Journalofosseointegration.eu
FRAnCiSley ÁvilA SouzA1
, AnA PAulA FARnezi BASSi1
, AleSSAndRA MARCondeS ARAnegA1
,
dAnielA Ponzoni1
, gABRielA BuFulin leonARdi2
, FeRnAndA BRASil dAuRA JoRge BooS3
,
eloÁ RodRigueS luvizuTo4
, HeloíSA HelenA níMiA5
, idelMo RAngel gARCiA JúnioR1
1DDs, Ms, PhD. Professors of the surgery and Integrated Clinic Department at the Araçatuba of Dental school – Univ est Paulista Júlio de
Mesquita Filho - UNesP, Brazil
2Undergraduate student of the Araçatuba of Dental school – Univ est Paulista Júlio de Mesquita Filho - UNesP
3DDs, Ms. student of the Post-Graduation Course in Dentistry, Area of Concentration in oral and Maxil ofacial surgery and Traumatology
of the Araçatuba of Dental school – Univ est Paulista Júlio de Mesquita Filho - UNesP
4DDs, Ms, PhD. substitute Professor of the surgery and Integrated Clinic Department at the Araçatuba of Dental school –
Univ est Paulista Júlio de Mesquita Filho - UNesP
5Nurse, Ms. Professor of Pontifical Catholic University. Puc-Minas, Poços de Caldas, Brasil. student of the Post-Graduation Course in Nurse
of the Guarulhos University – UNG., Brazil
Reconstruction of maxillary ridge atrophy
caused by dentoalveolar trauma, using autogenous
block bone graft harvested from chin: a case report
To CITe ThIs ARTICle
souza FÁ, Bassi APF, Aranega AM, Ponzoni D, leonardi GB, Boos FBDJ, luvizuto eR, Nímia
hh, Garcia IR Júnior. Reconstruction of maxil ary ridge atrophy caused by dentoalveolar
trauma, using autogenous block bone graft harvested from chin: a case report. J osseointegr
Dentoalveolar traumas are very common, and mainly
affect children and adolescents. The main causes are
car accidents, sporting activities and aggressions.
There are some predisposing factors for this condition,
such as accentuated overjet, childhood obesity (1),
Background Dentoalveolar trauma, especially when involving
upper lip incapable of covering the anterior teeth, and
front teeth, negatively affect the patient's life; in particular,
protrusion of the maxillary central incisor (2). The most
tooth avulsion is a complex injury that affects multiple tissues,
common dento-alveolar traumas include fractures,
and no treatment option offers stable long-term outcomes.
luxations and tooth avulsion; the latter occurs when
The aim of this study was to report a case of reconstruction of
the tooth is completely forced out of its alveolar socket.
atrophic anterior alveolar ridge after tooth loss, performed with
The most conservative treatment for avulsion is tooth
autograft harvested from the chin, and subsequent prosthetic
reimplantation; however, frequently this is not possible,
rehabilitation with the use of an osseointegrated implant.
leading to sequelae that include psychological effects
Case report A 23-years-old Caucasian girl, presented an
on the patient, compromising oral function, esthetics
atrophic alveolar bone in the area of tooth 11, as a result of tooth
and self-esteem (3), and biological damage to the hard
resorption 10 years after a tooth reimplantation procedure.
and soft tissues of the affected region (4). Nevertheless,
Reconstruction was performed with autogenous bone harvested
even when reimplantation is performed, the main and
from the chin. After 6-months healing period to al ow autograft
most likely complication is tooth resorption, which may
incorporation, a dental implant was inserted. After further 6-
trigger extensive bone resorption and severe atrophy
months, a screw-retained implant supported metal-ceramic
of the maxilla (5). This condition makes implants
prosthesis was fabricated.
insertion and prosthetic rehabilitations impossible or
Results The prosthetic rehabilitation was successful, and after
difficult. In these cases, bone regeneration procedures
a fol ow-up period of 5 years, the achieved result was stable.
are mandatory to allow the implant placement in a
Conclusion It can be concluded that the autogenous bone graft
correct tridimensional situation (6).
harvested from the chin, is a safe and effective option for alveolar
The goal of bone reconstructions by means of grafts
ridge defects reconstruction, al owing a subsequent placement
is to re-establish adequate bone dimension, allowing
of a dental implant supporting a prosthetic restoration.
correct rehabilitation with osseointegrated implants
(7). Autogenic bone grafts are considered the gold
standard among grafting materials in dentistry (8).
This is due to their relative resistance to infection,
KeywoRDs Autogenous bone graft; Dentoalveolar traumatism;
incorporation by the host, without the occurrence of
osseointegrated implants; Prosthetic rehabilitation; Tooth avulsion.
a foreign body reaction (9), in addition to osteogenic,
osteoinductive and osteoconductive capacity (8). The
June 2014; 6(2) ariesdue



Souza F.A. et al.
autogenous bone graft may be of trabecular, cortical or
FIG. 1A Adhesive
mixed (osseous coagulum and particulate bone) bone
partial denture.
from an intra or extra-oral donor area (10). The main
extra-oral donor sites are the iliac crest and calvarium,
and the intra-oral sites are the chin, retromolar areas
and maxillary tuberosity (11). The use of extra-oral
areas involves extensive surgeries, greater morbidity
and costs, requiring hospitalization of the patient (12),
whereas grafts from intra-oral sources are obtained
more easily due to the proximity between the donor and
receptor sites, when possible under local anesthesia,
and with less discomfort to the patient, in addition to
a low resorption potential (8). On the other hand, the
thickness defect.
main disadvantage of using intra-oral donor areas is
the limited quantity of bone tissue available (13).
One of the factors to be considered in the choice of donor
area is the quantity of bone graft required. Among the
intra-oral bone sites, the chin region is one of the most
used, particularly in case of receptor areas that need a
small quantity of bone volume and small augmentation
of the alveolar ridge. The chin presents both cortical and
medul ary bone types, which ensure good incorporation,
rapid revascularization and extremely little loss of
grafted bone volume (8, 14). Moreover, it offers a thick
block, larger bone volume, and moderate post-operative
pain and edema, when compared with other intraoral
donor areas (15). The limits of harvesting grafts from
the mental symphysis are connected to the presence of
the roots of teeth, mental foramen, inferior cortical and
lingual cortical borders (16). One of the main limitations
of this technique is the proximity to the mental nerve,
that could be damaged and cause an alteration of
sensitivity (8).
At present, there is great concern about the adequate
placement of implants, allowing a more functional FIG. 2 Initial panoramic radiograph.
prosthetic rehabilitation from the biomechanical point
of view, and enhanced esthetics, with benefits to the
patient's self-esteem, and a high level of satisfaction.
was born. She reported that, at that time, the protocol
Therefore, the aim of this study was to report a case
for late reimplantation was performed, with surface
of reconstruction of atrophic anterior alveolar ridge,
treatment of the tooth, endodontic treatment and
performed with autograft harvested from the chin, and
definitive restoration at the site of the coronal opening.
rehabilitated with an implant-supported prosthesis.
Nine years after, tooth 11 was lost as related by the
patient, because it had become mobile, with presence
of a purulent exudate. The surgical procedure for
CASe RePoRT
extraction was performed by the same clinician and an
adhesive fixed partial denture was fabricated on tooth
Case history
11, with adhesive abutments on teeth 12 and 21 (Fig.
A 23-year-old Caucasian girl, showed attendance 1a).
at the clinic of Oral and Maxillofacial Surgery of the
The patient reported to have used the denture up to
Araçatuba of Dental School – UNESP, in order to the moment of referral, but she complained about the
replace a partial fixed adhesive denture on teeth 12,
difficulty of cleaning it, and exacerbation of the nasal
11, and 21 with an osseointegrated implant. There was
filter sinking due to the alveolar bone resorption in
absence of tooth 11, lost as a consequence of tooth
correspondence of tooth 11.
resorption: the patient had suffered a tooth avulsion
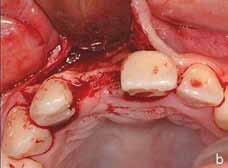
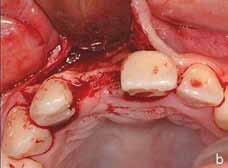
During the clinical intra-oral examination, bone
at the age of 10 years. On the day of the avulsion the
resorption of the vestibular wall was observed, in
tooth was reimplanted by a dental surgeon specialized
correspondence of the missing tooth (Fig. 1b). A
in Pediatric Dentistry, in the city where the patient
panoramic radiograph was requested (Fig. 2), in which
ariesdue June 2014; 6(2)

Reconstruction of traumatized atrophic ridge with bone block graft. A case report
of 3 positions (17), in the mandible. In addition,
subperiosteal infiltrative terminal anesthesia was also
performed in the vestibule of the anterior regions of
the maxilla and mandible with the intention of curbing
possible hemorrhages.
Surgical access began in the receptor area with a
Newman mucoperiosteal incision using a scalpel
blade (15s, Feather, Feather Safety, Japan) mounted
in a scalpel handle (Hu-Friedy, Berlin, Germany), for
detachment and exposure of the receptor site (Fig
3a). Extensive bone resorption was observed in the
FIG. 3B Vestibular
vestibular-palatine direction, proved by the thinness of
wall thickness.
the receptor site (Fig. 3b). Decortication of the vestibular
bone plate was performed by means of a Maxicut
spherical bur (Edenta, Zahn-Labor, Labordental, São
Paulo, Brazil) and perforations with Bur 702 (Maillefer
Instruments, Ballaigues, Switzerland), mounted in
a straight multiplicator handpiece (Kavo do Brasil,
Joinvile, Brazil) with electric motor (Kavo do Brasil,
Joinvile, Brazil), under constant irrigation with 0.9%
physiological solution (Darrow, Rio de Janeiro, Brazil).
An incision was made in the mucosa at the depth of the
anterior vestibular fornix, then a perpendicular muco-
it was possible to observe bone tissue without signs of
periosteal incision to detach and expose the chin donor
bone rarefaction, with preserved bone height between
area was performed (Fig. 4a). The size of the graft
the alveolar crest and floor of the nasal fossa.
necessary for the reconstruction was delimited in the
Complementary exams were requested in order to donor area (Fig 4b), followed by monocortical osteotomy
evaluate the patient's general state of health, which
(Fig. 4c), performed with Bur 702. The monocortical
included hemogram, complete coagulogram, fasting block bone graft was removed with the aid of Wagner
glycemia, urea, creatinine and electrolyte dosages chisels and hammer (Quinelato, São Carlos, Brazil), as
(Sodium, Potassium and Calcium); thus, the patient shown in Figure 4d. The recipient site was shaped for
was graded into surgical risk ASA I, in accordance with
passive graft accommodation insertion (Fig. 5a) and
the American Society of Anesthesiologists (1963). fixation by means of 2 bicortical screws measuring
Reconstruction of the alveolar ridge corresponding 1.3x11.0 mm (SIN, Sistema de Implante Nacional, São
to tooth 11 was planned, by means of an autogenous
Paulo, Brazil) (Fig. 5b). The desired thickness achieved
bone graft harvested from the chin, with an implant
after performing the graft can be noted (Fig. 5c). Then,
supported prosthetic rehabilitation to be performed at
the sharp angles were rounded off in order to avoid
possible exposure and/or fenestrations and the area
After the pre-operative review, on the day of surgery,
was sutured with simple "U"-shaped stiches, using
the patient received preventive antibiotic therapy of
5.0 nylon thread (Mononylon, Ethicon, Johnson, São
2g of Amoxicillin (Amoxicilina, Eurofarma, São Paulo,
José dos Campos, Brazil). Moreover, the acute edges
Brazil) and 5 mg of Diazepam (Valium, Products Roche
of the donor area were rounded off; the muscle plane
Chemistry and Pharmaceutics, Rio de Janeiro, Brazil)
was sutured with Polyglactin thread 910 (Vicryl 5.0,
to control anxiety, in addition to verbal tranquilization
Ethicon, Johnson, São José dos Campos, Brazil) and the
throughout the surgical procedure.
mucosal plane with 5.0 nylon thread (Fig. 5d).
After suturing, a compressive micropore dressing was
placed (Johnson & Johnson, São José dos Campos,
The surgical procedure began with intra-oral antisepsis
Brazil) on the chin and upper lip, and kept in place
with 0.12% chlorhexidine digluconate (Periogard, for 24 hours. A maintenance therapy prescription was
P&G, São Paulo, Brazil), and extra-orally with topical
prescribed, with 500 mg Amoxicillin (Amoxicilina,
application of 10% PVPI (Riodeine, Rioquímica, São
Eurofarma, São Paulo, Brazil) every 8h for 7 days,
José do Rio Preto), and apposition of sterile fields. 100mg Nimesulide (Nimessulida, Medley, Campinas,
Anesthesia was performed with bilateral regional block
Brazil) every 12h for 3 days, in addition to pain
of the anterior middle superior alveolar nerve, and of
control with 500 mg Sodium Dipyrone (Dipirona
the nasopalatine nerve in the maxilla.
Sódica, Eurofarma, São Paulo, Brazil) every 6h in case
Similarly, bilateral pterygo-mandibular anesthesia of pain. Furthermore, the patient was instructed to
was performed by means of the Smith technique perform a careful oral hygiene with moderate topical
June 2014; 6(2) ariesdue



Souza F.A. et al.
FIG. 4A Access to
Delimitation of bone graft.
of bone graft by
means of chisels.
FIG. 5B Fixation
of bone graft in
of bone graft in
receptor area.
receptor area.
FIG. 5D suturing
donor areas.
mouth washes with 0.12% Chlorhexidine Digluconate
described. After exposure of the reconstructed area,
(Periogard, P&G, São Paulo, Brazil) starting on the day
the 2 bicortical stabilization screws of the graft were
after surgery. On the same day, the adhesive prosthesis
removed and remodeling of the bone graft in the
was bonded with resin cement.
reconstructed area was observed (Fig. 6). The bone
After 14 days, the sutures were removed and the graft was fixed to the residual bone with absence of
wound was inspected to detect any infections and mobility, indicating that incorporation had occurred.
dehiscences. The patient was visited at least once per
Therefore, in this area, a cylindrical dental implant
month until implant surgery.
with a hexagon connection (SIN, Sistema de Implante
Nacional, São Paulo, Brazil) measuring 4.0x13.0
mm was placed (Fig. 7). Thus, the patient's adhesive
After 6 months the patient was submitted to the same
denture was bonded with resin cement, in order to
pre-operative and surgical procedures, as previously
avoid any interference in the peri-implant mucosa.
ariesdue June 2014; 6(2)
Reconstruction of traumatized atrophic ridge with bone block graft. A case report
• Absence of bone resorption of the graft.
Remodeling of bone graft after 6
There was successful implant osseointegration into
the area reconstructed with the autogenous block
bone graft harvested from chin, as the clinical
and radiographical results satisfied the criteria
for evaluation of implant survival suggested by
Chiapasco et al. (18):
• Absence of persistent pain or dysesthesia;
• Absence of peri-implant infection with suppuration;
• Absence of vertical or horizontal implant mobility
after masticatory force;
• Absence of continuous peri-implant radiolucency.
After a follow-up period of 5 years, stability of the
result achieved was assessed by means of clinical (Fig.
9) and radiographical (Fig. 10) evaluation.
FIG. 8 Provisional
The most conservative treatment for tooth avulsion
is tooth reimplantation (5), with success rate ranging
from 4% to 50% (19). When failure occurs, it is almost
always associated with tooth and bone resorption (4);
these bone defects are not only due to dento-alveolar
traumas, but also could be a consequence of diseases,
surgeries, tooth extractions or physiological resorption
that may affect bone quantity, height and volume (7).
The most common surgical procedure for reconstruction
Suture removal was performed 7 days after implant
retained definitive crown
after five years
After further 6 months, a new panoramic radiograph
was taken to evaluate the implant osseointegration,
and the absence of bone resorption. Re-opening of
the implant site was performed, and transfer molding
with square transfer coping (SIN, Sistema de Implante
Nacional, São Paulo, Brasil) was placed. A provisional
screw-retained resin denture (Fig. 8) was screwed with
a torque of 10 N/cm. Then, a definitive metal ceramic
screw-retained denture was delivered.
There was incorporation of the block bone graft
harvested from chin in the receptor site (maxilla), as
the clinical and radiographical results showed:
• Absence of persistent pain, dysesthesia or infection
with suppuration in the donor site or reconstructed
• Absence of bone graft mobility during implant
FIG. 10 Five years fol ow-up panoramic radiograph.
June 2014; 6(2) ariesdue
Souza F.A. et al.
of such areas is bone grafting, for which materials volume and preventing subsequent bone loss (12, 30).
of autogenous, allogeneic, xenogenic and synthetic For this reason, in the case here reported, the implant
origin are used. In this case report, autologous bone
was placed six months after the bone graft, which
was chosen due to its osteogenicity. In the literature,
corresponded to the final stage of autogenous bone
autogenous bone grafting has been established as the
grafts incorporation (8). In relation to the success of
best material for reconstructions, because it has live
bone grafting procedures, many studies report that
immunocompatible bone cells that are essential in the
surgical techniques performed, donor site, recovery
early stages of osteogenesis (20) and allows a better
time, and time of implant placement are also crucial.
incorporation into the receptor site (8).
Among the donor areas for autografts, intraoral sites
are preferred to extraoral ones due to their convenient
access, proximity between the donor and receptor
sites, lower degree of morbidity after graft harvesting
It can be concluded that the autogenous bone graft
and minimum discomfort to the patient (21). However,
harvested from the chin is a safe and effective option
in some cases it is not possible to use intraoral donor
for alveolar ridge defects reconstruction, allowing
areas, particularly when a large quantity of bone is
a further placement of dental implant supporting a
required. In case of single tooth area replacement, prosthetic restoration.
partial anterior reconstructions, or sinus membrane
elevation in a single maxillary sinus (14, 22), the
intraoral donor site provides a sufficient quantity of
bone to reconstruct the alveolar defect.
Some authors (23, 24) reported that bone harvested
1. Petti s, Cairella G, Tarsitani G. Childhood obesity: a risk factor for traumatic
from the mandible offers benefits inherent to its
injuries to anterior teeth. endod. Dent. Traumatol 1997;13:185-188.
embryological origin, such as small loss of grafted bone
2. Petti s, Tarsitani G. Traumatic injuries to anterior teeth in Italian school
volume and good incorporation into the host. Moreover,
children: prevalence and risk factors. endod. Dent. Traumatol 1996;12:294-
others authors (25, 26) showed that a low level of grafted
3. Giannetti l, Murri A, Vecci F, Gatto R. Dental avulsion: therapeutic protocols
bone resorption occurs due to the microarchitecture
and oral health-related quality of life. eur J Paediatr Dent 2007;8:69-75.
of the mandibular cortical and trabecular bone plates.
4. Andersson l, Andreasen Jo, Day P, heithersay G, Trope M, Diangelis AJ,
In the present case report, there was a considerable
Kenny DJ, sigurdsson A, Bourguignon C, Flores MT, hicks Ml, lenzi AR,
bone graft remodeling due the receptor site condition,
Malmgren B, Moule AJ, Tsukiboshi M. International Association of Dental
where a high level of bone resorption occurred as a
Traumatology guidelines for the management of traumatic dental injuries:
result of dento-alveolar trauma. A previous study (27)
2. Avulsion of permanent teeth. Dent Traumatol 2012;28:88-96.
5. Araújo MAM, Valera MC. Tratamento Clínico dos Traumatismos Dentários.
reported that bone resorption level after alveolar
são Paulo: Artes Médicas: eAP-APCD, 1 ed 1999;277p.
ridge (maxillary sites) augmentation with mandibular
6. Klokkevold PR, han TJ, Camargo PM. Aesthetic management of extractions
block bone graft represents 20% of initial volume
for implant site development: delayed versus staged implant placement.
for lateral augmentation and up to 41.5% in case of
Pract Periodontics Aesthet Dent 1999;11:603-610.
7. Chiapasco M, Casentini P, Zaniboni M. Bone augmentation procedures
The chin region as a donor site in bone grafting
inimplant dentistry. Int J oral Maxillofac Implants 2009;24:237-259.
procedures offers a low degree of morbidity (28), 8. Carvalho PsP, Pelizer eP. Fundamentos em Implantodontia. Uma visão
contemporânea. 1a ed. são Paulo: Quitenssence. 1 ed 2011;502p.
relatively good bone quantity and quality due to 9. Cricchio G, lundgren s. Donor site morbidity in two different approaches to
the presence of cortical and medullary bone (21), in
anterior iliac crest bone harvesting. Clin Implant Dent Relat Res 2003;5:161-
addition to a small loss of bone volume when grafted.
In this case report, the chin was used as donor site due
10. Nkenke e, stelzle F. Clinical outcomes of sinus floor augmentation
to the cortical-medullary anatomic characteristics of
for implant placement using autogenous bone or bone substitutes: a
the graft, thus providing a reconstruction with greater
systematic review. Clin oral Implants Res 2009;20:124-133.
bone volume in the reconstructed area, where there
11. Myeroff C, Archdeacon M. Autogenous bone graft: donor sites and
techniques. J Bone Joint surg Am 2011;93:2227-2236.
was extensive bone resorption.
12. Marx Re, Morales MJ. Morbidity from bone harvesting in major jaw
For a good integration of the grafted bone tissue into
reconstruction: a randomized trial comparing the lateral anterior and
the receptor bed and its good vascularization (29), the
posterior approaches to the ilium. J oral Maxillofac surg 1988;46:196-203.
surgical site should be immobilized, avoiding obstacles
13. Paleckis lGP, Picosse lR, Vasconcelos lw, Carvalho PsP. enxerto ósseo: por
during its healing phase. The placement of a temporary
que e quando utilizá-lo. Implant News 2005;2:369-372.
prosthetic (adhesive fixed denture), both during graft
14. Kahn A, shlomi B, levy y, Better h, Chaushu G. The use of autogenous
incorporation and implant osseointegration, allowed
block graft for augmentation of the atrophic alveolar ridge. Refuat hapeh
Vehashinayim 2003;20: 54-64.
healing of the treated site without interferences or
15. Misch, Ce, Dietsh F. Bone-grafting materials in implant dentistry. Implant
Implant placement soon after incorporation of the 16. yates DM, Brockhoff hC, Finn R, Phillips C. Comparison of intraoral
graft has a stimulating effect on bone, maintaining its
harvest sites for corticocancellous bone grafts.Int J oral Maxillofac surg
ariesdue June 2014; 6(2)
Reconstruction of traumatized atrophic ridge with bone block graft. A case report
24. Zins Je, whitaker lA. Membranous vs. endochondral bone autografts:
17. smith Ae (1918) Apud: steadman FsTJ. Anestesia local en odontología.
implications for craniofacial reconstruction. surg Forum 1979;30:521-523.
Barcelona: ed. Pubul 1929.
25. Misch CM, Misch Ce, Resnik RR, Ismail yh. Reconstruction of maxillary
18. Chiapasco M, Romeo e, Coggiola A, Brusati R. long-term outcome of
alveolar defects with mandibular symphysis grafts for dental implants: a
dental implants placed in revascularized fibula free flaps used for the
preliminary procedural report. Int J oral Maxillofac Implants 1992;7:360-
reconstruction of maxillo-mandibular defects due to extreme atrophy. Clin
oral Implants Res 2011;22:83-91.
26. ozaki w, Buchman G. Investigation of the influence of biomechanical force
19. Gonda F, Nagase M, Chen RB, yabata h, Nakajima T. Replantation an analysis
on the ultrastructure of human sagittal craniosynostosis. Plast Reconstr
of 29 teeth. oral surg oral Med oral Pathol 1990;70:650-655.
20. Guskuma Mh, hochuli-Vieira e, Pereira FP, Garcia-Júnior IR, okamoto
27. Cordaro l, Amadé Ds, Cordaro M. Clinical results of alveolar ridge
R, okamoto T, Magro-Filho o. evaluation of the presence of VeGF,
augmentation with mandibular block bone grafts in partially edentulous
BMP2 and CBFA1 proteins in autogenous bone graft: histometric and
patients prior to implant placement. Clin oral Implants Res 2002;13:103-11.
immunohistochemical analysis. J Craniomaxillofac surg 2013;doi: 10.1016/j.
28. schliephake h, Kroly C, wustenfeld h. experimental study by fluorescence
jcms.2013.05.022. [epub ahead of print].
microscopy and microangiograph of remodeling and regeneration of bone
21. Misch CM. Comparison of intraoral donor sites for onlay grafting prior to
inside alloplastic contour augmentation. Int J oral Maxillofac Implants
implant placement. Int J oral Maxillofac Implants 1997;12:767-776.
22. Mathias MV, Bassanta AD, saturnino AR, simone Jl. enxertos Autógenos
29. Branemark PI, Adell R, Albrektsson T, lekholm U, lundkvist s, Rockler B.
com sítios Doadores na Cavidade oral. RGo 2003;51:249-256.
osseointegrated titanium fixtures in the treatment of edentulousness.
23. Rabie AB, Dan Z, samman N. Ultrastructural identification of cells envolved
in the healing if intramembranous and endochondral bones. Int J oral
30. lidstrom RD, symington JM. osseointegrated dental implants in
Maxil ofac surg 1996;25:383-388.
conjunction with bone grafts. Int J oral Maxillofac surg 1988;17:116-118.
June 2014; 6(2) ariesdue
Source: http://www.journalofosseointegration.eu/wp-content/uploads/2014/07/JOsseointegr.2014.2.1.pdf
Dopage au quotidien Un document de base d'Addiction Suisse 1. Introduction A en croire les médias, on assiste à une augmentation de la tendance à recourir aux artifices les plus divers pour augmenter sa performance au travail et dans la vie privée. Même des personnes en parfaite santé n'hésitent pas à intervenir dans le fonctionnement de leur corps. Une pratique qui n'a rien de nouveau. Dans le domaine du physique ce souci d'optimisation, nourri par l'obsession contemporaine de la beauté et de la performance, se traduit déjà, du moins dans certains milieux, par la chirurgie esthétique, la médecine sportive et les médicaments « lifestyle » (par exemple les produits anti-âge). En matière de sport, le dopage a déjà provoqué un vaste débat éthique et philosophique, non seulement en raison des risques qu'il comporte pour la santé, mais surtout du manque de fair-play dont les sportifs de compétition font preuve, de l'avis général, en se procurant ainsi des avantages injustifiés sur leurs adversaires. Cette controverse a débouché sur l'établissement de règles concernant l'utilisation des produits dopants. En revanche, la discussion sur l'emploi de ces derniers dans le cadre de la vie privée et professionnel e ne fait que commencer.
Visit http://tinyurl.com/DMEandDR for online testing and instant CME certificate Current Management of Diabetic Macular Edemaand Diabetic Retinopathy Clinical Cases Original Release: January 2, 2015 Last Review: December 9, 2014 Expiration: January 31, 2016 This continuing medical education activity is jointly provided