Cobef.org.br
COMPETENCE STANDARDS FOR THE
PHARMACY PROFESSiON
COMPETENCE STANDARDS FOR THE
PHARMACY PROFESSiON
The Pharmacy Council of New Zealand (the Council) is established under the Health
Practitioners Competence Assurance Act 2003 (HPCAA) and has a duty to protect the
public and promote good pharmacist practice. The Pharmacy Council is responsible
for registration of pharmacists, the setting of standards for pharmacists' education,
scopes of practice and conduct.
Assessment against the Competence Standards for the Pharmacy Profession was
first implemented for registration in 1997, and in 2003 it was reviewed and implemented
for all pharmacists registering in the Pharmacist scope of practice1 in accordance
with the HPCAA. While the standards have remained relevant to the scope of practice
of pharmacists' since its implementation, Competence Standard One has recently
been revised and expanded to include cultural competence.
1 Pharmacist scope of practice as defined by the Pharmacy Council of New Zealand http://www.pharmacycouncil.org.nz/scopes
PuRPOSE OF THE COMPETENCE STANDARDS• Ensure that a pharmacist possesses all relevant competencies to undertake the roles and services described in the Pharmacist scope of practice
• Assist in the development of education and training and development of pharmacists and intern pharmacists e.g. inform development of initial
curriculum; assist providers in identifying learning outcomes; use as a self- assessment tool to evaluate their own level of competency; assist employers and pharmacists to identify ongoing training and development needs
• Assist the individual pharmacist to facilitate their continuing professional development (CPD) e.g. a tool for pharmacists to use to assess their own practice
STRuCTuRE OF THE COMPETENCE STANDARDS
The Competence Standards for the Pharmacy Profession consist of SEVEN competence standards.
Competency in all seven standards is required for initial registration in the Pharmacist scope of practice.
Competency in Competence Standard 1: Practise Pharmacy in a Professional and Cultural y Competent Manner must be maintained by all practising pharmacists regardless of their practice setting.
The seven broad areas of competency are:
• Practise Pharmacy in a Professional and Cultural y Competent Manner
• Contribute to the Quality Use of Medicines
• Provide Primary Health Care
• Apply Management and Organisation Skil s
• Research and Provide Information
• Dispense Medicines
• Prepare Pharmaceutical Products
Figure 1 il ustrates and explains the basic structure of the Competence Standards for the Pharmacy Profession.
Figure 1 Competence Standards Structure
Competence • Describes a broad area of pharmacy practice by the standard number and name.
Standard
• E.g: Competence Standard 1 Practice Pharmacy in a Professional and Cultural y Competent Manner
• It also includes a "descriptor" and a "range statement" which provides an overview of the standard and the practice
expectations of the pharmacist.
• A breakdown of the processes in relation to the overall expectation defined by the standard.
• Each standard is built with a number of essential elements.
• E.g: Element 1.4 Practice pharmacy within New Zealand's cultural y diverse environment; Element 1.5 Understands
Hauora Ma-ori; Element 1.6 Commit to continuing professional development and life-long learning.
• A breakdown of tasks that need to be performed to meet the processes described at the elemental level.
• Each element consists of a number of essential activities (sometimes referred to as "performance criteria").
• E.g: Activity 1.4.1 Undergoes a process of self-reflection to identify one's own cultural values; Activity 1.4.2 Identifies
the cultural diversity of one's own practice; Activity 1.4.3 Respects the individual.
• A range of examples are provided as a benchmark of evidence for every activity. The list of examples provided are not
exhaustive and those listed may not be relevant to the practice of all pharmacists.
• Their purpose is to guide ongoing learning.
• Identify examples as they relate specifical y to one's own practice and it is these that should be recorded.

COMPETENCE STANDARD 1
Practise Pharmacy in a Professional and Culturally Competent Manner
The Pharmacy Council recognises that cultural competence, clinical competence and ethical conduct are integral to professional pharmacy practice. Professionalism is encompassed by a set of attitudes, knowledge and skills based on clinical competence, communication skills, ethics, societal and legal requirements resulting in the application of behaviours that demonstrate a commitment to excel ence, respect, integrity, empathy and accountability. This standard outlines these responsibilities which apply to all pharmacists, regardless of their pharmacy practice.
• Cultural competence is the ability to interact respectful y and effectively with persons from a background that is different from one's own. It goes
beyond an awareness of or sensitivity to another culture to include the ability to use that knowledge in cross-cultural situations, and includes the development and implementation of processes, procedures and practices that support the delivery of cultural y competent (appropriate) services.
• Clinical competence, as expected of a pharmacist, is the application of knowledge and skil s to ensure the safe and quality use of medicines to
optimise health outcomes.
• Ethical conduct, as described in the Pharmacy Council Code of Ethics, is the expression of those principles and values that underpin the pharmacy profession.
All pharmacists must understand and apply the legal and ethical requirements to practise pharmacy professional y.

Culture includes, but is not restricted to, age, gender, sexual orientation,
Work professional y in pharmacy practice
race, socioeconomic status (including occupation), religion, physical,
Note: Examples of evidence are a guide only and are by no means an
mental or other impairments, ethnicity and organisational culture.
Legislation referred to in these competence standards includes the
1.1.1 Behaves in a professional manner
fol owing (refers to the latest editions and amendments) Acts and
Examples of Evidence:
Regulations, Guiding Documents and Codes of Practice that directly or
Maintains conduct becoming of a pharmacist towards other health
indirectly impact on the professional practice of pharmacy:
professionals, patients & public as defined in the Code of Ethics e.g.
• Advertising Standards Authority Inc. Code for Therapeutic
behaviour, demeanour, conduct
1.1.2 Maintains a consistent standard of work within relevant
• Consumer Guarantees Act 1993
scope of practice
• Dietary Supplement Regulations 1985
Examples of Evidence:Consistently performs to an acceptable standard of work and
• Fair Trading Act 1986
expects the same from others
• Hazardous Substances and New Organisms Act 1996
• Hazardous Substances and New Organisms Regulations
Explains quality systems and defines who is responsible in the
• Health & Safety in Employment Act 1992
• Health Act 1956
1.1.3 Accepts responsibility for own work tasks and
• Health and Disability Commissioner Act 1994
• Health and Disability Commissioner (Code of Health and Disability
Examples of Evidence:
Service Consumers' Rights) Regulations 1996
Accepts that their actions or inactions have an effect on a person's
• Health and Disability Services – Pharmacy Services Standard
Identifies tasks, or aspects of their practice for which she/he is
• Health Information Privacy Code 1994
personally responsible
• Health Practitioners Competence Assurance Act 2003
Identifies wider effect of his/her actions on individuals and the community
• Health (Needles and Syringes) Regulations 1998
Accepts responsibility for helping develop systems, processes and
• Health (Retention of Health Information) Regulations 1996
professional practices that are responsive to the cultural needs /
• He Korowai Oranga: Ma-ori Health Strategy 2002
paradigms of the patient
• Human Rights Act 1993
1.1.4 Works within the limitations of own professional
• Ma-ori Health Strategy for the Pharmacy Profession
expertise, and relevant competence standards
• Medicines Act 1981
Examples of Evidence:Identifies professional limitations
• Medicines Regulations 1984
Accesses information, advice and assistance for work tasks outside
• Medicines (Designated Prescriber: Nurse Practitioner)
one's own professional expertise or experienceWorks within the competence standards identified in one's own
• Medicines (Designated Prescriber: Optometrists) Regulations 2005
• Medicines (Standing Order) Regulations 2002
1.1.5 Works accurately
• Ministry of Health, Code of Practice for Child-resistant Packaging
Examples of Evidence:
of Toxic Substances 1998
Minimises mistakes
• Misuse of Drugs Act 1975
Acts immediately to rectify harm arising from mistakes.
• Misuse of Drugs Regulations 1977
Documents errors and steps taken to prevent their recurrence
• Pharmacy Council of New Zealand Code of Ethics 2011
1.1.6 Shares professional strengths with others
• Privacy Act 1993
Examples of EvidenceTrains other staff e.g. gives presentations relevant to pharmacy practiceDiscusses aspects of pharmacy practice with pharmacist col eaguesMentors and guides other pharmacists and staffActively supports and encourages development of cultural competency for all staff
COMPETENCE STANDARD 1
Practise Pharmacy in a Professional and Culturally Competent Manner
1.3.2 Communicates effectively with persons from a background
Comply with legal requirements and codes of ethics
different from one's own
1.2.1 Understands and is able to explain the application of the
Examples of Evidence:
legislation and codes relating to pharmacy practice
Uses correct pronunciation of names as a sign of respect for al
Examples of Evidence:
Explains the application of the current legislation relating to
Describes how cultural differences may affect communication
pharmacy practice
Describes where to access legislation and codes relating to
Understands and describes ways to avoid communication styles
pharmacy practice
(verbal and non-verbal) that might give offence
Explains the legal implications of negligence with respect to
Identifies those cultures for whom silence may not imply agreement
legislation and codes
Ascertains who family spokesperson is e.g. in some cultures a male
1.2.2 Complies with those parts of the legislation that apply to
family member acts in this role
his/her pharmacy practice
Wherever possible uses kanohi ki te kanohi (face to face)
Examples of Evidence:
communication with Ma-ori
Fulfils all legal requirements that regulate pharmacy practice e.g.
Involves patient's nominated representative, wha-nau or appropriate
Methadone dispensing within the Misuse of Drugs Act and
cultural services, where necessary, to better understand patient's
cultural needs and assist a patient in their understanding
Complies with the HDC Code of Health and Disability Services
Learns and uses appropriate expressions in the main languages used
Consumers' Rights
in their community
Complies with the Health Information Privacy Code
1.3.3 Adapts communication to the situation
1.2.3 Complies with code of ethics for pharmacy practice
Examples of Evidence:
Examples of Evidence:
Identifies barriers to communication and responds appropriately
Complies with the Pharmacy Council of NZ Code of Ethics
Ensures consultations take place in an appropriate setting,
Complies with workplace codes
minimising interruptions
Discusses the application of Pharmacy Council of NZ Code of Ethics
Adapts non-verbal communication styles to suit the receiver, which may differ from one's own
Uses a range of communication tools e.g. accesses appropriately
Communicate effectively
trained interpreter services, suitable to the level of a patient's
1.3.1 Listens effectively, and speaks and writes clearly in
literacy and understanding
1.3.4 Establishes and maintains effective working relationships
Examples of Evidence:
Examples of Evidence:
Communicates effectively in English within the workplace for the
Identifies and builds relationships with key partners within one's
purposes of practising as a pharmacist
Structures and presents written information e.g. fax, e-mail, letter,
Treats patients and col eagues as equal partners, building rapport,
memo, referrals, appraisals, in ways appropriate for each situation
respect and trust in partnerships
and to meet the needs of the receiver
Practises whanaungatanga (establishing connections) in order to
Ensures information, either given or received, is accurately
build connections and trust in relationships with Ma-ori
Works co-operatively with appropriate family, wha-nau, and
Uses "active and reflective listening" techniques such as "check-
community resource people where this is desired by the patient, and
back" interviewing to confirm that the receiver understands the
when it does not conflict with other clinical or ethical responsibilities
Col aborates with and includes others (pharmacy staff, col eagues,
Answers Medicine Information (MI) queries, either verbal y or in
other health professionals, cultural groups) in decision making
written format, meeting MI standards
Actively resolves and negotiates cross-cultural misunderstandings e.g. identifies cultural y appropriate and effective means of gaining consumer feedback.
Understands and explains different concepts of health and uses this
Practise pharmacy within New Zealand's cultural y
understanding in working towards optimal health outcomes
diverse environment
Understands that culture includes the practice of traditional healing
1.4.1 Undergoes a process of self-reflection to identify one's
own cultural values
1.4.5 Identifies and works towards reducing factors that
Examples of Evidence:
contribute to disparities in health outcomes
Understands the impact that one's own identity, including cultural
Examples of Evidence
values, has on one's own practice as a pharmacist
Learns about the nature and extent of health disparities in New
Uses appropriate tools e.g. self-assessment quiz, to identify his/her
own cultural values
Participates in programmes targeted at reducing health disparities
Reflects on one's own cultural values through peer group discussions
Acts as an advocate for patients in seeking provision of appropriate
Undertakes self-reflection on a regular basis
resources for treatment
Recognises that at times there may be conflict between one's own
Uses evidence-based approach to advise / treat individual patients
professional culture/values and the culture of the patient
and to educate community
1.4.2 Identifies the cultural diversity of one's own practice
Accesses local data on community health needs and uses
Examples of Evidence:
knowledge to contribute to improvements in health care
Develops community profile to identify cultural mix
Develops relationships with key groups and undertakes consultation
Knows where and how to access local community support
on a regular basis in order to work towards reducing health
Uses knowledge of their own community profile to better
understand the impact of health disparities in relation to that profile
understand Hauora Ma-ori (please see glossary)
1.4.3 Respects the individual
1.5.1 Understands the relevance of Te Tiriti o Waitangi
Examples of Evidence
Examples of Evidence:
Avoids stereotyping e.g. recognises that culture/ethnicity is not
Demonstrates an understanding of the contemporary application of
necessarily reflected in an individual's physical appearance.
Te Tiriti o Waitangi through the principles of partnership,
Demonstrates awareness that general cultural information may not
participation and protection
apply to specific patients
Accesses, describes and/or implements the principles of the DHB
Shows consideration for the patient's knowledge of their own
bicultural policy
condition and preferred course(s) of treatment
Learns about the impact of pre- and post-Te Tiriti o Waitangi events
Negotiates terms of the therapeutic relationship with the individual
on the health of New Zealanders
where appropriate
Develops working relationships with key Ma-ori stakeholders e.g. Iwi
Recognises the right of individuals to have health beliefs and
/ Hapu- / Wha-nau / Ma-ori organisations, where appropriate, in order
practices different to one's own
to improve Ma-ori health outcomes
Respects the right of the individual to exercise autonomy in decision-
1.5.2 Understands Ma-ori views of health
Examples of Evidence:
Treats the individual as an equal partner
Utilises knowledge of Ma-ori models of health when developing
1.4.4 Understands the impact of culture on health status and on
maintenance of health
Develops and uses knowledge of core Ma-ori practices including
Examples of Evidence
tikanga and kawa to improve relationships and health outcomes
Focuses on the influence of a patient's culture, in conjunction with
Demonstrates knowledge of principles of Rongoa- and endeavours to
their medical condition, to improve adherence to treatment and
engage with local Rongoa- practitioners
health outcomes e.g. fasting during Ramadan
Recognises that prior to European contact, Ma-ori had a range of
Assesses and enhances patient adherence while acknowledging the
world views and practises, and can explain the relevance to the
patient's view of health
current health status of Ma-ori
COMPETENCE STANDARD 1
Practise Pharmacy in a Professional and Culturally Competent Manner
1.5.3 Addresses the differing health status of Ma-ori and
Demonstrate problem solving skil s
Examples of Evidence:
1.7.1 Solves own problems
Commits to helping reduce the disparities in access to care and
Examples of Evidence:
treatment outcomes for Ma-ori
Differentiates between personal and professional problems
Accesses and contributes to the goals of the Ma-ori Health Strategy
Takes ownership of problems and chal enges, and resolves these
for the Pharmacy Profession
Uses evidence-based guidelines to promote consistency of care and
Recognises indicators of impaired personal performance and acts to
equity of health service delivery
mitigate risks to self, col eagues and patients
Investigates and utilises appropriate resources to deliver health
Demonstrates awareness of own personal limitations and has
information messages to Ma-ori
strategies in place in order to ameliorate these
1.5.4 Pronounces Te Reo Ma-ori correctly, in particular proper
1.7.2 Resolves conflicts
nouns, and understands common or relevant words
Examples of Evidence:
Examples of Evidence:
Identifies causes of conflict in the workplace
Common words e.g. wha-nau (family); poho (chest); kauma-tua (elder); hauora/ waiora (health); puku (stomach); tuara- (back); tamariki
Participates in conflict resolution processes
Uses negotiating and problem-solving skil s in shared decision-
Completes Te Reo Ma-ori course
making with a patient or col eague
Demonstrates fluency in Te Reo Ma-ori
1.7.3 Works to resolve workplace and professional practice
Examples of Evidence:
Commit to continuing professional development and
Identifies and explains potential workplace and professional practice
life-long learning
1.6.1 Reviews and reflects on own professional practice against
Adopts questioning and analytical approach to problem solving
relevant competence standards
Seeks solutions and opportunities to improve
Examples of Evidence:
Works with others to resolve workplace or practice problems
Undertakes a practice review against relevant standards for scope of practice every five yearsIf practice or scope of practice changes, undertakes a practice review immediatelyElicits feedback from others in order to identify learning needs for Continuing Professional Development (CPD)
1.6.2 Undertakes professional development
Examples of Evidence:Acquires knowledge, skil s and training to improve and enhance existing professional practice on an ongoing basisDiscusses professional and practice issues with col eaguesCompletes courses, as necessary, to achieve identified learning goalsIncludes cultural competency education in one's own professional developmentMeets the Recertification requirements as set by the Pharmacy Council of NZ by participating in an accredited programme e.g. ENHANCE
sub-tribe or kin group that is linked by a common ancestor. Hapu- is also a description for being pregnant.
Hauora Ma-ori Ma-ori health, vigour
tribe composed of descendants from a specific ancestor(s). A number of related hapu constitute an iwi. (ko)iwi is also a description associated with bones, or human remains.
kanohi ki te kanohi face to face
protocol – customs of the marae and wharenui
It is an English word which col ectively describes the indigenous peoples of New Zealand; however it is an introduced word and construct used to homogenise the traditional indigenous societal structures of wha-nau, hapu and iwi.
traditional Ma-ori healing
Te Tiriti o Waitangi Treaty of Waitangi: the English text of the
document (as distinct from the Ma-ori text, Te Tiriti o Waitangi), signed by the English representative of Queen Victoria and the Ma-ori chiefs present on 6 February 1840.
correct procedure, custom
cluster of families and individuals who descend from a common ancestor. Wha-nau also means giving birth or to be born.
whanaungatanga relationship, kinship, sense of family connection,
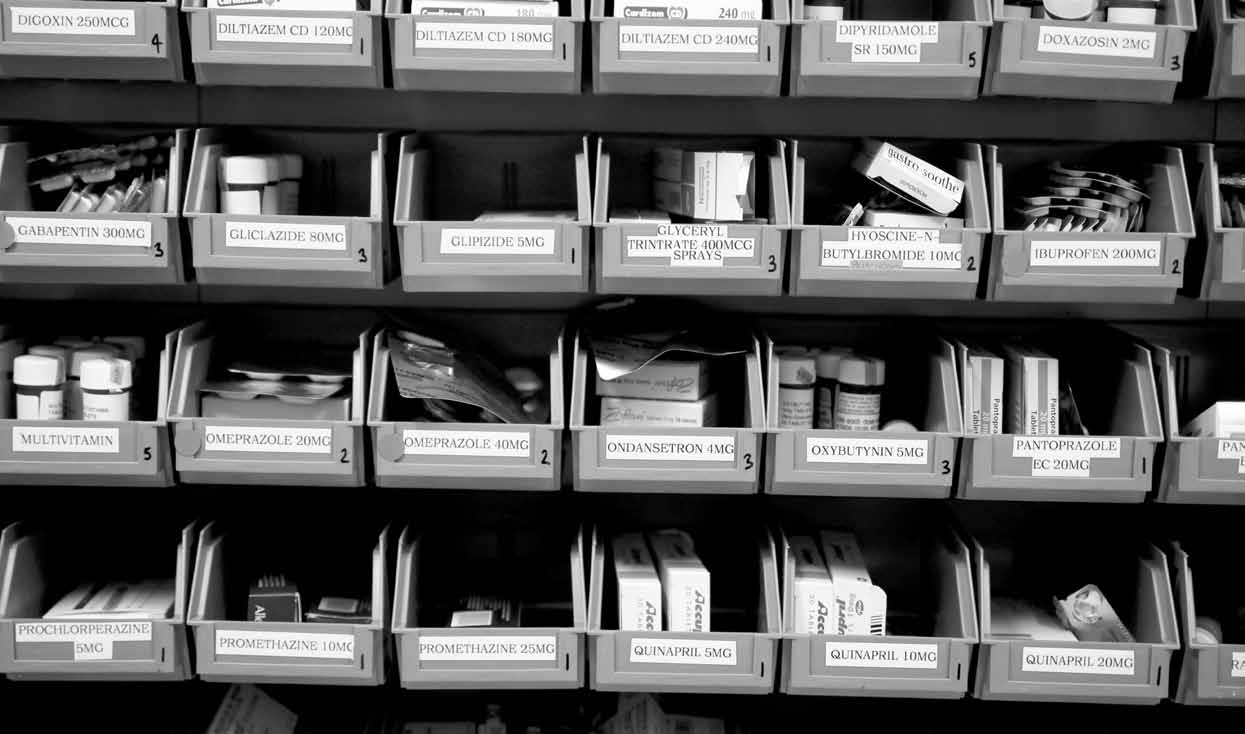
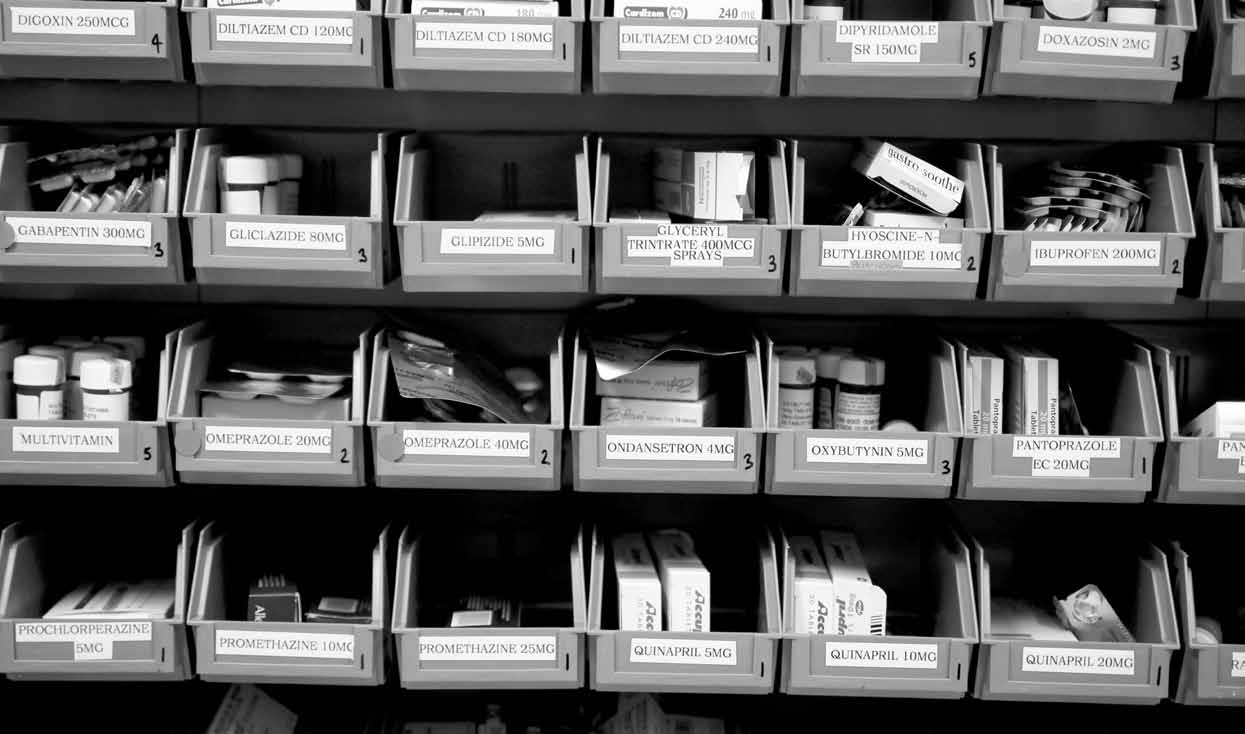
COMPETENCE STANDARD 2
Contribute to the Quality use of Medicines
This competence standard covers the role of the pharmacist in promoting the quality use of medicines within an environment of professional pharmaceutical care. The Pharmacist's role includes selecting, recommending, monitoring and evaluating medicine therapy as part of a health care team. Rational medicine use refers to the evidence-based selection, monitoring and evaluation of medicine therapy in order to optimise health outcomes.
RANgE STATEMENT:At this level the pharmacist's responsibilities are reactive, in that he/she carries out the tasks described in this standard in response to requests about individual patients. The pharmacist is responsible for making recommendations on and providing information about common medicines to other health professionals.
Common medicines are those listed in the latest edition of the MIMS New Ethicals
Readily available references are those available from within the pharmacy including current editions of Martindale, MIMS New Ethicals, BNF and Pharmaceutical Schedule.
2.3.4 Identifies which adverse drug reactions (ADR's) should be
Obtain individual patient history
reported to the Centre for Adverse Reactions Monitoring
2.1.1 Accesses patient medicine records
(CARM) and facilitates the reporting of these
Examples of Evidence:
Examples of Evidence:
Accesses records on pharmacy computer
Identifies reportable ADR's and facilitates the reporting of these
Obtains copies of records (computer/hard copy) from other health
Can explain how to report to CARM if the need arises
2.1.2 Interviews individual patients or their caregivers and/or
Recommend necessary changes to medicine therapy
other health professionals to obtain history of medicines
of individual patients
and other therapies, if necessary
2.4.1 Identifies necessary changes to medicine therapy
Examples of Evidence:
Examples of Evidence:
Obtains patient medicine history of prescription & non-prescription
Identifies potential medicine therapy problems e.g. overdoses,
medicines, complementary therapies and compliance details
contraindications, interactions, incompatibilities, possible ADR's,
possible effects with complementary therapies
interpret information about medicines
2.4.2 Recommends the optimal medicine, dose form and method
2.2.1 Identifies common medicines by their approved generic,
of administration for the patient
trade or common names
Examples of Evidence:
Examples of Evidence:
If necessary, calculates optimal medicine dose for patient
If given one form of a common medicine name, promptly identifies
For specific medicines, explains recommendations, including their
other forms from memory or a reference source
dose forms, formulations, methods of administration
2.2.2 Evaluates the available medicines, dose forms and methods
2.4.3 On request, monitors the medicine therapy of individual
Examples of Evidence:
Examples of Evidence:
Using readily available references, determines the advantages &
Recognises patient symptoms that indicate medicine therapy should
disadvantages of different medicines, their dosages & dose forms
be monitored, e.g. patient on warfarin is bruising easily; patient on
for specific situations or patients
NSAID develops GI problems
2.2.3 Interprets generic equivalence of medicines from different
Liaises with methadone clinic re monitoring reducing doses in
Examples of Evidence
Recommends blood tests for therapies that need monitoring e.g.
Determines brand equivalence from readily available reference
Interprets patient indicators for therapy recommendations, e.g. blood tests for lipid lowering agents, clozapine, gentamicin dosing,
Review the medicine therapy of individual patients
2.3.1 Interprets individual patient's medical history and
Maintain patient records
Examples of Evidence:
2.5.1 Records patient information and updates patient records
Explains possible purposes of each medicine
Examples of Evidence:
2.3.2 For each medicine, checks the dosages and methods of
Complies with workplace procedures & regulations to maintain
administration are optimal
patient records, e.g. maintains prescription records for 10 years
Examples of Evidence:
2.5.2 Maintains privacy and security of patient information
Assesses efficacy & safety of medicine recognising pharmacokinetic
Examples of Evidence:
factors, e.g. age, weight, pregnancy, other therapies
Complies with the Health Information Privacy Code and amendments
Assesses the suitability of dosage form with respect to efficacy,
& workplace procedures regarding security of patient information
safety & compliance, e.g. tablets for a child, inhaler type for
2.5.3 Records clinical decisions and recommendations.
Examples of Evidence:
2.3.3 Assesses the effectiveness of the total medicine therapy
Documents recommendations & outcomes of medicine therapy
Examples of Evidence:
reviews, e.g. interventions book, annotations on prescriptions,
Considers patient's history, indicators of efficacy & patient factors
written report to prescriber
that may affect outcomesEvaluates factors affecting availability & cost of medicine, e.g. unavailable brands, Pharmaceutical Schedule considerations
ElEMENT 2.6
Communicate effectively
2.6.1 Communicates verbal and written information fit for the
receiver
Examples of Evidence
Uses language fit for the receiver, e.g. avoids unnecessary technical
jargon
Uses questioning & listening skil s effectively
Explains clinical & medicine information clearly
2.6.2 Communicates effectively with prescribers and other
health professionals
Examples of Evidence:
Uses questioning & listening skil s to elicit information
Communicates clearly with individual health professionals
Provides medicine information & recommendations in format fit for
the situation: letters, faxes, emails & verbal y by telephone or
face-to-face
2.6.3 Communicates effectively with patients
Examples of EvidenceUses questioning & listening skil s to elicit patient history informationExplains clinical & medicine information clearlyIf necessary uses aids to ensure patients understand information, e.g. language cards, videos, large print labels and Brail e cards.

COMPETENCE STANDARD 3
Provide Primary Health Care
This competence standard concerns the role of the pharmacist in encouraging and assisting people to take responsibility for their own health. Primary health incorporates holistic care of patients including attention to lifestyle, diet, health promotion, illness prevention, referral and the supply of non-prescription medicines, therapies, diagnostic and therapeutic aids. This involves the pharmacist in treatment, referral and education.
RANgE STATEMENT:At this level the pharmacist's responsibilities are reactive in that he/she provides primary health care advice and treatment to individual patients in response to requests. The pharmacist provides assessment, treatment and advice for common minor conditions. The pharmacist's treatment options include all over-the-counter medicines (including Pharmacist Only medicines) and therapies, common diagnostic and therapeutic aids, advice and counselling and referral to other health professionals. Therapies include complementary medicines, herbal remedies and other healthcare products not provided by another healthcare provider.
COMPETENCE STANDARD 3
Provide Primary Health Care
Checks that product is safe for patient,e.g considers interactions,
Elicit a patient history
contraindications & patient factors (e.g. pregnancy & age).
3.1.1 Elicits relevant patient history information
Checks appropriate dose form e.g liquid for child
Examples of Evidence:
3.3.2 Counsels patients about the use of non-prescription
Ascertains current signs & symptoms, other medical conditions,
current & previously tried medicines, al ergies & sensitivities
Examples of Evidence:
Observes patient, e.g. approximate age, visible symptoms
Informs patients on correct & safe use, side effects, storage,
Ensures patient privacy & confidentiality of patient information
precautions & contraindications
3.1.2 Identifies the immediate problem with which the patient
3.3.3 Complies with legal requirements and professional
and ethical conventions regarding the supply of non-
Examples of Evidence:
prescription medicines
Examples of Evidence:
Makes an assessment of patient's condition on basis of history
Records sales of Pharmacist Only Medicines
3.1.3 Interprets patient medicine records
Examples of Evidence:
If an accredited Emergency Contraceptive Pill (ECP) pharmacist, supplies ECP in accordance with Pharmacy Council of NZ ECP
If appropriate, looks in records for contraindications, interactions &
standards and best practice guidelines
factors contributing to presenting problem
Identifies requests that indicate potential for misuse
Complies with Pharmacy Council of NZ Code of Ethics and
Determine the best treatment options for patients
professional guidelines regarding potential misuse of non-
3.2.1 Evaluates patients' situations to determine whether to treat
prescription medicines
or refer
Examples of Evidence:
Evaluates signs, symptoms & history to determine what can be
Advise on diagnostic aids
managed by pharmacist
3.4.1 Explains the use and purpose of diagnostic products
Identifies situations that cannot be managed by pharmacist
Examples of Evidence:e.g. blood glucose test kits, pregnancy tests, blood pressure meters
3.2.2 Refers patients and complies with professional, ethical
and workplace conventions and legal requirements when
3.4.2 Advises and counsels patients about the use of
Examples of Evidence:
Examples of Evidence:
Explains to patient the need to see another health professional
Advises on correct use & care of diagnostic aids
Refers patients to prescriber if patients' medicine fails in its purpose
Demonstrates & explains the correct way to use products, e.g.
or causes an untoward effect
Offers to assist with accessing other health professionals
Checks for patient understanding, e.g. asks patient to repeat back instructions
Seeks informed consent, maintains confidentiality & fulfils requirements of the Privacy Act when contacting another health
professional on behalf of patient
Advise on non-pharmaceutical methods to treat
current primary health conditions
Facilitates the supply of non-prescription medicines or
3.5.1 Counsels patients about self-help measures to reduce
current symptoms or discomfort
Examples of Evidence:
3.3.1 Selects non-prescription medicines to meet patient's
acute needs
Provides advice on non-medicine measures to al eviate symptoms,
Examples of Evidence:
e.g. steam inhalations for head cold congestion
Checks ingredients to ensure product is indicated for patient's situation
3.5.2 Informs and advises patients about community health
3.7.2 Informs and advises patients about preventing the spread
support agencies/organisations and pharmacy-based
of disease
primary health care programmes
Examples of Evidence:
Examples of Evidence:
Counsels patients about preventing the spread of disease including
Advises patients about available agencies & programmes & where
appropriate immunisation, preventing the spread of meningococcal
& how to access them, e.g Plunket, Ma-ori health workers, Age
disease, headlice, chicken pox, measles, safe sexual practices
Concern, Asthma Society, Pharmacy Self Care, methadone & needle
related to STDs and HIV/AIDS, intravenous drug use & blood-borne
3.7.3 Informs and advises patients about screening programmes
and community programmes relating to health care and
3.6.1 Applies emergency first aid measures
Examples of Evidence:
Examples of Evidence:
Counsels patients about measures to detect diseases, e.g. cervical
For entry into scope of practice as a pharmacist – holds a current First
screening, mammography, glaucoma checks, mole & skin cancer
Aid Certificate in the NZQA unit standards 6400 – Manage First Aid ,
6401 – Provide First Aid and 6402 – Provide Resuscitation Level 2.
Participates in national programmes and local initiatives, e.g.
Holds a certificate in an approved course to NZ Resuscitation
provides sun-sense information, DARE programmes, safe disposal of
Council Level 2 or NZQA Unit Standard 6402 – Provide resuscitation
medicines campaign (DUMP).
level 2. (Refresher courses must be undertaken every three years to remain current)
3.6.2 Refers first aid emergencies to other health professionals
Communicate effectively
Examples of Evidence:
3.8.1 Establishes rapport with the patient.
Explains referral procedures for specified first aid emergencies, e.g.
Examples of Evidence:
cardiac arrest ➡ ambulance, asthma attack ➡ doctor.
Uses body language to establish empathy & rapport
Identifies symptoms of, & potential for, poisoning from medicine
Uses open & approachable body stance, facial expression
Respects individual & cultural differences
3.6.3 Provides treatment for minor injuries
3.8.2 Uses active listening techniques and asks questions
Examples of Evidence:
relevant to the situation
Range: minor sprains, strains, cuts & grazes, burns, al ergic reactions.
Examples of Evidence:
Uses Standard Precautions when dealing with blood/body fluids, e.g.
Is attentive to patient and asks relevant questions in a logical
wears gloves for handling blood/body fluids; washes hands between
Paraphrases to confirm & clarify information from patient
3.6.4 Advises on the use of bandages and dressings
3.8.3 Tailors information to fit the patient and the situation
Examples of Evidence:
Examples of Evidence:
Explains purpose & use of different dressings/bandages
Adapts information for patient's level of comprehension & avoids
Advises & counsels patients about correct use of bandages/dressings
Uses varied formats (e.g. verbal & written information, physical
Counsel and advise to promote good health and
demonstration, diagrams/pictures, placebo devices) to best fit
3.7.1 Counsels patients about lifestyle changes, which may
3.8.4 Checks patients' understanding
Examples of Evidence:
Examples of Evidence:
Listens, questions & interprets body language to ensure understanding
Counsels patients about measures to promote health & reduce disease,
Gets patient to demonstrate or explain the treatment or advice
e.g. smoking cessation, exercise, healthy diet, moderating alcohol
Asks patient to repeat back information if necessary
intake, sun protection, lifestyle factors related to heart disease, diabetes & osteoporosis.

COMPETENCE STANDARD 4
Apply Management and Organisation Skills
This competence standard covers the organisation and management skills common to all pharmacists. it encompasses the ability to deal with contingencies in the workplace as well as routine work.
RANgE STATEMENT:At this level the pharmacist is responsible for management and organisation of his or her own work and professional duties within the workplace. The pharmacist may work alone or with other pharmacists and, if in a pharmacy, takes responsibility for the work of non-pharmacist staff.
Oversees non-pharmacist staff to ensure they fol ow workplace
Take responsibility in the workplace
guidelines for the handling, storage & disposal of potential y
4.1.1 Organises own work
hazardous materials
Examples of Evidence:
4.3.4 Follows the safety procedures to be implemented in the
Explains own work & responsibilities in workplace
event of an emergency
Examples of Evidence:
Describes examples of pharmacy emergencies
Explains existing workplace safety procedures
Decides what to do, plans to get it done & does it
4.1.2 Takes responsibility for the work of non-pharmacist staff
Examples of Evidence:
Contribute to the management of workplace services
Describes roles & responsibilities of non-pharmacist staff
4.4.1 Contributes to the maintenance and development of
Supervises work of non-pharmacist staff e.g technicians &
workplace procedures and services
Examples of Evidence:
Works with others to prioritise & organise workflow
Works with other staff to develop & amend workplace procedures
4.1.3 Supports the work of colleagues in the workplace
Examples of Evidence:
Contributes ideas for improving services
Describes pharmacist's role & responsibilities in workplace
Works with others to ensure adequate staffing levels
Works in partnership with col eagues in workplace, if applicable, to
If a locum, contributes suggestions for developing workplace
ensure safe practice
4.4.2 Works with others to ensure adequate supplies of stock
Work effectively within the workplace organisation
Examples of Evidence:
4.2.1 Works with the documented procedures and systems
Works within workplace guidelines to order medicines & equipment
Examples of Evidence:
Oversees non-pharmacist staff to ensure they work within
Works within organisation's Standard Operating Procedures (SOPs).
workplace guidelines for ordering medicines & equipment
Uses computer programmes & other systems in workplace
4.4.3 Complies with agreed conditions of employment
4.2.2 Maintains effective working relationships with other staff
Examples of Evidence:
Examples of Evidence:
If an employee, complies with employment conditions agreed with
Works with others to maintain an open & supportive team
employer e.g hours of work
Explains the effects of own actions on other staff
If an employer, complies with employment conditions agreed with
4.2.3 Supports workplace-based training
Examples of Evidence:
Participates in workplace-based training
Communicate effectively
Trains staff in workplace systems & operations
4.5.1 Communicates effectively with other personnel in the
Facilitate a safe working environment
Examples of Evidence:Participates in staff discussions
4.3.1 Complies with legislation relating to occupational health,
welfare and safety
Explains new or changed procedures to staff members
Examples of Evidence:
Maintains constructive dialogue with all staff
Explains own responsibilities under the Health & Safety in
4.5.2 Communicates effectively with representatives from
Employment Act 1992
outside the workplace
4.3.2 Ensures work areas are safe and hygienic
Examples of Evidence:
Examples of Evidence:
If necessary, maintains constructive dialogue with drug company
Takes responsibility for maintaining cleanliness & safety of
representatives, stock & equipment wholesalers & manufacturers &
other health professionals
Ensures work areas comply with Health and Disability Services Pharmacy Services Standard NZS 8134.7
4.3.3 Ensures the safe handling, storage and disposal of
potentially hazardous materials
Examples of Evidence:
Fol ows workplace guidelines for the handling, storage & disposal of
potential y hazardous materials – both pharmaceutical and
workplace chemicals

COMPETENCE STANDARD 5
Research and Provide information
This competence standard covers the role of the pharmacist in providing health-related information to other health professionals, patients and the public. The pharmacist's role includes finding, interpreting, evaluating, compiling, summarising, generating and disseminating information, for the purpose of optimising medicine related health outcomes.
The research component of this standard applies to both applied and practice-based research covering medicines and all areas within pharmacy and health. This includes science, social, cultural, economic and management factors in the health field.
RANgE STATEMENT:The pharmacist's medicine and health care information responsibilities are reactive, in that he/she carries out the tasks described in this standard in response to requests from patients, members of the public and health professionals. The pharmacist accesses and uses standard reference sources to obtain information about medicines or health care and provides accurate information to other health professionals, patients and the public in a manner that is timely and suitable for the receiver.
Common medicines are those listed in the latest edition of the MIMS New Ethicals.
Readily available references are those available from within the pharmacy including current editions of Martindale, MIMS New Ethicals, BNF, Pharmaceutical Schedule, a medical dictionary and web-based sources.
The pharmacist undertakes workplace-based research that provides new personal knowledge and/or facilitates more effective medicine use or workplace management.
use, patient factors, ADRs, interactions & contraindications for
use reference sources to compile medicines and
healthcare information
Provides references to substantiate information
5.1.1 Describes reference sources
5.3.2 Advises about the use of medicines
Examples of Evidence:
Examples of Evidence:
Describes availability & scope of common reference sources
Explains the safe use of medicines, including warnings &
including reference texts and computer databases
precautions & special storage requirements of specific medicines
Explains limitations of available reference sources
5.3.3 Provides medicines and health care information to
5.1.2 Finds information in reference sources
individuals and groups
Examples of Evidence:
Examples of Evidence:
Accesses tertiary medicine information sources e.g. BNF, MIMS
Provides responses to queries from members of the public or other
health professionals
Accesses secondary medicines information sources
If asked, addresses groups of health care professionals, patients or
e.g. Martindale, Medline
members of the public e.g. Asthma Society meeting or a group of
Selects optimal reference sources for situation
diabetes patients
Finds specified information in a timely manner, including information on: patient factors, interactions, precautions & contraindications,
therapeutic efficacy, dosages, dose forms, methods of
Apply research findings in the workplace
administration & side effects
5.4.1 Identifies research opportunities in the workplace
Examples of Evidence:
Identifies the need for research, e.g. identify the need to improve
interpret information about medicines and health care
workflow in the dispensary, cut down clerical cal s to doctors,
5.2.1 Evaluates situation to determine if able to provide
improve use of pharmacy floor space
information to the required level or needs to refer
5.4.2 Gathers information and resolves identified problems
Examples of Evidence
Examples of Evidence:
Responds to enquiries, if within own level of expertise
Gathers information on a workplace/research problem & works to
If necessary, refers enquiry to another health professional e.g
resolve this e.g. produces a regular bul etin to doctors about
specialist medical practitioner, CARM, medicines information centre
5.2.2 Differentiates between information sources regarding
Adopts a questioning approach to problem solving
their reliability
Examples of Evidence:
Recognises differences between peer-reviewed research and
Communicate effectively
promotional material e.g. advertising material
5.5.1 Responds to queries and requests for medicines and health
Explains difference between manufacturers' information (e.g.
Medicines data sheets) & independent editorial-based sources
Examples of Evidence:
(e.g. Martindale)
Listens and interprets information from enquirer e.g. paraphrases to
5.2.3 Compares information from different sources
ensure request is understood
Examples of Evidence:
Asks questions to elicit all the information
Compares information when two reference sources give different
Agrees on time frame for response
advice, and determines what outcome to recommend e.g. significance of drug interactions
5.5.2 Communicates verbal and written information fit for the
Recognises that cultural, economic and political contexts shape
Examples of Evidence:
information from different sources
Avoids technical jargon when talking with patients
5.2.4 Interprets information on behalf of other health
professionals, patients and members of the public
Provides information fit for situation: letters, faxes, emails & verbal y
Examples of Evidence:
by telephone & face-to-face
Relates information to specific situations. patients or requests
5.5.3 Communicates effectively with other health professionals
Relates information found to the situation e.g. gives patient-specific
and patients
answer if appropriate
Examples of Evidence:Communicates clearly with individual health professionals to pass
Provide information about medicines use and
Explains information clearly to patients & if necessary uses
health care.
additional aids e.g. language cards,
5.3.1 Explains the pharmacology and therapeutic use of
common medicines
Examples of Evidence:
Either from memory or reference sources, explains therapeutic
COMPETENCE STANDARD 6
Dispense Medicines
This competence standard covers the supply of Prescription Medicines and Pharmacist Only Medicines, including extemporaneously compounded products. The dispensing process includes all actions and responsibilities of the pharmacist from receipt of a prescription, medicine order or patient request through to counsel ing the patient about the use of the medicine.
RANgE STATEMENT:The pharmacist processes all prescriptions and medicine orders (including Practitioners Supply Orders and Bulk Supply Orders) received in written form or by fax, telephone or computer. He or she dispenses Pharmacist Only Medicines and all categories of Prescription Medicines.
6.3.2 Explains the therapeutic use of prescribed medicines
Validate prescriptions
Examples of Evidence:
6.1.1 Checks prescriptions are complete, legal and authentic
Explains pharmacology of each medicine, using reference if
Examples of Evidence:
Identifies whether or not prescriptions are complete &/or legal.
6.3.3 Interprets prescription instructions
Checks compliance with Regs 41 & 42, Med Regs 1984
Examples of Evidence:Interprets abbreviations of dosage & dose forms
Identifies possible fraudulent prescriptions
Interprets the prescriber's intention
6.1.2 Obtains information needed to make prescriptions
complete and correct
Examples of Evidence:
Review patients' medicines in relation to their histories
Obtains information from prescriber, patient & other sources as
6.4.1 Accesses patient medicine records
defined in Reg 41 Med Regs 1984
Examples of Evidence:
Checks with prescriber if instructions/prescription details unclear
Accesses computerised/written records held in own pharmacy.
6.1.3 Annotates prescriptions
Accesses medicine records held in other pharmacies or by other
Examples of Evidence:
Annotations as defined in DHB's Procedures Manual e.g. ensures
6.4.2 Verifies details of patient medicine records with patients,
annotations are distinguishable from what doctor has written
their caregivers or other health professionals
Annotates according to hospital pharmacy procedures (e.g. SOPs)
Examples of Evidence:
6.1.4 Verifies prescriptions received by fax, telephone or email
Ensures records reflect actual medicine intake of patient
Examples of Evidence:
6.4.3 Detects medicine problems from individual patients'
Complies with legal requirements: Reg 40 Meds Regs 1984, Reg 34
Misuse of Drugs Regs 1977
Examples of Evidence:
Fol ows workplace practices & professional conventions when
Identifies omissions, dosage changes, inappropriate use, ADRs,
verifying prescriptions
non-compliance, prolonged use, misuse or abuse, interactions, incompatibilities, contraindications
6.4.4 Identifies patient factors likely to affect the efficacy or
Assess Prescriptions
safety of specified medicines
6.2.1 Determines whether individual prescriptions should be
Examples of Evidence:
e.g. age, weight, pregnancy, breast-feeding, disabilities, al ergies,
Examples of Evidence:
risk factors, other medicines
Recognises problem prescriptions, e.g. incorrect/inappropriate prescribing
6.2.2 Follows workplace dispensing criteria when dispensing a
Decide what is safe and appropriate to dispense
6.5.1 Confirms that each selected medicine is suitable for the
Examples of Evidence:
Checks medicine funding status in the Pharmaceutical Schedule
Examples of Evidence:
Checks if medicine fulfils hospital dispensing criteria
Confirms that dosage, route of administration & duration of therapy
6.2.3 Prioritises prescriptions
Examples of Evidence:
Identifies possible interactions or incompatibilities
Checks urgency needed to dispense each prescription
6.5.2 Addresses factors likely to affect patient compliance
Organises prescriptions in order of priority
Examples of Evidence:
6.2.4 Determines the stock availability of prescribed medicines
Identifies factors likely to affect patient compliance & determines
Examples of Evidence:
ways to deal with these, e.g. tablet use in children, breaking tablets
Checks medicine available in pharmacy
Selects compliance aids, e.g. asthma spacers; tablet cutter; single
Determines where & when the medicine can be obtained if not
available, e.g. wholesaler or another pharmacy
6.5.3 Applies all patient information to dispensing decisions
Examples of Evidence:
Based on all information gathered decides whether can dispense or
interpret prescriptions
need to contact prescriber or patient
6.3.1 Identifies prescribed medicines
6.5.4 Contacts prescriber to recommend medicine, dose or dose
Examples of Evidence:
Identifies trade, generic & common names for prescribed medicines
Examples of Evidence:
Uses reference sources to find medicine names
Contacts prescriber and documents discussion outcomes, e.g. annotates on prescription, records in interventions book
COMPETENCE STANDARD 6
Dispense Medicines
Fil prescriptions
Maintain dispensing records
6.6.1 Obtains prescribed medicines
6.8.1 Maintains patient records
Examples of Evidence:
Examples of Evidence:
Locates stock in pharmacy
Maintains patient medicine records, including patients'
Obtains stock from other sources, if not available in pharmacy
administrative information & details of prescribed medicines, e.g. repeats al owed, prescriber details.
6.6.2 Maintains a logical, safe and disciplined dispensing
6.8.2 Maintains medicine records
Examples of Evidence:
Examples of Evidence:
Selects correct product, dose form & quantity for each prescribed
Maintains medicine records, e.g. emergency supply, Pharmacist Only
Medicines, Control ed Drugs, unregistered medicines
Dispenses off prescription, not label
6.8.3 Fulfils legal requirements and professional conventions
regarding maintenance of records
6.6.3 Fulfils the conditions & requirements specified in the
Examples of Evidence:
relevant legislation
Examples of Evidence:
Complies with legal requirements: Reg 57 Meds Regs 1984, Health (Retention of Information) Regs 1996, Sect 18 Meds Act 1981
Complies with legal requirements of Misuse of Drugs Regs and Medicines Regs
Maintains dispensing records of patients on IMMP & forwards to CARM in Dunedin every 4 months.
6.6.4 Provides emergency supplies of prescription medicines
Examples of Evidence:
Determines need for an emergency supply
Minimise dispensing errors
Complies with legal requirements & professional conventions
6.9.1 Explains the general potential for errors in the dispensing
regarding dispensing emergency supplies of prescription medicines
(Reg 44 Meds Regs 1984)
Examples of Evidence:
Identifies steps in dispensing procedure that are potential problem
Package medicines to optimise safety and compliance
areasIdentifies actions to minimise actual/potential problem areas
6.7.1 Packages medicines in suitable containers
Examples of Evidence:
6.9.2 Acts to minimise the effects of his/her dispensing errors
Selects optimal container for the medicine, e.g. light-protective
Examples of Evidence:
Identifies potential/actual errors in own dispensing
Selects optimal container for the patient, e.g. child resistant
Acts to minimise effect on patient, e.g. contacts patient, contacts
closures, single dose packaging
prescriber, supplies correct medicine.
6.7.2 Produces comprehensible and complete labels for
Documents own dispensing errors & actions undertaken to minimise
Examples of Evidence:
Complies with workplace procedures for documenting dispensing
Includes all information specified by prescriber & necessary
6.9.3 Rectifies dispensing errors immediately
Attaches labels securely without obscuring relevant information, eg
Examples of Evidence:
Alters own dispensing procedure to prevent recurrence of previous
Fulfils legal requirements & professional conventions re labelling of
medicines (Reg 23 Meds Regs 1984)Adapts labelling to meet patients' needs, e.g. poor sight
Counsel patients about their medicines
Communicate effectively
6.10.1 Ensures patient receives the correct medicine
6.11.1 Communicates effectively with prescribers
Examples of Evidence:
Examples of Evidence:
Check patient details, e.g. name & address.
Uses questioning and listening skil s to elicit information
6.10.2 Ascertains patients' understanding of their medicines
Clearly communicates proposed prescription changes and
Examples of Evidence:
Talks with/questions patients to find out their understanding of
6.11.2 Uses language and non-verbal communication to suit the
medicines purpose & compliance
6.10.3 Informs and advises about medicines
Examples of Evidence:
Examples of Evidence:
Talks to patients in lay terms, avoiding technical jargon
Explains indications for use & benefits of medicines
Uses gestures, voice tone, stance, & facial expressions to suit
Advises on dosage, storage, alterations in formulation/packaging,
situation & patient
different brands supplied on generic-request medicines
6.11.3 Tailors information to suit the patient
Advises about precautions & adverse effects without alarming
Examples of Evidence:
Adapts information to suit patient's comprehension level
Advises on frequency; relationship to food & duration of therapy
Uses varied formats to provide information in a way that suits
Provides written information, e.g. pamphlets, self care cards
patients' needs, e.g. verbal, physical demonstration, written, pictorial, models & placebo devices
6.10.4 Demonstrates the correct method of administering
6.11.4 Asks relevant questions
Examples of Evidence:
Examples of Evidence Guide:
Provides compliance aids if necessary, e.g. asthma spacers; tablet
Uses questions to check patient understands advice & counselling
Listens attentively to response
Provides verbal & written information & physical demonstrations to explain special techniques for using:– inhalers, ear, nose & eye drops, nasal & oral sprays, suppositories
– creams, lotions, patches & dressings– cutting/dissolving tablets
6.10.5 Check patients' understanding of the advice and
counselling
Examples of Evidence:
Listens attentively or questions patient to determine understanding
Gets patient to repeat information to ensure understanding
6.10.6 On request informs and advises patients about their
conditions and diseases
Examples of Evidence:
Ascertains patients' understanding of their conditions/diseases
Provides verbal & written advice, e.g. pamphlets, self care cards
COMPETENCE STANDARD 7
Prepare Pharmaceutical Products
This competence standard covers the preparation of pharmaceutical products in community and hospital pharmacies.
RANgE STATEMENT:The pharmacist prepares small quantities of non-sterile products and/or sterile products, including creams, ointments, suppositories, mixtures, suspensions, solutions and/or TPNs, eye drops, injections and subcutaneous syringes according to the Health and Disability Services Pharmacy Services Standard NZS 8134.7 Standards 5, 6 and 7.
The pharmacist explains the principles of aseptic dispensing and recognises situations in which it is necessary.
Explains the role of TPN components and the balance required
Explain compounding principles and procedures
7.1.1 Explains the principles of compounding
7.3.4 Modifies formulations within existing guidelines
Examples of Evidence:
Examples of Evidence:
Explains use of techniques & equipment, e.g. grinding, mixing,
Modifies formulations to ensure product is stable & suitable for
heating, order of addition of ingredients, balances & weights.
Describes role of buffers, preservatives, antioxidants & suspending
Fol ows manufactures' guidelines, or appropriate reference source,
for dilution of solutions, suspensions & ointments
Explains the principles of sterile compounding, e.g. no-touch
Explains the limits of modifications that can be made to formulations,
technique, use of laminar-flow cabinets.
e.g. addition of electrolytes to TPNs, additions to creams
7.1.2 Explains the principles of medicine stability
Examples of Evidence:
Compound pharmaceutical products
Explains effects of moisture, oxygen, sunlight, temperature & micro-organisms on stability & clinical effectiveness of finished
7.4.1 Prepares worksheet and calculations and labels
Examples of Evidence:Calculates quantities of ingredients & end product to 100%
accuracy, and documents this
Recognises under what conditions extemporaneously
Produces clear labels for end products, including full patient
prepared products can be prepared
instructions, expiry dates, storage information and any
7.2.1 Differentiates between prescriptions that require aseptic
supplementary advisory labels
dispensing and those that don't
7.4.2 Obtains stock and equipment and prepares work area
Examples of Evidence:
Examples of Evidence:
Identifies dosage forms that must be prepared with aseptic
Obtains correct form & strength of ingredients needed for product
techniques in a clean room environment e.g. those instil ed, injected
Checks each ingredient to ensure it is fit to use, e.g. checks expiry
or used to irrigate sterile body cavities
date, signs of degradation, stored correctly (temperature & protection
Does not attempt to make eyedrops in normal dispensary area
from light & moisture), stability if packaging already opened.
7.2.2 Recognises extemporaneously prepared products that
Checks ingredient is pharmaceutical grade.
must be prepared under special conditions to minimise
Ensures equipment and work area are appropriate, clean & tidy
e.g. ointment slab cleaned; positive pressure areas maintained in
Examples of Evidence:
Identifies cytotoxic preparations that must be prepared in a
Ensures personnel are appropriately prepared for aseptic production,
chemotherapy isolator or preparation unit.
e.g. handwashing, appropriate clothing
Identifies potential y harmful ingredients and products e.g.
7.4.3 Compounds pharmaceutical products applying suitable
podophyl in, and ensures they are dealt with safely, including
compounding techniques and principles
storage and transport
Examples of Evidence:
Uses appropriate compounding technique to prepare product
Determines appropriate formulation
Weighs or measures correct quantity of ingredients
7.3.1 Selects formulations
Fol ows professional conventions & formulation principles when
Examples of Evidence:
Selects correct formulations for specified products
Uses aseptic, no-touch technique for sterile preparations
Accesses formulations used in workplace or uses reference sources
7.4.4 Examines final product for particulate contamination and
7.3.2 Interprets formulations
Examples of Evidence :
Examples of Evidence:
Interprets common terminology & abbreviations, e.g. ingredients,
Undertakes a visual final check for product, e.g. checks for particulate
instructions, dose forms, quantities
contamination, uniform mixing, aesthetical y pleasing products
Identifies trade, generic & common names of ingredients
Complies with workplace quality control procedures for assessment of final product e.g. assays of active ingredients, sterility checks
Identifies problem formulations, e.g. incorrect proportions, drug instability, vehicle instabilities, inaccuracies, precipitations, syringe
7.4.5 Complies with Health and Disability Services Pharmacy
Services Standard NZS 8134.7 and workplace practices
for the compounding and preparation of pharmaceutical
7.3.3 Explains the purpose of ingredients within formulations
Examples of Evidence:
Examples of Evidence:
Explains what each ingredient is – stabilisers, therapeutic agents,
Complies with rules of schedule or formulary, relevant for the product
preservatives, vehicles, diluents, antioxidants, suspending agents, flavouring agents e.g. methylcellulose is a suspending agent.
Complies with Code of GMP, Quality Standards for Pharmacy in NZ & workplace SOP's
COMPETENCE STANDARD 7
Prepare Pharmaceutical Products
7.4.6 Packs and labels compounded products to optimise safety
Communicate effectively
Examples of Evidence:
7.5.1 Writes in clear English
Packs each compounded product in container suitable for type,
Examples of Evidence:
quantity, intended use & storage requirements of product, e.g.
Produces all labels, records & instructions in clear legible English
protected from light & moisture, container suited to product & use,
with no spelling or grammatical errors
bottle with dropper dispenser for ear drops.
7.5.2 Communicates effectively with prescribers, health
Attaches labels securely, without obscuring relevant information,
professionals, care givers and patients
e.g. graduations on syringes, poison bottle ribs
Examples of Evidence:
7.4.7 Ensures optimal storage of ingredients and compounded
Uses questioning and listening skil s to elicit information
Clearly communicates proposed formulation requirements and
Examples of Evidence:
changes with prescriber
Complies with optimal storage conditions regarding: temperature, light, moisture, type of container, transport of product
Communicates effectively with end user of product about the use of the product, e.g. TPN administration, eye drop use
7.4.8 Cleans and maintains compounding equipment
Examples of Evidence:Cleans all equipment after useChecks & maintains equipment according to manufacturers' instructions & workplace SOP'sEnsures aseptic preparation areas are monitored, serviced and cleaned regularly
7.4.9 Completes documentation and records
Examples of Evidence:Completes batch sheets, worksheets & records accurately & legiblyCompletes & verifies worksheets & batch sheets & files documentation according to current legislation, codes, standards & workplace practices e.g. Control ed Drug Register.
Ensures an authorised person verifies all work.
PHARMACY COuNCil MEDiCiNES
MANAgEMENT COMPETENCE FRAMEWORk
Since 2006 the Council has had in place a competence framework for pharmacists providing medicines management services. in relation to the profession of pharmacy the Council defines medicines management as a range of patient-centred services that improves medicines-related health outcomes. These services are in addition to the existing dispensing pharmacy services.
The Council competence framework outlines the four levels of medicines management services and these are aligned with the Medicine Review Services in the DHBNZ National Framework for Pharmacist Services. Detailed service descriptions and specifications can be found in the DHBNZ National Framework document.
The competence framework (see figure below) recognises the relationship between the level of competency (knowledge, skills and attributes) required and the complexity of medicines management related issues. A pharmacist requires additional competencies as they move across the range of medicines management services i.e. from level A to level D.
While four levels of medicines management services can be provided within the Pharmacist scope of practice, additional education and training is required for the provision of level B, C and D medicines management services. The Pharmacist Prescriber scope of practice will be a separate scope of practice, and pharmacists will be required to meet separate competencies and qualifications to register in this separate scope.
E.g. Comprehensive Medicines Management
E.g. Medicines Therapy Assessment
E.g. Medicines Use Review
plexity o
Pharmacy Council of NZ Definition of
Medicines Management:
A range of patient-centred services that improve
medicines-related health outcomes
Competencies Required (Skills, knowledge,attitudes)
Source: http://www.cobef.org.br/arquivos/04%20-%20Competence%20Standards%20for%20New%20Zeland.pdf
Sustainable Public Procurement-fiche: advanced 1) Subject matter Indoor furniture produced with environmentally friendly materials and processes. "For <….> (name of the public authority), the care for the environment and social aspects is important. It is stated in her <strategic policies>, <mission>, <vision>, <procurement policy>, …" 2) Exclusion criteria Non compliance with environmental and social legislation, which has been the subject of a final judgment or a decision having equivalent effect, may be considered an offence concerning the professional conduct of the economic operator concerned or grave misconduct, permitting to exclude the party concerned from competing for the contract Ref: Art. 53 and 54 of Directive 2004/17/EC and Art. 45 of Directive 2004/18/EC 3) Technical capacity / 4)) Technical specifications
Visit http://tinyurl.com/DMEandDR for online testing and instant CME certificate Current Management of Diabetic Macular Edemaand Diabetic Retinopathy Clinical Cases Original Release: January 2, 2015 Last Review: December 9, 2014 Expiration: January 31, 2016 This continuing medical education activity is jointly provided