Levitra enthält Vardenafil, das eine kürzere Wirkdauer als Tadalafil hat, dafür aber schnell einsetzt. Männer, die diskret bestellen möchten, suchen häufig nach levitra kaufen ohne rezept. Dabei spielt die rechtliche Lage in der Schweiz eine wichtige Rolle.
Parkinsonismo iatrogeno

PROGETTO UNIVA 2013
Journal Club
Pietro Gareri, MD, PhD
Geriatra ASP Catanzaro
Lamezia Terme 3 Luglio 2013


Drug-induced parkinsonism (DIP) was recognized in the early 1950s as a commoncomplication of antipsychotic therapy; initially considered to be present in 4 - 40%of patients treated with the first neuroleptics
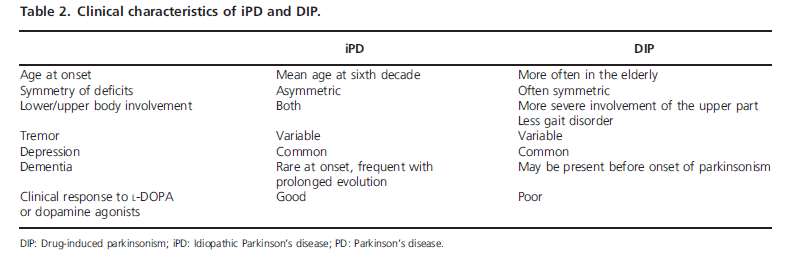
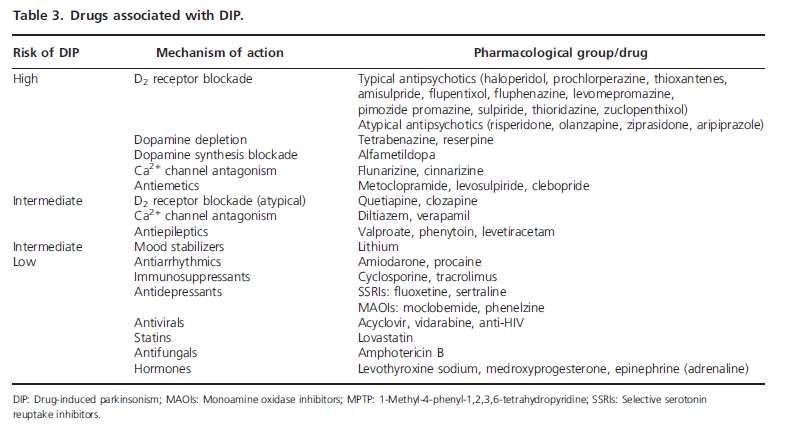
Reported as a complication of treatments with diverse compounds including newgeneration antipsychotics, CCB, gastrointestinal prokinetics, antiarrhythmics,antidepressants and others
Reversible after drug suppression
Persistency of the clinical deficits after culprit withdrawal may indicate a
previous subclinical parkinsonism unmasked by the involved drugs
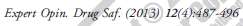
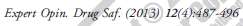
Two groups of DIP patients: those with normal SPECT (suggesting normal densityof dopamine terminals) and patients with reduced striatal uptake (suggestive oflesion of the presynaptic dopamine terminals)
Some individuals, perhaps with genetic variants of genes involved in familialParkinson's disease (PD), are especially susceptible to this complication
Key points
• Despite advances in ancillary tests, the clinical course of parkinsonism after
drug discontinuation is paramount for a correct differential diagnosis.
• Management of DIP includes prevention, early recognition and withdrawal
of the offending drug.
• Certain variables such as age, use of multiple drugs or previous vascular
damage to the nigrostriatal pathway increase the risk of DIP. However, DIP
susceptibility is highly variable and unpredictable among different subjects.
• DIP is the second cause of parkinsonism but is still perceived as a neglected
pathology on the day-to-day clinics by most of the studies
• Population studies have detected incidences of DIP among the
50 -- 99 years age group of 22.94 per 100,000 person-years
• In the USA estimation of 20,000 -- 25,000 incident cases of DIP
• Another study focused on an elderly population of 64 years or
older patients estimated the prevalence of DIP to be 3.3%,representing a 37% of all cases of parkinsonism
• DIP as the second cause of parkinsonism after iPD with a
prevalence of 20 -- 56%
• Antipsychotics are the prototypical and most common
compounds producing DIP
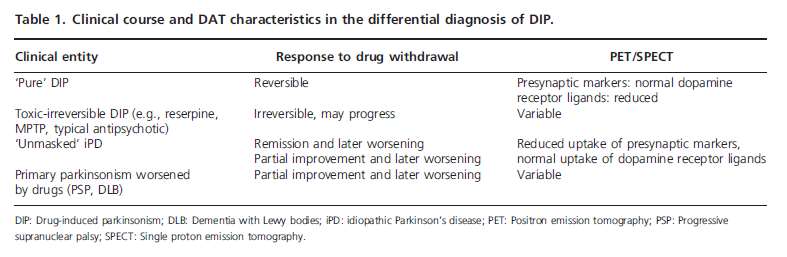
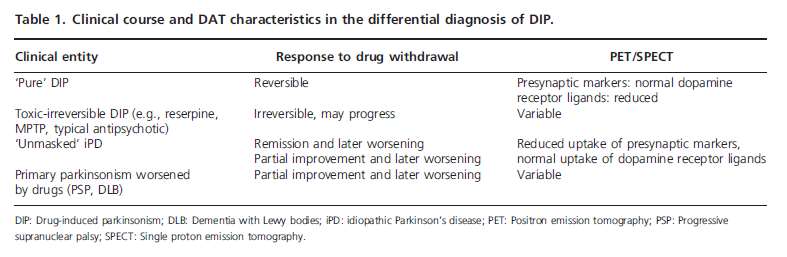
• Akinetic rigid syndrome
• Type of causative drug• Age of the patient• Length of exposure • Dose
• Asymmetry is less characteristic of DIP although it may happen. • In contrast with vascular parkinsonism, which severely involves the legs and
produces frequent impairment of gait, DIP produces a less severe gait disorder
and a relatively more pronounced ‘masked' facial expression.
• The first symptom is a decrease in arm swing when walking, rather than a
difficulty to rise from a low seat. The presence of tremor is variable.
• It is uncommon with drugs that selectively involve the dopamine
neurotransmission, such as dopamine D2 blockers, and much more frequent
with other compounds that act through a less selective mechanism, such as
amiodarone or calcium channel blockers
• Patients not achieving full recovery after a long period of time should be
excluded from the diagnosis of ‘pure' DIP.
• There is evidence supporting that certain drugs can induce a persistent and
even progressive parkinsonism.
• Lack of reversibility can also be explained considering that at least some
patients with DIP are individuals in the presymptomatic phase of PD
2 Muscarinic
D2 receptor occupancy(%)
Pathogenetic mechanisms (1)
• Diminished D2 receptor stimulation in the striatum• The pharmacological effect of antipsychotics are achieved with a blockade
of a 60 -- 70% of the dopamine receptors and parkinsonism appears whenthe blockade reaches 75 -- 80% (occupancy not equal to antagonism)
• Other compounds act by inhibiting uptake of dopamine into granular
vesicles of presynaptic neurons. Monoamines are concentrated from thecytoplasm into vesicles by vesicular monoamine transporters (VMATs)(two isoforms).
• VMAT1 is located predominantly in peripheral endocrine and paracrine
cells while VMAT2 is located in the brain and sympathetic neurons. TBZ
and reserpine bind to the same site on the VAMT2 but to different
conformations. While reserpine binds irreversibly being potentially toxic,
TBZ displays reversible binding.
Pathogenetic mechanisms (2)
• Certain calcium channel antagonists decrease neuronal activity, reduce
monoamine neurotransmission and dopaminergic viability and reduce the
levels of HVA in the CSF of healthy primates suggesting that, even without
previous dopamine dysfunction, they can produce a calcium-dependent
reduction of dopamine release.
• Other compounds responsible for DIP may produce not only a reversible
pharmacological impairment of dopamine neurotransmission, but alsoneurotoxic effects on dopamine neurons. Short-term blockade ofdopamine D2 receptors inhibits the production of neurotrophic substancesfor dopamine neurons, such as BDNF and stimulates the firing ofdopamine neurons increasing the metabolism of dopamine andproduction of free radicals.
Pathogenetic mechanisms (3)
• Treatment with haloperidol increases oxidative metabolism in the brain, reduces
the phosphorylation of Akt and activates caspase-3
• Pharmacokinetic has explained interindividual differences in susceptibility to DIP
by haloperidol variability related to CYP34A and the polymorphic CYP3A5
isoenzyme systems, which metabolize haloperidol to its pyridinium ion.
Compounds interacting with this system such as antidepressants may enhance
toxicity related to the pyridinium ion in patients treated with haloperidol.
• Parkin knockout mice are more susceptible to the toxic effects of cinnarizine than
wild-type controls.
• In parkin-deficient mice, cinnarizine produced changes in the metabolism of
dopamine and increased the expression of proapoptotic proteins and reduced the
proportion of astroglia and hyperactivated microglial cells, suggesting that in
these genetically modified animals, cinnarizine selectively triggers the expression
of neurotoxic factors that could produce an irreversible damage to the
nigrostriatal dopamine system.
• Prevention: many patients with cognitive impairment or communication
disorders are given antipsychotics ‘larga manu' to cover lack of adequate
behavioral stimulation, medical attention or to play a ‘calming effect' on
medical problems such as pain, constipation or urinary retention, or for
conditions unrelated to psychosis including insomnia, anxiety or depression
• The second management strategy is to substitute certain compounds by a
related drug with a better side-effect profile (i.e. domperidone).
• Clozapine is a useful agent for the treatment of drug-induced psychosis in PD,
but it can also improve the clinical symptoms of DIP induced by other D2
• The third strategy would be to carefully monitor individuals with special risk
factors for developing DIP. Senior individuals, those with family history of
parkinsonism, dementia or tremor and those under treatment with multiple
drugs are more prone to suffer DIP.
• The prognosis of complete recovery is uncertain and 10 -- 30% of the patients
will continue to have symptoms several months after the discontinuation of
the causative drug.
• At least 10% of patients will develop a persistent and progressive parkinsonian
Certain variables such as age, previous vascular damage to the nigrostriatalpathway, treatment with multiple drugs and genetic variants have been identifiedas risk factors for the appearance of DIP, but we still lack the knowledge todetermine why some people are so resistant to astonishingly high doses ofdopamine blockers and others are incredibly sensible to lower doses of the sameagents.
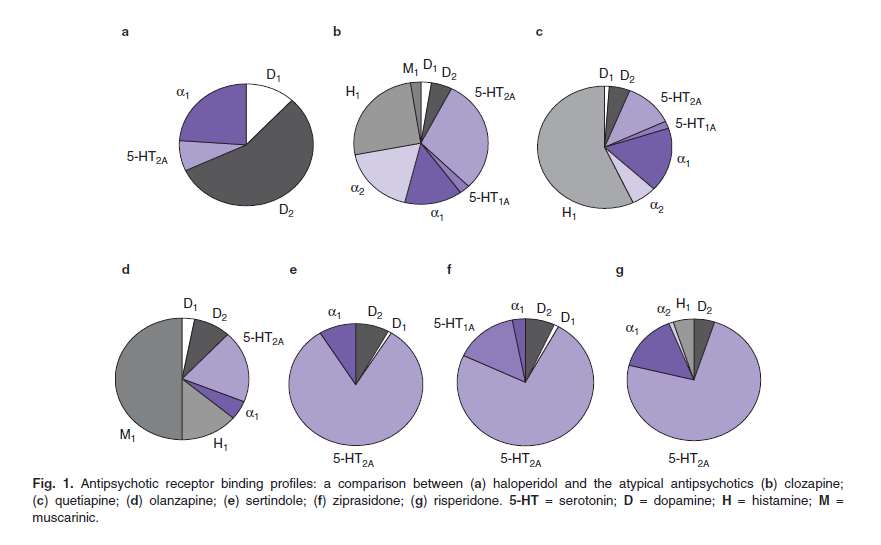
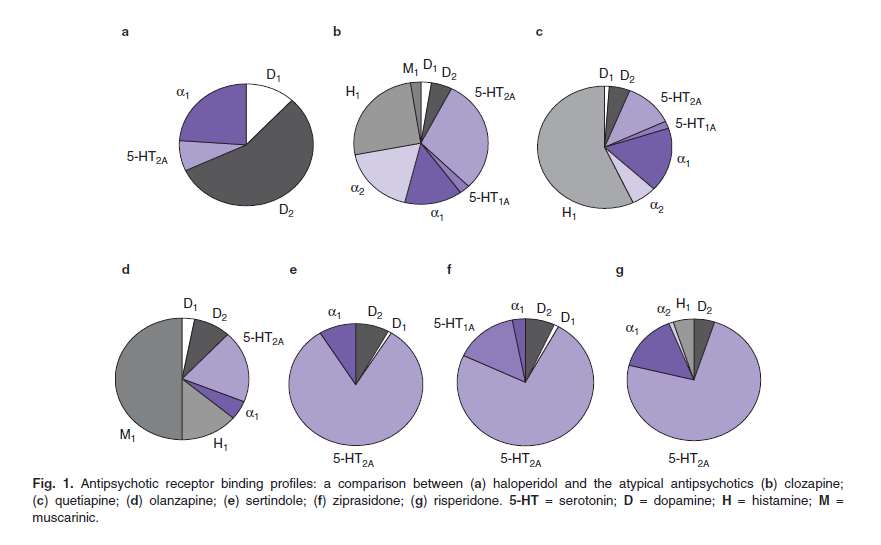
Several mechanisms including a more antagonistic effect toward serotonin-2Areceptors than toward dopamine receptors, and a faster dissociation from D2
receptors explain the lower frequency of DIP with second- compared with first-generation antipsychotics
The culprits have to be looked for and withdrawn if possible, second- and third-generation are preferred to first-generation antipsychotics, there is no evidencesupporting the use of levodopa, dopamine agonists or anticholinergics for thetreatment of DIP and gastrointestinal motility drugs not crossing the blood--brainbarrier (such as domperidone) are preferred to those with central effects.
Second-generation antipsychotics such as quetiapine are associated with very lowrates of DIP. Others, such as clozapine, have not been associated with DIP butentail a spectrum of undesirable side effects.
Grazie per la vostra
Source: http://www.univacalabria.it/formazione/2013/pdf/3luglio/Gareri.pdf
FOR CANCER By Harvey Kaltsas, D.O.M., A.P. Hyperthermia and Electrotherapy Janice wasn't flattered when the German shopkeeper congratulated her on the baby she looked about to deliver. For despite her severely swollen abdomen, Janice was not pregnant. She had advanced, multi-drug resistant peritoneal cancer with an accumulation of fluid in her abdominal cavity. Janice had been told she was in the end stages of an eight-year battle that had started with ovarian cancer and metastasized into liver, colon and bladder cancer.
WHO Technical Report Series EVALUATION OF CERTAIN Sixty-third report of the Joint FAO/WHO Expert Committee on World Health Organization Geneva 2005 30/5/2005, 11:10 AM WHO Library Cataloguing-in-Publication Data Joint FAO/WHO Expert Committee on Food Additives (2004 : Geneva, Switzerland) Evaluation of certain food additives : sixty-third report of the Joint FAO/WHO Expert Committeeon Food Additives.