dvornikov E, Cojocaru L, Levy S. Lowincidence of delirium in very old patients after surgery for hip fractures. Am J Geriatr Psychiatry 2004; 12:306-314.
Olofsson B, Lundström M, Borssén B, Nyberg L, Gustafson Y. Delirium is associated with poor rehabilitation outcome in elderly patients treated for femoral neck fractures. Scand J Caring Sci 2005; 19;1-9.
Lundström M, Olofsson B, Stenwall M, Karlsson S, Nyberg L, Englund U,Borssén B, Svensson O, Gustafson Y. 2007. Postoperative delirium in old patients with hip fracture: a randomized intervention study. Aging Clin Exp Res 19:178-186.
Vidán M, Serra JA, Moreno C, Riquelme G, Ortiz J. Efficiacy of acomprehensive geriatric intervention in older patients hospitalized for hip fracture: A randomized, controlled trial. J Am Geriatr Soc 2005; 53:1476-1482.
American Psychiatric Association. Diagnostic and Statistical Manual of MentalDisorders. (1980). (Third edition (DSM III)) Washington DC. American Psychiatric Association.
Greiner FC. Das Traum und das fieberhafte Irreseyn. Brockhaus, Altenburg. 1812.
Gottlieb GI, Johnson J, Wanich C, Sullivan E. Delirium in the medically ill elderly: operationalizing the DSM-III criteria. Int Psychogeriatr 1991; 3:181-196.
American Psychiatric Association. Diagnostic and Statistical Manual of MentalDisorders. (1994). (Fourth edition (DSM IV)) Washington DC. American Psychiatric Association.
Rockwood K & Lindesay J: The concept of delirium: historical antecedents and present meanings. In: Rockwood K, Lindesay J, Macdonald A. (Eds). Deliriumin old age, 1st edition. Oxford, Oxford University Press, 2002, pp 1-8.
Lipowski ZJ. Transient cognitive disorder (delirium, acute confusional states) in elderly. Am J Psychiatry 1983; 140:1426-1436.
Lipowski ZJ. Update on delirium. Psychiatric Clin North Am 1992; 15:335-346.
Lipowski ZJ. Delirium: How its concept has developed. Int Psychogeriatr. 1991;3:115-120.
Foreman MD. Acute confusional states in hospitalized elderly: a research dilemma. Nurs Res 1985; 1: 34-38.
Billig N, Ahmed SW, Kenmore P, Amaral D, Shakhashiri MZ. Assessment of depression and cognitive impairment after hip surgery. J Am Geriatr Society 1986; 34:499-503.
Foreman MD. Acute confusion in the elderly: a research dilemma. Annu Rev Nurs Res 1993; 11:3-30.
Tune LE. Postoperative delirium. Int Psychogeriatr 1991: 3:325-332.
Granberg-Axell A, Bergbom I, Lundberg D. Clinical signs of ICU syndrome/delirum: an observational study. Intensive Crit Care Nurs 2001; 17:72-93.
Sandberg O, Gustafson Y, Brännström B, Bucht G. Clinical profile of delirum in older patients. J Am Geriatr Soc 1999; 47:1300-1306.
Lundström M, Edlund A, Bucht G, Karlsson S, Gustafson Y. Dementia after delirium in patients with femoral neck fractures. J Am Geriatr Soc 2003; 51:1002-6.
Marcantonio ER, Goldman L, Orav EJ, Cook EF, Lee TH. The association of intraoperative factors with the development of postoperative delirium. Am J Med 1998; 5:380-4.
Brauer C, Morrison S, Silberzweig SB, Siu AL. The cause of delirium in patients with hip fracture. Arch Int Med 2000; 160:1856-60.
Schor JD, Levkoff SE, Lipsitz LA, Reilly CH, Cleary PD, Rowe JW, Evans DA. Risk factors for delirium in hospitalized elderly. JAMA 1992; 267:827-31.
Inouye SK, Viscoli CM, Horwitz RI, Hurst LD, Tinetti ME. A predictive model
for delirium in hospitalized elderly medical patients based on admissioncharacteristics. Ann Intern Med 1993; 119:474-481.
Inouye SK, Charpentier PA. Precipitating factors for delirium in hospitalizedelderly persons. Predictive model and interrelationship with baseline vulnerability. JAMA 1996; 275:852-857.
Elie M, Cole MG, Primeau FJ, Bellavance F. Delirium risk factors in elderly hospitalized patients. J Gen Intern Med 1998; 13:204-212.
Lipowski ZJ. Delirium: Acute confusional states. Oxford, Oxford UniversityPress, 1990.
Gibson GE, Peterson C, Sansone J. Neurotransmittor and carbohydrate metabolism during aging and mild hypoxia. Neurobiol Aging 1981; 2:165-172.
Gustafson Y. Intervention mot postoperativa konfusionstillstånd sparar lidande och kostnader. I: Kirurgi och anestesi på den äldre patienten - framtidens vardagoch utmaning. Symposium, 1998.
Ancelin ML, De Roquefeul G, Ritchie K. Anesthesia and postoperative cognitive dysfunction in the elderly: a review of clinical and epidemiological observations. Rev Epidemiol Sante Publique 2000; 48:459-472.
McGoldrick K E. The Graying of America: Anesthetic Implications for Geriatric Outpatients. ASA Refresher Courses in Anesthesiology. Lippincott, Williams & Wilkins. 2005; 33:165-174.
Rasmussen LS, Larsen K, Houx P, Skovgaard LT, Hanning CD, Moller JT, and the ISPOCD group. The assessment of postoperative cognitive dysfunction. Acta Anaesthesiol Scand 2001; 45:275-289.
Monk TG, Weldon BC, Garvan CW, Dede DE, van der Aa MT, Heilman KM, Gravenstein JS. Predictors of cognitive dysfunction after major noncardiac surgery. Anesthesiology 2008; 108:18-30.
Keefover RW. Aging and cognition. Neurol Clin 1998; 16:635-648.
Riedel-Heller SG, Busse A, Aurich C, Matschinger H, Angermeyer MC.
Incidence of dementia according to DSM-III-R and ICD-10. Results of the Leipzig Longitudinal Study of the Aged (LEILA75+), Part 2. Br J Psychiatry.
2001; 179:255-260.
Crosby G, Culley DJ. Anesthesia, the aging brain, and the surgical patient. Can JAnesth 2003; 50:6:R1-R5.
Hanning CD. Postoperative cognitive dysfunction. Br J Anaesth 2005; 95:82-7.
McDowell I, Kristjansson E: Mental status testing, In: McDowell I, Newell C. (Eds). Measuring health. A guide to rating scales and questionnaires, 2nd edition. New York, Oxford University Press, 1996, pp 287-334.
Atkinson RL, Atkinson RC, Smith EE, Hilgard ER. Introduction to Psychology.
9th ed. Orlando, Fla, Harcourt Brace Jovanovich, Publishers, 1985.
SFR. Äldre och åldrande Ett nationellt forskningsprogram. Swedish Council for Social Research, Socialvetenskapliga Forskningsrådet, Stockholm, 1999, p8.
Victor C. What is old age? In: Redfern S and Ross F (Eds), Nursing in oldpeople, London, Churchill Livingstone, 2000, pp 3-17.
Balducci L. Geriatric oncology: challenges for the new century. Eur J Cancer. 2000; 36:176-82.
Andersson EM, Knutsson IK, Hallberg IR, Norberg A. The experience of beingconfused: a case study. A breakdown in communication between a confusedpatient and a nurse may have everything to do with the nurse's point of view.
Geriatr Nurs 1993; 14:242-247.
Andersson E, Hallberg I, Norberg A, Edberg A-K. The meaning of acuteconfusional state from the perspective of elderly patients. Int J Geriatr Psychiatr2002; 17:652-663.
Duppils GS, Wikblad K. Patient's experiences of being delirius. J Clin Nurs. 2007; 16:810-818.
Fagerberg I, Jönhagen M. Temporary confusion: a fearful experience. J Psychiatr Ment Health Nurs 2002; 9:339-346.
Rolfson D. The causes of delirium. In: Rockwood K, Lindesay J, Macdonald A. (Eds). Delirium in old age, 1st edition. Oxford, Oxford University Press, 2002, pp 101-122.
Thorngren KG, Hommel A, Norrman P O, Thorngren J, Wingstrand H.
Epidemiology of femoral neck fractures. Injury, Int J Care Injured 2002; 33:Suppl.3:1-7.
Oden A, Dawson A, Dere W, Johnell O, Jonsson B, Kanis JA. Lifetime risk of hip fractures is underestimated. Osteoporos Int 1998; 8:599-603.
Nordell E, Jarnlo G-B, Jetsén C, Nordström L, Thorngren KG. Accidental faals and related fractures in 65-74 years olds. A retrospective study of 332 patients. Acta Orthop Scand 2000; 71:175-179.
Kanis JA, Johnell O, Oden A, Jonsson B, De Laet C, Dawson A. Risk of hip fracture according to the World Health Organization criteria for osteopenia and osteoporosis. Bone 2000; 27:585-590.
Rogmark C, Sernbo I, Johnell O, Nilsson JA. Incidence of hip fractures in Malmö, Sweden, 1992-1995. A trend-break. Acta Orthop Scand 1999; 70:19-22.
Nymark T, Lauritsen JM, Ovesen O, Röck ND, Jeune B. Decreasing incidence ofhip fracture in the Funen County, Denmark. Acta Orthop 2006; 77:109-113.
Cooper C, Campion G, Melton LJ 3rd. Hip fractures in the elderly: a world-wideprojection. Osteoporos Int 1992; 2:285-289.
Thorngren K-G. Swedish National Hip Fracture Register, Yearbook. Annualreport for 2006. In Swedish. Rikshöft-SAHFE. Lund: Department of Orthopaedics, Lund University Hospital. 2007.
American Society of Anesthesiologists. New classification of physical status. Anesthesiology 1963; 24:11.
100. Hommel A, Ulander, K, Thorngren, K-G. Improvements in pain relief, handling
time and pressure ulcers through internal audits of hip fracture patients. Scand JCaring Sci 2003; 17:78-83.
101. Pfeiffer E. A short portable mental state questionnaire for the assessment of
organic brain deficit in elderly patients. J Am Geriatr Soc 1975; 23:433-441.
102. Hommel A. Improved safety and quality care for patients with a hip fracture.
Intervention audited by the National Quality Register RIKSHÖFT. Dissertation,Lund University, Lund, Sweden 2007.
103. Parker MJ, Currie C, Mountain JA, Thorngren K-G. Standardised audit of hip
fracture in Europe (SAHFE). Hip Int 1998; 8:10–15.
104. Schmidt AH, Asnis SE, Haidukewych G, Koval KJ Thorngren K-G. Femoral
neck fractures. Instructional Course Lecture 2005; 54:417-445.
105. Parker M, Johansen A. Hip fracture. BMJ 2006; 333:27-30.
106. Thorngren KG. Femoral neck fractures. In: Bulstrode C, Buckwalter J, Carr A,
Marsh L, Fairmank J, Wilson-MacDonald J, Bowden G. (Eds). Oxford Textbookof Orthopedics and Trauma. 1st edition. New York, Oxford University Press. 2002, Vol 3.
107. Cornwall R, Gilbert MS, Koval KJ, Strauss E, Siu AL. Functional outcomes and
mortality vary among different types of fractures: a function of patient characteristics. Clin Orthop Relat Res 2004; Aug:64-71.
108. Michel J-P, Klopfenstein C, Hoffmeyer P, Stern R, Grab B. Hip fracture surgery:
Is the pre-operative American Society of Anesthesiologists (ASA) score a predictor of functional outcome? Aging Clin Exp Res 2002; 14:389-394.
109. Wolters U, Wolf T, Stützer H, Schröder T. ASA classification and perioperative
variables as predictors of postoperative outcome. Br J Anaesth 1996; 77: 217-222.
110. Aharonoff GB, Koval KJ, Skovron ML, Zuckerman JD. Hip fractures in the
elderly: predictors of one year mortality. J Orthop Trauma 1997; 11:162-165.
111. Owens WD, Felts JA, Spitznage ELJr. ASA physical status classifications. A
study of inconsistency in ratings. Anesthesiology 1978; 49:239-43.
112. Ranta S, Hynynen M, Tammisto T. A survey of the ASA physical status
classification: significant variation in allocation among Finnishanaesthesiologists. Acta Anaesthesiol Scand. 1997; 41: 629-632.
113. Aronson WL, McAuliffe MS, Miller K. Variability in the American society of
anesthesiologists physical status classification scale. AANA J 2003; 71:265-274.
114. Karen Z, Nagelhout J. Nurse Anesthesia, 3rd Edition. St. Louis, Elsevier
Saunders, 2005/2007.
115. Parker MJ, Handoll HHG, Griffiths R. Anaesthesia for hip fracture surgery in
adults. The Cochrane Database of Systematic Reviews 2004, Issue 4. Art. No.: CD000521.pub2.
116. Koval KJ, Aharonoff GB, Rosenberg AD, Bernstein RL, Zuckerman JD.
Functional outcome after hip fracture. Clin Orthop Relat Res 1998; 348:37-41.
117. Gilbert TB, Hawkes WG, Hebel R, et al. Spinal anesthesia versus general
anesthesia for hip fracture repair: a longitudinal observation of 741 elderlypatients during 2-year follow-up. Am J Orthop 2000; 29:25-35.
118. Folstein MF, Folstein SE, McHugh PR. 'Mini-mental state': a practical method
for grading the cognitive state of patients for the clinician. J Psychiatry Res1975; 12:189-198.
119. Papaioannou A, Fraidakis O, Michaloudis D, Balalis C, Askiopoulou H. The
impact of the type of anaesthesia on cognitive status and delirium during the first postoperative dadys in elderly patients. Eur J Anaesthesiol 2005; 22:492-499.
120. Lyons AR. Clinical outcome and treatment of hip fractures. Am J Med. 1997;
121. Hamlet WP, Lieberman JR. Freedman EL, Dorey FJ, Fletcher A, Johnson EE.
Influence of health status and the timing of surgery on mortality in hip fracture patients. Am J Orthop 1997; 26:621-627.
122. Edlund A, Lundström M, Brännström B, Bucht G, Gustafson Y. Clinical Profile
of Delirium in Patients Treated for Femoral Neck Fractures. Dement Geriatr Cogn Disord 1999; 10:325-329.
123. Orosz GM, Hannan EL, Magaziner J, Koval K, Gilbert M, Aufses A,Straus E,
Vespe E. Fracture in the older patient: reasons for delay in hospitalization and timing of surgical repair. J Am Geriatr Soc 2002; 50:1336-1340.
124. Hefley FGJr, Nelson CL, Puskarich-May CL. Effect of delayed admission to the
hospital on the preoperative prevalence of the deep-vein thrombosis associated with fractures about the hip. J Bone Joint Surg Am 1996; 78: 581-583.
125. Rogers FB, Shackford SR, Keller MS. Early fixation reduces morbidity and
mortality in elderly patients with hip fractures from low-impact falls. J Trauma 1995; 39: 261-265.
126. Thomas S, Ord J, Pailthorpe C. Study of waiting time for surgery in elderly
patients with hip fracture and subsequent in-patient hospital stay. Ann R Surg Engl 2001; 83:37-39.
127. Zuckermann JD, Skovron ML, Koval KJ, Aharonoff G, Frankel VH.
Postoperative complications and mortality associated with operative delay in older patients who have a fracture of the hip. J Bone Joint Surg Am 1995;77:1551-1556.
128. Bottle A, Aylin P. Mortality associated with delay in operation after hip fracture:
observational study. BMJ 2006; 332:947-951.
129. Grimes JP, Gregory PM, Noveck H, Butler MS, Carson JL. The effets of time-to-
surgery on mortality and morbidity in patients following hip fracture. Am J Med. 2002; 112:702-709.
130. Orosz GM, Magaziner J, Hannan EL, Morrison RS, Koval K, Gilbert M,
McLaughlin M, Halm EA, Wang JJ, Litke A, Silberzweig SB, Siu AL. Association of timing of surgery for hip fracture and patient outcomes. JAMA2004; 291:1738-1743.
131. Williams A, Jester R. Delayed surgical fixation of fractured hips in older people:
impact on mortality. J Adv Nurs 2005; 52:63-69.
132. Moran CG, Wenn RT, Sikand M, Taylor AM. Early mortality after hip fracture:
is delay before surgery important? J Bone Joint Surg Am 2005: 87: 483-489.
133. Morrison RS, Siu AL. A comparison of pain and its treatment dementia and
cognitively intact patients with hip fracture. J Pain Sympton Manage 2000; 19: 240-248.
134. Verrier RL, Mittelman MA. Cardiovascular consequences of anger and other
stress states. Baillieres Clin Neurol. 1997; 6: 245-259.
135. Warner DO. Preventing postoperative pulmonary complications: the role of the
anesthesiologist. Anesthesiology 2000; 92:1467-1472.
136. Hedenstierna G, Edmark L. The effects of anesthesia and muscle paralysis on the
respiratory system. Intensive Care Med 2005; 31:1327-1335.
137. Kalkman CJ, Visser K, Moen J, Bronsel GJ, Grobbee DE, Moons KGE.
Preoperative prediction of severe postoperative pain. Pain 2003; 105:415-423.
138. Morrison RS, Magaziner MG, Gilbert M, Koval KJ, McLaughlin MA, Orosz G,
Strauss E, Siu AL. Relationship between pain and opioids analgesics on thedevelopment of delirium following hip fracture. J Gerontol A Biol Sci Med Sci2003; 1:76-81.
139. Lynch EP, Lazor MA, Gellis JE, Orav J, Goldman L, Marcantonio ER. The
impact of postoperative pain on the developement of postoperative delirium.
Anesth Analg 1998; 86:781-785.
140. Hallström I, Elander G, Rooke L. Pain and nutrition as experienced by patients
with hip fracture. J Clin Nurs 2000; 9:639-646.
141. Herr K, Titler MG, Schilling ML, Marsch JL, Xie X, Ardery G, Clarke WR,
Everett LQ. Evidence-based assessment of acute pain in older adults. Currentnursing practices and perceived barriers. Clin J Pain 2004; 5:331-340.
142. Haljamae H, Stefansson T, Wickstrom I. Preanesthetic evaluation of the female
geriatric patient with hip fracture. Acta Anaesthesiol Scand 1982; 26: 393-402.
143. Lynne-Davies P. Influence of age on the respiratory system. Geriatrics 1977;
144. Krasheninnikoff M, Ellitsgaard N, Rude C, Moller JT. Hypoxaemia after
osteocynthesis of hip fractures. Int Orthop 1993; 17:27-29.
145. Clayer M, Bruckner J. Occult hypoxia after femoral neck fracture and elective
hip surgery. Clin Orthop Relat Res 2000; 370: 265-271.
146. Gustafson Y, Brännström B, Norberg A, Bucht G, Winblad B. Underdiagnosis
and poor documentation of acute confusional states in elderly hip fracturepatients. J Am Geriatr Soc 1991b; 39:760-5.
147. Pedersen T, Eliasen K, Henriksen E. A prospective study of risk factors and
cardiopulmonary complications associated with anaesthesia and surgey: risk indicators of cardiopulmonary morbitiy. Acta Anaesth Scand 1990; 34:144 155.
148. Moller JT, Rasmussen LS, Houx P, Rasmussen H, Canet J, Rabbitt P, Jolles J,
Larsen K, Hanning CD, Langeron O, Johnson T, Lauven PM, Kristensen PA, Biedler A, Van Beem H, Fraidakis O, Silverstein JH, Beneken JEW, Gravenstein JS. Long-term postoperative cognitive dysfunction in the elderly: ISPOCD1 study. Lancet 1998; 21:857-861.
149. Kehlet H, Rosenberg J. Late post-operative hypoxaemia and organ dysfunction.
Eur J Anaesthesiol Suppl 1995; 10:31-34.
150. Hole A, Terjesen T, Breivik H. Epidural versus general anaesthesia for total hip
arthroplasty in elderly patients. Acta Anaesthesiol Scand 1980; 24: 279-287.
151. Izaks GJ, Westendorp RGJ, Knook DL. The definition of anemia in older
persons. JAMA 1999; 18: 1414-1417.
152. Gruson KI, Aharonoff GB, Egol KA, Zuckerman JD, Koval KJ. The relationship
between admission hemoglobin level and outcome after hip fracture. J Orthop Trauma 2002; 1:39-44.
153. Halm EA, Wang JJ, Boockvar K, Penrod J, Silberzweig SB, Magaziner J, Koval
KJ, Siu AL. The effect of perioperative anemia on clinical and functional outcomes in patients with hip fracture. J Orthop Trauma 2004; 18:369-374.
154. Shander A, Knight K, Thurer R, Adamson J, Spence R. Prevalence and outcomes
of anemia in surgery: A systematic review of the literature. Am J Med 2004; 5, Suppl.7A: 58S-69S.
155. Halm EA, Wang JJ, Boockvar K, Penrod J, Silberzweig SB, Magaziner J, Koval
KJ, Siu AL. Effects of blood transfusion on clinical and functional outcomes in patients with hip fracture. Transfusion 2003; 43:1358-1365.
156. Mukand JA, Cai C, Zielinski A, Danish M, Berman J. The effects of dehydration
on rehabilitation outcomes of elderly orthopedic patients. Arch Phys MedRehabil 2003; 1:58-61.
157. Odumala AO, Ayekoloye CI, Packer G. Predictors of excessive blood loss during
operative treatment of hip fractures. J R Coll Surg Edinb 2002; 3:552-556.
158. Wu W-C, Schifftner TL, Henderson WG, Eaton CB, Poses RM, Uttley G,
Sharma SC, Vezeridis M, Khuri SF, Friedmann PD. Preoperative hematocrit levels and postoperative outcomes in older patients undergoing noncardiacsurgery. JAMA. 2007; 297:2481-2488.
159. Lawrence VA, Silverstein JH, Cornell JE, Pederson T, Noveck H, Carson JL.
Higher Hb level is associated with better functional recovery after hip fracture repair. Transfusion 2003; 43: 1717-1722.
160. Muravchick S. Anesthesia for the elderly. In: Miller RD (Edit). Anesthesia. New
York, Churchill Livingstone, 1990, pp 1969-1983.
161. Paulson OB, Strangaard S, Edvinsson L. Cerebral autoregulation. Cerebrovasc
Brain Metab Rev 1990; 2:161-192.
162. Lewis JR, Hassan SKZ, Wenn RT, Moran CG. Mortality and serum urea and
electrolytes on admission for hip fracture patients. Injury 2006; 37:698-704.
163. Mentes J, Culp K, Maas M, Rantz M. Acute confusion indicators: risk factors
and prevalence using MDS data. Res Nurs Health 1999; 2:95-105.
164. Eneroth M, Olsson U-B, Thorngren KG. Insufficient fluid and energy intake in
hospitalised patients with hip fracture. A prospective randomised study of 80 patients. Clin Nutr 2005; 24:297-303.
165. Koval KJ, Maurer SG, Sue ET Aharonoff GB, Zuckerman JD. The effects of
nutritional status on outcome after hip fracture. J Orthop Trauma 1999; 3:164-169.
166. Avenell A, Handoll HH. A systematic review of protein and energy
supplementation for hip fracture aftercare in older people. Eur J Clin Nutr 2003; 57:895-903.
167. Burns A, Gallagley A, Byrne J. Delirium. J Neurol Neurosurg Psychiatry 2004;
168. Tinetti ME, Baker DI, Garrett PA, Gottshalk M, Koch ML, Horwitz RI. Yale
FICSIT: risk factor abatement strategy for fall prevention. J Am Geriatr Soc 1993; 3:315-320.
169. Mintzer J, Burns A. Anticholinergic side-effects of drugs in elderly people. J R
Soc Med 2000; 93:457-462.
170. Magaziner J, Hawkes W, Hebel JR, et al. Recovery from hip fracture in eight
areas of function. J Gerontol A Biol Sci Med Sci 2000; 55:M498-M507.
171. Hannan EL, Magaziner J, Wang JJ, Eastwood EA, Silberzweig SB, Gilbert M,
Morrison RS, McLaughlin MA, Orosz GM, Siu, AL. Mortality and locomotion 6 months after hospitalization for hip fracture. JAMA 2001; 285:2736-2742.
172. Haentjens P, Autier Ph, Barette M, Boonen S. Predictors of functional outcome
following intracapsular hip fracture in elderly women. A one-year prospectivecohort study. Injury 2005; 36:842-850.
173. Heikkinen T, Willig R, Hänninen A, et al. Hip fractures in Finland – a
comparison of patients characteristics and outcomes in six hospitals. Scand J Surg 2004; 93:234-240.
174. Goldacre MJ, Roberts SE, Yeats D. Mortality after admission to hospital with
fractured neck of femur: a database study. BMJ 2002; 325:868-869.
175. Foss NB, Kehlet H. Mortality analysis in hip fracture patients: implications for
design of future outcome trials. Br J Anaesth 2005; 94:24-29.
176. Rosell PAE, Parker MJ. Functional outcome after hip fracture. A 1-year
prospective outcome study of 275 patients. Injury 2003; 34:529-532.
177. Heikkinen T, Jalovaara P. Four or twlvw months´follow-up in the evaluation of
functional outcome after hip fracture surgery. Scand J Surg 2005; 94:59-66.
178. Inouye SK, Bogardus ST, Charpentier PA, Leo-Summers L, Acampora D,
Holford TR, Cooney LM. A multicomponent intervention to prevent delirium in hospitalized older patients. The New England J Med 1999b; 340:669-676.
179. Foreman MD, Wakefield B, Culp K, Milisen K. Delirium in Elderly Patients: An
overview of the state of the science. J Gerontol Nurs 2001; 17:12-20.
180. Britton A, Rusell R. Multidisciplinary team interventions delirium in patients
with chronic cognitive impairment. [Update of Cochrane Database Syst Rev. 2001;(1):CD000395; PMID: 11279689]. Cochrane Database of SystematicReviews,2) CD000395.
181. Milisen K, Lemiengre J, Braes T, Foreman MD. Multicomponent intervention
strategies for managing delirium in hospitalized older people: sytematic review. J Adv Nurs 2005; 52:79-90.
182. Williams MA, Campbell EB, Raynor WJ Jr, Musholt MA, Mlynarczyk SM,
Crane LF. Predictors of acute confusional states in hospitalized elderly patients. Res Nurs Health 1985a; 8:31-40.
183. Phy MP, Vaness DJ, Melton LJ.Effect of a hospitalist model on elderly patients
with hip fracture. Arch Int Med 2005; 165:796-801.
184. Egbert AM, Parks LH, Short LM, Burnett ML. Randomized trial of postoperative
patient-controlled analgesia vs intramuscular narcotics in frail elderly men. Arch Intern Med 1990; 150:1897-1903.
185. Rockwood K Educational interventions in delirium. Dement Geriatr Cogn Disord
1999; 10:426-429.
186. Cole MG. Delirium: effectiveness of systematic interventions. Demen Geriatr
Cogn Disord 1998; 10:406-411.
187. Siddiqi N, Stockdale R, Britton AM, Holmes J. Interventions for prevention
delirium in hospitalised patients. Cochrane Database of Systematic Reviews 2007, Issue 2. Art. No.:CD005563.
188. Souder E, O'Sullivan PS. Nursing documentation versus standardized assessment
of cognitive status in hospitalized medical patients. Appl Nurs Res 2000; 13:29-36.
189. Söderqvist A, Strömberg L, Ponzer S, Tidermark J. Documenting the cognitive
status of hip fracture patients using the Short Portable Mental Status Questionnaire. J Clin Nurse 2006; 3:308-314.
190. Milisen K. An intervention study for delirium in elderly hip fracture patients.
Dissertation, Katholic University, Leuven, Belgium,1999.
191. Levkoff SE, Evans DA, Liptzin B, Cleary PD, Lipsitz LA, Wetle TT, Reilly CH,
Pilgrim DM, Shor J, Rowe J. Delirium. The occurence and persistence ofsymptoms among elderly hospitalized patients. Arch Int Med 1992; 152:334-340.
192. Johnson J. Identifying and recognizing delirium. Dement Geriatr Cogn Disord
1999; 10:353-358.
193. Inouye SK, Foreman MD, Mion LC, Cooney LMJr. Nurses´recognition of
delirium and it´s symptoms: comparison of nurse researcher ratings. Arch Int Med 2001; 161:2467-2473.
194. Meagher DJ. Delirium: optimising management. BMJ 2001; 322:144-149.
195. Foreman MD. 1987. Reliability and validity of mental status questionnaires in
elderly hospitalized patients. Nurs Res 36:216-220.
196. Robertsson B. The instrumentation of delirium. In: Rockwood K, Lindesay J,
Macdonald A. (Eds). Delirium in old age, 1st edition. Oxford, Oxford University Press, 2002, pp 9-26.
197. Tombbaugh TN, McIntyre NJ. The Mini-Mental State Examination: a
comprehensive review. J Am Geriatr Soc 1992; 40:922-935.
198. Strömberg L, Lindgren U, Nordin C, Öhle'n G, Svensson O. The appearance and
disappearance of cognitive impairment in elderly patients during treatment for hip fracture. Scand J Caring Sci 1997; 1:167-175.
199. Field SJ, Jackson HJ, Hassett AM, Pattison P. Ability of the mini-mental state
examination to discriminate diagnostic entities in a psychogeriatric population. Int J Geriatr Psychiatry 1995; 10:47-53.
200. Fitten LJ, Lusky R, Hamann C. Assessing treatment decision-making in elderly
nursing home residents. J Am Geriatr Soc 1990; 38:1097-1104.
201. Smith MJ, Breitbart WS, Platt MM. A critique of instruments and methods to
detect, diagnose, and rate delirium. J Pain Symptom Manage. 1995; 10:35-77.
202. Erkinjuntti T, Sulkava R, Wikström J, Autio L. Short portable mental status
questionnaire as a screening test for dementia and delirium among the elderly. JAm Geriatr Soc 1987; 35:412-16.
203. Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI.
Clarifying confusion: the confusion assessment method. A new method fordetection of delirium. Ann Intern Med 1990; 113:941-948.
204. Rockwood K, Cosway S, Stolee P, Kydd D, Carver D, Jarrett P, O´Brien B.
Increasing the recognition of delirium in elderly patients. JAGS 1994; 42:252-256.
205. Breitbart W, Rosenfeld B, Roth A, Smith MJ, Cohen K, Passik S. The Memorial
Delirium Assessment Scale. J Pain Symptom Manage 1998; 13:128-137.
206. Gustafson L, Westling B, Lindgren M. The OBS-scale.A new rating scale for
evaluation of confusional states and other organic brain syndromes. In 2ndInternational Congress on Psychogeriatric Medicine Abstract No. 128. Umeå, Sweden, 1985.
207. Gustafson L, Lindgren M, Westling B. 1995. The OBS scale. A factor analysis
approach to evaluation of confusional states and other Organic Brain Syndromes.
Departments of Psychogeriatrics, Lund University.
http://www.psykiatr.lu.se/pg/OBSscale.pdf
208. Jensen E, Dehlin O, Gustafson L. A comparison between three psychogeriatric
rating scales. Int J Geriatr Psychiatry 1993; 8:215-229.
209. Edberg A-K, Norberg A, Hallberg IR. Mood and general behavior of patients
with severe dementia during one year of supervised, individualized planned care and systematic clinical supervision. Comparison with a similar group. Aging1999; 11:395-403.
210. Hallberg IR, Norberg A, Erikson S. 1990. Functional impairment and
behavioural disturbances in vocally disruptive patients in psychogeriatric wards compared with controls. Int J Geriatr Psychiatry 5:53-61.
211. Sandberg O, Gustafson Y, Brännström B, Bucht G. Prevalence of dementia,
delirium and psychiatric symptoms in various care settings for the elderly. ScandJ Soc Med 1998; 26:1:56-62.
212. Elmståhl S, Annerstedt L, Åhlund O. How should a group living unit for
demented elderly be designed to decrease psychiatric symptoms? Alzheimer Dis Assoc Disord 1997; 11:47-52.
213. Gustafson Y, Olsson T, Eriksson S, Asplund K, Bucht G. Acute confusional
states (delirium) in stroke patients. Cerebrovasc Dis 1991c; 1:257 265.
214. Gustafson Y, Olsson T, Asplund K, Hägg E. Acute Confusional State (Delirium)
Soon after Stroke is Associated with Hypercortisolism. Cerebrovasc Dis 1993;3:33-38.
215. Sandberg O, Franklin KA, Bucht G, Gustafson Y. Sleep apnea, delirium,
depressed mood, cognition, and ADL ability after stroke. J Am Geriatr Soc 2001;49:391-397.
216. Eriksson M, Samuelsson E, Gustafson Y, Åberg T, Engström KG. Delirium after
coronary bypass surgery evaluated by the organic brain syndrome protocol.
Scand Cardiovasc J 2002; 36:250-255.
217. Bitsch M, Foss N, Kristensen B, Kehlet H. Pathogenesis of and management
strategies for postoperative delirium after hip fracture: a review. Acta OrthopScand 2004; 75;378-389.
218. Scientific Advisory Committee of the Medical Outcomes Trust (SAC). Assessing
health status and quality-of-life instruments: attributes and review criteria. Qual Life Res 2002; 11:193-205.
219. Shaddish W R, Cook T D, Campbell D T. (Eds) Experimental and quasi-
experimental designs for generalized causal inference. Boston, Houghton Mifflin, 2002.
220. Lohr KN, Aaronson NK, Alonso J, Burnam MA, Patrick DL, Perrin EB, Roberts
JS. Evaluating quality-of-life and health status instruments: development ofscientific review criteria. Clin Ther 1996; 18:979-992.
221. Melzack R, Katz J. Pain assessment in adult patients, Wall and Melzack's
Textbook of pain, 5th ed. McMahon SB, Koltzenburg M (Eds). Philadelphia, Elsevier Churchill Livingstone, 2006, pp 291-304.
222. Kurz A, Sessler DI, Lenhardt R. Perioperative normothermia reduces the
incidence of surgical wound infection and shorten hospitalization. Study ofwound infection and temperature group. N Engl J Med 1996; 334:1209-1215.
223. Schmied H, Kurz A, Sessler DI, Kozek S, Reiter A. Mild hyperthermia increases
blood loss and transfusion requirements during hip arthroplasty. Lancet 1996; 347:289-292.
224. Kempainen RR, Brunette DD. The evaluation and management of accidental
hypothermia. Respir Care 2004; 49:192-205.
225. Björkelund KB, Hommel A, Thorngren KG, Lundberg D, Larsson S. Factors at
admission associated with 4-months outcome in elderly patients with hip fracture. AANA J In press. 2008a.
226. Björkelund KB, Hommel A, Thorngren KG, Lundberg D, Larsson S. The
influence of perioperative care and treatment on 4-months outcome in elderlypatients with hip fracture. In manuscript. 2008b.
227. Ritchie K, Polge C, de Roquefeuil G, Djakovic M, Ledesert B. Impact of
anesthesia on the cognitive functioning of the elderly. Risk factors for dementia. Int Psychogeriatr 1997; 3:309-326.
228. Flacker JM, Marcantonio ER. Delirium in the elderly. Optimal management.
Drugs Aging 1998; 2:119-130.
229. Urwin SC, Parker MJ, Griffiths R. General versus regional anaesthesia for hip
fracture surgery: a meta-analysis of randomized trials. Br J Anaesth 2000; 84:450-455.
230. Tierney AJ. Undernutrition and elderly hospital patients: a review. J Adv Nurs
1996; 4: 228-236.
231. Koval KJ, Maurer SG, Sue ET Aharonoff GB, Zuckerman JD. The effects of
nutritional status on outcome after hip fracture. J Orthop Trauma 1999; 3:164-169.
232. Avenell A, Handoll HH. A systematic review of protein and energy
supplementation for hip fracture aftercare in older people. Eur J Clin Nutr 2003; 57: 895-903.
233. Titler MG, Herr K, Schilling ML, Marsh JL, Xie XJ, Ardery G, Clark WR,
Everett LQ. Acute pain treatment for older adults hospitalized with hip fracture: current nursing practices and perceived barriers. Appl Nurs Res 2003; 16:211-227.
234. Milisen K, Abraham IL, Broos PL. Postoperative variation in neurocognitive and
functional status in elderly hip fracture patients. J Adv Nurs 1998; 1:59-67.
235. Milisen K, Foreman MD, Wouters B, et al. Documentation of delirium in elderly
patients with hip-fracture. J Gerontol Nurs. 2002; 28:23-29.
236. Ambulans, Katastrof och Beredskapsförvaltningen, Region Skåne. Ambulans-
överläkargruppen och Utbildningsenheten. Riktlinjer och behandlings- anvisningar. Akut prehospitalt omhändertagande, Lund, Sweden, 2001.
237. Bjorkelund KB, Larsson S, Gustafson L, Andersson E. The Organic Brain
Syndrome (OBS) scale: a systematic review. Int J Geriatr Psychiatry. 2006; 3:210-22.
238. Altman DG. Practical statistics for medical research. London: Chapman & Hall,
239. Bland JM, Altman DG. Multiple significance tests: the Bonferroni method. BMJ
1995; 310:170.
240. Hosmer DW, Lemeshow S. Applied logistic regression. New York: John Wiley
& Sons, Inc, 2000.
241. McDowell I, Newell, C. Measuring Health: a guide to rating scales and
questionnaires. New York, Oxford University Press, 1996.
242. Streiner DL, Norman GR. Health measurement scales: a practical guide to their
development and use. Oxford, Oxford University Press, 1995.
243. Deklarations of Helsinki. Revised version. Adopted by the World Medical
Association (WMA), October 1996. I: Medicinska forskningsrådet (MFR).
Riktlinjer för etisk värdering av medicinsk humanforskning : forskningsetisk policy och organisation i Sverige. MFR-rapport 2. Stockholm: Medicinskaforskningsrådet., 2000.
244. The ICN Code of Ethics for Nurses. International Council of Nurses (ICN). ICN
Code of Etics. Geneva, International Council of Nurses, 2000.
245. Hermerén, G. Kunskapens pris. Forskningsetiska problem och principer i
humaniora och samhällsvetenskap. Stockholm: Forskningsrådets förlagstjänst, 1986.
246. Minthon L, Edvinsson L, Gustafson L. Correlation between clinical
characteristics and cerebrospinal fluid neuropeptide Y levels in dementia of the Alzheimer type and frontotemporal dementia. Alzheimer Dis Assoc Disord 1996;10:197-203.
247. Nilsson K, Warkentin S, Hultberg B, Fäldt R, Gustafson L. Treatment of
cobalamin deficiency in dementia, evaluated clinically and with cerebral bloodflow measurements. Aging 2000; 12:199-207.
248. Granberg-Axell A, Bergbom I, Lundberg D. Clinical signs of ICU
syndrome/delirium: an observational study. Intensive Crit Care Nurs 2001; 17:72-93.
249. Holmquist IB, Svensson B, Höglund P. Psychotropic drugs in nursing- and old-
age homes: relationships between needs of care and mental health status. Eur J Clin Pharmacol 2003; 59:669-676.
250. Polit DF, Beck CT. Nursing research. Principles and methods. Philadelphia,
Lippincott Williams & Wilkins, 2004.
251. Kazdin A E. Research design in clinical psychology (4th ed.), Boston, Allyn &
252. Kamber Skåne. Riktlinjer och behandlingsanvisningar. Akut prehospitalt
omhändertagande, Lund, Sweden, 2004.
253. Fillenbaum GG. Comparison of two brief tets of organic brain impairment, the
MSQ and the Short Portable MSQ. J Am Geriatr Soc 1980; 28:381-384.
254. Yeh S-C J, Liu Y-Y. Influence of social support on cognitive function in elderly.
BMC Health Services Research. 2003; 9:1-9.
255. Gunningberg L, Lindholm C, Carlsson M, Sjoden PO. The development of
pressure ulcers in patients with hip fractures: inadequate nursing documentationis still a problem. J Adv Nurs 2000; 31:1155-1164.
256. Nunnally JC, Bernstein IH. Psychometric theory. New York, McGraw-Hill,
257. Holte K, Sharrock NE, Kehlet H. Pathophysiology and clinical implications of
perioperative fluid excess. Br J Anaesth 2002; 89:622-32.
258. Lindesay J, Rockwood K, Rolfson D. The epidemiology of delirium. In:
Rockwood K, Lindesay J, Macdonald A. (Eds). Delirium in old age, 1st edition. Oxford, Oxford University Press, 2002, pp 27-50.
259. Beaupre LA, Cinats JG, Senthilsevan A, Lier D, Jones CA, Sharfenberger A,
Johnston DWC, Saunders LD. Qual Saf Health Care 2006; 15:375-379.
Source: http://portal.research.lu.se/portal/files/3306115/1057240.pdf
ARTIGO DE REVISÃO / REVIEW ARTICLE Data de recepção / Received in: 17/09/2010 Data de aceitação / Accepted for publication in: 10/11/2010 Marta Salgado, Rute Reis, António Vinhas de Sousa, Elza Tomaz, Irina Dydenko, Andreia Ferrão, Fátima Ferreira, Filipe Inácio Serviço de Imunoalergologia / Immunoallergology Department – Hospital de São Bernardo, Setúbal
Mardi 19 octobre 2010 Numéro 202 Créé en 1950 Vendu en kiosques et par abonnement Prix 4,50 CHF (TVA 2,4% incl.) - 3,00 EUR [email protected] Rédacteur en chef: François Schaller ACCORD SUR DES SANCTIONS AUTOMATIQUESLa fin de la désinvolturebudgétaire en Europe PAGE 21 JA-PP/JOURNAL — CASE POSTALE 5031 — CH-1002 LAUSANNE DOW JONES 11143.69