The effectiveness of farabloc technology with mirror therapy in reducing phantom limb pain in individuals with an acute lower extremity vascular amputation
The effectiveness of Farabloc technology with Mirror Therapy in reducing phantom limb pain in
individuals with a unilateral lower extremity vascular amputation
Director of Thesis: Anne Dickerson
Major Department: Occupational Therapy, East Carolina University
Abstract
Objective: The objective of this study was to investigate the effectiveness of combining two
interventions, Farabloc technology to eliminate electromagnetic fields and Mirror Therapy to
assist in the sensory cortex reorganization, to decrease or eliminate phantom limb pain in
vascular amputees.
Methods:Fourteen older adults with a unilateral vascular amputation participated in the study.
Nine individuals started the intervention within 48 hours of surgery and were compared to five
individuals who were approximately 18 months post-surgery. Measures of residual limb edema
and temperature, phantom limb pain variables, activities of daily living and quality of life
interference were completed pre and post intervention and 4 weeks after the end of therapy.
Results:All fourteen subjects reported an overall decrease in phantom limb pain using a visual
analogue scale. For the acute group, wound healing and edema reduction decreased time to
prosthetic fitting from 12 weeks to eight weeks, significant for improving functional ambulation,
return to work and decreasing wheelchair mobility dependence. Activities of daily living and
quality of life variables both showed significant differences.
Conclusion: Use of this combined treatment protocol shows promising results for not only acute
amputee intervention, but also improved perception of pain and improved quality of life for
amputees with chronic phantom limb pain. Implications for activities of daily living and quality
of life are discussed.
The effectiveness of Farabloc technology with Mirror Therapy in reducing phantom limb pain in
individuals with a unilateral lower extremity vascular amputation
Presented to the Faculty of the Department of Occupational Therapy
East Carolina University
In Partial Fulfillment of the Requirements for the Degree
Post-professional Master's in Occupational Therapy
The effectiveness of Farabloc technology with Mirror Therapy in reducing phantom limb pain in
individuals with a unilateral lower extremity vascular amputation
APPROVED BY: DIRECTOR OF DISSERTATION/THESIS: _
Anne Dickerson, PhD, OTR, FAOTA
COMMITTEE MEMBER: _
Leonard Trujillo, PhD, OTR/L, FAOTA
COMMITTEE MEMBER: _
CHAIR OF THE DEPARTMENT OF OCCUPATIONAL THERAPY _
Leonard Trujillo, PhD, OTR/L, FAOTA
DEAN OF THE GRADUATE SCHOOL
Dr. Paul Gemperline, PhD
Table of Contents
CHAPTER 2: Literature Review……………………………………………….
Summary and conclusions …………………………………………….
APPENDIX A: Institutional Review Board Approval…………………………
APPENDIX B: Prosthesis Evaluation Questionnaire………………………….
APPENDIX C: Daily Log…………………………………………………….
APPENDIX D: Brief Pain Inventory - short form…………………………….
APPENDIX E: Hubbard Scientific 6083 Liquid Crystal Temperature Strip….
APPENDIX F: Log of Continuity Tester Measurements………………………
APPENDIX G: Instructions to Therapists…………………………………….
APPENDIX H: Exercise Protocol for Mirror Therapy Exercises…………….
CHAPTER 1: Introduction
Phantom limb pain (PLP) is defined as painful sensations perceived in the missing
portion of the amputated limb (Davis, 1993). It can be an extremely debilitating and complicated
phenomenon limiting participation in daily life activities throughout the life of an individual with
an amputation. Due to varied etiology, a variety of different treatment options have been
explored to attempt to manage PLP. Yet, it continues to remain a challenging and disabling
condition which continues to plague many amputees and at best, is difficult to treat.
The purpose of this study was to explore the effect of combining two therapies, Farabloc
technology with Mirror Therapy, to explore the effect that this combined treatment protocol
would have on PLP for acute compared to chronic, unilateral, lower extremity vascular above or
below knee amputees.
According to the World Health Organization (WHO), "Electromagnetic fields (EMF) can
affect the nervous systems of people exposed to them, resulting in adverse health consequences
such as nerve stimulation" , whereas, "The absence of EMF can reduce persons chronic pain"
(Nixdorf, 2012, p 1.). Farabloc technology (Farabloc Development Corporation, 2012)uses a
fabric that is woven using 9.5% steel wire fibers consisting of iron, nickel, chromium and nylon,
which has significant shielding effects on high frequency EMF (greater than 1MHz) (Bach &
Clement, 2007). This washable fabric has an appearance similar to linen (Bach & Clement,
2007) and can be tailored into an amputee limb cover that is worn over the stump/ residual limb.
It has been promoted and has been demonstrated to have a favorable effect on PLP in several
studies (Bach, & Clement, 2007; Conine, Hershler, Alexander, & Crisp, 1993; Clement &
Taunton, 2001; Halbert, Crotty, & Cameron, 2002; Zhang, Clement, & Taunton, 2000).
Mirror Therapy (Ramachandran, 1996) uses a mirror placed between the amputated and
non-amputated limb, in which the non-amputated limb is observed while performing bilateral
synchronous exercises, such that it appears that both limbs are intact. "The patient sits with a
mirror facing the remaining leg, moves the remaining leg and watches the reflection in the
mirror, so that it appears that both the good and the amputated leg are moving" (Helm, 2008).
Mirror Therapy has been shown to significantly reduce PLP in individuals with an amputation
(Chan et al., 2007; Flor, 2008; MacLachlan, McDonald, &Waloch, 2004; Ramachandran, 1996).
By combining Farabloc technology and Mirror Therapy, this study investigated whether
PLP experienced by acute above/below knee amputees could be prevented or reduced in
frequency, intensity or duration compared to chronic amputees. Farabloc and Mirror Therapy
have been researched independently. This study is unique, as it utilizes the findings of the
research done in these areas, as a combined intervention strategy.
As a primary provider of therapeutic interventions, occupational therapists' focus would
be on an individual's functional participation in activities of everyday life. Living with chronic
pain, such as PLP can be disabling and severely limit one's quality of life as well as one's ability
to independently participate in everyday life tasks (Harrison, 2011). To maximize participation,
occupational therapists need a treatment protocol to treat the effects of PLP in amputee clients.
The objective of this study is to establish a viable treatment intervention protocol for this
CHAPTER 2: Literature Review
Phantom Limb Pain
More than 100,000 lower-limb amputations are performed each year in the United States, with
many of these individuals facing secondary disabling pain conditions (Harness &Pinzur, 2001).
"The severity of the neurological injury associated with an amputation overrides all the other risk
factors that influence the development of chronic pain syndromes" (Byrne, 2011, p. 1).
Phantom limb pain (PLP) is defined as "painful sensations perceived in the
missing portion of the amputated limb" (Davis, 1993, p. 79).
Phantom limb sensations are "non-painful sensations perceived as emanating
from the portion of the amputated limb that is missing" (Melzack, 1992, p. 121).
Residual limb pain is perceived as "originating in the residual portion of the limb
(i.e., the stump) (Davis, 1993, p. 79).
Phantom limb sensations remain a substantial and unpredictable problem in the amputee
population (Ottaviani, Robert, Huh, & Jaffe, 2009). The sensations are experienced by up to 98%
of all patients with limb amputations, and may be experienced as a warm or cold feeling, an
itching sensation, pressure, and even a sense of position, shortly after losing a limb
(Ramachandran &Hirstein, 1998). The focus in this study was on phantom limb pain.
Origins of Amputations. Amputations result from three major sources: congenital
malformations, trauma and from diseases such as diabetes, peripheral vascular disease and
neoplasms (Nikolajsen & Jensen, 2001). Improvised explosive devices used in Iraq and
Afghanistan have led to an increased incidence in U.S. veterans returning home with limb loss
and subsequently increased phantom limb pain (PLP). A need for a simple, effective treatment
for this debilitating disorder is more important than ever (Leskowitz, 2009).
Vascular Disease in the United States. Diabetes and resulting peripheral vascular
disease is on the rise in the United States. In 2010, 8.3 percent or 25.8 million American adults
had diabetes. Seven million of these are undiagnosed and 18.8 million people have been
diagnosed with diabetes. According to the Centers for Disease Control and Prevention, diabetes
is the seventh leading cause of death in the United States. It is also a leading cause for other
chronic complications such as blindness, kidney failure, and lower extremity amputations
(Prevention, 2011).
In 2010, North Carolina ranked 13th highest for adults diabetes prevalence in the nation.
The national average was 8.3 percent, and the prevalence in North Carolina was 9.8 percent. In
North Carolina, 643,000 adults had diagnosed diabetes and another 376,000 adults have pre -
diabetes. Diabetes is more prevalent in ethnic minorities who live in the Northeastern and
Southeastern portions of the state, with the highest prevalence seen in African Americans at 15.6
percent. One in every five African American adults, age 65 and older, has diabetes in North
Carolina (North Carolina Diabetes Prevention and Control Program [NC DPH Diabetes], n.d.).
The Amputee Coalition of America statistics report that dysvascular-related amputations account
for eighty-two percent of limb loss, and lower-limb amputations account for ninety-seven
percent of all amputations ("Amputee statistics by cause. Limb loss in the United States", 2008).
History of phantom limb pain. Sensation post-amputation was first described by
Ambroise Pare´ (1510 – 1590). He was a French military surgeon, who observed that many
patients complained of severe pain in the missing limb after an amputation. Pare´ was the first to
characterize post-amputation syndrome and he proposed several different models to explain this
post-amputation pain (Keil, 1990).
Other individuals were instrumental in providing important detailed descriptions of this
post-amputation pain phenomenon throughout history: Charles Bell - 1830, Magendie - 1833,
Rhone - 1842, Gueniot – 1861 (Nikolajsen & Jensen, 2001). A civil war physician, Silas Weir
Mitchell in 1871, coined the phrase "phantom limb" to describe this phenomenon and noted that
PLP is often resistant to standard medical and neurosurgical treatments for pain (Mitchell, 1871).
Almost all amputees experience phantom sensations after an amputation (whether these
are painful or not). The non-painful sensations don't often pose a clinical problem and may
provide the necessary proprioceptive feedback for these amputees to be able to use a prosthetic
limb in a functional manner. In amputees with PLP however, the area distal to the residual limb
becomes the site of severe pain and debility and once established this pain may be exceedingly
difficult to eradicate or treat (Nikolajsen & Jensen, 2001). In the majority of cases, PLP onset is
often experienced immediately upon awakening from anesthesia (Weeks & Tsao, 2010).
PLP Prevalence. There is a wide variety about the consensus of the prevalence of PLP,
with rates ranging from 0.5% to 100% of persons with amputations. However using improved
methods, more recent studies, have suggested that 90% of individuals, undergoing limb
amputations will experience some degree of PLP (Chan et al., 2007).
In 75% of cases, PLP occurs within the first few days after an amputation (Nikolajsen &
Jensen, 2001). PLP is described as shooting, stabbing, squeezing, throbbing or burning. It is
primarily localized in the distal parts of the missing limb such as the toes, instep, top of foot and
ankle in lower limb amputees (Nikolajsen, Ilkjaer, Kroner, Christensen, & Jensen, 1997).
In an important study by Sherman, Sherman and Parker, of 2694 amputees, 51%
experienced phantom limb pain "severe" enough to hinder lifestyle on more than 6 days per
month. Twenty-seven percent of this sample experienced PLP more than 15 hours each day and a
further 21% reported daily pain over a 10 – 14 hour period. Sherman and his colleagues also
found that 44% of amputees reported that their PLP had not diminished over a 30-year period
(Sherman, Sherman, & Parker, 1984). This indicates that PLP is a significant, ongoing problem
requiring intervention. Because PLP is such a persistent problem that interferes with daily
function, it is an important problem for occupational therapists to address in order to maximize
functional independence in their clients.
In a national survey of 914 persons with limb loss chronic, persistent pain was identified
as leading to limitations in function, both physically and psychosocially (Ephraim, Wegener,
Mackenzie, Dillingham, &Pezzin, 2005). This study noted that it is often not the underlying
condition (i.e., the amputation) that primarily impairs the individual's function, but rather the
chronic pain that they experience. According to Mohamad, Ebrahimzadeh and Harris, 2009,
amputees can have significant persistent symptoms that negatively influence their function, for
as long as two decades post amputation. Early prosthesis use has been shown to reduce PLP by
reorganizing the cortical patterns (Lotze, Grodd, Birbaumer, Erb, Huse, & Flor, 1999).
Theories of the origin of PLP. There are a variety of theories to explain PLP. In 1943,
Livingston proposed the idea of "closed, self-sustaining, reverberating circuits" which are set up
by chronic peripheral irritation or by the release of spinal cord cells from inhibitory control
through the loss of afferent input. When these abnormal impulses reach the brain, they are
experienced as painful. Furthermore, once these circuits are established, surgical removal of the
peripheral source has no effect on them and, therefore, will not abolish the pain (Hill, 1999).
Melzack proposed the idea of the neuromatrix, a "network of neurons that extends
throughout widespread areas of the brain, composing the anatomical substrate of the physical
self" (Melzack, 1990, p. 91). Melzack believed that the primary components are genetically
prewired, and experiences "add or delete, strengthen or weaken existing synapses" (Melzack,
1992, p. 124). His theory proposes that abnormal input to the neuromatrix following amputation
alters the pattern generated by the neuromatrix and results in output which is experienced as a
painful phantom. Abnormal input can either result from lack of normal sensory input following
amputation or from high levels of input caused by excessive firing in damaged nerves. Following
amputation, the neuromatrix no longer receives signals from the periphery that the limb is
moving. The output from the neuromatrix includes the basic neuro-signature which has been
modulated to include strong messages for the limb to move. This excessive output results in the
report of a cramping type of pain, and an EMG spike of activity associated with this aspect of
PLP (Hill, 1999).
Harris believed that a distorted cortical representation of a limb can result in
discrepancies between motor intention, proprioception and vision, which lead to the affective
sensation of pain (Harris, 1999), while Arnstein described an active sprouting of new neurons
after an amputation, which leads to cortical remapping (Arnstein, 1997). Karl et al. noted a direct
association between, greater neural plasticity and an increase in PLP (Karl, Birbaumer,
Lutzenberger, Cohen, &Flor, 2001). Illusory body experiences, relate in some way to the re-
mapping of the somatosensory cortex when the inputs from an amputated areas cease, allowing
migration of neighboring somatosensory receptions sites into these "vacant areas"( Flor et al.,
1995; Halligan, Zeman, & Berger, 1999; MacLachlan, McDonald, &Waloch, 2004). According
to Manchikanti and Singh (2004) "the etiology and pathophysiological mechanisms of phantom
pain are not clearly defined. Peripheral and central neuronal mechanisms are both likely to
occur" (p.366). There are a series of mechanisms that are involved in generating PLP which
include the peripheral nerves, spinal cord and brain. The stimulation occurs initially in the
periphery, which subsequently stimulates the spinal cord neurons, which in turn recruit cortical
brain structures. The brain structures may be responsible for the sensation that characterizes
certain PLP sensations (Nikolajsen & Jensen, 2001). Strange and sometimes painful phantom
limb sensations can result from loss of afference to the brain (Bultitude&Rafal, 2009).
Based on these theories, early treatment to prevent or interrupt these pain circuits is
essential in treating PLP because once these pathways are established they appear to be more
difficult to abolish. The question remains whether by preventing these painful neural pathways
from becoming established, PLP can be diminished or prevented altogether.
Neurological mechanisms involved in PLP. The neurological mechanisms underlying
PLP have not been completely clarified. However, there is evidence of peripheral, spinal and
central contributions. "It is likely that the initiating events for PLP, phantom limb sensation and
stump pain start in the periphery, which generates a chain of events at the spinal and central
nervous system level" (Chapman, 2011).
Peripheral factors. Peripheral factors indicate that PLP is significantly more frequent in
those amputees with long-term pain, than those without persistent pain (Nikolajsen & Jensen,
2001). Pre-amputation pain has been thought to create a permanent imprint on the dorsal horn
and in the central nervous system pain processing system (Morley-Forster, 2009). After nerves
are cut in surgery, the formations of amputation neuromas frequently result. These masses
develop in nerve tissue in a residual limb due to abnormal regrowth of the severed nerves. These
neuromas show spontaneous and abnormal activity with mechanical or chemical stimulation and
are assumed to be the result of a novel expression or upregulation of sodium channels
(Nikolajsen & Jensen, 2001). The amputated nerves within the neuroma are surrounded by
irregularly sized sprouts that are not myelinated (Yuh, Fisher, Shields, &Ehrhardt, 1992). With
mechanical or neurochemical stimulation, spontaneous and abnormal evoked activity is observed
in nerve-end neuromas (Devor& Seltzer, 1999).
Dorsal root ganglion cells also undergo changes after nerves are completely cut. These
cell bodies show similar abnormal activity and increased sensitivity to mechanical and
neurochemical stimulation and switch from one sodium channel type to another (Waxman,
1999). From animal studies it has been shown that the sympathetic nervous system may also
generate, and maintain PLP (Devor, Janig, &Michaelis, 1994).
Spinal plasticity. Spinal level factors involved in PLP are primarily due to
deafferentation. These nerves receding from the amputated site are the result of the loss of large
myelinated A-afferent nerve fiber input ("fast-pricking pain") in the dorsal horn cells with an
unopposed unmyelinated C-fiber input ("slow-burning pain")(American Academy of Orthotics
and Prosthetics, 2005). After nerve injury, there is an increase in excitability of the spinal cord
neurons. C-fibres and Aδ-afferents gain access to secondary pain signaling neurons. Experiments
have found that the residual limb is much more sensitive to stimuli than that of the same region
on the opposite limb. Sensitization of the dorsal horn neurons is mediated by release of
glutamate. Glutamate is an excitatory neurotransmitter amino acid and tachykinins which are
agents that act at the various neurokinin receptors. This process may manifest as mechanical
hyperalgesia which is an increased sensitivity to pain, and expansion of peripheral receptive
fields (Doubell, Mannion, & Woolf, 1999).The use of N-methyl-D-aspartate (NMDA) receptor
blockade for relief of PLP supports the theory of central sensitization by peripheral nerve injury.
N-methyl-D-aspartate (NMDA antagonist) blocks the glutamine receptors in the central nervous
system. Glutamine is an excitatory neurotransmitter which is thought to activate the central
nervous system after noxious stimuli (American Academy of Orthotics and Prosthetics, 2005).
A recent study showed that the homunculus may actually stay intact after amputation and
perhaps the remapping occurs at the levels of the spinal motor neurons (MacIver, Lloyd, Kelly,
Roberts, &Nurmikko, 2008).
Cerebral reorganization. In adult monkeys, following amputation and deafferentation,
there is a reorganization of the primary somatosensory cortex, subcortex and thalamus
(Nikolajsen & Jensen, 2001). In humans, subcortical level changes, an unusually large thalamic
stump representation and a similar reorganization has been observed. This is particularly true in
individuals with PLP (Davis et al., 1998). "Somatosensory cortex reorganization has been
concluded to be at least as important as events in the periphery" (Morley-Forster, 2009).
Reduction in grey matter is found within the thalamus in amputees contralateral to side of
amputation (Draganski et al., 2006). A linear relationship between pain and degree of
reorganization has been observed using magnetoencephalographic techniques (Flor et al., 1998).
During early studies, Melzack proposed that the reticular activating system plays an important
role in PLP (Melzack, 1971). He proposed that when peripheral fibers are destroyed, thereby
reducing input, inhibition is decreased and synchronous, self-sustaining activity develops at all
neural levels. Thus, lack of input from the periphery following amputation will result in
disinhibition not only at the spinal level, but also at the cortical level, which has been confirmed
by more recent research (Hill, 1999). Individuals with an amputation are therefore at risk of
hyperstimulation of these neural pathways, which may lead to PLP.
PLP treatments. Treatment of PLP after an amputation is challenging. A large variety of
treatments have been suggested, however empirical data to support these treatments has been
lacking, with the vast majority based on small sample sizes with no control groups. Although it
is obvious that a series of changes which may play a role in the induction and maintenance of
chronic PLP in the peripheral and central nervous system occur after nerve injury, without the
underlying knowledge of the pathophysiological causes behind PLP, it is difficult to establish a
clear, rational treatment regime (Nikolajsen & Jensen, 2001).
There are a variety of surgical, medical and non-medical techniques and protocols.
Surgical intervention procedures however, carry a risk of further deafferentation, resulting in
even more pain and should be avoided (Nikolajsen & Jensen, 2001). Medical interventions
include tricyclic antidepressants (Kalso, Tasmuth, &Neuvonen, 1995), sodium channel blockers,
and anticonvulsant drugs (Sindrup& Jensen, 1999). Non-steroidal anti-inflammatory drugs
(NSAIDs) and paracetamol are considered to be ineffective in PLP by most practitioners
(Nikolajsen & Jensen, 2001). Some amputees can benefit from opioids, with a limited risk of
drug dependence (Dellemijn, 1999). Side effects associated with these pharmacological
treatments are extensive. Tricyclic antidepressants may produce "sedation, confusion and
anticholinergic side effects such as constipation, dry mouth, blurred vision, urinary hesitancy and
orthostatic dizziness" (Simmons & Feldman, 2000, p. 1). They are contradicted for use in
individuals with heart disease, orthostatic hypotension or angle-closure glaucoma.
Anticonvulsants have side effects such as dizziness, somnolence, headache, diarrhea, confusion,
nausea and peripheral edema (Simmons & Feldman, 2000). Narcotic analgesics have side effects
of nausea, sedation, constipation, respiratory depression and are controversial for treatment in
that they are habit forming with chronic use (Lacy, Armstrong, Goldman, & Lance, 2010).
Capsaicin cream has been shown to have "poor compliance because of the need of frequent
applications, an initial exacerbation of symptoms and frequent burning and redness at application
site" (Simmons & Feldman, 2000, p. 3). Furthermore surveys suggest that although physicians
believe treatments are effective (Sherman, Sherman, & Gall, 1980), fewer than 10% of patients
with PLP receive lasting relief from prescribed medical treatments (Sherman et al., 1984).
Non-medical treatments include transcutaneous electrical nerve stimulation (TENS),
vibration therapy, acupuncture, hypnosis, biofeedback and electroconvulsive therapy, although
clear evidence of effect is limited. Electrical stimulation of the spinal cord, deep brain structures
and motor cortex may relieve chronic neuropathic pain, including PLP; however the effect of
treatment often decreases with time (Nikolajsen & Jensen, 2001). TENS, applied to the outer ear,
was found in a placebo-controlled crossover design by Katz and Melzack, 1991 to reduce PLP;
however its long-term effectiveness in alleviating PLP remains unknown. TENS applied to the
contra-lateral limb was shown to reduce PLP, an effect which was maintained at a one-year
follow-up (Giuffrida, Simpson, & Halligan, 2010). Sherman suggests that pain reductions after 1
year of treatment are comparable to placebo (Jensen, Wilson, & Rice, 2002). More recent
treatments including local anesthesia, sympathectomy, dorsal root entry-zone lesions,
cordotomy, neurostimulation methods, or pharmacologic interventions such as anticonvulsants,
barbiturates, antidepressants, neuroleptics, and muscle relaxants have been beneficial only 30%
of the time (Flor, 2002).
Two newer therapies have emerged. Farabloc technology and Mirror Therapy have been
used effectively to treat PLP. Both therapies are without side effects and are drug-free
alternatives to treating PLP.
Farabloc Technology Therapy
History of Farabloc. In 1978 Frieder Kempe designed a metallic fabric called Farabloc
to help his father, an above knee amputee, deal with his PLP. Rudolf Kempe lost his leg in 1944
in the World War II battle of Monte Cassino. Frieder noted that his father's pain often seemed to
be weather related (F. Kempe, personal communication, April 7, 2010).
The first publication of documented changes in pain perception associated with the
weather was in the American Journal of Medical Sciences in 1887. This case report described a
person with PLP who concluded that "approaching storms, dropping barometric pressure and
rain were associated with increased pain complaint"(Shutty, Cunduff, &DeGood, 1992, p. 199).
Individuals with PLP have been reported to be especially sensitive to weather changes
(Harlfinger, 1991). Meteorological factors that contribute to changes in pain include temperature,
barometric pressure, precipitation, humidity, thunderstorms, sunshine and increased ionization of
the air (Harlfinger, 1991). Due to the fact that tendons, muscles, bones and scar tissue are of
various densities, cold and damp may expand or contract them in different ways. Change in
barometric pressure may also cause a transient "disequilibrium" in body pressure that may
sensitize nerve endings and account for increased pain preceding changes in temperature or
humidity (Jamison, 1996). Farabloc could be used to shield the high-frequency electromagnetic
fields (EMF) that accompany such a change in the environment.
Frieder Kempe used the principles of the Faraday Cage developed by the 19th century
British scientist Michael Faraday, to shield sensitive tissue, calm damaged nerve ends and
stimulate blood circulation. The Faraday cage is used to protect sensitive MRI machines from the
Earth's magnetic shifts. Farabloc in a similar manner, shields the human body from immediate
shifts in the Earth's electromagnetic field. Published studies have shown that Farabloc relieves
pain, as measured by using the Visual Analogue Scale (VAS), comparing pain reports using
Farabloc compared with a placebo fabric of identical color and texture (Bach & Clement, 2007).
Mechanisms involved in Farabloc therapy. Farabloc has been demonstrated to have
external electromagnetic shielding properties (McDiarmid& Trudeau, 1998) and block
electromagnetic fields (EMF) four times more effectively than placebo fabric (Clement &
Taunton, 2001). Double layers of Farabloc are able to completely block high frequency EMF
(greater than 1 MHz), such as radio waves (Zhang, Clement, & Taunton, 2000). The exact
mechanism of action for Farabloc is unknown, however, it is theorized that the absence of EMF
has an effect on damaged cells and subsequent pain (Clement & Taunton, 2001). Farabloc has
no magnetostatic shielding properties (McDiarmid& Trudeau, 1998).
Farabloc has been shown to shield high frequency EMF, but not to shield low frequency
EMF. Benefits of low frequency EMF have been demonstrated in orthopedic practice, in
combination with controlled weight bearing, to stimulate ionic transfer across cell membranes in
bone caniculi to facilitate healing (Pilla, 2002). Low frequency EMF exposure to human
lymphocytes showed a reduction in cell membrane fluidity and an increase in superoxide
dismutase (Bordiushkov et al., 2000). This suggests that low frequency EMF appeared to reduce
permeability, while high frequency EMF increase permeability, with extreme cell membrane
destruction the obvious result in ionizing radiation (Bach & Clement, 2007). Thus, Farabloc
could reduce cell membrane permeability and promote healing in individuals with acute
Phantom limb treatments are based on the assumption that long-term PLP is due to
functional or structural changes in the central nervous system, in response to noxious
somatosensory input. "Peripheral factors may contribute to central changes and enhance map
reorganization" (Flor, 2008, p. 815). Amputated nerves have an increased excitability, or reduced
threshold of stimulus (Gudin, 2004). An external mechanism to reduce this excitability, in the
form of a Farabloc amputee limb cover, could be beneficial in reducing this noxious
somatosensory input by reducing the high frequency EMF frequencies that over-stimulate these
nerve pathways. Another possibility is that Farabloc may increase the blood supply of the
residual limb, as indicated by the increased temperature perceived by users. Although the
temperature of the residual limb with and without Farabloc has not been clinically measured,
users report that an increase in temperature is perceived while using the Farabloc fabric, which
may contribute to its pain relieving properties (Bach & Clement, 2007).
Published studies regarding the absence of EMF.
The absence of EMF as PLP treatment. In 1987 Bach conducted a study of 13
individuals with PLP and observed positive results. Two-thirds of the amputees reported a
decrease in PLP, and some reported that they no longer required analgesics for pain. After 32
individuals were studied, 81.25% reported the Farabloc treatment success as "good" or "very
good" (Bach, 1987). In this study, Farabloc was demonstrated to be an alternative or adjunct to
oral medications.
In a sequential, controlled, double blind cross-over study on PLP in 1993, conducted by
Conine et al., Farabloc fabric, wrapped around the post amputation stump was found to be
statistically significant in reducing PLP, as compared to a placebo fabric. The greatest pain relief
occurred during the period when double layers of Farabloc covered the stump of the amputated
extremity. Nine of the 34 subjects reported pain relief of greater than 5 points on the VAS, while
the average relief was measured at 3 points. Twenty-one of the thirty-four patients reported their
greatest PLP relief during Farabloc intervention, with no adverse effects (Conine, Hershler,
Alexander, & Crisp, 1993). The authors concluded that Farabloc therapy compared to placebo
fabric demonstrated the ability to relieve PLP in the residual limb of amputees.
The effect of the absence of EMF with other diagnoses. In 2000 a randomized single-
blind placebo-controlled crossover study using double layers of Farabloc fabric wrapped around
the thigh post exercise produced similar results as these earlier studies. Zhang et al., exposed
untrained subjects to eccentric exercises to produce delayed onset muscle soreness (DOMS) in
the quadriceps. Farabloc technology therapy demonstrated significantly reduced pain, reduced
strength loss and reduced serum inflammatory markers (malondialdehyde, creatine
phosphokinase, myoglobin, leukocytes and neutrophils), compared to placebo fabric (Zhang et
al., 2000). Pain reduction of 3 points on the VAS was also found in this study.
Although the results of the study are unable to explain the exact mechanism in which the
body's response alters muscle activity, by the use of Farabloc therapy, it is hypothesized that
Farabloc shields the body from the effects of EMF and thereby stabilizes the muscle cell
membrane and reduces release of these substances into the serum. The reduction in levels of
leukocytes and neutrophils indicates a reduced inflammatory response, since white blood cells
are known to increase with severe exercise and muscle damage (Clement & Taunton, 2001). The
significant reduction in levels of malondialdehyde with the use of Farabloc is consistent with a
decrease in lipid peroxidation and reduced cascade of free radical damage to cell membranes.
The reduced elevation of creatine phosophokinase and myoglobin suggests that disruption of
muscle cell membranes was lessened when Farabloc was used immediately after exercise.
Farabloc is speculated to permit continued exposure to low frequency EMF, but effectively block
high-frequency EMF which increased the cells' resistance to disruption. Changing the balance of
the EMF toward lower frequencies may suppress free radical formation, by inhibition of iron-
containing enzymes, limiting the potential cascade of lipid peroxidation that is characteristic of
inflammation in delayed onset muscle soreness (DOMS) (Zhang et al., 2000). This study
indicates that the use of Farabloc leads to a decrease in the blood markers for inflammation and
cell destruction (Bach & Clement, 2007). These results suggest a substantial clinical reduction in
post-exercise disability and limitation of muscle damage and neurological pain (Clement &
In a study in 2007, by Bach and Clement, to investigate the effectiveness of Farabloc as
an analgesic in primary fibromyalgia, quality of pain, quantity of pain and total paracetamol
dosage were significantly reduced in subjects that used Farabloc garments at night. The results of
this study imply some alteration in somatic pain perception. This supports an analgesic effect
with the use of Farabloc fabric when compared to placebo fabric for neurological pain (Bach &
In summary, in all of these studies, the absence of EMF - due to Farabloc, an
electromagnetic shielding fabric, reduced pain in human subjects, who suffer from PLP, DOMS
and fibromyalgia, when assessed in placebo-controlled cross-over designed studies. The exact
mechanism behind these observations is still not known, however it is hypothesized that
alteration in EMF may have biological effects secondary to stabilization of the cell membrane
and enhancement of antioxidant properties. This could explain the reduced levels of anti-
inflammatory markers in the DOMS study (Clement & Taunton, 2001). Alteration of EMF by
shielding from high-frequency exposure could alter the permeability of the cell membrane, and
the subsequent reduced transfer of ions may stabilize the cell's response to excess exercise. None
of the studies reported any negative observations or side effects (Clement & Taunton, 2001).
Systematic reviews PLP interventions. In a systematic review by Halbert, Crotty and
Cameron, 2002, regarding the optimal management of acute and chronic PLP, Farabloc research
was only one of three studies to score the maximum of five points for a quality assessment. For
late PLP (greater than 2 weeks post-operatively), this review agreed that there is evidence
suggesting that Farabloc is an effective treatment (Halbert et al., 2002). These findings were
echoed in a review by Stanndard, Kalso and Ballantyne, 2010, in which Farabloc was listed as an
intervention, supported by evidence, for the management of PLP (Stannard, Kalso, & Ballantyne,
Mirror Therapy
History of Mirror Therapy. Mirror-box Therapy was initially introduced to treat upper
extremity PLP by Dr.Vilayanur S. Ramachandran at the University of California, San Diego, in
the early 1990s. Ramachandran was able to relieve PLP in 60% of his subjects in a study of ten
subjects (Ramachandran & Rogers-Ramachandran, 1995).
In 2001, Herta, Flor and colleagues performed functional neuroimaging experiments to
explore the neural reorganization that leads to PLP in upper extremity amputees, and discovered
that Mirror Therapy can eliminate the remapping associated with PLP (Lotze, Flor, Grodd,
Larbig, &Birbaumer, 2001). In this way it is theorized to "normalize the cortical reorganization
in the brain" (Chapman, 2011). More recently, Jack Tsao et al. (2007) evaluated the effect of
Mirror Therapy to treat PLP in lower extremity traumatic amputees (primarily due to blast
injuries), in a randomized, sham-controlled trial of Mirror Therapy versus imagery therapy. Tsao
reported that, "After four with four weeks of treatment, all patients using Mirror Therapy
reported a decrease in pain" (Chan et al., 2007).
Although vascular amputations are more numerous, the majority of studies with Mirror
Therapy have been conducted on amputees with lower extremity amputations due to traumatic
amputations or with upper extremity amputations. Presently, there is little research on the use of
Mirror Therapy with lower extremity amputees, due to vascular insufficiency or disease.
Theoretical Mechanisms involved in Mirror Therapy. According to Ramachandran,
Mirror Therapy produces a modulation of pain pathways in the amputated limb through visually
perceived movement of the amputated limb (Ramachandran & Rogers-Ramachandran, 1996). He
explains that PLP may be induced by a conflict between visual feedback and proprioceptive
representations of the amputated limb (Ramachandran &Hirstein, 1998). While periodic limb
movements during sleep and while awake do not activate central motor regions, normal
descending motor information, retained and activated during purposeful "phantom limb
movements" from the motor cortex is important in neutralizing the sensory (e.g. paresthesias and
pain) and motor discomfort (urge to move) of the restless leg (Giummarra& Bradshaw, 2010).
Simply imagining a motor sequence, which only activates the premotor regions, is insufficient to
relieve motor discomfort (Skidmore, Drago, Foster, &Heilman, 2009). Intentional movement
may also activate descending dopaminergic system in the striatum (Glasauer, 2001). This
explains the need for purposeful physical movement, not just imagining the movements in order
to obtain relief from motor discomfort. Thus the effectiveness of Mirror Therapy in reducing
PLP with amputees might be explained by the theory that when a person performs or observes
someone else's performance, mirror neurons in the hemisphere of the brain that is contralateral
to the amputated limb may be activated (Rossi, Tecchio, &Pasqualetti, 2002).
PLP has been associated with expansion of the amputated limb's sensory or motor cortex
map into nearby cortical structures. This reorganization appears to be both reversible and directly
related to pain symptoms. The degree of pain reduction following rehabilitation correlated with
normalization of the extent of primary sensory cortex. The ability to execute movements in the
mirror suggests that the capability of the unaffected hemisphere to generate these postures can be
transferred to the affected hemisphere if the affected motor system is provided with visual
information that can replace, bypass or dominate the disturbance of kinesthesis
(Bultitude&Rafal, 2009). Mirror therapy is thought to reverse this cortical remapping and
thereby alleviate pain (Hanling, Wallace, Hollenbeck, Belnap, &Tulis, 2010). "Appropriate
visual feedback (that matches the proprioceptive and motor feedback of a phantom sensation)
can correct the mismatch between visual and proprioceptive and motor cues, thereby reducing
the symptoms of PLP" (Weeks & Tsao, 2010). Visual-kinesthetic feedback which combines
observation and motor imagery has been shown to be beneficial to amputees experiencing PLP
(Beaumont, Mercier, Michon, Malouin, & Jackson, 2011).
Published Mirror Therapy studies for lower extremity amputees. The first study to
examine Mirror Therapy treatment in a person with a lower extremity amputation, who was
reporting PLP, was conducted by MacLachlan, et al, 2004. This was an individual case study in
which Mirror Therapy was used with a patient with PLP, who had been unable to obtain relief
from other treatments or interventions. An increased sense of motor control of the phantom limb,
and associated reduction in PLP, as previously reported with upper limb amputations, was
observed. A "fading out" of therapist-mediated intervention was explicitly designed to encourage
"ownership" of the treatment. Mirror Therapy exercises were directly supervised initially and the
level of supervision was decreased as the subject demonstrated increased competency with
demonstration of these exercises (MacLachlan, McDonald, &Waloch, 2004).
A landmark study was performed with 22 lower limb amputees by Tsao et al. (Chan et
al., 2007). Patients were assigned to three groups: One that viewed a reflected image of their
intact foot in a mirror, one that viewed a covered mirror, and one that was trained in mental
visualization. Patients were instructed to attempt to move both their intact and amputated limbs
or imagine performing the movements in the mental-visualization group. Under direct
observation, patients performed their assigned therapy for 15 minutes daily for four weeks. The
primary end point was the severity of pain after four weeks of therapy. The results indicated that
pain intensity, as well as number, and duration of pain episodes decreased with Mirror Therapy.
One hundred percent of patients in the Mirror Therapy group reported a decrease in pain, with a
median change on the VAS of 24mm with a range of -54 to -13. Two patients had brief reactions
(< 2 minutes) of grief on viewing the reflected intact lower limb. In the covered-mirror group,
only 17% indicated a decrease in pain, with 50% reporting worsening pain. In the mental-
visualization group 33% reported a decrease in pain and 67% reported worsening pain. The
mirror group differed significantly from the covered-mirror group and the mental-visualization
group. PLP decreased in 89% who switched to the mirror therapy group after the four weeks.
This study provides support to Mirror Therapy being effective in reducing PLP in
patients who had undergone amputation of lower limbs. It is suspected that this pain relief may
be due to the activation of mirror neurons in the hemisphere of the brain that is contralateral to
the amputated limb. These neurons fire when a person either performs an action or observes
another person performing an action (Rossi et al., 2002). Alternatively, visual input of what
appears to be movement of the amputated limb might reduce the activity of systems that perceive
protopathic pain. Protopathic pain is described as sensing pain, pressure, heat, or cold in a
nonspecific manner, usually without localizing the stimulus - used especially of certain sensory
nerves (Henson, 1977). Although the underlying mechanism accounting for the success of this
therapy remains to be fully elucidated, these results suggest that Mirror Therapy may be helpful
in alleviating PLP in an amputated lower limb (Chan et al., 2007). In other studies, Mirror
Therapy as a home program, has proven effective in decreasing PLP (MacLachlan, McDonald,
&Waloch, 2004; Darnall, 2009).
PLP and Occupational Therapy. Occupational therapy intervention enables clients to
maximize their independence during activities of daily living such as bathing, dressing, toileting,
bathroom transfers, returning to work, and instrumental activities of daily living tasks such as
cooking, cleaning, laundry, yard-work, money and medication management. If chronic pain
impairs the client's ability to participate in activities that the client needs or wants to do,
decreasing the impact that this pain has on the client's participation, becomes important to the
occupational therapist.
PLP can impact the roles, routines, habits and the self-concept of an individual with an
amputation and negatively affect quality of life. Therapeutic techniques and modalities used by
occupational therapists can decrease the effect that this chronic PLP has on the quality of life of
our clients. By decreasing PLP, facilitating earlier prosthetic use and increasing functional
participation in daily life activities, occupational therapists may to help clients achieve their
Summary.
From this research there is strong evidence that the absence of EMF, through the use of
Farabloc, is effective in treating PLP, as well as other neurological types of pain. In other studies,
Mirror Therapy research has been demonstrated to reduce PLP in upper as well as lower
extremity amputees. The success of Farabloc appears to be due to the shielding of high-
frequency EMF from entering the residual limb (an external process), while the effectiveness of
Mirror Therapy appears to be due to the re-organization of the sensory-cortex (an internal
process) and the pain relief is the "result of resolving the multisensory dissonance between visual
and motor/proprioceptive systems" (Weeks & Tsao, 2010). Farabloc and motor imagery therapy
were both identified as successful evidence-based nonpharmacologic therapies for PLP (Miller &
Rodriquez, 2010). Once PLP pathways have been established they appear more difficult to
eradicate and treat, therefore, it would seem critical to address the issue of PLP early in the
process, soon after the amputation. Thus the purpose of this study was to investigate if the
combined protocol using Farabloc and Mirror Therapy treatment, in the acute stages following
surgery, would reduce the experience of PLP and increase the quality of life (QOL) for amputees
with an acute lower limb above or below knee amputation. The hypothesis is that a treatment
protocol that targets external (peripheral) and internal (central) neuronal mechanisms
simultaneously is likely to be able to reduce PLP more substantially than either treatments alone,
particularly when used as an early intervention.
The primary research questions are:
What is the effectiveness of combining two interventions, Farabloc technology to eliminate
electromagnetic fields and mirror therapy to assist in the sensory cortex reorganization, to
decrease or eliminate phantom limb pain in above or below knee vascular amputees? The study
also investigated whether 1) the intervention was effective with acute and chronic amputees and
2) whether improvement was maintained after intervention was discontinued.
Implications for activities of daily living and quality of life were measured as well as physical
conditions of the amputee residual limb.
CHAPTER 3: Methods
Subjects
Sixteen subjects were recruited from January to July 2011 with all subjects completing
the study requirements by September 2011. The subjects were recruited from a population of
unilateral above or below knee vascular amputees. Eleven acute subjects were recruited from
Vidant Medical Center, Greenville, NC and were identified with reference to the inclusion and
exclusion criteria for this study. Five chronic subjects were recruited from the Eastern North
Carolina Amputee Support Group and were included if they met inclusion criteria and were
experiencing PLP. All subjects consented to participate. However, two subjects had medical
complications that forced their elimination from the study, leaving nine subjects in the acute
Inclusion criteria. Adults 19 years of age or older, able to understand the use of a VAS,
comprehend and write in English, with a minimum of 15cm of residual femur or tibia remaining
over which an amputee limb cover could be placed. The only difference between the two groups
was the time from amputation to beginning the study. Subjects in the acute group had surgery
less than six weeks previously, while subjects in the chronic group had surgery more than six
weeks previously.
Exclusion criteria. Individuals with bilateral lower extremity amputations; upper
extremity amputations; guillotine amputations (delayed closure due to risk of infection), hip
disarticulation amputations, foot, partial foot or toe amputations and individuals who were
pending revision surgeries. Individuals were also excluded if they were involved in a
compensation claim; had a diagnosis of neurological or psychological disorder that would
interfere with the study; required dialysis; had a known uncontrolled systemic disease (i.e.,
cancer, lupus etc.); had a history of substance abuse or dependence; were unable to provide
written consent and written authorization for use or release of health and research study
information; had a prior history of vertebral disc disease/condition, sciatica or radiculopathy;
were unable to follow study instructions or were unlikely to complete all required visits; were
participating in another investigational drug or device study for phantom limb pain or had
participated in these studies 30 days immediately prior to study enrollment; had any condition or
situation that may have put the subject at significant risk, confounded the study results, or
interfered significantly with the subject's participation in the study; subjects who were taking
anti-convusant/ neuropathic pain medications which exceeded maximum recommended daily
dosages (e.g. pregabalin (Lyrica) 450mg/day, duloxetine (Cymbalta) 60 mg/day or gabapentin
(Neurontin) levels 3600mg/day). Institution Review Board approval was received for this study
and each subject signed consent before starting the study (Appendix A).
Demographics. Demographics were gathered in a brief pre-interview before doing any
pretesting and are illustrated in Table 1. Sample group demographics represented the typical
population of vascular amputee patients treated at Vidant Medical Center. Mean age for subjects
was 59.43 years, SD = 9.96, range = 48 - 78, with the mean age for the acute group was 58.22
years, SD = 11.19, range = 48 – 78 years and mean age for the chronic group 61.60 years, SD =
7.92, range = 51-73 years. There was no statistically significant difference between the mean
ages of the groups t= .216, p= .832. Seven of the sixteen were female and nine were males. The
ethnicity of subjects included ten Caucasian, four African American and two of Hispanic origin.
The subjects were evenly divided regarding the side of amputation (50% right and 50% left
amputations), with five above knee amputations and eleven below knee amputations. Four
subjects were working, three were on disability and nine were retired. The highest level of
education completed was high school for nine of the subjects and college for seven of the
subjects, with six high school and five college graduates in the acute group, and three high
school, with two college graduates in the chronic group. Average time from surgery until
subjects began the study for the acute group was 35.5 hours, range = 26 – 48 hours, with the
chronic group averaging 18.2 months since surgery, range = 8 – 28 months.
This experimental pilot study used a repeated-measures design. There were two subject groups.
Subjects were either assigned to the
acute group if the amputation had occurred within six weeks
of the beginning of the study or the
chronic group if the amputation had occurred more than six
weeks previously. All subjects were measured on the dependent variables, received the
traditional amputee treatment protocol, as well as the experimental protocol combining Farabloc
Therapy and Mirror Therapy for four weeks. The independent variable was the combined
intervention therapy. Measurement of the dependent variables occurred at pre-treatment,
immediately after the intervention (post-treatment) and after a four week period of no treatment
(maintenance).There were multiple dependent variables that included: 1) physical measurements
(e.g. edema, temperature of residual limb), 2) perception of phantom limb pain (e.g. intensity,
frequency, duration, bothersomeness), 3) impact on the activities of daily living (e.g. self-care,
walking ability, car transfers, low-chair transfers, sleep) and 4) well-being (e.g. satisfaction with
how things worked out since amputation, mood and quality of life). Each of the dependent
variables are explained below. For the variables that were the subject's perception, a visual
analogue scale (VAS) was used. This unidimensional pain scale has been shown to be useful in
the assessment of pain intensity (Hjermstad, et al., 2011).
Residual limb effects.
Edema: measured in centimeters (cm) around the widest part of the residual limb
Temperature amputee limb cover: measured in degrees Celsius (°C),temperature of
residual limb covered with amputee limb cover
Temperature no cover: measured in degrees Celsius (°C),temperature of residual limb
PLP variables.
Intensity: Worst PLP daily, averaged over 4 weeks on a VAS in millimeters from
0 (no pain) to 10 (pain as bad as you can imagine)
Frequency: How often subjects experienced PLP over 4 weeks from
0 (never) to 6 (all the time)
Duration: How long each PLP episode lasts on a VAS in millimeters from
0 (I have none) to 6 (more than two days)
Bothersomeness: How bothersome PLP was over 4 weeks on a VAS in millimeters from
0 (extremely bothersome) to 100 (extremely mild)
ADL interference.
Self-care: the amount that PLP interferes with self-care tasks daily rated on a scale of
0 (Does not interfere) to 10 (Completely interferes)
Walking: the amount that PLP interferes with walking ability daily rated on a scale of
0 (Does not interfere) to 10 (Completely interferes)
Car transfer: ability to get in and out of car in the past four weeks using VAS, measured
in millimeters from
0 (Cannot) to 100 (No Problem)
Low-chair transfer: ability to sit down and get up from chair with a low seat (e.g. an easy
chair or deep sofa) in the past four weeks using VAS, measured in millimeters from
0 (Cannot) to 100 (No Problem)
Sleep: the amount that PLP interferes with sleep daily rated on a scale of
0 (Does not interfere) to 10 (Completely interferes)
Well-being.
Satisfaction: with how things have worked out since amputation, in the past four weeks
using VAS, measured in millimeters from
0 (Extremely dissatisfied) to 100 (Extremely satisfied)
Mood : the amount that PLP interferes with mood daily, rated on a scale of
0 (Does not interfere) to 10 (Completely interferes)
QOL: Quality of Life in the past four weeks using VAS, measured in millimeters from
0 (Extremely dissatisfied) to 100 (Extremely satisfied)
Measurements There were three primary instruments used in this study. The Prosthetic
Evaluation Questionnaire (PEQ) (Appendix B) which was completed at each of the three
measurement periods. The Daily Log (Appendix C) and Brief Pain Inventory (BPI) (Appendix
D) which were completed daily by each subject for eight weeks and were returned to the
Principal Investigator (PI) after each four week period. Physical measurements were completed
with each testing period to ascertain wound healing and included residual limb edema and
temperature of residual limb.
Prosthesis Evaluation Questionnaire. The PEQ was developed to fill the need for a
comprehensive self-report instrument for individuals with lower limb loss (Legro, 1998) and is
widely used in rehabilitation health service research settings. The PEQ is divided into seven
Groups or topical sections, in order to categorize related issues, which include: Group 1
Your
Prosthesis/Amputee Limb Cover, Group 2
Specific Bodily Sensations, Group 3
Social and
Emotional Aspects of Using a Prosthesis(not be included in this study), Group 4
Your Ability to
Move Around, Group 5
Your Satisfaction with Particular Situations, Group 6
Your Ability to Do
Your Daily Activities, Group 7
How Important Different Qualities of your Prosthesis/Amputee
Limb Cover are to You. The items in each Group include nine validated scales, with four
included in this study:
Appearance, Residual Limb Health, Utility, and Well-Being. There are
also individual questions not combined into scale scores and include:
satisfaction, pain, transfer,
prosthetic care, self-efficacy, and
importance questions.
Scoring. The PEQ is a self-administered questionnaire consisting of 82 items with a
linear analog scale response format. The PEQ is composed of nine validated scales that are each
comprised of multiple questions. The scales are computed from 42 items and include :
ambulation, appearance, frustration, perceived response, residual limb health, social burden,
sounds, utility, well-being. The forty remaining items pertain to other evaluation areas and are
not grouped into to scales. The scales are not dependent on each other, making it possible to only
use the scales pertinent to this study. A guide is provided which contains coding instructions for
all the questions ("Prosthetic Evaluation Questionnaire Evaluation Guide", 1998).
The linear visual analog scale format consists of a continuous numerical variable
measured as the distance in millimeters from the left to endpoint of the line to the point at which
the respondent's mark crosses the line. Each line is 100 mm long and is always measured from
the left to right or from 0-100. All questions are worded so that a higher number will correspond
with a more positive response. When a question is not applicable, it is coded "100" and or "nr"
no response. Any question that is left blank is scored as a non-response and treated as missing.
To calculate the scale scores, the arithmetic mean is computed of all the questions answered by
the respondent on that scale. A minimum of half the questions of a scale have to be
answered,(i.e. not answered "nr") to be valid. For this study, the questions have been re-
numbered from the original to make the questionnaire more usable.
Reliability. Two aspects of the PEQ's scale reliability were examined: internal
consistency and temporal stability (Legro et al., 1998). The internal consistency of each scale
was tested by computing a Cronbach's alpha and ranged from .73 to .89 for the 10 scales except
for
Transfers, which was .47 (Legro et al., 1998). The second reliability test determined the
degree to which the scores were stable over time for subjects who had not experienced a change
in health or prosthesis. The intra-class correlation (ICC) estimates for the mean scores of the first
and second administration of the scales were calculated. The results ranged from r = .79 to r =
.90 with two exceptions-
Perceived Responses and
Frustration (Legro et al., 1998).
Validity. The scales have been validated for internal consistency and temporal stability and are
scored as a unit. To demonstrate whether the scales could differentiate between groups of people
whose scale scores would be expected to be different, scores for the 10 scales were calculated for
participants grouped by gender, age, presence or absence of co-morbidities, level of amputation,
and years since the amputation. Statistical differences were found between men and women on
two scales (Legro et al., 1998). Men reported significantly better for the variable
Ambulation (70
versus 56 for women) and women reported a significantly greater
Social Burden (34 versus 18).
The scales of
Residual Limb Health and Frustration have differed significantly across age
groups such that younger patients identified more problems with their residual limbs and greater
frustration, than participants who were 40 years or older (Legro et al., 1998).
Ambulation scores
differed significantly between those with and without co-morbidities such that those with no co-
morbidities reported better
Ambulation (Legro et al., 1998). On the other hand, no statistically
significant differences were noted due to amputation level or years since amputation, as indicated
by correlations between r = .49 and r = .61 (Legro et al., 1998). In fact, the
Ambulation scale was
strongly correlated (r = .61) with the SF-36 subscale of physical function (Legro et al., 1998).
The
Social Burden scale of the PEQ demonstrated a strong negative correlation (r = -.52) with
the social interaction score. This is as expected since a high
Social Burden score indicates
experiencing no social burden and a low score on the Sickness Impact Profile (SIP) subscale
indicates no problem with social interactions (Bergner, Bobbitt, Carter, Gibson, 1981).
Additionally,
Well-being showed a moderate, negative correlation (r = -.49) with the total score
on the Profile of Mood States – short form (POMS-sf) (Shacham, 1983). This is appropriate
since a high score on the
Well-being scale is a positive response and a low score on the POMS-sf
indicates "low mental distress" (Legro et al., 1998, p. 935). Psychometric analysis supported the
reliability and validity of the PEQ for evaluating the function of the prosthesis and the major
health related quality of life domains. As questions on the PEQ are phrased within the past
month, support from a recent study demonstrated that validity of the time frame (Broderick,
Schneider, Schwartz, & Stone, 2010). Responses from the PEQ, should therefore be valid when
compared to the two other assessments used in the study, the BPI and Daily Log.
Daily Log. The log included questions regarding adhering to the treatment protocol, the
effect of PLP on sleep, duration of PLP episodes, as well as number of PLP episodes within 24
hours. Subjects were instructed to complete this log within one hour of waking up, daily for eight
weeks. The Daily Log does not have standardized validity and reliability; however, such logs
have been used elsewhere in research (Schumacher et al., 2002).
Brief Pain Inventory (BPI): Short Form. The BPI (Daut et al., 1983) was modeled
after the McGill Pain Questionnaire (Melzack, 1975). The BPI is a 17 item patient self-rating
scale assessing demographic data, use of medications, as well as sensory, and reactive
components of pain. It identifies components of sensory pain including severity, location,
chronicity and degree of relief due to therapy and reactive pain components including
depression, suffering and perceived availability of relief. Pain ratings are performed daily which
is a more accurate record of pain, when compared to scales in which recall periods are 3 days or
longer(Broderick, Schneider, Schwartz, & Stone, 2010) .
Scoring. The BPI uses 0 to 10 numeric rating scales for item rating for simplicity, lack of
ambiguity and cross-linguistic pain measurement. Subjects rate their pain at the time of
responding to the questionnaire (pain now), and also at its worst, least, and average over the
previous week. The ratings can also be made for the last 24 hours. Interference of function can
be thought of as a reactive dimension. Because an effective intervention for pain control should
demonstrate its effectiveness on more than a reduction in pain intensity alone, the BPI rates the
degree to which pain interferes with mood, walking and other physical activity, work, social
activity, relations with others, and sleep. The mean of these scores can be used as a pain
interference score.
Validity.Validity of the relationship between the increased use of pain medications and
high pain ratings was demonstrated for both narcotic (x=28.17, df =3, p<0.002) and non-narcotic
(x=23.75, df =3, p<0.002) pain relievers (Fabry Registry, 2004-2010). Validity of the BPI was
also supported by the moderate correlation between worst pain intensity ratings and ratings of
interference with six areas of activity and mood (r = .245 to .478. p<0.02 for all but social
relationships were p<0.05) (Fabry Registry, 2004-2010). There is a logical pattern in the
differences in inter-correlations among various pain and activity interference measures for
different diseases.
Reliability. The BPI has demonstrated respectable test-retest item correlations; at least
over short intervals (Daut, Cleeland, & Flannery, 1983). Evidence for the validity of the BPI
comes from several studies using the instrument with cancer patients and patients with other
diseases who had pain (Cleeland& Ryan, 1994). Expected differences in pain severity were
found between groups of patients with pain who differed in the presence or absence of
metastases. Ratings of pain interference with various activities increased as ratings of pain
severity were higher. The proportion of patients receiving opioid analgesics increased with
increased severity rating. The BPI has demonstrated over short intervals using test retest item
correlation; worst pain, r=.93; usual pain, r=.78; pain now, r=.59 (Fabry Registry, 2004-2010).
The correlations among the items differed in a logical way from one disease to another,
suggesting that the BPI is sensitive to differences in pain characteristics associated with different
diseases (Cleeland& Ryan, 1994).
Flexible Fabric Metric Tape Measure. This tape was used to examine wound healing
properties and measure the edema of residual limb is an indicator of wound healing.
Measurements were calculated in millimeters (mm), by obtaining a circumferential measurement
at widest point of distal residual limb. Once each subject has been measured, the length from the
end of the residual limb to the widest point of the residual limb was recorded, in order to ensure
that the same circumferential measurement was documented with each measurement, for each
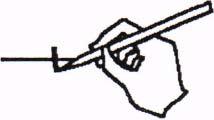
Hubbard Scientific 6083 Liquid Crystal Temperature Strip (APPENDIX E). Skin
temperature measurements were taken at all three measurement periods and included the
temperature of the residual limb both with and without coverings and the contralateral limb, as a
baseline measurement. Measurements were taken in degrees Celsius.
Procedure
Institution Review Board (IRB) approval was sought and obtained from East Carolina
University and Vidant Medical Center prior to beginning data collection. Potential subjects were
identified by the Staff Research Assistant, at Vidant Medical Center, according to the inclusion
and exclusion criteria. The Staff Research Assistant notified the principal investigator (PI) of
these potential subjects. Individuals with acute amputations were on bed-rest per the current
amputee protocol, when approached about the study. Individuals, who had amputation surgery
more than six weeks earlier and complained of PLP, were also identified by the Staff Research
Assistant, at the Eastern North Carolina Amputee Support Group. After completing the consent
process, individuals were assigned to the appropriate group, acute or chronic, by the Staff
Research Assistant.
Materials. The PI measured each subject's residual limb and fabricated two amputee
limb covers using Farabloc technology, for each subject. Farabloc technology (Farabloc
Development Corporation, 2012)uses a fabric that is woven using 9.5% steel wire fibers
consisting of iron, nickel, chromium and nylon, which has significant shielding effects on high
frequency EMF (greater than 1MHz) (Bach & Clement, 2007). This washable fabric has an
appearance similar to linen (Bach & Clement, 2007) and can be tailored into an amputee limb
cover that is worn over the stump/ residual limb. The dimensions for the Farabloc amputee limb
cover was measured by the PI, using the distal circumference of the residual limb, and a
proximal circumference a minimum of 15cm above this. The PI sewed two double layer cone-
shaped amputee limb covers, with a three inch elastic section included within the covers
proximally to improve fit and Velcro closures proximally. These were worn over the stump
dressing (4 x 4 gauze, dry dressing with liner to hold in place), and elastic shrinker, 23 hours/day
for the acute group, and whenever the prosthesis was removed for the chronic group. Two were
issued so that one could be worn while the other was hand-washed and air dried.
Pretesting. A Certified Prosthetist performed testing regarding the integrity and quality
of the amputee limb cover material, prior to issuing product to the subject, to ensure that the
amputee limb covers applied to subjects were functioning as anticipated. A continuity tester mini
multi-meter was used to test the integrity of each amputee limb cover. The Certified Prosthetist
measured the voltage that each amputee limb cover was conducting. All Farabloc amputee limb
covers conducted electricity due to the metal fibers embedded within them, which demonstrated
that the integrity of the fabric was intact. The PI kept a log (Appendix F) the readings obtained
from each amputee limb cover. This testing occurred at pre-treatment and post-treatment.
Occupational therapy and physical therapy evaluations were initiated post-operation day
one, per the standard acute amputee protocol. These evaluations include assessment of current
functional level as well as education on the standard amputee treatment protocol. Chronic
amputees completed this therapy at the time of their initial surgery. The education provided by
therapists is described in an amputee booklet issued to all amputee patients. All subjects received
this booklet, in which the care of residual limb, desensitization techniques for residual limb,
instructions for donning stump-liner and stump shrinker, techniques and assistive devices for
activities of daily living, mobility and functional transfers, durable medical equipment
recommendations in preparation for discharge, as well as appropriate exercises for upper
extremities and lower extremities are described. All subjects participating, regardless of group
placement, met or exceeded standards of care.
Pre-treatment measures. For all the subjects in both groups, the PI administered the
measurements prior to beginning the treatment protocol. For the acute subjects, this occurred
within the first two days after amputation. For chronic subjects, upon consent, the PI
administered measurements in their home, or at the prosthetist clinic. The measures included all
the dependent variables described and were completed as appropriate in one session.
Intervention. Within 48 hours of surgery, the Certified Prosthetist provided two stump-
liners and two stump shrinkers to all acute subjects per standard amputee treatment protocol.
Chronic amputees were issued with stump liners and shrinkers on an ongoing basis, as needed,
by a prosthetist. In addition all subjects received two Farabloc amputee limb covers. The
amputee limb cover was placed over the stump-liner and stump shrinker.
For the acute subjects, the PI notified the assigned occupational therapists treating the
subjects. Trained prior to the study on methods of intervention of Farabloc and Mirror Therapy
protocols, these therapists followed the written instructions designed by the PI (Appendices
G&H). The PI monitored the interventions to ensure the appropriate protocols were followed.
For the chronic group, the PI educated the subjects and family members on the Mirror
Therapy and Farabloc protocol. The PI monitored the interventions telephonically by checking
with chronic subjects and their families, to ensure the appropriate protocols were followed. The
PI provided all subjects with an educational binder, with instructions regarding tasks that
subjects were expected to perform daily throughout the duration of the study. The PI reviewed
this material with each subject and required demonstration from each subject in order to verify
comprehension. The PI provided each subject, with a 1/8" plexi-glass mirror (27 x 15") with
instructions on how to perform the Mirror Therapy exercise protocol. The subject was asked for
a demonstration of the Mirror Therapy exercise protocol to ensure there was an understanding.
The PI also provided instruction regarding how to don and care for the Farabloc amputee limb
covers and provided printed instructions in an educational binder.
For the acute subjects, the hospital's discharge planners began the referral process to
inpatient rehabilitation, or other discharge destinations as appropriate. Chronic subjects returned
to their place of residence. The PI notified the appropriate therapist working with subjects in
each setting about the subject's inclusion in this study. As appropriate, therapists assigned to
follow up with the subjects were contacted. Each therapist was given verbal and written
instructions via e-mail regarding the protocol and procedures, specifically regarding how to
apply and care for Farabloc amputee limb covers and supervise subjects performing Mirror
Therapy intervention. The PI monitored subjects and followed up with therapists in each setting
to ensure that protocols for the study were adhered to. For chronic subjects who were living in
their residences, the PI met with these subjects and their families after the Amputee Support
Group monthly, or at the prosthetist's office.
Post-treatment Measures at four weeks. One week prior to the vascular clinic in which
all acute subjects were seen four weeks post-surgery, the physician assistant notified the PI of the
schedule for the acute subjects. Each subject was asked to bring their mirror, PLP documentation
and amputee limb covers to this appointment. All dependent variables were measured by then PI.
Testing regarding the integrity of the Farabloc amputee limb cover material was completed to
ensure that the integrity of the fabric had remained intact. For the chronic subjects, the post-
treatment measurements were done if they returned to the Eastern North Carolina Amputee
Support Group, in the rehabilitation classroom at the end of the group, when all other members
had left. The PI met the chronic subjects at the office of the prosthetist to conduct these
measurements if the subject did not return to the Amputee Support Group. It was at this time that
the intervention was changed for all subjects. Subjects were instructed to continue with their
Daily Log and BPI documentation as well as the standard treatment protocol. However, subjects
were instructed not to use the Farabloc materials or perform Mirror Therapy intervention.
Maintenance measurements at eight weeks. The dependent variables were measured
again for all subjects. Acute subjects attended the Amputee Clinic and the chronic subjects
returned to the Amputee Support Group or their prosthetist's clinic. The PI collected the Daily
Log and BPI documentation from the subject. Subjects were thanked for their participation and
study materials were returned to subjects who requested their continued use.
Data analysis.
For each phase the mean and standard deviation was calculated for each variable, for all
subjects. A complete block design analysis of variance was conducted for each variable with a
.05 significance level. The week was the main effect and the individual was the blocking effect.
The analysis was repeated for each group (acute and chronic) separately. An LSD post-hoc
analysis was performed on all significant variables to compare the mean difference and standard
error between time periods (pre-treatment to post-treatment, pre-treatment to maintenance and
post-treatment to maintenance) using a significance level of .05 and 95% confidence interval.
CHAPTER 4: Results
Table 2 shows the results of the ANOVA for the combined subject groups. There were
significant differences for all the variables (residual limb effects, phantom limb pain, ADL
interference and Well-being), with the exception of the
temperature of the residual limb without
the amputee limb cover (control),
PLP duration and
satisfaction. These results suggest that the
treatment was effective for subjects with chronic and acute amputations. However, when
separating the two groups with separate ANOVAs, not all variables were significant, as seen in
Table 3. Specifically the variables of
PLP intensity (p =.098),
duration of PLP (p = .441),
low
chair transfers (p =.074) and
satisfaction (p = .652) for acute subjects were not significant.
Variables of
edema (p =.983),
residual limb temperature without amputee limb cover (p =.672)
,
duration (p =.087),
self-care (p = .160),
walking ability (p=.219),
car transfers (p =.301),
low
chair transfers (p=.162) for chronic subjects were not significant. Marginally non-significant
values for Well-being for the chronic group were also noted:
satisfaction (p =.054)
, mood (p =
.055)
, QOL (p = .056)
. All other variables were significant for both acute and chronic subjects.
Table 4 illustrates the post hoc analysis for the combined subject groups between the
three time periods for all the significant variables for the combined group. A pattern of
significant differences are evident from pre-treatment to post-treatment and from pre-treatment
to maintenance for all significant variables (
edema, intensity of PLP, frequency of PLP,
bothersomeness of PLP, PLP interference with self-care, walking, car transfers, low chair
transfers, sleep, mood and
quality of life), with the exception of one variable, the
temperature of
the residual limb with the amputee limb cover. However, there are not significant differences
between post-treatment and maintenance. This indicates that changes were more evident during
the actual intervention of the Farabloc and mirror therapy. Exceptions to this pattern were noted
for residual limb
temperature with amputee limb cover, which had significant differences from
pre-treatment to maintenance as well as from post-treatment to maintenance.
Table 5 illustrates the post-hoc analyses of subjects in the acute and chronic groups
across the three time periods. For the acute subjects, the same pattern emerged with significant
differences from pre-treatment to post-treatment and from pre-treatment to maintenance, but not
from post-treatment to maintenance for
edema, PLP frequency, and
PLP bothersomeness, PLP
interference with self-care, walking, car transfers, low chair transfers, sleep, mood and QOL.
For the chronic subjects, this pattern was shown for the variables of
PLP frequency, PLP
bothersomeness and PLP interference with
sleep, suggesting that the intervention was effective
as change stopped after discontinuation. This pattern indicates that significant differences are
noted during the periods in which the treatment occurred but that significant differences were not
noted during the period in which the treatment protocol was not being used.
A variation in this pattern was noted for the acute subjects, for the variable of
residual
limb temperature with amputee limb cover, in which there were significant differences from pre-
treatment to maintenance and from post-treatment to maintenance (Table 5). Post-hoc analyses
were not performed for the variables that were not significant in the initial ANOVA (e.g.
PLP
intensity, PLP duration, PLP interference with car transfers, and
satisfaction) (see Table 3).
The variable of
residual limb temperature with amputee limb cover for the chronic group
also varied from the typical pattern and showed significant differences, for all time periods (see
Table 5).
PLP intensity was significantly different from pre-treatment to maintenance and from
post-treatment to maintenance for the chronic subjects. Post-hoc analyses were not conducted the
variables of
edema, residual limb temperature without a cover, PLP duration, PLP interference
with self-care tasks, walking, car transfers,
low chair transfers, satisfaction, mood or
QOL.
Table 6 illustrates the time from surgery until subjects were ready to be fitted with
prosthesis. This was not a planned variable, but a real outcome measure for performance of
clients. Chronic subjects were read to begin prosthetic fitting at 12 weeks post-surgery, whereas
acute subjects (with the exception of two who had medical complications), were ready to begin
prosthetic fitting at eight weeks. Wearing tolerance of prostheses increased from 0-2 hours pre-
intervention to 8-12 hours per day for the chronic subjects. "For acute vascular amputee subjects,
no prostheses are issued immediately after surgery (prior to intervention) per the vascular
amputation protocol", Manalo, E., (personal communication, March 17, 2012), but after the
intervention seven of the nine subjects were able to tolerate wearing prostheses between four and
10 hours per day. With the exception of the two with medical complications, all subjects in
combined groups were able to use prosthesis after the intervention part-time (five subjects) or
full-time (seven subjects) and return to work, for those working prior to surgery.
Table 7 illustrates an observation of residual limb temperatures. A mean difference of
1.18°C was noted for subjects in the combined group, between
residual limb temperature with
amputee limb cover versus
residual limb temperature without cover. For the
residual limb
temperature without amputee limb, mean was 32.3°C, SD = 8.44, range = 30 to 33.5°C, with a
confidence interval of [31.4, 33.1]. For the
residual limb temperature with amputee limb cover,
mean was 29°C, SD = 8.44, range = 29 to 34°C with a confidence interval of [24.13, 33.87], and
were an average 1.18 °C cooler when wearing the amputee limb cover. This indicates a
significant difference for the residual limb temperature with and without the amputee limb cover
Discussion
The purpose of this study was to investigate the effectiveness of combining two phantom
limb pain treatments with vascular amputees, specifically, the absence of electromagnetic fields
using Farabloc technology (external source) and implementing Mirror Therapy as a method of
sensory cortex reorganization (internal source) to reduce phantom limb pain. The results suggest
that the combination of these therapies, significantly reduced PLP for both acute and chronic
vascular amputees. For all fourteen subjects, there were significant differences noted from before
to after treatment intervention and even after treatment stopped on the majority of the
measurements, including physical measures, reported pain or discomfort, ADL performance and
quality of life. No significant differences were noted for residual limb temperature without
amputee limb cover, which acted as a control for each subject, PLP duration or satisfaction with
how things had worked out since the amputation for the combined group. When analyzed further
it was clear that there were differences between the two groups based on whether the individual
was recovering from an acute amputation or their amputation was more remote. Overall,
individuals with acute amputations having greater gains in residual limb healing, occupational
performance measures, and well-being, while the individuals with chronic amputations, had
greater gains in PLP intensity reduction.
An unexpected and significant result of this study was the decreased time from surgery
until acute amputees were ready for prosthetic fitting. In accordance to typical vascular amputee
protocols for this facility, (personal communication Manalo, E., 17 March, 2012) fitting of a
prosthesis occurs around 12 weeks post amputation and this was true for 5 of the 5 chronic
subjects. However, in this study, use of the two treatments appeared to reduce edema and
accelerate wound healing so significantly, that all but two of the acute participants, seven of the
nine acute amputees (78%), were ready for prosthetic fitting an average of four weeks early. The
implications of this finding are considerable, as it could improve individual health outcomes as
well as society outcomes in terms of cost. Currently the majority of amputee intervention is
provided by occupational therapists in acute or in-patient rehabilitation settings. Use a more
effective treatment protocol to improve residual limb healing for acute amputees would decrease
the time until acute amputees can become functional prosthetic users, improving functional
independence, decreasing cost of services as well as reducing PLP for improving in quality of
Objective Measures
Edema. For the combined group there were significant differences with respect to
residual limb edema. Although amputees are encouraged to exercise their residual limb, they
are not always able to do so. With this study's protocol increased active motion of the
residual limb was evident when subjects performed bilateral lower extremity movements
during mirror therapy exercises. This increased active motion may explain some of the
decreased edema noted with the use of this treatment protocol, as edema has been shown to
decrease with active motion (Colditz, 2011).
As noted,
edema decreased significantly for the acute group with the use of this
treatment protocol. Although edema continued to decrease there was not a significant
difference between post-treatment and maintenance. Significant changes were noted during
periods in which the amputee limb cover was worn. Although it is not surprising that edema
would decrease to some extent with this group, the marked decrease in edema that facilitated
earlier prosthetic wear, was remarkable. A more likely explanation for the edema reduction
may be the high frequency EMF shielding effects of the amputee limb cover. High frequency
EMF increases cell permeability (Bach & Clement, 2007), so the absence of high frequency
EMF provided by the amputee limb cover may mean that the cells are less permeable with a
reduction in cell membrane fluidity and an increase in superoxide dismutase, which has anti-
inflammatory properties (Bordiushkov et al., 2000). This has been shown in other studies.
Coupled with the increased exercise, the combination of these two therapies, have important
implications for treatment.
Edema reduction was not anticipated for the chronic group, as wound healing was
complete with this group. However, what was significant was the increased tolerance that the
chronic group noted for wearing their prostheses. Logs of the subjects show that four of the
five subjects reported an increase in their prosthetic wearing time and another was able to
wear their prosthesis for the first time since surgery, 17 days after initiating treatment
protocol. Chronic vascular amputees frequently struggle with prosthetic fitting and wearing,
due to volume changes in the residual limb (Klute, Berg, Biggs, Pongnumkul, Popovic, &
Curless, 2011). Farabloc can be incorporated into the socket of prostheses which may result
in stabilization of residual limb volume, due to stabilization of muscle cell membranes
(Clement & Taunton, 2001) and improved consistency with prosthesis wearing.
Residual limb temperature. Temperature of residual limb with no cover was the control
for each subject to compare the
temperature of residual limb with the amputee limb cover.
Residual limb temperatures were an average of 1.18°C cooler for the combined group of
subjects, when wearing the Farabloc amputee limb cover, than without the amputee limb cover.
This reduction, could possibly be due to the shielding effects and absence of high frequency
EMF, and appears to be associated with the reduction in PLP.
This suggests that the differences in temperature are related to the use of the Farabloc
amputee limb cover, as all subjects used the same treatment protocol throughout the study. Since
excessive heat and sweating of the residual limb within the socket of a prosthesis is the primary
compliant for amputees and this decreases wearing time and QOL (Huff, Ledoux, Berge,
&Klute, 2008), these results suggest that fabrication of prosthesis sockets with the Farabloc
fabric could lead to a decrease in temperature which may increase wearing times further and
corresponding participation in life.
These results were not anticipated and the implication of the residual limb temperature
reduction is not clear. The reduced inflammatory response, resulting in a reduction of leukocytes
and neutrophils as blood markers for inflammation and cell destruction (Clement & Taunton,
2001) while wearing the amputee limb cover, may be one explanation for the temperature
reduction. Despite this decrease in temperature, users perceived an increase in temperature while
wearing the Farabloc amputee limb cover. These results are similar to another study in which
users of Farabloc garments also perceived increased temperatures (Bach & Clement, 2007).
This is the first study using Farabloc technology in which the temperature of the residual
limb with and without the cover was measured. Unfortunately, temperature readings with the
use of the Hubbard Scientific 6083 Liquid Crystal Temperature Strip thermometer are not
sufficiently sensitive. Improved accuracy of temperature readings would be required before clear
associations could be made between residual limb temperatures and PLP reduction. Additionally
wound bed temperature was not measured which might indicate wound healing. The initial
results here warrant further investigation, and would be an interesting aspect of further research.
Further continued research into lowering of residual limb temperatures with prosthesis use is
needed to improve the QOL for these amputees.
PLP Subjective Measures
PLP Variables.
Intensity, Frequency, Duration and Bothersomeness of PLP. Significant decreases in
phantom limb pain intensity, frequency and bothersomeness for the combined group were noted
during the treatment period and this reduction continued through the maintenance period,
indicating a continued treatment effect. The long-term effects of this reduction require further
investigation to establish whether these continued treatment effects are maintained. Individuals
with vascular disorders from disease processes such as diabetes, frequently suffer from
peripheral neuropathic pains for many months or years prior to an amputation (Health, 2011).
Once neuropathic pain is established it is extremely difficult to eradicate (Nikolajsen & Jensen,
2001), therefore a treatment which was able to decrease the intensity of neuropathic pain prior to
an amputation may lead to an even greater improvement in intensity, frequency and
bothersomeness of PLP after amputation. The shielding properties of a Farabloc garment, such as
those used in another study (Bach, 2007), may be useful in preventing this neuropathic pain.
Decreases were also noted in duration of phantom limb pain for the combined group;
however these decreases were not statistically significant. The brevity of the treatment protocol
period (four weeks) might have influenced this result. Further research is required to ascertain
the optimal treatment period, as well as long-term maintenance results of this treatment protocol.
Overall, the significant decreases noted during the treatment period of PLP frequency and
bothersomeness are important for the acute group in order to maximize their ability to participate
in the rehabilitation process, which occurs within the first month after surgery. PLP intensity and
duration did not significantly decrease for the acute group, however if reductions in the other two
variables are noted, an overall improvement of participation can be anticipated, as demonstrated
Similarly, significant improvements were noted for PLP intensity, frequency and
bothersomeness for the chronic group. These findings are promising, as all subjects in the
chronic group agreed to participate in this study because they had PLP which interfered with
their function and QOL. Despite the time since surgery (an average of 18.2 months), these
subjects were able to benefit from this treatment protocol in managing their PLP symptoms. This
implies that occupational therapists can use this treatment protocol to help amputees deal with
chronic PLP symptoms, which may continue to limit their participation with ADL tasks.
ADL Interference.
Significant reductions for the combined group were noted for PLP interference with self-
care, walking ability, car transfers, low chair transfers and sleep. The mean value improved from
pre-treatment to post-treatment and then again from post-treatment to maintenance, indicating a
continuation of treatment effect for all categories of variables. PLP interference decreased
significantly for all tasks for the acute group during the treatment and maintenance periods, with
the exception of low chair transfers which was not significant for either the acute or chronic
group, possibly due to a lack of power when the groups were divided. Low chair transfers
represent a variety of different heights of surfaces, which can increase the difficulty of the
transfer depending on the transfer performed e.g. transfer-board transitions as opposed to stand-
pivot transfers, which may vary as subjects strength improved and have little to do with PLP
interference. The differences noted with low-chair transfers may have been due to the lack of
standardization of the term "low" which could represent a variety of heights of surfaces. This
was a limitation of the PEQ evaluation tool. Despite this lack of standardization, significant
improvements were noted for all ADL tasks. The use of a treatment protocol to increase acute
amputee participation in ADL tasks is especially important for occupational therapists, as this is
the population of amputees with whom the majority of occupational therapy interventions occur.
This treatment protocol appears to have had a more of an effect on reducing the
interference of PLP on ADL tasks with the acute group, as compared to the chronic group.
Compensation techniques learned by the chronic amputees to adapt to their functional
limitations, may be influential in limiting the effect that PLP interference has on ADL task
performance, as chronic amputees have well established roles and routines.
Significant reductions were noted with PLP interference with sleep. The decrease in PLP
interference with sleep for both groups is most encouraging. Amputees frequently report
increased PLP symptoms at night and report sleep disturbances due to PLP, which influences all
other ADL tasks and falls within the occupational therapy scope of practice (AOTA, 2009). A
treatment protocol, in which occupational therapists can positively influence the amount that
PLP interferes with sleep for all amputees, is important. These types of evidence-based treatment
interventions are exactly what the occupational therapy profession needs to expand our toolboxes
and maximize the functional outcomes of our clients.
Well-being.
Statistically significant improvements in mood and QOL were observed for the combined
group during the treatment and maintenance periods. Post hoc comparisons for the acute group
did not demonstrate statistically significant differences for satisfaction with how things had
worked out since amputation. An explanation for the decreased satisfaction experienced by
amputees in the acute group may be explained by the following, "Vascular amputees are
frequently frustrated by the increased time required for wound healing and the resulting
functional limitations of remaining at a wheelchair level for approximately three months, as
opposed to using a lower extremity prosthesis immediately." (Personal communication, Faulk,
C., March 17, 2012).An area of further investigation would be to compare acute non-vascular
amputees who are able to be fitted with early post-operative prostheses (E-P.O.P.), compared to
vascular amputees who have to remain primarily at a wheelchair level of function due to wound
healing issues, because of their disease process. It is postulated that satisfaction improvements
would be noted with amputees using an E-P.O.P. as opposed to amputees who remain at a
wheelchair level of function. Subjects in the chronic group reported differences for satisfaction,
mood and QOL during the treatment and maintenance periods, however these were marginally
not statistically significant.
In conclusion, the results of this study are promising as they indicate significant
differences for all categories of variables (residual limb, PLP, ADL interference and Well-being)
for all subjects. The majority of these differences occurred during time period in which the
treatment protocol was actively being used by subjects, which indicates that the differences noted
were associated with the use of the treatment protocol. Despite the lack of discernible change
during the maintenance period, the differences achieved from pre-treatment to post-treatment
continued through the maintenance period for all significant variables. This demonstrates that
differences noted with the implementation of the treatment protocol were not eradicated after the
treatment protocol had ended.
A decrease in PLP leads to a subsequent increase in participation of daily life activities
because pain and discomfort no longer limit participation. In fact, this was shown in the results.
Specifically that both groups demonstrated significant improvements regarding reduction of
PLP, increased participation in ADL tasks and a corresponding improvement in well-being.
There does not appear to be a distinct advantage to using this treatment protocol with acute
amputees as compared to chronic amputees. Both groups benefitted from the use of this
treatment protocol. The implications of this study are that through the use of this treatment
protocol, occupational therapists can have a positive influence in reducing PLP, reducing the
amount that PLP interferes with ADL tasks and improving Well-being, which would help our
amputee clients meet their goals, to maximize functional independence and improve their QOL.
Implications of Functional Outcomes
As discussed, the implications for decreasing time from amputation surgery to initial
fitting of the prosthesis for the acute participants in this group was an unexpected and very
positive result. Equally unexpected and impressive was the impact of the treatment protocol on
the individuals with amputations that had already been fitted with prosthesis, but were not
wearing them due to discomfort and pain. The impact on the functional performance of these
clients is significant as outlined in the following short descriptions.
A 73 year-old Caucasian male had pre-existing diabetic peripheral neuropathy prior to his
amputation and spent the majority of his time on the couch. Prosthetic use was limited to two
hours per day. After completing the treatment protocol, he is wearing his prosthesis ten hours per
day. He has resumed yard work, going out to eat with his wife, and attending out-patient
physical therapy sessions to improve his gait patterns.
Prior to the study, this 51 year-old Hispanic woman was incapacitated and remained in
bed with PLP every 30 minutes. She was unable to tolerate wearing her prosthesis and the pain
severely limited her quality of life, including participating in the care of a teenage daughter.
Incredibly, within 17 days of beginning the protocol, she was tolerating wearing her prosthesis
an average of 8 hours per day. She has return to important roles in her life, including that of
mother, with significant improvement in her quality of life.
One participant was unable to use her prosthesis due to complications of wound healing;
including negative pressure wound therapy and revision of the amputation to improve the shape
of her residual limb. After the eight week study, this 63 year-old Caucasian female was able to
fit and wear her prosthesis during her waking hours (12 hours per day). She has returned to
community participation tasks, particularly meaningful church attendance with significant
quality of life improvement.
Finally, a 62 year-old African American male was only able to tolerate wearing his
prosthesis for two hours per day due to phantom limb pain interfering with functional tasks.
Since completing the study's protocols, he is able to tolerate wearing his prosthesis for 12 hours
per day. This participant reports that he puts his prosthesis on in the morning when he gets up
and takes it off at night when he goes to bed, with increased participation in occupational roles
and routines greatly improved.
Limitations
Results of this study are limited primarily due to the small sample size, which decreases
the ability to generalize the findings of this study to the larger population of vascular amputees.
The variety of settings (acute, rehabilitation, home) in which the subjects used the treatment
protocol, is also a limitation, as this increases the number of external influences which may have
an effect on these results. The choice to use vascular amputees compared with traumatic
amputees, also increases the co-morbidities involved in this study. However, the positive results
of this study on subjects with more complex medical conditions - than might be typical of a
traumatic amputation, leads to further support the outcomes. Clearly, the same protocols need to
be applied to other amputee populations.
Another limitation was the relatively short length of time that individuals with acute
amputations tend to remain in acute care and in-patient rehabilitation settings, in which the
conditions can be closely monitored. Vidant Medical Center and Vidant Health serves 29
surrounding counties, therefore monitoring therapy conditions upon discharge from this facility
was challenging. The PI was diligent about educating therapists in an identical and systematic
manner so that those who would directly work the clients in home-health, out-patient, or
rehabilitation, were educated regarding the identified treatment protocols. Subjects were given
written instructions, a home-exercise program to follow upon discharge and follow-up calls
weekly by the PI, which assisted with compliance to the treatment protocol. It would seem that
the strategies implemented were effective, as results were evident for both groups of subjects –
even for a small sample.
A limitation may be that there was no control group of subjects without the Farabloc or
not using the mirror therapy. This is a significant limitation. It is possible that the subjects
improved simply because they were getting additional attention and motivated to improve.
However, the physical changes of the residual limb as well as the significant improvements in
the quality of life, particularly for the chronic group, seems to be more than can be expected
from any placebo effect, making this unlikely.
Summary and Conclusions
This study aimed to ascertain the effectiveness of using a combined treatment protocol of
eliminating electromagnetic fields by use of the Farabloc technology and the exercise program of
Mirror Therapy. The main hypothesis was that the combined treatment protocol would have a
more significant effect than either treatment in isolation. Decreasing edema and the discomfort
due to phantom limb pain would improve the functional activities and quality of life of vascular
amputees with lower extremity amputations. This was found to be true. A specific hypothesis
question was whether the intervention effects would remain after a four-week period of no
intervention (maintenance). Results varied between the acute and chronic subjects, but overall
the changes were maintained, if not improved, for all subjects, suggesting that the combined
intervention of the two treatments has a biological impact that will remain once intervention is
over. Further research will be needed to determine the ideal length of intervention.
Finally, the last hypothesis questioned the impact of the interventions on quality of life.
All the quantitative measures suggested that the subject's quality of life was improved.
However, the unexpected decrease of time between amputation and prosthetic fitting for those
with acute amputations has major implications for recovery of functional tasks and quality of
life. Even more significant was the resultant changes for the individuals with previous
amputations, who were either not wearing their prosthesis or wearing them for very limited
periods of time. For these five subjects, the increased tolerance and use of their prosthesis and
the impact this will have on their return to functional participation in their activities of daily
living, is substantial and noteworthy.
With the limitations of such a small sample, it will be critical to expand this study to a
larger population, using a multi-site study, randomly selected from a variety of geographic areas
increasing the reliability and generalizability of results. A double-blind cross-over design in
which placebo amputee limb covers could be compared to Farabloc amputee limb covers would
also be beneficial to decrease the placebo effect. Additionally, the use of the protocols with
traumatic amputees and upper extremity amputees would be beneficial.
Results of this study could have far reaching impact. If research continues show the same
results, an alternative treatment protocol to decrease the debilitating effects of PLP in amputees
would be established. This protocol provides a cost-effective, drug-free alternative to current
PLP treatments. This combined treatment protocol reduces PLP to the extent to which amputees
can increase participation in their activities of everyday life and subsequently improve their
QOL. Further, if the time between amputation and prosthetic fitting can be decreased, as it has in
this study, medical costs can be significantly reduced and function and quality of life for our
older adults with vascular disorders can be improved.
American Academy of Orthotics and Prosthetics.(2005). Pain management for the lower-limb
Amputee statistics by cause. Limb loss in the United States. (2008). Retrieved from
Amputee. (2009). In The American Heritage® Dictionary of the English Language (4th ed.) Arnstein, P. M. (1997). The neuroplastic phenomenon: a physiologic link between chronic pain
and learning.
The Journal of Neuroscience Nursing, 29, 179-186.
Bach, G. L. (1987). Farabloc™ in the Treatment of Phantom Pain, Rheumatic Pain and Other
Painful Symptoms.
Bach, G. L., & Clement, D. B. (2007, March). Efficacy of Farabloc as an analgesic in primary
fibromyalgia, 26(3), 405-410. DOI: 10.1007/s10067-006-0494-9
Bergner M, Bobbitt RA, Carter WB, Gilson BS. The Sickness Impact Profile: development and final revision of a health status measure.
Medical Care 1981; 19:787-805. Beaumont, G., Mercier, C., Michon, P.-E., Malouin, F., & Jackson, P. L. (2011, February).
Decreasing phantom limb pain through observation of action and imagery: a case series.
Pain Medicine, 12(2), 289-299.
Bordiushkov, I. N., Goroshinskaia, I. A., Frantsiiants, E. M., Tkacheva, G. N., Gorlo, E. I., &
Neskubina, I. V. (2000, Jan-Feb). Structural-functional changes in lymphocyte and erythrocyte membranes after exposure to alternating magnetic field.
Vopr Med Khim, 46(1), 72-80.
Broderick, J. E., Schneider, S., Schwartz, J. E., & Stone, A. A. (2010, June 11). Interference with
activities due to pain and fatigue.
Quality of Life Research, 19(8), 1163-1170.
Brodie, E. E., Whyte, A., & Waller, B. (2003, May 1). Increased motor control of a phantom leg
in humans results from the visual feedback of a virtual leg.
Neuroscience letters, 341(2), 167-169. DOI: 10.1016/S0304-3940(03)00160-5
Bultitude, J. H., &Rafal, R. D. (2009, December 6). Derangement of body representation in
complex regional pain syndrome: report of a case treated with mirror and prisms. Experimental brain research.
Byrne, K. P. (2011, May). Survey of phantom limb pain, phantom sensation and stump pain in
Cambodian and New Zealand amputees.
Pain Medicine, 12(5), 794-798.
Chan, B. L., Witt, R., Charrow, A. P., Magee, A., Howard, R., Pasquina, P. F., Heilman, K. M.,
& Tsao, J. W. (2007, November 22). Mirror Therapy for Phantom Limb Pain.
New England Journal of Medicine, 357(21), 2206-2207.
Chapman, S. (2011, January 12). Pain management in patients following limb amputation.
Nursing Standard, 25(19), 35-40.
Choudhury, A. (2009).
Statistical correlation. Retrieved January 15th, 2012, from Experimental
Cleeland, C. S., & Ryan, K. M. (1994, March). Pain Assessment: Global Use of the Brief Pain
Inventory. Annals, academy of medicine, Singapore, 23(2), 129-138. Retrieved from http://www.painknowledge.org/physiciantools/opioid_toolkit/components/Cleeland_Article.pdf
Clement, D. B., & Taunton, J. E. (2001, December). Alleviation of pain with the use of Farabloc,
an electromagnetic shield: A review.
British Columbia Medical Journal, 43(10), 573-577.
Colditz, J. C. (2011). Therapist's management of the stiff hand. In T. M. Skirven, L. Osterman, J.
M. Fedorczyk, & P. C. Amadia,
Rehabilitation of the hand and upper extremity, sixth edition (pp. 1021 - 1029). Philadelphia, PA: Mosby, Inc.
Conine, T. A., Hershler, C., Alexander, S. A., & Crisp, R. (1993).The Efficacy of Farabloc™ in
the Treatment of Phantom Limb Pain.
Canadian Journal of Rehabilitation, 6(3, 993), 155-161.
Cramer, J., Rosenheck, R., Xu, W., Henderson, W., Thomas, J., &Charney, D. (2001).Detecting
Improvement in Quality of Life and Symptomatology in Schizophrenia.
Schizophrenia Bulletin, 27, 227-234. Retrieved from http://schizophreniabulletin.oxfordjournals.org
Culver, A. (2009).
There is evidence showing mirror therapy to reduce phantom limb pain in
adult clients with lower limb amputations. Retrieved from http://commons.pacificu.edu/otpf/6
Darnall, B. D. (2009, January). Self-Delivered Home-Based Mirror Therapy for Lower Limb
Phantom Pain.
American journal of Physical Medicine and Rehabilitation, 88(1), 78-81. DOI: 10.1097/PHM.0b013e318191105b
Daut, R. L., Cleeland, C. S., & Flannery, R. C. (1983).Development of the Wisconsin Brief Pain
Questionnaire to assess pain in cancer and other diseases.
Pain, 17, 197-210.
Davis, K. D., Kiss, Z. H., Luo, L., Tasker, R. R., Lozano, A. M., &Drostrovsky, J. O. (1998,
January 22). Phantom sensations generated by thalamic microstimulation.
Nature, 391, 385-387. DOI: 10.1038/34905
Davis, R. W. (1993). Phantom sensation, phantom pain, and stump pain.
Archives of Physical
Medicine and Rehabilitation, 74, 79-91.
Dellemijn, P. (1999). Are opioids effective in relieving neuropathic pain?
Pain, 135, 453-462. Devor, M., & Seltzer, Z. (1999).Pathophysiology of damaged nerves in relation to chronic
pain.(4th ed.). Retrieved from http://www.sciencedirect.com
Devor, M., Janig, W., &Michaelis, M. (1994).Modulation of activity in dorsal root ganglion
neurones by sympathetic activation in nerve-injured rats.
Journal of Neurophysiology, 71(1), 38-47.
Doubell, T. P., Mannion, R. J., & Woolf, C. J. (1999). The dorsal horn: state-dependent sensory
processing, plasticity and the generation of pain.
Textbook of Pain, 4th edition, 165-181.
Draganski, B., Moser, T., Lummel, N., Ganssbauer, S., Bogdahn, U., Haas, F., & May, A.
(2006). Decrease of thalamic gray matter following limb amputation.
Neuroimage, 31, 951-957. DOI: 10.1016/j.neuroimage.2006.01.018
E-hand.com. (n.d.).
Complications in Hand Surgery. Retrieved March 11, 2012, from E-
Endolite USA. (n.d.). http://www.endolite.com/edu_glossary.php Ephraim, P. L., Wegener, S. T., Mackenzie, E. J., Dillingham, T. R., &Pezzin, L. E. (2005).
Phantom pain, residual limb pain, and back pain in amputees: results of a national survey.
Archives of Physical Medicine and Rehabilitation, 86, 1910-1919.
Evans, F. J. (1974). The placebo response in pain reduction.
Advances in Neurology, 4, 289-296. Fabry Registry. (2004-2010). Brief Pain Inventory. Retrieved from
Farabloc. (1993). http://www.farabloc.com/mUBC.html Farabloc Development Corporation. (2012, February 29).
Farabloc Development Corporation.
Retrieved March 1, 2010, from Farabloc Development Corporation Web site: www.farabloc.com
Flor, H. (2002). Phantom-limb pain: characteristics, causes, and treatment .
The Lancet
Neurology, 1, 182-189.
Flor, H. (2008). Maladaptive plasticity, memory for pain and phantom limb pain: review and
suggestions for new therapies. Expert Review of Neurotherapeutics, 8(5), 809-818.
Flor, H., Elbert, T., Knecht, S., Wienbruch, C., Pantev, C., Birbaumer, N., Larbig, W., &Taub, E.
(1995, June 8). Phantom-limb pain as a perceptual correlate of cortical reorganization following arm amputation.
Nature, 375(6531), 482-484.
Flor, H., Elbert, T., Muhlnickel, W., Pantev, C., Wienbrusch, C., &Taub, E. (1998).Cortical
reorganization and phantom phenomena in congenital and traumatic upper-extremity amputees.
Experimental Brain Research, 119, 205-212.
Florence, S. L., &Kaas, J. H. (1995). Large-scale reorganization at multiple levels of the
somatosensory pathways follows therapeutic amputation of the hand in monkeys.
Journal of Neuroscience, 15, 8083-8095.
Giuffrida, O., Simpson, L., & Halligan, P. W. (2010). Contralateral Stimulation, using TENS, of
phantom limb pain: two confirmatory cases.
Pain Medicine, 11(1), 133-141.
Giummarra, M. J., & Bradshaw, J. L. (2010). The phantom of the night: restless leg syndrome in
amputees.
Medical Hypotheses, 76, 967-972. DOI: 10.1016/j.mehy.2009.12.009
Glasauer, F. E. (2001). Restless legs syndrome.
Spinal Cord, 39(3), 125-133. Gudin, J. A. (2004). Expanding our understanding of central sensitization.
Medscape Neurology
& Neurosurgery, 6(1).
Halbert, J., Crotty, M., & Cameron, I. D. (2002, March/April).
Evidence for the Optimal
Management of Acute and Chronic Phantom Pain: A Systematic Review, 18(2), 84-92.
Halligan, P. W., Zeman, A., & Berger, A. (1999, September 4). Phantoms in the brain - question
the assumption that the adult brain is "hard wired".
British Medical Journal, 319(7210), 587-588.
Hanling, S. R., Wallace, S. C., Hollenbeck, K. J., Belnap, B. D., &Tulis, M. R. (2010, February).
Preamputation mirror therapy may prevent development of phantom limb pain: a case series.
Anesthesia & Analgesia, 110(2), 611-614.
Harden, R. N., Houle, T. T., Green, S., Remble, T. A., Weinland, S. R., Colio, S., Lauzon, J.,
&Kuiken, T. (2005, March). Biofeedback in the treatment of phantom limb pain: A time-series analysis.
Applied Psychophysiology and Biofeedback, 30(1), 83-93. DOI:10.1007/s 10484-005-2177-8
Hareendran, A., Doll, H., Wild, D., Moffatt, C., Musgrove, E., Wheatley, C., & Franks, P.
(2007). The venous leg ulcer quality of life (VLU-QoL) questionnaire: development and psychometric validation.
Wound Repair and Regeneration, 15, 465-473.
Harlfinger, O. (1991). Weather-induced effects on pain perception.
Fortschr Medical Journal,
109, 647-650.
Harness, N., &Pinzur, N. S. (2001). Lower Extremity - Health Related Quality of Life in Patients
with Dyvascular Transtibial Amputation.
Clinical Orthopaedics and Related Research, 383, 204-207. DOI: 10.1097/00003086-20010200-00023
Harris, A. J. (1999, October 23). Cortical origin of pathological pain.
The Lancet, 354(9188),
Harrison, T. (2011, March).
Minnesota Medicine. Retrieved February 29, 2012, from Minnesota
Health, N. I. (2011, August 10).
Peripheral Neuropathy Fact Sheet. Retrieved March 17, 2012,
from National Institute of neurological disorders and stroke: http://www.ninds.nih.gov/disorders/peripheralneuropathy/detail_peripheralneuropathy.htm
Helm, S., II (2008). Retrieved from
Henson, R. A. (1977). Henry Head: his influence on the development of ideas on sensation.
British Medical Bulletin, 33,doi: Retrieved from www.nejm.org
Henson, R. A. (1977, May). Henry Head: his influence on the development of ideas on sensation.
British Medical Bulletin, 33(2), 91-96.
Hill, A. (1999). Phantom limb pain: A review of the literature on attributes and potential
mechanisms.
Journal of Pain and Symptom Management, 17(2), 125-142.
Hjermstad, M., Fayers, P., Haugen, D., Caraceni, A., Hanks, G., Loge, J., et al. (2011, June).
Studies Comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for Assessment of Pain Intensity in Adults: A Systematic Literature Review.
Journal of Pain and Symptom Management, 41(6), 1073-1093.
Huff, E., Ledoux, W., Berge, J., & Klute, G. (2008). Measuring Residual Limb Skin
Temperatures at the Skin-Prosthesis Interface.
American Academy of Orthotists and Prosthetists, 20(4), 170-173.
Jamison, R. N. (1996). Influence of Weather on Report of Pain [Newsletter]. Boston,
Massachusetts: International Association for the study of pain. Technical corner of IASP newsletter (http://www.iasp-pain.org/AM/Template.cfm?Section=Home&Template=/CM/ContentDisplay.cfm&ContentID=2201), Harvard Medical School.
Jensen, T. S., Krebs, B., Nielsen, J., & Rasmussen, P. (1985). Immediate and long-term phantom
pain in amputees: incidence, clinical characteristics, and relationship to pre-amputation pain.
Pain, 21(3), 267-78.
Jensen, T. S., Wilson, P. R., & Rice, A. S. (2002).Clinical Pain Management: Chronic Pain.
Kalso, E., Tasmuth, T., &Neuvonen, P. J. (1996). Amitriptyline effectively relieves neuropathic
pain following treatment of breast cancer.
Pain, 64(2), 293-302.
Karl, A., Birbaumer, N., Lutzenberger, W., Cohen, L. G., &Flor, H. (2001, May 15).
Reorganization of Motor and Somatosensory Cortex in Upper Extremity Amputees with Phantom Limb Pain.
Journal of Neuroscience, 21(10), 3609-3618.
Katz, J., & Melzack, R. (1991). Auricular transcutaneous electrical nerve stimulation (TENS)
reduces phantom limb pain.
Journal of Pain and Symptom Management, 6, 73-83.
Keil, G. (1990). Sogenannteerstbeschreibung des phantomschmerzes von Ambroise Pare.
Fortschritte der Medizin, 108, 62-66. Retrieved from http://bja.oxfordjournals.org/cgi/content/full/87/1/10
Klute, G., Berg, J., Biggs, W., Pongnumkul, S., Popovic, C., & Curless, B. (2011, October).
Vacuum-assisted socket suspension compared with pin suspension for lower extremity amputees: effect on fit, activity, and limb volume.
Archives of Physical Medicine and Rehabilitation, 92(10), 1570 - 1575.
Lacy, C. F., Armstrong, L. L., Goldman, M. P., & Lance, L. L. (Eds.). (2010). Lexi-Comp's
Drug Information Handbook 2010-2011: A Comprehensive Resource for All Clinicians and Healthcare Professionals (19th ed.). Hudson, Ohio: Lexi-Comp, Inc.
Legro, M. W., Reiber, G. D., Smith, D. G., Del Aguila, M., Larson, J., & Boone, D. (1998,
August). Prosthesis Evaluation Questionnaire for persons with lower limb amputations: assessing prosthesis-related quality of life.
Archives of Physical Medicine and Rehabilitation, 79, 931-938.
Leskowitz, E. (2009, April). Energy medicine perspectives on phantom-limb pain.
Alternative
and Complimentary Therapies, 15(2), 59-63. DOI: 10.1089/act.2009.15210
Livingston, W. K. (1943).
Pain mechanisms: A Physiologic Interpretation of Causalgia and Its
Related Status. New York: Macmillan.
Lotze, M., Flor, H., Grodd, W., Larbig, W., &Birbaumer, N. (2001).Phantom movements and
pain.An fMRI study in upper limb amputees.
Brain, 124, 2268-2277.
Lotze, M., Grodd, W., Birbaumer, N., Erb, M., Huse, E., & Flor, H. (1999). Does use of
myoelectric prosthesis prevent cortical reorganization and phantom limb pain?
Nature Neuroscience, 2(6), 501-502.
MacIver, K., Lloyd, D. M., Kelly, S., Roberts, N., &Nurmikko, T. (2008).Phantom limb pain,
cortical reorganization and the therapeutic effect of mental imagery.
Brain a Journal of Neurology, 131, 2181-2191. DOI: 10.1093/brain/awn124
MacLachlan, M., Desmond, D., &Horgan, O. (2003, January/February). Psychological correlates
of illusory body experiences.
Journal of Rehabilitation Research & Development, 40(1), 59-66.
MacLachlan, M., McDonald, D., &Waloch, J. (2004, July 22 - August 4). Mirror treatment of
lower limb phantom pain: a case study.
Disability & Rehabilitation, 26(14-15), 901-904.
Maihofner, C., Handwerker, H. O., Neundorfer, B., &Birklein, F. (2004).Cortical reorganization
during recovery from complex regional pain syndrome.
Neurology, 63, 693-701.
Manchikanti, L., & Singh, V. (2004).Managing Phantom Pain.
Pain Physician, 7, 365-375. McDiarmid, S., & Trudeau, M. (1998).A Study of the Electromagnetic Properties of Farabloc . McQuay, H. J., & Dickerson, A. H. (1990).Implications of nervous system plasticity for pain
management.
Anaesthesia, 45, 101-102.
Melzack, R. (1971). Phantom limb pain: implications for treatment of pathologic pain.
Anaesthesiology, 35, 409-419.
Melzack, R. (1975). The McGill PainQuestionnaire: major properties and scoring methods.
Pain,
Melzack, R. (1990). Phantom limbs and the concept of a neuromatrix.
Trends in Neurosciences,
13, 88-92.
Melzack, R. (1992). Phantom limbs.
Science America, 266, 120-126. Miller, M. D., & Rodriquez, J. E. (2010, January). What is the best nonpharmacologic therapy
for phantom limb pain?
Evidence-based Practice, 13(1), 7.
Mitchell, S. W. (1871). Phantom limbs.
Lippinscott's Magazine of Popular Literary Science, (8),
Mohamad, H., Ebrahimzadeh, M. H., & Hariri, S. (2009, June). Long-term outcomes of
unilateral transtibial amputations.
Military Medicine, 174(6), 593-597.
Morley-Forster, P. K. (2009, Dec). The vexing problem of post-amputation pain: what is the
optimal perioperative pain management for below-knee amputation?
Canadian Journal of Anesthesia, 56(12), 908-913.
Neuroma.(2007). In Merriam-Webster's Medical Dictionary.
Nikolajsen, L., & Jensen, T. S. (2001). Phantom limb pain.
British Journal of Anaesthesia, 87(1),
Nikolajsen, L., Ilkjaer, S., Kroner, K., Christensen, J. H., & Jensen, T. S. (1997). The influence
of preamputation pain on postamputation stump and phantom pain.
Pain, 72, 393-405.
Nixdorf, D. (2012).
The Clinic. Retrieved March 10, 2012, from Dr.Don Nixdorf, D.C.:
North Carolina Diabetes Prevention and Control Program.(n.d.).
Impact of Diabetes. Retrieved
Ottaviani, G., Robert, R. S., Huh, W. W., & Jaffe, N. (2009). Functional, psychological and
professional outcomes in long-term survivors of lower-extremity osteosarcomas: amputation versus limb salvage.
Pediatric and Adolescent Osteosarcoma, cancer treatment and research, 152, 421. DOI: 10.1007/978-1-4419-0284-9_23
Parkes, C. M. (1973).Factors determining the persistence of phantom limb pain in the amputee.
Journal of Psychosomatic Research, 17, 97-108.
Pilla, A. A. (2002). Low-intensity electromagnetic and mechanical modulation of bone growth
and repair: are they equivalent?
Journal of Orthopedic Science, 7(3), 420-428.
Prosthetic Evaluation Questionnaire Evaluation Guide. (1998). Retrieved from http://www.prs-
Protopathic pain. (2009). In The American Heritage® Dictionary of the English Language. (4th
Ramachandran, V. S., & Rogers-Ramachandran, D. (1996).Synaesthesia in phantom limbs
induced with mirrors.
Proceedings of the Royal Society of Biological Sciences, 263, 377-386.
Ramachandran, V., &Hirstein, W. (1998).The perception of phantom limbs.
Brain, 121, 1603-
Rossi, S., Tecchio, F., &Pasqualetti, P. (2002).Somatosensory processing during movement
observation in humans.
Clinical Neurophysiology, 113, 16 - 24.
Rossi, S., Tecchio, F., Pasqualetti, P., Ulivelli, M., Pizzella, V., Romani, G. L., Passero, S.,
Rossini, P. M. (2002).Somatosensory processing during movement observation in humans.
Clinical Neurophysiology, 113, 16-24.
Schumacher, K. L., Koresawa, S., West, C., Dodd, M., Paul, S. M., Tripathy, D., Koo, P.,
&Miaskowski, C. (2002, October). The usefulness of a daily pain management diary for
outpatients with cancer-related pain.
Oncology Nursing Forum, 29, 1304-1313. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12370700
Shacham S. A shortened version of the Profile of Mood States. J Pers Assess 1983;47:305-6. Sherman, .A., & Sherman, C. J. (1983).Prevalence and characteristics of chronic phantom limb
pain among American veterans.
American Journal of Physical Medicine, 62, 227-238.
Sherman, R. A. (1989). Stump and phantom limb pain.
Neurologic Clinics, 7, 249-264. Sherman, R. A. (1994, January). Phantom limb pain. Mechanism-based management.
Clinics in
Podiatric Medicine and Surgery, 11(1), 106.
Sherman, R. A. (1997). Phantom pain. Retrieved from http://www.iasp-
Sherman, R. A., Sherman, C. J., & Parker, L. (1984). Chronic phantom and stump pain among
American veterans: results of a survey.
Pain, 18, 83-95.
Sherman, R. A., Sherman, C. J., & Parker, L. (1984).Concurrent variation of burning phantom
limb and stump pain with near surface blood flow in the stump.
Orthopedics, 10, 395-401.
Sherman, R., Sherman, C., & Gall, N. (1980).A survey of phantom limb pain treatment in the
United States.
Pain, 8, 85-89. DOI: 10.1016/0304-39599(80)90092-5
Shutty, M. S., Cunduff, G., &DeGood, D. E. (1992). Pain complaint and the weather: weather
sensitivity and symptom complaints in chronic pain patients.
Pain, 49, 199-204.
Simmons, Z., & Feldman, E. (2000, Summer). The pharmacological treatment of painful diabetic
neuropathy.
Clinical Diabetes, 18(3).
Sindrup, S. H., & Jensen, T. S. (1999). Efficacy of pharmacological treatments of neuropathic
pain: an update and effect related to mechanism of drug action.
Pain, 83, 389-400.
Skidmore, F. M., Drago, V., Foster, P. S., &Heilman, K. M. (2009). Bilateral restless legs
affecting a phantom limb, treated with dopamine agonists.
Journal of Neurology, Neurosurgery and Psychiatry, 5, 569-570.
Stannard, C., Kalso, E., & Ballantyne, J. (2010).
Evidence-based Chronic Pain Management.
Hoboken, NJ, USA: Blackwell Publishing Ltd.
The Free Dictionary.(n.d.). http://www.thefreedictionary.com/phantom+limb+pain
Title of measure: The Brief Pain Inventory. (2007). Retrieved from
Wall, P. D., &Gutnick, M. (1974). Ongoing activity in peripheral nerves: The physiology and
pharmacology of impulses originating from a neuroma.
Exploratory Neurology, 43, 580-593.
Waxman, S. G. (1999). The molecular pathophysiology of pain: abnormal expression of sodium
channel genes and its contributions to hyperexcitibility of primary sensory neurons.
Pain Supplement, 6, 133-140.
Weeks, S. R., & Tsao, J. W. (2010). Incorporation of another person's limb into body image
relieves phantom limb pain: a case study.
Neurocase, 16(6), 461-465.
Wewers, M., Lowe, N., & Crichton, N. (1990). A critical review of visual analogue scales in the
measurement of clinical phenomena.
Research in Nursing and Health, 13, 227-236.
World Health Organization. (2007).
Electromagnetic Fields: Extremely low frequency fields.
Environmental health criteria monograph No. 238. Geneva: WHO Press.
Yuh, T. C., Fisher, D. J., Shields, R. K., &Ehrhardt, J. C. (1992). Phantom limb pain induced in
amputee by strong magnetic fields.
Journal of Magnetic Resonance Imaging,
2, 221-223. DOI: 10.1002/jmri.1880020216
Zhang, J., Clement, D., & Taunton, J. (2000, January).The efficacy of Farabloc, an
electromagnetic shield, in attenuating delayed-onset muscle soreness.
Clinical Journal of Sports Medicine, 10(1), 15-21.
contralateral limb. (2008). In The Free Dictionary. Retrieved from http://www.thefreedictionary.com/contralateral
APPENDIX A
IRB or IACUC approval letters - required if human subjects or animals are used
UNIVERSITY AND MEDICAL CENTER INSTITUTIONAL REVIEW BOARD
HUMAN BIOMEDICAL INTERNAL PROCESSING FORM
SUBMISSION FOR UMCIRB REVIEW
FULL AND EXPEDITED RESEARCH
Please note: For studies that involve greater than minimal risk, this application must be accompanied by a research protocol. For a template to assist in developing such a document, go to
DEMOGRAPHIC INFORMATION Type of application:
Modification Date form was completed: 8/20/2010
1.Title of proposed research (this title must match protocol, funding application and consent form):
The effectiveness of Farabloc technology with Mirror Therapy in reducing phantom limb pain in individuals with an acute lower extremity vascular amputation.
a. PI Name, Degree(s) Name: Helen Houston, OTR/L, ECU graduate student b. Degrees/Credentials:
Bachelor of Science in Occupational Therapy completed in 1993. Presently enrolled in Masters of Science (post-professional) in Occupational Therapy, ECU.
UHS Employee/Agent
d. Department, Section, School or College:
Department of Occupational Therapy, College of Allied Health Sciences, East Carolina University
Address: 305 Club Pines Drive, Greenville, NC, 27834
e. E-mail address:
[email protected]
Telephone #: (252) 531-8993
2.Contact Person
a. Name: Helen Houston
b. Department, Section, School or College: Department of Occupational Therapy, ECU
c. E-mail address:
[email protected]
Telephone #: (252) 531-8993
Note: You now should list all key personnel (which includes sub-investigators) on Question 34, along with their credentials, responsibilities and their signatures. 3.List all items related to this research study submitted for UMCIRB review and approval: Consent form, Institutional Approval for Research Form 4.SOURCE OF FUNDING
No funding Institution or Department Sponsor, Name: Government Agency, Name:
Grant: include 3 copies of the final grant application for full committee reviews or 1 copy for expedited
Private Agency, Name:
Materials for study donated to Principal Investigator by Farabloc Development Corporation
5.Fund number for IRB fee collection (applies to all for-profit, private industry or pharmaceutical company sponsored projects): N/A
Activity (optional)
NOTE: The UMCIRB Conflict of Interest Disclosure Form needs to be submitted for expedited and full review.
6. CHECK ALL INSTITUTIONS OR SITES WHERE THIS RESEARCH STUDY WILL BE
East Carolina University
Beaufort County Hospital
Vidant Medical Center
Carteret General Hospital
Heritage Hospital
Boice-Willis Clinic
NOTE: Those research studies utilizing Pitt County Memorial Hospital resources, Brody School of Medicine resources or involving ionizing radiation should complete th 7.CHECK THE FOLLOWING INVOLVED IN THIS STUDY:
Population Specifically Targeted
Methods/Procedures
Normal volunteers
Surveys / Questionnaires
Adults (> 18 yrs old)
Minors (< 18 yrs old)
Standardized Written / Oral / Visual Tests
Institutionalized Participants
Videotaping / Voice Recording / Photography
Inpatient participants
Pregnant Participants
Participants of child bearing potential
Medical Devices
Embryos or fetuses
Sterile Surgical / Invasive Procedures
Non-sterile Invasive Procedures
Wards of the State
Surgical or otherwise discarded Tissue/Samples
Autopsy or cadaver tissue
Non-English speaking
Therapeutic Radiation
Desperately / Terminally Ill Participants
Diagnostic Radiation
Traumatized/Comatose Participants
Banking of biological materials
Communicable Disease
Genetic testing
Outpatient participants
International research
Registry / Database
Cognitively or emotionally impaired
Recombinant DNA / Gene Transfer Technology
INVESTIGATIONAL TEST ITEMS 8.Does your proposal involve investigational drugs?
9.Does your proposal involve approved drugs for non-approved uses?
10.Does this proposal have an IND
b. Manufacturer:
c. IND No: d. IND Filing date: e. Drug study phase:
11.Does your proposal involve investigational devices, instruments, machines?
12.Is this device exempt from the requirements of 21CFR812?
13.Does your proposal involve approved devices for non-approved uses?
14.Is this a significant risk (SR) device?
15.Does this proposal have an IDE?
a. Name: b. Manufacturer:
c. IDE No., device study type: d. Device study phase: e. Provide the FDA letter of SR/NSR designation or the sponsor letter of risk designation. f.
Attach a copy of the FDA approval letter of the IDE.
RESEACH RISK AND LEVEL OF REVIEW REQUIRED 16.Research participants will be placed at as defined below:
No more than minimal risk More than minimal risk
Minimal risk means that the probability and magnitude of harm or discomfort anticipated in the research are not greater in and of themselves than those ordinarily encountered in daily life or during the performance of routine physical or psychological examinations or tests.he definition for prisoners differs and is located 17.What level of review does your proposal require?
RESEARCH QUESTIONS
18. Subject Selection
a. Describe how participants will be selected or recruited for the research, including enrollment procedure. All acute individuals that are scheduled for amputation will be considered for selection. Chronic amputees reporting phantom limb pain will also participate. If the individual meets the inclusion/exclusion criteria, the PI will be notified. The PI will speak to the potential subject, explaining all elements of the study and secure a consent form, if the individual agrees to participate. Enrollment will include signing of consent forms and explanation of risks and benefits of study. b. Identify the projected number of participants to be enrolled. 60 subjects c. Outline the inclusion and exclusion criteria for this research study.
Inclusion criteria: individuals who are 19 years of age or older, able to comprehend, read and write in English, and understand the use of a visual analogue scale. The study is targeting individuals who have undergone a recent (less than 6 weeks) unilateral, above or below knee amputation due of vascular insufficiency with a minimum of 15cm of residual femur or tibia remaining over which an amputee limb cover can be placed and chronic amputees (more than 6 weeks previously), who report phantom limb pain. Exclusion criteria: individuals with one or more of the following types of amputations: bilateral lower extremity; upper extremity; guillotine (delayed closure due to risk of infection), hip disarticulation, foot, partial foot and toe amputation and individuals pending revision surgeries.
Individuals will also be excluded if they:
are involved in a compensation claim; have a diagnosis of neurological or psychological disorder that would interfere with the study; require dialysis as this is often associated with an increase in cognitive deficits and fluctuating medical status;
have a known uncontrolled systemic disease (i.e., cancer, lupus etc.); have current substance abuse or dependence; are unable to provide written consent and written authorization for use or release of health and research study
have a prior history of vertebral disc disease/condition, sciatica or radiculopathy;
are unable to follow study instructions and or are unlikely to complete all required visits;
are participating in another investigational drug or device study for phantom limb pain or have participated in
these studies 30 days immediately prior to study enrollment;
have any condition or situation that, in the investigator's opinion, may put the subject at significant risk,
confound the study results, or interfere significantly with the subject's participation in the study.
are taking anti-seizure/ neuropathic pain medications which exceed maximum recommended daily dosages e.g.
Lyrica 450mg/day, Cymbalta 60 mg/day or Neurontin levels 3600mg/day. c. Provide a justification for the sample size selected.
There will be two experimental groups of a minimum of five subjects each. For statistical analysis, there needs to be 30 subjects in each group, so the minimum of subjects needed for the study are 60 subjects who complete the study.
d. Describe the safeguards in place to protect the rights and welfare of any vulnerable participants enrolled in
this research study. If there is a subject that is vulnerable, for example, not able to understand the purpose and process of the study due to cognitive deficits, the PI will not enroll them in the study. The exclusion criteria is extensive, in part to protect the subjects that have complex medical needs and therefore should not participate.
19. Are there any advertisements (public display in written, radio, or TV form) for participant recruitment?
No If yes, attach the advertisements to the processing form.
20. Does the research include any monetary inducements, compensation or reimbursement for participation in this
No If yes, attach the payment schedule to the processing form or provide specific protocol
21. Will the sponsor reimburse for any items or procedures or supply any items at no cost involved in this research
If yes, attach written documentation of the items that will be reimbursed or
supplied by the sponsor unless this information is specifically noted in the research protocol.
See Attachment 22. Are there any associated costs that participants will incur as a result of participating in this research study?
No If yes, describe these costs.
23. Risk Determination Describe the research setting, listing any safeguards in place for participant safety. Research will be initiated for the acute group, while amputees are inpatients in the acute care setting of Vidant Medical Center, or after six weeks for the chronic group. All subjects participating, regardless of group placement, will meet or exceed standards of care.
According to current amputee treatment protocol, all amputees receive occupational therapy or physical
therapy evaluation and treatments, beginning on post-operation day one, per current treatment protocol. This protocol includes the evaluation of current functional level and education as usually addressed on the current amputee treatment protocol. The education is described in a booklet issued to all amputee patients. It explains the care of residual limb, desensitization techniques for residual limb, donning stump-liner and stump shrinker, activities of daily living, mobility and functional transfers, assessment for need of durable medical equipment or assistive devices in preparation for discharge, as well as appropriate exercises for upper extremity exercises and lower extremities. For subjects in the intervention groups, they will get additional occupational therapy intervention. This intervention has proven to be effective treatment, and does not have any known risks. As with any patient seen by therapists, any patient that shows illness or post-surgical complications will be brought to immediate attention of the medical staff. 24. Risk Determination
a. Describe all foreseeable physical, psychological, economic, social, legal and dignitary risks to the
participants, with steps outlined to minimize those risks. Risks should be described in terms of probability or likelihood, magnitude and duration when possible. There are no foreseeable risks involved with this study, as all subjects will adhere to the traditional treatment protocol.
b. Outline the mechanism for reporting adverse events or unanticipated risks to participants or others for this
study. If any adverse events or unanticipated risks become evident, these will be reported to current participants via telephone contact and appropriate modifications will be made, with IRB approval, in order to continue with the study.
c. Specifically address any risk associated with the use of placebo, if applicable.
25. Data/Safety Monitoring:
a. Describe any additional data monitoring challenges when the principal investigator or another research
team member is not directly involved in data collection or monitoring because they are not available on the research site. Once participants have been discharged from the hospital they will be monitored by home-health, skilled nursing or outpatient therapists. These therapists will be contacted via telephonic means by the primary investigator and will receive written instructions via e-mail. These therapists will be educated regarding monitoring of participants compliance with the treatment protocol. The primary investigator will remain in telephonic contact with participants to ensure adherence to study protocols. At four, and eight weeks the primary investigator will meet with the participants to monitor safety and collect data. Subjects will meet with their physicians at four, and eight weeks for medical monitoring, per the current treatment protocol.
b. Describe the data monitoring plan according to Good Clinical Practices (and Data Safety Monitoring
Board/Committee, if applicable) to ensure safety of subjects. All data will be stored in a locked location in the occupational therapy department at East Carolina University and the Occupational Therapy department at Vidant Medical Center, to ensure that participant confidentiality is adhered to. Data and personal participant identifiers will be separated.
26. Anticipated Benefits
a. Describe the benefits of the research study to participants or others.
Participants of this study may benefit in that they may not develop phantom limb pain after amputation, or that it may be minimized due to this treatment protocol. If an effective combined protocol is developed due to the results of this study, others will benefit as they will not experience phantom limb pain or it may be able to be reduced due to this treatment intervention post-amputation surgery, thereby improving quality of life and potential to increase participation in activities of daily living.
27. Data Confidentiality and Subject Privacy
a. Describe how confidentiality will be maintained by providing details about the storage facility, duration of
storage, data destruction method, and persons with access to the data.
All data will be kept in a locked drawer within the PI's work office or within ECU's Department of Occupational Therapy thesis director's office. Data will be stored for three years and after this time data will be shredded using the professional shredding services provided at Pitt County Memorial Hospital. The only people with access to the data will be the PI, the thesis director, and the review committee. Results of the study will be shared with the sponsor.
b. How will subject privacy be maintained during recruitment, data collection and data analysis?
All names will be eliminated from the documentation except for the consent form. An ID number will be assigned and used for identification.
c. If the participants' data or samples will be used for future research, describe how their privacy will be
protected. Only ID numbers will be used.
d. Describe any additional safeguards in place to manage illegal, significantly intimate or potentially
embarrassing information gathered in this research study.
There is no obvious intimate or embarrassing information that is being collected. Nevertheless, all will be adequately supervised and secured.
e. Include steps to handle information that requires mandatory reporting to officials, for example physical
abuse, emotional abuse or health problems.
The PI is an employee of Vidant Medical Center and will follow all mandatory reporting as required by the facility.
If the research study involves HIV testing, describe the plans for pre/post-test counseling and other related considerations. N/A
28. Obtaining Consent or Parental Permission:
Describe the consent process, including members of the research team that will be obtaining informed consent from study participants. a. The PI will speak to the potential subject, explaining all elements of the study and secure a consent form, if
the individual agrees to participate. Enrollment will include signing of consent forms and explanation of risks and benefits of study.
b. Describe the setting in which the consent will be obtained.
Inpatient acute care setting at Vidant Medical Center and Eastern NC Amputee Support Group
c. Describe the process to minimize undue influence and coercion during the consent process.
The risks and benefits of participating will be explained to individuals who meet inclusion/exclusion criteria, however all individuals will continue with traditional treatment protocol irrespective of whether they participate in this research study or not.
d. Outline procedures for obtaining informed consent from participants with limited or low literacy.
One of the inclusion criteria for this study includes the ability to comprehend, read and write in English, and understand the use of a visual analogue scale. Subjects with limited or low literacy will thereby not be included as these skills are required to be able to complete the daily log and Brief Pain Inventory surveys daily.
e. Describe the process for determining cognitive impairment or other conditions that may make a participant
more vulnerable. Due to the extensive exclusion criteria for this study, individuals with cognitive impairments or other conditions which may make a participant vulnerable will not be included in this study.
f. Describe the process for identifying the legally authorized representative and the process to debrief and
subsequently obtain consent from the study participant, when feasible.
Individuals that meet inclusion and exclusion criteria will be adults, without cognitive deficits and will be able to represent themselves, so legal representatives will not be applicable.
29. Assent Related Issues for children: NA
a. Describe the assent processes given the range of ages intended for this research study. b. If a separate assent is not being used, how will assent be documented? c. How will custody changes during participation in the study be determined? d. Describe the processes as required for enrolling wards of the state if they are a target population for this
study. Note: If a child becomes a ward of the state, the IRB must be notified immediately to seek advice on further protections that may be required.
a. The current state of knowledge surrounding the research questions to be addressed in this study.
Phantom limb pain (PLP) is an extremely debilitating and complicated phenomenon which can limit
participation in daily life activities throughout the life of an individual with an amputation. The purpose of this study is to explore the effect of combining two therapies, Farabloc technology with Mirror Therapy, in order to decrease the experience of PLP for acute, unilateral, lower extremity vascular above or below knee amputees. Farabloc technology uses a fabric that is woven with fibers of extremely fine steel and nylon which has significant shielding effects on high frequency electromagnetic fields (greater than 1MHz) (Bach & Clement, 2007). When wrapped around a post amputation residual limb, Farabloc therapy has been demonstrated to have a favorable effect on PLP (Conine, Hershler, Alexander, & Crisp, 1993). Mirror Therapy uses a mirror placed between the amputated and non-amputated limb, in which the non-amputated limb is observed while performing bilateral synchronous exercises, such that it appears that both limbs are intact. Mirror Therapy has been shown to significantly reduce phantom limb pain in individuals with an amputation (Chan et al., 2007). By combining the two therapies, this study will investigate whether phantom limb pain experienced by acute above/below knee amputees can be prevented or reduced in frequency, intensity or duration compared with chronic amputees. This study is unique as a combined intervention strategy. The expectation is that the results of this study will provide a cost-effective, drug-free alternative to current phantom limb pain treatments and may prevent or
reduce phantom limb pain to the extent to which amputees could increase participation in their activities of everyday life. References: Bach, G. L., & Clement, D. B. (2007, March).
Efficacy of Farabloc as an analgesic in primary fibromyalgia,
26(3),
Chan, B. L., Witt, R., Charrow, A. P., Magee, A., Howard, R., Pasquina, P. F., Heilman, K. M., & Tsao, J. W.
(2007, November 22). Mirror Therapy for Phantom Limb Pain.
New England Journal of Medicine,
357(21), 2206-2207.
Conine, T. A., Hershler, C., Alexander, S. A., & Crisp, R. (1993).The Efficacy of Farabloc™ in the Treatment of
Phantom Limb Pain.
Canadian Journal of Rehabilitation,
6(3, 993), 155-161.
b. Describe the uncertainty to be addressed by this research study (research question).
Once phantom limb pain pathways have been established they appear more difficult to eradicate and treat, therefore, it is critical to address the issue of phantom limb pain early in the process, soon after the amputation. There is strong evidence that Farabloc is effective in treating phantom limb pain and Mirror Therapy research has been demonstrated to reduce phantom limb pain in upper as well as lower extremity amputees, but they have only been studied separately. Thus, the purpose of this study is to investigate if the combined use of Farabloc and Mirror Therapy treatment protocol will reduce the experience of phantom limb pain and increase the quality of life for amputees with an acute lower limb above or below knee amputation. The hypothesis is that a treatment protocol that targets external (peripheral) and internal (central) neuronal mechanisms simultaneously is likely to be able to reduce phantom limb pain more substantially than either treatments alone, particularly when used as an early intervention. The specific research questions will be:
By using a combined Farabloc Therapy and Mirror Therapy treatment protocol in the acute phase after
surgery, can PLP be reduced or prevented in individuals who have a unilateral, above or below knee amputation when compared to the same treatment protocol used in chronic amputees (more than six weeks post-operatively)?
Will any intervention effects be maintained after a four week maintenance period? Is a reduction in PLP associated with an increased in participation in activities of daily living, or an
increased quality of life? c. Describe the rationale for the type of research design chosen for this study.
A repeated-measures, experimental design has been chosen for this study. There are two experimental
groups- with subjects assigned to the acute group if the amputation occurred less than six weeks previously and to the chronic group if the date of the amputation occurred more than six weeks previously. Both groups will receive the traditional amputee treatment protocol. Both groups will also receive the experimental protocol combining Farabloc Therapy and Mirror Therapy for four weeks. After the four week intervention, each subject received no experimental intervention for four weeks.
RESEARCH ABSTRACT
Phantom limb pain (PLP) is significant for amputees since its occurrence can be as high as 90% and is
overwhelming and debilitating to those who experience it. Numerous treatment options have been studied, with some success. The purpose of this study will be to examine an effective treatment protocol to decrease PLP with acute amputation individuals using two relatively new and innovative therapies in combination. This study proposes combining two effective treatments 1) preventing the overstimulation of raw nerve endings from external sources, by providing an electromagnetic shielding fabric in the form of an amputee limb cover (Farabloc technology), and 2) reorganizing the sensory cortex internally, using Mirror Therapy, hypothesizing that this protocol will decrease or even prevent the experience of PLP in post-surgical lower extremity amputees by treating PLP limb pain from these two combined sources.
Key Personnel: Each key personnel must certify the following by signing below:
a. I acknowledge my responsibilities in the conduct of this research study and have received adequate
training to fulfill those responsibilities.
b. I agree to follow the procedures for the conduct of this study as described in the IRB approved
c. I agree to uphold the rights and welfare of all study participants.
Responsibilities
– select all that
b,d,e,i,j,l,m,n,o
Graduate student
prosthetist: c,d,n
Responsibilities of key personnel:
a. Screens potential participants
k. Administers IV Meds
b. Obtains Informed Consent**
l. Prepares Study initiation activities
c. Conducts physical exams
m. Enters patient data into electronic research records
d. Enters data on paper research records
n. Educates participants, families, or staff
e. Data management
o. Other: List other applicable duties
f. Collects specimens
g. Dispenses medications
h. Administers P.O. medications
1. Sub-investigator
i. Addresses Regulatory issues
2. Research Nurse
j. Communicates with IRB
3. Graduate Research Assistant
**For those individuals involved with obtaining informed consent, please provide a copy of their CV.
Confidentiality Statement
For Key Personnel Directly Involved in Research
All information pertaining to individuals participating as research participants in ECU or Affiliate research projects, including but not limited to names, addresses, and other identifying information, must be held in strictest confidence. Unauthorized disclosure of information related to research participants by staff constitutes serious misconduct, which is subject to disciplinary action, including termination. Under certain circumstances, unauthorized disclosure could result in criminal, civil, or judicial penalty. Research information cannot be disclosed to third parties other than those to which the participant agreed in the consent process and documented in the UMCIRB approved Informed Consent Form. This does not prevent disclosures required or permitted by state or federal law for the protection of human life or protection of children.
I have read and understand the above Confidentiality Statement and I agree to comply with all requirements for confidentiality.
Key Personnel Signature
Note to Principal Investigator: A copy of this statement is to be signed by each key personnel who has access to confidential information covered by the IRB approved research project, including all sub-investigators and research/graduate assistants. DO NOT submit this original statement with the IRB application. All signed copies of this statement and the person's documentation certifying completion of educational training in human research protections must be maintained by the Principal Investigator for a period no less than three years after the end of IRB approval. During the research and for a minimum period of three years afterwards, the IRB may require the Principal Investigator to provide copies of this documentation. It is the Principal Investigator's responsibility to ensure that such documentation is available and current. Principal Investigator (type name)
Principal Investigator Signature
Date of Signature
REQUIRED RESEARCH APPROVALS Is it reasonably foreseeable that studies will be done on participants of attending physicians other than investigators listed on the proposal?
If yes, obtain their signatures below or describe the method for obtaining their approval prior to the involvement of their patients.
The following physicians acknowledge their willingness to participate in the above named research study, have read the protocol, describing the study, and agree to allow their patients to participate. Signature
CHIEF OF SERVICE OR DEPARTMENT CHAIR APPROVAL STATEMENT
I have reviewed this project. I believe that the research is sound, the goals are scientifically achievable, and that it does not involve any significant human rights issues. There are appropriate departmental resources (financial and otherwise) available to conduct the research. The investigator is qualified to conduct all aspects of this research project based on education, training or experience, and has the necessary authorizations or privileges to conduct all outlined procedures. I endorse the investigator and outlined research project as indicated by my signature below. I have reviewed the UMCIRB Conflict of Interest Disclosure Form and evaluated the principal investigator of this project for risk related to conflict of interest according to the UMCIRB Standard Operating Procedure Manual. I endorse the investigator and the attached plan (if required) for managing conflict of interest related to this research study as indicated by my signature below. NOTE: (1) A department chair may not sign this statement if listed as an investigator, and should seek the signature of the division chair/dean. (2) If you don't have a department chair (such as a private practice investigator) then attach a current CV. Signature of Chief of Service/Department Chair
RESPONSIBLE FACULTY MEMBER: For any Principal Investigator that has an undergraduate, graduate, post-graduate student status including residents and fellows, or visiting status to serve as a responsible individual in the oversight of the research study. Responsible Faculty: Anne Dickerson, PhD, OTR/L, FAOTA
Mailing address: HSB 3305 Telephone Number: 744-6190
Fax Number: 744-6198
e-mail:
[email protected]
I have reviewed the study proposal and all documents and materials to be used in the study. _
Signature responsible faculty as above
INVESTIGATOR RESPONSIBILITIES
The principal and key personnel, including sub-investigators, agree to: 1.
Obtain UMCIRB approval prior to undertaking any aspect of this research study, including identifying or recruiting participants.
Obtain UMCIRB approval prior to instituting any change in the research study, unless it is necessary to protect the safety and welfare of human participants. Any action instituted to protect the safety and well-being requires immediate reporting to the UMCIRB.
Engage in a continuing exchange of information with the UMCIRB ensuring a continuing review process for the protection of human participants, including submission of a closure form upon completion of the study.
Engage in a continuing exchange of information with the appropriate departments within the institutional study site, the institutional officials, the department chairs when appropriate, and the research study sponsor.
Ensure the research study is conducted only within the periods of UMCIRB approval.
Inform the UMCIRB, research site institution, sponsor or appropriate federal regulatory agency, in writing of any serious adverse events and unanticipated problems involving risks to study participants or others as soon as possible.
Maintain all study records for 3 (three) years after completion of the study at all sites or longer if required by a professional organization, sponsor, regulatory body or others.
Regard participant informed consent as an ongoing process.
Enroll participants only after obtaining ethically and legally effective informed consent, using only the most currently approved UMCIRB consent document, as required.
10. Obtain assent from children and parental permission prior to enrollment, as required. 11. Notify the UMCIRB if any relationships develop that may be considered a conflict of interest. 12. Abide by the UMCIRB Standard Operating Procedures, all applicable federal regulations, Good Clinical
Practice, state laws, respective institutional policies to conduct this research study. Ethical standards include the Belmont Report and other professional standards for an individual research area.
13. To comply with regulatory reviews, data audits, and 3rd party observation for the consenting process by
appropriate institutional regulatory officials.
14. Notify the UMCIRB prior to relocating (i.e., leaving ECU/UHS) to provide for the orderly study closure or to
transfer the study to another investigator.
Signature Principal Investigator

APPENDIX B
Prosthesis Evaluation Questionnaire
Study Number _ Date _
Prosthesis Evaluation Questionnaire (modified)
1998, Prosthetics Research Study Seattle, WA, USA
Instructions As you read each question, remember there is no right or wrong answer. Just think of YOUR OWN OPINION on the topic and make a mark THROUGH the line anywhere along the line from one end to the other to show us your opinion. Example How important is it to you to have coffee in the morning? NOT AT ALL
EXTREMELY IMPORTANT
Over the past four weeks, rate your morning coffee. TERRIBLE
OR check I haven't drunk coffee in the morning in the past four weeks. This example shows that the person who answered these questions feels that having coffee in the morning is important to him. He also thinks the coffee he has had lately has not been very good. If he hadn't drunk any coffee in the last four weeks, he would have put a check by that statement instead of putting a mark on the line between TERRIBLE and EXCELLENT. As in this example, make a mark across the line rather than using an X or an O.
Please answer all the questions.
Support for development of the PEQ was provided by the U.S. Department of Veterans Affairs.
A. Over the past four weeks, rate the feel (such as the temperature and texture) of the amputee limb cover on
your residual limb (stump).
B. Over the past four weeks, rate the ease of putting on (donning) your amputee limb cover.
C. Over the past four weeks, rate how your amputee limb cover has looked.
D. Over the past four weeks, rate the damage done to your clothing by your amputee limb cover.
EXTENSIVE DAMAGE
E. Over the past four weeks, rate how much you sweat inside your amputee limb cover.
F. Over the past four weeks, rate how smelly your amputee limb cover was at its worst.
EXTREMELY SMELLY
G. Over the past four weeks, rate how much of the time your residual limb was swollen to the point of changing the fit of your amputee limb cover.
H. Over the past four weeks, rate any rash(es) that you got on your residual limb. EXTREMELY BOTHERSOME
OR check I had no rashes on my residual limb in the last month.
Over the past four weeks, rate any ingrown hairs (pimples) that were on your residual limb.
EXTREMELY BOTHERSOME
OR check I had no ingrown hairs on my residual limb in the last month. J. Over the past four weeks, rate any blisters or sores that you got on your residual limb. EXTREMELY BOTHERSOME
OR check I had no blisters or sores on my residual limb in the last month.
Group 2 The next section covers very SPECIFIC BODILY SENSATIONS. Here are our definitions: 1. SENSATIONS are feelings like "pressure", "tickle" or a sense of position or location, such as the toes being curled. Amputees have described sensations in their missing (phantom) limb such as "the feeling that my (missing) foot is wrapped in cotton." 2. PAIN is a more extreme sensation described by terms such as "shooting", "searing", "stabbing", "sharp", or "ache". 3. PHANTOM LIMB refers to the part that is missing. People have reported feeling sensations and/or pain in the part of the limb that has been amputated — that is, in their phantom limb. 4. RESIDUAL LIMB (STUMP) refers to the portion of your amputated limb that is still physically present. REGARDING SENSATIONS IN YOUR PHANTOM LIMB A. Since your surgery/ over the past four weeks, rate how often you have been aware of non-painful sensations in your phantom limb. a. _ never b. _ only once or twice c. _ a few times (about once/week) d. _ fairly often (2-3 times/week) e. _ very often (4-6 times/week) f. _ several times every day g. _ all the time or almost all the time B. If you had non-painful sensations in your phantom limb since your surgery/ over the past four weeks, rate how intense they were on average. EXTREMELY INTENSE
OR check _ I did not have non-painful sensations in my phantom limb. C. Since your surgery/ over the past four weeks, how bothersome were these sensations in your phantom limb? ALL THE TIME
OR check _ I did not have non-painful sensations in my phantom limb.
D. Since your surgery/ over the past four weeks, rate how often you had pain in your phantom limb. a. _ never b. _ only once or twice c. _ a few times (about once/week) d. _ fairly often (2-3 times/week) e. _ very often (4-6 times/week) f. _ several times every day g. _ all the time or almost all the time E. How long does your phantom limb pain usually last? a. _ I have none b. _ a few seconds c. _ a few minutes d. _ several minutes to an hour e. _ several hours f. _ a day or two g. more than two days
F. If you had any pain in your phantom limb since your surgery/ over the past four weeks, rate how intense it
EXTREMELY INTENSE
OR check _ I did not have any pain in my phantom limb.
G. Since your surgery, / over the past four weeks, how bothersome was the pain in your phantom limb?
EXTREMELY BOTHERSOME
OR check _ I did not have any pain in my phantom limb. REGARDING PAIN IN YOUR RESIDUAL LIMB (STUMP) H. Since your surgery, / over the past four weeks, rate how often you had pain in your residual limb. a. _ never b. _ only once or twice c. _ a few times (about once/week) d. _ fairly often (2-3 times/week) e. _ very often (4-6 times/week) f. _ several times every day g. _ all the time or almost all the time
If you had any pain in your residual limb since your surgery, / over the past four weeks, rate how intense it was on average.
EXTREMELY INTENSE
OR check _ I did not have any pain in my residual limb.
J. Since your surgery/ over the past four weeks, how bothersome was the pain in your residual limb?
EXTREMELY BOTHERSOME
OR check _ I did not have any pain in my residual limb. REGARDING PAIN IN YOUR OTHER (NON-AMPUTATED) LEG OR FOOT K. Since your surgery, / over the past four weeks, rate how often you had pain in your other leg or foot. a. _ never b. _ only once or twice c. _ a few times (about once/week) d. _ fairly often (2-3 times/week) e. _ very often (4-6 times/week) f. _ several times every day g. _ all the time or almost all the time L. If you had any pain in your other leg or foot since your surgery, / over the past four weeks, rate how intense it was on average. EXTREMELY INTENSE
OR check _ I had no pain in my other leg or foot. M. Since your surgery / over the past four weeks, how bothersome was the pain in your other leg or foot? EXTREMELY BOTHERSOME
OR check _ I had no pain in my other leg or foot. Group 3 excluded
Group 4 This section is about YOUR ABILITY TO MOVE AROUND.
A. Over the past four weeks, rate your ability to get in and out of a car.
B. Over the past four weeks, rate your ability to sit down and get up from a chair with a high seat (e.g., a
dining chair, a kitchen chair, an office chair).
C. Over the past four weeks, rate your ability to sit down and get up from a low or soft chair (e.g. an easy
chair or deep sofa).
D. Over the past four weeks, rate your ability to sit down and get up from the toilet.
E. Over the past four weeks, rate your ability to bathe safely.
Group 5 The following section asks about YOUR SATISFACTION WITH PARTICULAR SITUATIONS given that you have an amputation.
A. Over the past four weeks, rate how satisfied you have been with your amputee limb cover.
EXTREMELY DISSATISFIED
EXTREMELY SATISFIED
B. Over the past four weeks, rate how satisfied you have been with how things have worked out since your
EXTREMELY DISSATISFIED
EXTREMELY SATISFIED
C. Over the past four weeks, how would you rate your quality of life?
WORST POSSIBLE LIFE
BEST POSSIBLE LIFE
Group 6 This next section asks you to rate your ability TO DO YOUR DAILY ACTIVITIES when you are having problems with your amputee limb cover.
A. When the fit of my amputee limb cover is poor, I will get.
B. When the comfort of my amputee limb cover is poor, I will get.
C. Without my amputee limb cover, I will get.
Group 7 This last section asks you to rate HOW IMPORTANT different aspects (or qualities) of your amputee limb cover are to you.
A. How important is it that the weight of your amputee limb cover feels right?
EXTREMELY IMPORTANT
B. How important is the ease of putting on (donning) your amputee limb cover?
EXTREMELY IMPORTANT
C. How important is the appearance of your amputee limb cover (how it looks)?
EXTREMELY IMPORTANT
D. How important is it that your amputee limb cover is durable (cannot be torn)?
EXTREMELY IMPORTANT
E. How bothersome is it when you sweat a lot inside your amputee limb cover?
EXTREMELY BOTHERSOME
F. How bothersome to you is swelling in your residual limb (stump)?
EXTREMELY BOTHERSOME
G. How important is it to avoid having any ingrown hairs (pimples) on your residual limb (stump)?
EXTREMELY IMPORTANT
H. How bothersome is it to see people looking at you and your amputee limb cover?
EXTREMELY BOTHERSOME
Final Notes A. If any of the following have happened in the past four weeks, please check off and give a brief description: _ a serious medical problem (yours) _ a noticeable change in pain _ a serious personal problem (yours) _ a serious problem in the family _ some other big change has occurred in your life If you checked any of the five previous items, please give a brief description. B. Please share with us anything else about you or your amputee limb cover that you think would be helpful for us to know (continue on the back of this page if you need more space). THANK YOU VERY MUCH! Acknowledgement: Roorda LD, Roebroeck ME, Lankhorst GJ, van Tilburg T, Bouter LM. Measuring functional limitations in rising and sitting down: Development of a questionnaire. Arch Phys Med Rehabil 1996;77;663-669 for their influence on questions 4-J, 4-K, and 4-L. PEQ Evaluation Guide:
Validated Scale Name for PEQ Questions (original numbering)
for each scale by page number and question letter
Original Numbers
13A, 13B, 13C, 13D, 14E, 14F, 14G,
None in this scale
Frustration (FR)
None in this scale
Perceived Response (PR)
10A, 11D, 11E, 11G, 12H
None in this scale
Residual Limb Health (RL)
4Q, 4R, 4S, 5T, 5U, 5V
1E, 1F, 1G, 1H, 1I, 1J
Social Burden (SB)
None in this scale
None in this scale
1B, 1C, 1D, 2E, 2F, 2G, 2H, 2I
PEQ Question Modifications
Key: Green = Questions for this study Purple = Original numbers of questions per scoring and analysis guide
No Group 3 questions Group 4:
PEQ Guide for Scoring and Analysis
Scale or Single Question
Question Content
…rate the feel of the amputee limb cover
on your residual limb (stump)
…rate the ease of putting on (donning)
your amputee limb cover
…rate how your amputee limb cover
Appearance Scale
…rate the damage done to your clothing
Appearance Scale
by your amputee limb cover
…rate how much you sweat
Residual Limb Health Scale
inside your amputee limb cover
…rate how smelly your amputee limb cover
Residual Limb Health Scale
was at its worst
…rate how much of the time your residual limb was swollen to the point of changing the fit of your amputee
Residual Limb Health Scale
…rate any rash(es) that you got on your residual limb_ Or check I had no
Residual Limb Health Scale
my residual limb
…rate any ingrown hairs (pimples) that were on your residual limb _Or check I
Residual Limb Health Scale
ingrown hairs on my residual limb
…rate any blisters or sores that you got on your residual limb _Or rate I had
Residual Limb Health Scale
or sores on my residual limb
…rate how often you have been aware of non-painful sensations in your phantom limb
a. never…g. all the time or almost
If you had non-painful sensations in your phantom limb during the past month, rate how intense they were on average _ Or check
I did not have non-painful
sensations in my
as "nr" (no
…how bothersome were these sensations in your phantom limb _ Or check
I did not have non-painful
sensations in my
as "nr" (no
…rate how often you had pain in
a. never… g. all the time or almost all the time How long does your phantom limb pain usually last?
a. I have none…g. more than two
If you had any pain in your phantom limb during the past month, rate how intense
it was on average_ Or check
I did not have any pain in my
as "nr" (no
…how bothersome was the pain in your
phantom limb _ Or check
I did not have any pain in my
as "nr" (no
…rate how often you had pain in your residual limb.
a.never…g. all the time or almost
If you had any pain in your residual limb during the past month, rate how intense it
was on average_Or check
I did not have any pain in my
as "nr" (no
…how bothersome was the pain in your
residual limb_ Or check
I did not have any pain in my
as "nr" (no
…rate how often you had pain in your other leg or foot
a. never … g. all the time or
almost all the time
If you had any pain in your other leg or foot during the past month, rate how intense
it was on average _ Or check
I had no pain in my other leg or
as "nr" (no
… how bothersome was the pain in your
other leg or foot _ Or check
I had no pain in my other leg or
as "nr" (no
…rate your ability to get in and
Transfer Question
…rate your ability to sit down and get up from a chair with a high seat (e.g. a dining chair, a kitchen
Transfer Question
chair, an office chair)
… rate your ability to sit down and get up from a low or soft chair
Transfer Question
(e.g. an easy chair or deep sofa)
… rate your ability to sit down and get up
Transfer Question
… rate your ability to shower or
Transfer Question
… rate how satisfied you have been
Satisfaction Question
with your amputee limb cover
… rate how satisfied you have been with how things have worked out
Well Being Scale
since your amputation
… how would you rate your
Well Being Scale
When the fit of my amputee limb
Self Efficacy Question
When the comfort of my amputee limb cover is poor,
Self Efficacy Question
Without my amputee limb cover, I
Self Efficacy Question
How important is it that the
Importance Question
amputee limb cover feel right
How important is the ease of putting on (donning) your amputee limb
Importance Question
How important is the appearance of your
Importance Question
amputee limb cover (how it looks)
How important is it that your amputee limb
Importance Question
cover is durable (cannot be torn)
How bothersome is it when you sweat a lot inside your amputee limb
Importance Question
How bothersome to you is swelling
Importance Question
in your residual limb (stump)
How important is it to avoid having any ingrown hairs (pimples) on your residual limb
Importance Question
How bothersome is it to see people looking at you and your amputee limb
Importance Question
APPENDIX C
Study participant number:
(For the past 24 hours = day + night).
Please complete this log within one hour of waking up daily.
Please also complete the Brief Pain Inventory at the same time as the log every day.
Thank you for helping other amputees!
Questions to answer daily: Date:
Did phantom limb pain limit your sleep last night?
Number of phantom limb pain episodes in past 24 hours
How long did phantom limb pain episodes last (average)
Time stump shrinker was put on
Time amputee Limb Cover was put on
Mirror Therapy exercises performed for 15 minutes (Yes/ No)
Time stump shrinker was removed
Time amputee limb cover was removed
Other problems or information
APPENDIX D
Brief Pain Inventory- short form
http://www.rtog.org/pdf_document/QOL_PRO_Library/BriefPainInventory.pdf
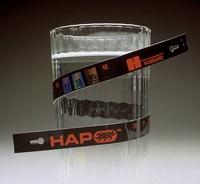
APPENDIX E
Hubbard Scientific 6083 Liquid Crystal Temperature Strip
APPENDIX F
Log of Continuity tester measurements
(performed on each amputee limb cover x 2)
Tested with multi-meter
Farabloc Fabric in
conducted prior conducted upon working order?
APPENDIX G
Instruction to therapists
This patient is in a research study.
Subjects continue to follow the standardized treatment protocol for treatment: wash residual limb twice/day with antibacterial soap
and water. Apply a piece of 4 x 4 gauze lengthways over incision. Don stump liner (panty-hose thickness) to hold gauze in place – no tape on the
residual limb. Please continue to educate patients on putting on stump shrinker over liner with "four hands" and that shrinker needs to be smooth
and evenly placed for even distribution of pressure. All subjects continue desensitization techniques to treat phantom limb pain (rubbing/ tapping
end of residual limb as needed) and upper and lower extremity exercises – per amputee booklet issued from Vidant Medical Center. All subjects
will be filling out a daily log to track pain, and completing the Brief Pain Inventory (in their binders).
Subjects are to continue with the above mentioned standardized treatment protocol and are being issued with two amputee limb covers
and a plexi-glass mirror to continue with their Mirror Therapy exercises. After the above treatment protocol has been completed and the amputee
has the shrinker on, the amputee limb cover is placed over the residual limb and fastened with the Velcro fastener (snug but loose enough that you
can place two fingers underneath the cover). Subjects are to wear these 23 hours per day and swap to the second amputee limb cover when they
take their morning bath and bath their residual limb. Please have them wash the amputee limb cover that they are taking off, at this time and place
on a dry towel to air dry. Do NOT allow them to wring out the amputee limb cover as this could break the metal fibers which will prevent the
treatment effects. All amputee limb covers have been tested for conductivity prior to issue to subjects.
Subjects also need to perform Mirror Therapy exercises for 15 minutes/day. Please supervise that they doing so correctly per the
protocol below. Supervision is to be "faded-out", as subjects learn to perform these exercises independently.
If you notice any adverse reactions, such as skin breakdown, red areas, dehiscence of the surgical incision site, please primary
APPENDIX H
Exercise protocol for Mirror Therapy exercises for lower extremity
Place mirror lengthways between legs, so that the non-amputated foot can be seen in the mirror. Subjects
can perform exercises in long-sitting or seated. Subjects are to view the non-amputated leg, but to attempt to move
both legs simultaneously. It will appear that they have two legs.
This may upset some amputees so please warn them of this reaction prior to viewing their lower extremities
Thank you for your assistance with this project.
The following 10 exercises were to be completed 10 times each
1. Slowly straighten knee and then bend your legs at the knee at the same time.
2. Slowly straighten and then bend your legs at the knee alternatively as if walking.
3. Point your feet upward, and then point your feet downwards at the same time.
4. Turn your sole in towards each other and then away from each other at the same time.
5. Move your feet around in a circle to the left and to the right.
6. Lift your feet off the ground in a walking movement.
7. Point your toes upwards and then downwards while trying to keep your ankle and foot still.
8. Clench and unclench your toes.
9. Spread your toes and then relax them.
10. Point up your big toes and point down the other toes, then reverse it so that your big toe is pointing down and
your other toes are pointing up.
(Brodie, Whyte, & Waller, 2003) ;( MacLachlan et al., 2004) ;( Culver, 2009).
<bold>APPENDIX I bold>
APPENDIX I
Source: http://www.farabloc.com.tw/Clinical%20Studies/helen%20Houston%20April%202012.pdf
CASE REPORT HUGE NODULAR GOITRE WITH RETROSTERNAL EXTENSION- A rare case report Raj Nagarkar1, Shirsendu Roy1, Mohammad Akheel2, Nayana Kulkarni3 1-Surgical oncologists 2-Senior Registrar, 3-Anesthetist, Dept of head & neck oncology services, HCG Curie Manavata cancer centre, Nashik, India. ABSTRACT:
Aus dem Physiologischen Institut (Geschäftsführender Vorstand: Prof. Dr. med. Bleich) der Christian-Albrechts-Universität zu Kiel DIE WIRKUNG VON CARBAMAZEPIN AUF NEURONALE UND EPITHELIALE KCNQ-KANÄLE Inauguraldissertation Erlangung der Doktorwürde der Medizinischen Fakultät der Christian-Albrechts-Universität zu Kiel Olga Haferkamp