European resuscitation council guidelines for resuscitation 2015: section 4. cardiac arrest in special circumstances

Contents lists available at
European Resuscitation Council Guidelines for Resuscitation 2015
Section 4. Cardiac arrest in special circumstances
Anatolij Truhláˇr , Charles D. Deakin , Jasmeet Soar , Gamal Eldin Abbas Khalifa ,
Annette Alfonzo , Joost J.L.M. Bierens , Guttorm Brattebø , Hermann Brugger ,
Joel Dunning , Silvija Hunyadi-Antiˇcevi ´c , Rudolph W. Koster , David J. Lockey ,
Carsten Lott , Peter Paal , Gavin D. Perkins , Claudio Sandroni , Karl-Christian Thies ,
David A. Zideman , Jerry P. Nolan , on behalf of the Cardiac arrest in special
circumstances section
a Emergency Medical Services of the Hradec Králové Region, Hradec Králové, Czech Republic
b Department of Anaesthesiology and Intensive Care Medicine, University Hospital Hradec Králové, Hradec Králové, Czech Republic
c Cardiac Anaesthesia and Cardiac Intensive Care, NIHR Southampton Respiratory Biomedical Research Unit, Southampton University Hospital NHS Trust,
d Anaesthesia and Intensive Care Medicine, Southmead Hospital, North Bristol NHS Trust, Bristol, UK
e Emergency and Disaster Medicine, Six October University Hospital, Cairo, Egypt
f Departments of Renal and Internal Medicine, Victoria Hospital, Kirkcaldy, Fife, UK
g Society to Rescue People from Drowning, Amsterdam, The Netherlands
h Bergen Emergency Medical Services, Department of Anaesthesia and Intensive Care, Haukeland University Hospital, Bergen, Norway
i EURAC Institute of Mountain Emergency Medicine, Bozen, Italy
j Department of Cardiothoracic Surgery, James Cook University Hospital, Middlesbrough, UK
k Center for Emergency Medicine, Clinical Hospital Center Zagreb, Zagreb, Croatia
l Department of Cardiology, Academic Medical Center, Amsterdam, The Netherlands
m Intensive Care Medicine and Anaesthesia, Southmead Hospital, North Bristol NHS Trust, Bristol, UK
n Department of Anesthesiology, University Medical Center, Johannes Gutenberg-Universitaet, Mainz, Germany
o Barts Heart Centre, St Bartholomew's Hospital, Barts Health NHS Trust, Queen Mary University of London, London, UK
p Department of Anaesthesiology and Critical Care Medicine, University Hospital Innsbruck, Austria
q Warwick Medical School, University of Warwick, Coventry, UK
r Critical Care Unit, Heart of England NHS Foundation Trust, Birmingham, UK
s Department of Anaesthesiology and Intensive Care, Catholic University School of Medicine, Rome, Italy
t Birmingham Children's Hospital, Birmingham, UK
u Department of Anaesthetics, Imperial College Healthcare NHS Trust, London, UK
v Anaesthesia and Intensive Care Medicine, Royal United Hospital, Bath, UK
w School of Clinical Sciences, University of Bristol, UK
special causes, special environments and special patients. The
first part covers treatment of potentially reversible causes of car-
Irrespective of the cause of cardiac arrest, early recognition and
diac arrest, for which specific treatment exists, and which must
calling for help, including appropriate management of the deteri-
be identified or excluded during any resuscitation. For improv-
orating patient, early defibrillation, high-quality cardiopulmonary
ing recall during ALS, these are divided into two groups of four,
resuscitation (CPR) with minimal interruption of chest compres-
based upon their initial letter – either H or T – and are called
sions and treatment of reversible causes, are the most important
the ‘4Hs and 4Ts': Hypoxia; Hypo-/hyperkalaemia and other elec-
trolyte disorders; Hypo-/hyperthermia; Hypovolaemia; Tension
In certain conditions, however, advanced life support (ALS)
pneumothorax; Tamponade (cardiac); Thrombosis (coronary and
guidelines require modification. The following guidelines for resus-
pulmonary); Toxins (poisoning). The second part covers cardiac
citation in special circumstances are divided into three parts:
arrest in special environments, where universal guidelines have
to be modified due to specific locations or location-specific causes
of cardiac arrest. The third part is focused on patients with spe-
cific conditions, and those with certain long-term comorbidities
E-mail address: (A. Truhláˇr).
1 The members of the Cardiac arrest in special circumstances section Collaborators
where a modified approach and different treatment decisions may
are listed in the Collaborators section.
be necessary.
0300-9572/ 2015 European Resuscitation Council. Published by Elsevier Ireland Ltd. All rights reserved.
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
Summary of changes since 2010 Guidelines
cardiac arrest. A new section covers the common causes and rel-
evant modification to resuscitative procedures in this group of
The main changes in the ERC Guidelines 2015 in comparison
with the Guidelines summarised below:
• Cardiac arrest following major cardiac surgery is relatively com-
mon in the immediate post-operative phase. Key to successful
resuscitation is recognition of the need to perform emergency
• Survival after an asphyxia-induced cardiac arrest is rare and sur-
resternotomy, especially in the context of tamponade or hae-
vivors often have severe neurological impairment. During CPR,
morrhage, where external chest compressions may be ineffective.
early effective ventilation of the lungs with supplementary oxy-
Resternotomy should be performed within 5 min if other inter-
gen is essential.
ventions have failed.
• A high degree of clinical suspicion and aggressive treatment can
• Cardiac arrest from shockable rhythms (Ventricular Fibrillation
prevent cardiac arrest from electrolyte abnormalities. The new
(VF) or pulseless Ventricular Tachycardia (pVT)) during car-
algorithm provides clinical guidance to emergency treatment of
diac catheterisation should immediately be treated with up to
three stacked shocks before starting chest compressions. Use
• Hypothermic patients without signs of cardiac instability
of mechanical chest compression devices during angiography is
(systolic blood pressure ≥90 mmHg, absence of ventricular
recommended to ensure high-quality chest compressions and
arrhythmias or core temperature ≥28 ◦C) can be rewarmed exter-
reduce the radiation burden to personnel during angiography
nally using minimally invasive techniques (e.g. with warm forced
with ongoing CPR.
air and warm intravenous fluid). Patients with signs of cardiac
• In dental surgery, do not move the patient from the dental chair
instability should be transferred directly to a centre capable of
in order to start CPR. Quickly recline the dental chair into a hor-
extracorporeal life support (ECLS).
izontal position and place a stool under the head of the chair to
• Early recognition and immediate treatment with intramuscular
increase its stability during CPR.
adrenaline remains the mainstay of emergency treatment for
• The in-flight use of AEDs aboard commercial airplanes can result
in up to 50% survival to hospital discharge. AEDs and appropriate
• The mortality from traumatic cardiac arrest (TCA) is very high.
CPR equipment should be mandatory on board of all commer-
The most common cause of death is haemorrhage. It is recognised
cial aircraft in Europe, including regional and low-cost carriers.
that most survivors do not have hypovolaemia, but instead have
Consider an over-the-head technique of CPR if restricted access
other reversible causes (hypoxia, tension pneumothorax, cardiac
precludes a conventional method, e.g. in the aisle.
tamponade) that must be immediately treated. The new treat-
• The incidence of cardiac arrest on board helicopter emergency
ment algorithm for TCA was developed to prioritise the sequence
medical services (HEMS) and air ambulances is low. Importance
of life-saving measures. Chest compressions should not delay the
of pre-flight preparation and use of mechanical chest compres-
treatment of reversible causes. Cardiac arrests of non-traumatic
sion devices are emphasised.
origin leading to a secondary traumatic event should be recog-
• Sudden and unexpected collapse of an athlete on the field of play
nised and treated with standard algorithms.
is likely to be cardiac in origin and requires rapid recognition and
• There is limited evidence for recommending the routine trans-
port of patients with continuing CPR after out-of-hospital cardiac
• The duration of submersion is a key determinant of outcome
arrest (OHCA) of suspected cardiac origin. Transport may be ben-
from drowning. Submersion exceeding 10 min is associated with
eficial in selected patients where there is immediate hospital
poor outcome. Bystanders play a critical role in early rescue and
access to the catheterisation laboratory and an infrastructure
resuscitation. Resuscitation strategies for those in respiratory or
providing prehospital and in-hospital teams experienced in
cardiac arrest continue to prioritise oxygenation and ventilation.
mechanical or haemodynamic support and percutaneous coro-
• The chances of good outcome from cardiac arrest in diffi-
nary intervention (PCI) with ongoing CPR.
cult terrain or mountains may be reduced because of delayed
• Recommendations for administration of fibrinolytics when pul-
access and prolonged transport. There is a recognised role of
monary embolism is the suspected cause of cardiac arrest remain
air rescue and availability of AEDs in remote but often-visited
unchanged. Routine use of surgical embolectomy or mechani-
cal thrombectomy when pulmonary embolism is the suspected
• The cut-off criteria for prolonged CPR and extracorporeal
cause of cardiac arrest is not recommended. Consider these
rewarming of avalanche victims in cardiac arrest are more
methods only when there is a known diagnosis of pulmonary
stringent to reduce the number of futile cases treated with extra-
corpoereal life support (ECLS). ECLS is indicated if the duration
• Routine use of gastric lavage for gastrointestinal decontamina-
of burial is >60 min (instead of >35 min), core temperature at
tion in poisoning is no longer recommended. Reduced emphasis
extrication is <30 ◦C (instead of <32 ◦C), and serum potassium
is placed on hyperbaric oxygen therapy in carbon monoxide poi-
at hospital admission is ≤8 mmol L−1 (instead of ≤12 mmol L−1);
otherwise standard guidelines apply.
• Safety measures are emphasised when providing CPR to the vic-
Special environments
tim of an electrical injury.
• Recommendations for management of multiple victims should
• The special environments section includes recommendations for
prevent delay of treatment available for salvageable victims dur-
treatment of cardiac arrest occurring in specific locations. These
ing mass casualty incidents (MCIs). Safety at scene is paramount.
locations are specialised healthcare facilities (e.g. operating the-
A triage system should be used to prioritise treatment and, if the
atre, cardiac surgery, catheterisation laboratory, dialysis unit,
number of casualties overwhelms healthcare resources, withhold
dental surgery), commercial airplanes or air ambulances, field of
CPR for those without signs of life.
play, outside environment (e.g. drowning, difficult terrain, high
altitude, avalanche burial, lightning strike and electrical injuries)
or the scene of a mass casualty incident.
• Patients undergoing surgical procedures involving general anaes-
• The section on special patients gives guidance for CPR in
thesia, particularly in emergencies, are at risk from perioperative
patients with severe comorbidities (asthma, heart failure with
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
ventricular assist devices, neurological disease, obesity) and
Safar, complete airway obstruction after breathing air will result
those with specific physiological conditions (pregnancy, elderly
in PEA cardiac arrest in 5–10 min.is rarely the first monitored
rhythm after asphyxial cardiac arrest – in one of the largest series of
• The first line treatment for acute asthma is inhaled beta-2 ago-
hanging-associated out-of-hospital cardiac arrests (OHCAs), from
nists while intravenous beta-2 agonists are suggested only for
Melbourne, Australia, just 7 (0.5%) of 1321 patients were in VF.
those patients in whom inhaled therapy cannot be used reliably.
Inhaled magnesium is no longer recommended.
• In patients with ventricular assist devices (VADs), confirmation
Treating the cause of the asphyxia/hypoxaemia is the highest
of cardiac arrest may be difficult. If during the first 10 days after
priority because this is a potentially reversible cause of the car-
surgery, cardiac arrest does not respond to defibrillation, perform
diac arrest. Effective ventilation with supplementary oxygen is a
particular priority in these patients. The better outcomes for OHCA
• Patients with subarachnoid haemorrhage may have ECG changes
victims receiving compression-only CPRnot the case for asphyx-
that suggest an acute coronary syndrome (ACS). Whether a com-
ial cardiac arrests, which have much better survival rates with
puted tomography (CT) brain scan is done before or after coronary
conventional CPR.the standard ALS algorithm when resus-
angiography will depend on clinical judgement regarding the
citating these patients.
likelihood of a subarachnoid haemorrhage versus acute coronary
• No changes to the sequence of actions are recommended in resus-
Survival after cardiac arrest from asphyxia is rare and most sur-
citation of obese patients, although delivery of effective CPR may
vivors sustain severe neurological injury. Of five published series
be challenging. Consider changing rescuers more frequently than
that included a total of 286 patients with cardiac arrest follow-
the standard 2-min interval. Early tracheal intubation by an expe-
ing hanging where CPR was attempted (this was attempted in
rienced provider is recommended.
only about 16% of cases), there were just six (2%) survivors with
• For the pregnant woman in cardiac arrest, high-quality CPR with
a full recovery; 11 other survivors all had severe permanent brain
manual uterine displacement, early ALS and delivery of the fetus
one third (89; 31%) of these 286 patients, rescuers
if early return of spontaneous circulation (ROSC) is not achieved
were able to achieve ROSC – thus when CPR is attempted, ROSC
remain key interventions.
is not uncommon but subsequent neurologically intact survival
is rare. Those who are unconscious but have not progressed to a
A – SPECIAL CAUSES
cardiac arrest are much more likely to make a good neurological
Hypo-/hyperkalaemia and other electrolyte disorders
Cardiac arrest caused by pure hypoxaemia is uncommon. It is
seen more commonly as a consequence of asphyxia, which accounts
Electrolyte abnormalities can cause cardiac arrhythmias or
for most of the non-cardiac causes of cardiac arrest. There are many
cardiac arrest. Life-threatening arrhythmias are associated most
causes of asphyxial cardiac arrest although there is
commonly with potassium disorders, particularly hyperkalaemia,
usually a combination of hypoxaemia and hypercarbia, it is the
and less commonly with disorders of serum calcium and
hypoxaemia that ultimately causes cardiac arrest.
magnesium. Consider electrolyte disturbances in patient groups
at risk – renal failure, severe burns, cardiac failure and diabetes
If breathing is completely prevented by airway obstruction or
The electrolyte values for definitions have been chosen as a
apnoea, consciousness will be lost when oxygen saturation in
guide to clinical decision-making. The precise values that trigger
the arterial blood reaches about 60%. The time taken to reach
treatment decisions will depend on the patient's clinical condition
this concentration is difficult to predict, but is likely to be of the
and rate of change of electrolyte values. There is little or no evi-
order 1–2 min.on animal experiments of cardiac arrest
dence for the treatment of electrolyte abnormalities during cardiac
caused by asphyxia, pulseless electrical activity (PEA) will occur
arrest. Guidance during cardiac arrest is based on the strategies
in 3–11 min. Asystole will ensue several minutes later.compar-
used in the non-arrest patient.
ison with simple apnoea, the exaggerated respiratory movements
that frequently accompany airway obstruction will increase oxy-
Prevention of electrolyte disorders
gen consumption resulting in more rapid arterial blood oxygen
When possible, identify and treat life-threatening electrolyte
desaturation and a shorter time to cardiac arrest. According to
abnormalities before cardiac arrest occurs. Monitor renal function
in patients at risk and avoid combination of drugs that may exac-
Table 4.1
erbate hyperkalaemia. Prevent recurrence of electrolyte disorders
Causes of asphyxial cardiac arrest
by removing any precipitating factors (e.g. drugs, diet).
Airway obstruction: soft tissues (coma), laryngospasm, aspiration
Potassium disorders
Potassium homeostasis. Extracellular potassium concentration is
Central hypoventilation – brain or spinal cord injury
regulated tightly between 3.5 and 5.0 mmol L−1. A large con-
Chronic obstructive pulmonary disease
centration gradient normally exists between intracellular and
extracellular fluid compartments. This potassium gradient across
cell membranes contributes to the excitability of nerve and muscle
cells, including the myocardium. Evaluation of serum potassium
Impaired alveolar ventilation from neuromuscular disease
must take into consideration the effects of changes in serum pH.
Tension pneumothorax
When serum pH decreases (acidaemia), serum potassium increases
because potassium shifts from the cellular to the vascular space; a
Traumatic asphyxia or compression asphyxia (e.g. crowd crush)
process that is reversed when serum pH increases (alkalaemia).
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
Hyperkalaemia. This is the most common electrolyte disorder asso-
• first degree heart block (prolonged PR interval >0.2 s);
ciated with cardiac arrest. It is usually caused by impaired excretion
• flattened or absent P waves;
by the kidneys, drugs or increased potassium release from cells
• tall, peaked (tented) T waves (i.e. T wave larger than R wave in
and metabolic acidosis. Hyperkalaemia occurs in up to 10% of
more than 1 lead);
hospitalised kidney disease (CKD) is com-
• ST-segment depression;
mon in the general population and the incidence of hyperkalaemia
• S & T wave merging (sine wave pattern);
increases from 2 to 42% as glomerular filtration rate (GFR) drops
• widened QRS (>0.12 s);
from 60 to 20 mL min−1with end-stage renal disease
• ventricular tachycardia;
are particularly susceptible, particularly following an OHCA.
longed hyperkalaemia is an independent risk factor for in-hospital
• cardiac arrest (PEA, VF/pVT, asystole).
Acute hyperkalaemia is more likely than chronic
Treatment of hyperkalaemia.
There are five key treatment
hyperkalaemia to cause life-threatening cardiac arrhythmias or
cardiac arrest.
• cardiac protection;
There is no universal definition. We have defined
• shifting potassium into cells;
hyperkalaemia as a serum potassium concentration higher than
• removing potassium from the body;
5.5 mmol L−1; in practice, hyperkalaemia is a continuum. As the
• monitoring serum potassium and blood glucose;
potassium concentration increases above this value the risk of
• prevention of recurrence.
adverse events increases and the need for urgent treatment
increases. Severe hyperkalaemia has been defined as a serum potas-
When hyperkalaemia is strongly suspected, e.g. in the presence
sium concentration higher than 6.5 mmol L−1.
of ECG changes, start life-saving treatment even before laboratory
The main causes of hyperkalaemia are:
results are available. The treatment strategy for hyperkalaemia
has been reviewed the hyperkalaemia
renal failure (i.e. acute kidney injury or chronic kidney disease);
emergency treatment algorithm salbutamol
drugs (e.g. angiotensin converting enzyme inhibitors (ACE-I),
monotherapy, which may be ineffective. There is insufficient evi-
angiotensin II receptor antagonists (ARB), potassium-sparing
dence to support the use of sodium bicarbonate to decrease serum
diuretics, non-steroidal anti-inflammatory drugs, beta-blockers,
potassium. Consider the need for early specialist or critical care
tissue breakdown (e.g. rhabdomyolysis, tumour lysis, haemoly-
The main risks associated with treatment of hyperkalaemia are:
metabolic acidosis (e.g. renal failure, diabetic ketoacidosis);
Hypoglycaemia following insulin-glucose administration (usu-
• endocrine disorders (e.g. Addison's disease);
ally occurs within 1–3 h of treatment, but may occur up to 6 h
• diet (may be sole cause in patients with advanced chronic kidney
after blood glucose and treat hypoglycaemia
spurious – pseudo-hyperkalaemia (suspect in cases with normal
Tissue necrosis secondary to extravasation of intravenous cal-
renal function, normal ECG and/or history of haematological dis-
cium salts. Ensure secure vascular access prior to administration.
order). Pseudo-hyperkalaemia describes the finding of a raised
Intestinal necrosis or obstruction following use of potassium
serum (clotted blood) K+ value concurrently with a normal
exchange resins. Avoid prolonged use of resins and give laxative.
plasma (non-clotted blood) potassium value. The clotting process
Rebound hyperkalaemia after the effect of drug treatment has
releases K+ from cells and platelets, which increases the serum
worn off (i.e. within 4–6 h). Continue to monitor serum potassium
K+ concentration by an average of 0.4 mmol/L. The most common
for a minimum of 24 h after an episode.
cause of pseudo-hyperkalaemia is a prolonged transit time to the
Patient not in cardiac arrest
laboratory or poor storage conditions.
The risk of hyperkalaemia is even greater when there is a
Use systematic ABCDE approach and correct any abnormalities,
combination of factors such as the concomitant use of angiotensin-
obtain IV access.
converting enzyme inhibitors or angiotensin II receptor blockers
Check serum potassium.
and potassium-sparing diuretics.
Record an ECG.
Monitor cardiac rhythm in patients with severe hyperkalaemia.
Recognition of hyperkalaemia.
Exclude hyperkalaemia in all
Treatment is determined according to severity of hyperkalaemia.
patients with an arrhythmia or cardiac arrest. Patients may present
Approximate values are provided to guide treatment. Follow
with weakness progressing to flaccid paralysis, paraesthesia, or
hyperkalaemia emergency treatment algorithm (
depressed deep tendon reflexes. Alternatively, the clinical picture
can be overshadowed by the primary illness causing hyper-
Mild elevation (5.5–5.9 mmol L−1).
kalaemia. The first indicator of hyperkalaemia may also be the
• Address cause of hyperkalaemia to correct and avoid further rise
presence of ECG abnormalities, arrhythmias, or cardiac arrest. The
in serum potassium (e.g. drugs, diet).
use of a blood gas analyser to measure potassium can reduce delays
• If treatment is indicated, remove potassium from the body:
in recognition.
potassium exchange resins-calcium resonium 15–30 g, or sodium
The effect of hyperkalaemia on the ECG depends on the abso-
polystyrene sulfonate (Kayexalate) 15–30 g, given either orally or
lute serum potassium as well as the rate of reported
by retention enema/PR (per rectum) (onset in >4 h).
frequency of ECG changes in severe hyperkalaemia is variable, but
most patients appear to show ECG abnormalities at a serum potas-
Moderate elevation (6.0–6.4 mmol L−1) without ECG changes.
sium concentration higher than 6.7 mmol L−1presence of
• Shift potassium intracellularly with glucose/insulin: 10 units
ECG changes strongly correlates with mortality.some cases,
short-acting insulin and 25 g glucose IV over 15–30 min (onset
the ECG may be normal or show atypical changes including ST
in 15–30 min; maximal effect at 30–60 min; duration of action
4–6 h; monitor blood glucose).
The ECG changes associated with hyperkalaemia are usually
• Remove potassium from the body (see above; consider dialysis
progressive and include:
guided by clinical setting).
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
Fig. 4.1. Emergency treatment of hyperkalaemia. PR per rectum; ECG electrocardiogram; VT ventricular tachycardia.
Reproduced with permission from Renal Association and Resuscitation Council (UK).
Severe elevation (≥6.5 mmol L−1) without ECG changes.
• Protect the heart with calcium chloride: 10 mL 10% cal-
• Seek expert help.
cium chloride IV over 2–5 min to antagonise the toxic
• Give glucose/insulin (see above).
• Give salbutamol 10–20 mg nebulised (onset in 15–30 min; dura-
brane. This protects the heart by reducing the risk of
tion of action 4–6 h).
VF/pVT but does not lower serum potassium (onset in
• Remove potassium from the body (consider dialysis).
• Use shifting agents (glucose/insulin and salbutamol).
Severe elevation (≥6.5 mmol L−1) with toxic ECG changes.
• Remove potassium from the body (consider dialysis at outset or
• Seek expert help.
if refractory to medical treatment).
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
Modifications to cardiopulmonary resuscitation.
• arrhythmias, especially if patient is taking digoxin;
modifications to standard ALS guidelines are recommended in the
• cardiac arrest (PEA, VF/pVT, asystole).
presence of severe hyperkalaemia:
This depends on the severity of hypokalaemia
Confirm hyperkalaemia using a blood gas analyser if available.
and the presence of symptoms and ECG abnormalities. Gradual
Protect the heart: give 10 mL calcium chloride 10% IV by rapid
replacement of potassium is preferable, but in an emergency, intra-
bolus injection.
venous potassium is required. The maximum recommended IV
Shift potassium into cells: Give glucose/insulin: 10 units short-
dose of potassium is 20 mmol h−1, but more rapid infusion (e.g.
acting insulin and 25 g glucose IV by rapid injection. Monitor
2 mmol min−1 for 10 min, followed by 10 mmol over 5–10 min) is
blood glucose.
indicated for unstable arrhythmias when cardiac arrest is immi-
Give sodium bicarbonate: 50 mmol IV by rapid injection (if severe
nent. Continuous ECG monitoring is essential during IV infusion
acidosis or renal failure).
and the dose should be titrated after repeated sampling of serum
Remove potassium from body: Consider dialysis for hyper-
potassium levels.
kalaemic cardiac arrest resistant to medical treatment. Several
Many patients who are potassium deficient are also deficient
dialysis modalities have been used safely and effectively in car-
in magnesium. Magnesium is important for potassium uptake and
diac arrest, but this may only be available in specialist centres.
for the maintenance of intracellular potassium values, particularly
Consider use of a mechanical chest compression device if pro-
in the myocardium. Repletion of magnesium stores will facilitate
longed CPR is needed.
more rapid correction of hypokalaemia and is recommended in
Indications for dialysis.
The main indications for dialysis in
patients with hyperkalaemia are:
• severe life-threatening hyperkalaemia with or without ECG
Calcium and magnesium disorders
changes or arrhythmia;
The recognition and management of calcium and magnesium
• hyperkalaemia resistant to medical treatment;
disorders is summarised in
• end-stage renal disease;
• oliguric acute kidney injury (<400 mL day−1 urine output);
• marked tissue breakdown (e.g. rhabdomyolysis).
Accidental hypothermia
Special considerations for management of cardiac arrest in a
Definition. Every year approximately 1500 people die of pri-
dialysis unit are addressed in the section Special environments (see
mary accidental hypothermia in the United
cardiac arrest in a dialysis unit).
hypothermia is defined as an involuntary drop of the body core
temperature <35 ◦C. The Swiss staging system is used to estimate
Hypokalaemia. Hypokalaemia is the most common electrolyte dis-
core temperature at the scene. Its stages are based on clinical signs,
order in clinical is seen in up to 20% of hospitalised
which roughly correlate with the core temperature:
increases the incidence of arrhythmias
• hypothermia I; mild hypothermia (conscious, shivering, core
and sudden cardiac death (SCD).risk is increased in patients
temperature 35–32 ◦C);
with pre-existing heart disease and in those treated with digoxin.
• hypothermia II; moderate hypothermia (impaired consciousness
without shivering, core temperature 32–28 ◦C);
Hypokalaemia is defined as a serum potassium level
• hypothermia III; severe hypothermia (unconscious, vitals signs
<3.5 mmol L−1. Severe hypokalaemia is defined as a serum potas-
present, core temperature 28–24 ◦C);
sium level <2.5 mmol L−1 and may be associated with symptoms.
• hypothermia IV; cardiac arrest or low flow state (no or minimal
The main causes of hypokalaemia include:
vital signs, core temperature <24 ◦C);
gastrointestinal loss (e.g. diarrhoea);
hypothermia V; death due to irreversible hypothermia (core tem-
drugs (e.g. diuretics, laxatives, steroids);
perature <13.7 ◦C).
renal losses (e.g. renal tubular disorders, diabetes insipidus, dial-
Diagnosis. Hypothermia is diagnosed in any patient with a core
endocrine disorders (e.g. Cushing's syndrome, hyperaldostero-
temperature <35 ◦C, or where measurement unavailable, a history
of exposure to cold, or when the trunk feels
metabolic alkalosis;
hypothermia may be under-diagnosed in countries with a temper-
magnesium depletion;
ate climate. When thermoregulation is impaired, for example, in
poor dietary intake.
the elderly and very young, hypothermia may follow a mild insult.
Treatment strategies used for hyperkalaemia may also induce
The risk of hypothermia is increased by alcohol or drug ingestion,
exhaustion, illness, injury or neglect especially when there is a
decrease in the level of consciousness.
Recognition of hypokalaemia.
Exclude hypokalaemia in every
A low-reading thermometer is needed to measure the core tem-
patient with an arrhythmia or cardiac arrest. In dialysis patients,
perature and confirm the diagnosis. The core temperature in the
hypokalaemia may occur at the end of a haemodialysis session or
lower third of the oesophagus correlates well with heart tem-
during treatment with peritoneal dialysis.
perature. Tympanic measurement using a thermistor technique
As serum potassium concentration decreases, the nerves and
is a reliable alternative but may be considerably lower than core
muscles are predominantly affected, causing fatigue, weakness,
temperature if the environment is very cold, the probe is not
leg cramps, constipation. In severe cases (serum potassium
well insulated, or the external auditory canal is filled with snow
<2.5 mmol L−1), rhabdomyolysis, ascending paralysis and respira-
or available tympanic thermometers based on
tory difficulties may occur.
infrared technique do not seal the ear canal and are not designed for
ECG features of hypokalaemia are:
low core temperature readings.in-hospital core temperature
measurement site should be the same throughout resuscitation
• T wave flattening;
and rewarming. Bladder and rectal temperatures lag behind core
• ST segment changes;
this reason, measurement of bladder and
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
Table 4.2
Calcium and magnesium disorders with associated clinical presentation, ECG manifestations and recommended treatment
HypercalcaemiaCalcium > 2.6 mmol L−1
Primary or tertiary
Short QT interval
Fluid replacement IV
Prolonged QRS interval
Furosemide 1 mg kg−1 IV
Hydrocortisone 200–300 mg IV
Pamidronate 30–90 mg IV
Treat underlying cause
HypocalcaemiaCalcium < 2.1 mmol L−1
Chronic renal failure
Prolonged QT interval
Calcium chloride 10% 10–40 mL
Acute pancreatitis
Magnesium sulphate 50%
Calcium channel blocker
4–8 mmol (if necessary)
Toxic shock syndrome
RhabdomyolysisTumour lysis syndrome
HypermagnesaemiaMagnesium > 1.1 mmol L−1
Prolonged PR and QT
Consider treatment when
magnesium > 1.75 mmol L−1
Respiratory depression
Calcium chloride 10% 5–10 mL
repeated if necessary
Ventilatory support if necessary
Saline diuresis – 0.9% saline with
furosemide 1 mg kg−1 IV
HypomagnesaemiaMagnesium < 0.6 mmol L−1
Prolonged PR and QT
Severe or symptomatic: 2 g 50%
magnesium sulphate (4 mL;
ST-segment depression
8 mmol) IV over 15 min
Torsade de pointes: 2 g 50%
Arrhythmias – torsade
Flattened P waves
magnesium sulphate (4 mL;
Increased QRS duration
8 mmol) IV over 1–2 min
Torsade de pointes
Seizure: 2 g 50% magnesium
sulphate (4 mL; 8 mmol) IV over
rectal temperature has been de-emphasised in patients with severe
the traditional guiding principle that ‘no one is dead until warm
and dead' should be considered. In remote areas, the impracticali-
ties of achieving rewarming have to be considered. In the hospital
Decision to resuscitate. Cooling of the human body decreases cel-
setting involve senior doctors and use clinical judgement to deter-
lular oxygen consumption by about 6% per 1 ◦C decrease in
mine when to stop resuscitating a hypothermic victim in cardiac
core 28 ◦C, oxygen consumption is reduced by
approximately 50% and at 22 ◦C by approximately 75%. At 18 ◦C the
brain can tolerate cardiac arrest for up to 10 times longer than at
Modifications to cardiopulmonary resuscitation
37 ◦C. This results in hypothermia exerting a protective effect on the
• Do not delay careful tracheal intubation when it is indicated. The
brain and heart,intact neurological recovery may be possible
advantages of adequate oxygenation and protection from aspi-
even after prolonged cardiac arrest if deep hypothermia develops
ration outweigh the minimal risk of triggering VF by performing
before asphyxia.
Beware of diagnosing death in a hypothermic patient because
• Check for signs of life for up to 1 min. Palpate a central artery and
hypothermia itself may produce a very slow, small-volume,
assess the cardiac rhythm (if ECG monitor available). Echocardi-
irregular pulse and unrecordable blood pressure. In a deeply
ography, near-infrared spectroscopy or ultrasound with Doppler
hypothermic patient (hypothermia IV) signs of life may be so mini-
may be used to establish whether there is (an adequate) cardiac
mal that it is easy to overlook them. Therefore, look for signs of life
output or peripheral blood flow.there is any doubt, start
for at least 1 min and use an ECG monitor to detect any electrical
CPR immediately.
cardiac activity. Neurologically intact survival has been reported
• Hypothermia can cause stiffness of the chest wall, making ven-
after hypothermic cardiac arrest with a core temperature as low as
tilations and chest compressions difficult. Consider the use of
13.7 ◦CCPR for as long as six and a half hours.
mechanical chest compression
Intermittent CPR, as rescue allows, may also be of benefit.
• Once CPR is under way, confirm hypothermia with a low-reading
continuous CPR cannot be delivered, a patient with hypothermic
cardiac arrest and a core temperature <28 ◦C (or unknown), should
• The hypothermic heart may be unresponsive to cardioac-
receive 5 min of CPR, alternating with periods ≤5 min without CPR.
tive drugs, attempted electrical pacing and defibrillation. Drug
Patients with a core temperature <20 ◦C, should receive 5 min of
metabolism is slowed, leading to potentially toxic plasma con-
CPR, alternating with periods ≤10 min without CPR.
centrations of any drug evidence for the efficacy
In the prehospital setting, resuscitation should be withheld in
of drugs in severe hypothermia is limited and based mainly
hypothermic patients only if the cause of cardiac arrest is clearly
on animal studies. For instance, in severe hypothermic cardiac
attributable to a lethal injury, fatal illness, prolonged asphyxia, or
arrest, the efficacy of amiodarone is reduced.may
if the chest is all other hypothermic patients,
be effective in increasing coronary perfusion pressure, but not
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
may also increase the chances of suc-
for extracorporeal rewarming. In hypothermia V, reasons for with-
cessful defibrillation, but with a core temperature <30 ◦C, sinus
holding or terminating CPR should be investigated (e.g. obvious
rhythm often degrades back into VF. Given that defibrillation
signs of irreversible death, valid DNAR, conditions unsafe for res-
and adrenaline may induce myocardial injury, it is reasonable
cuer, avalanche burial ≥60 min and airway packed with snow and
to withhold adrenaline, other CPR drugs and shocks until the
asystole). In the absence of any of these signs, start CPR and transfer
patient has been warmed to a core temperature ≥30 ◦C. Once
the patient to an ECLS centre.
30 ◦C has been reached, the intervals between drug doses should
be doubled when compared to normothermia (i.e. adrenaline
In-hospital rewarming. Unless the patient goes into VF, rewarm
every 6–10 min). As normothermia (≥35 ◦C) is approached, use
using active external methods (i.e. with forced warm air) and
standard drug protocols.
minimally invasively methods (i.e. with warm IV infusions). With
a core temperature <32 ◦C and potassium <8 mmol L−1, consider
Treatment of arrhythmias. As core temperature decreases, sinus
ECLS ECLS rewarmings have been performed
bradycardia tends to give way to atrial fibrillation followed by
using cardiopulmonary bypass, but more recently, veno-arterial
VF and finally asystole.other than VF tend to
extracorporeal membrane oxygenation (VA-ECMO) has become the
revert spontaneously as core temperature increases, and usually
preferred method due to its rapid availability, the need for less anti-
do not require immediate treatment. Bradycardia is physiological in
coagulation, and the potential to prolong cardiorespiratory support
severe hypothermia. Cardiac pacing is not indicated unless brady-
after rewarming.
cardia associated with haemodynamic compromise persists after
If an ECLS centre is not available, rewarming may be attempted
rewarming. The temperature at which defibrillation should firstly
in hospital using a dedicated team and a combination of external
be attempted, and how often it should be attempted in the severely
and internal rewarming techniques (e.g. forced warm air, warm
hypothermic patient, has not been established. If VF is detected,
infusions, forced peritoneal lavage).
defibrillate according to standard protocols. If VF persists after three
Continuous haemodynamic monitoring and warm IV fluids
shocks, delay further attempts until core temperature is ≥30 ◦C.
are essential. Patients will require large volumes of fluids during
CPR and rewarming may have to be continued for several hours to
rewarming, as vasodilation causes expansion of the intravascular
facilitate successful defibrillation.
space. Avoid hyperthermia during and after rewarming. Once ROSC
has been achieved use standard post-resuscitation care.
Insulation. General measures for all victims include removal from
the cold environment, prevention of further heat loss and rapid
transfer to hospital.the field, a patient with moderate or severe
Introduction. Hyperthermia occurs when the body's ability to ther-
hypothermia (hypothermia ≥ II) should be immobilised and han-
moregulate fails and core temperature exceeds that normally
dled carefully, oxygenated adequately, monitored (including ECG
maintained by homeostatic mechanisms. Hyperthermia may be
and core temperature), and the whole body dried and insulated.
exogenous, caused by environmental conditions, or secondary to
Remove wet clothes while minimising excessive movement of
endogenous heat production.
the victim. Removal of wet clothing or use of a vapour barrier
Environment-related hyperthermia occurs where heat, usually
seems to be equally effective to limit heat loss.vic-
in the form of radiant energy, is absorbed by the body at a rate faster
tims (hypothermia I) can mobilise as exercise rewarms a person
than can be lost by thermoregulatory mechanisms. Hyperthermia
more rapidly than shivering.will continue cooling after
is a continuum of heat-related conditions, starting with heat stress,
removal from a cold environment (i.e. afterdrop), which may result
progressing to heat exhaustion, then to heat stroke and finally to
in a life-threatening decrease in core temperature triggering a car-
multiple organ dysfunction and cardiac arrest.
diac arrest during transport (i.e. ‘rescue death'). Prehospitally, avoid
Malignant hyperthermia is a rare disorder of skeletal mus-
prolonged investigations and treatment, as further heat loss is diffi-
cle calcium homeostasis characterised by muscle contracture and
cult to prevent. Patients who stop shivering (e.g. hypothermia II–IV,
life-threatening hypermetabolic crisis following exposure of genet-
and sedated or anaesthetised patients) will cool faster.
ically predisposed individuals to halogenated anaesthetics and
depolarising muscle relaxants.
Prehospital rewarming. Rewarming may be passive, active external,
or active internal. In hypothermia I passive rewarming is appropri-
ate as patients are still able to shiver. Passive rewarming is best
Heat exhaustion is a non-life-threatening clinical
achieved by full body insulation with wool blankets, aluminium
syndrome of weakness, malaise, nausea, syncope, and other non-
foil, cap and a warm environment. In hypothermia II–IV the appli-
specific symptoms caused by heat exposure. Thermoregulation is
cation of chemical heat packs to the trunk has been recommended.
not impaired. Heat exhaustion is caused by water and electrolyte
In conscious patients who are able to shiver, this improves thermal
imbalance due to heat exposure, with or without exertion. Rarely,
comfort but does not speed the patient is uncon-
severe heat exhaustion after physical exertion may be complicated
scious and the airway is not secured, arrange the insulation around
by rhabdomyolysis, myoglobinuria, acute renal failure, and dissem-
the patient lying in a recovery (lateral decubitus) position. Rewarm-
inated intravascular coagulation (DIC).
ing in the field with heated intravenous fluids and warm humidified
Symptoms are often vague, and patients may not
gases is not active rewarming must not delay
realise that heat is the cause. Symptoms may include weakness,
transport to a hospital where advanced rewarming techniques,
dizziness, headache, nausea, and sometimes vomiting. Syncope due
continuous monitoring and observation are available.
to standing for long periods in the heat (heat syncope) is common
and may mimic cardiovascular disorders. On examination, patients
Transport. Transport patients with hypothermia stage I to the
appear tired and are usually sweaty and tachycardic. Mental status
nearest hospital. In hypothermia stage II–IV, signs of prehospital
is typically normal, unlike in heatstroke. Temperature is usually
cardiac instability (i.e. systolic blood pressure <90 mmHg, ventri-
normal and, when elevated, usually does not exceed 40 ◦C.
cular arrhythmia, core temperature <28 ◦C) should determine the
Diagnosis is clinical and requires exclusion of other
choice of admitting hospital. If any signs of cardiac instability are
possible causes (e.g. hypoglycaemia, acute coronary syndrome,
present, transport the patient to an ECLS centre, contacting them
infections). Laboratory testing is required only if needed to rule
well in advance to ensure that the hospital can accept the patient
out other disorders.
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
Cooling techniques.
Several cooling methods have been
Fluids and electrolyte replacement.
Treatment involves remov-
described, but there are few formal trials to determine which
ing patients to a cool environment, lying them flat, and giving IV
is optimal. Simple cooling techniques include drinking cold flu-
fluids and electrolyte replacement therapy; oral rehydration may
ids, fanning the completely undressed patient and spraying tepid
not be effective in rapidly replacing electrolytes, but may be a more
water on the patient. Ice packs over areas where there are large
practical treatment. Rate and volume of rehydration are guided by
superficial blood vessels (axillae, groins, neck) may also be useful.
age, underlying disorders, and clinical response. Replacement of
Surface cooling methods may cause shivering. In cooperative sta-
1–2 L crystalloids at 500 mL h−1 is often adequate. External cool-
ble patients, immersion in cold water can be however,
ing measures are usually not required. Consider external cooling in
this may cause peripheral vasoconstriction, shunt blood away from
patients with a core temperature of ≥40 ◦C.
the periphery and reduce heat dissipation. Immersion is also not
practical in the sickest patients.
Further techniques to cool patients with hyperthermia are sim-
ilar to those used for targeted temperature management after
Heat stroke (HS) is defined as hyperthermia
cardiac arrest (see post resuscitation intravenous flu-
accompanied by a systemic inflammatory response with a core
ids will decrease body temperature. Gastric,
temperature >40 ◦C, accompanied by mental state change and vary-
or bladder lavage with cold water will lower the core temperature.
ing levels of organ dysfunction.
Intravascular cooling techniques include the use of cold IV fluids,
There are two forms of HS:
intravascular cooling cathetersextracorporeal circuits,
1. Classic (non-exertional) heat stroke (CHS) occurs during high
e.g. continuous veno-venous haemofiltration or cardiopulmonary
environmental temperatures and often effects the elderly during
There are no specific drug therapies
2. Exertional heat stroke (EHS) occurs during strenuous physi-
in heat stroke that lower core temperature. There is no good evi-
cal exercise in high environmental temperatures and/or high
dence that antipyretics (e.g. non-steroidal anti-inflammatory drugs
humidity and usually effects healthy young
or paracetamol) are effective in heat stroke. Diazepam may be use-
ful to treat seizures and facilitate cooling.has not been
Mortality from heat stroke ranges between 10 and
The elderly are at increased risk for
heat-related illness because of underlying illness, medication
Malignant hyperthermia
use, declining thermoregulatory mechanisms and limited social
Malignant hyperthermia is a life-threatening genetic sensitivity
support. There are several risk factors: lack of acclimatisation, dehy-
of skeletal muscles to halogenated volatile anaesthetics and depo-
dration, obesity, alcohol, cardiovascular disease, skin conditions
larising neuromuscular blocking drugs, occurring during or after
(psoriasis, eczema, scleroderma, burn, cystic fibrosis), hyper-
anaesthesia.triggering agents immediately; give oxygen,
thyroidism, phaeochromocytoma and drugs (anticholinergics,
correct acidosis and electrolyte abnormalities. Start active cooling
diamorphine, cocaine, amphetamine, phenothiazines, sympath-
and give dantrolene.
omimetics, calcium channel blockers, beta-blockers).
Other drugs such as 3,4-methylenedioxymethamphetamine
Heat stroke can resemble septic shock and may
(MDMA, ‘ecstasy') and amphetamines also cause a condition
be caused by similar mechanisms.single centre case series
similar to malignant hyperthermia and the use of dantrolene may
reported 14 ICU deaths in 22 heat stroke patients admitted to ICU
with multiple organ included:
Modifications to cardiopulmonary resuscitation.
• core temperature ≥40 ◦C;
specific studies of cardiac arrest in hyperthermia. If cardiac arrest
• hot, dry skin (sweating present in about 50% of cases of exertional
occurs, follow standard guidelines and continue cooling the patient.
Use the same cooling techniques as for targeted temperature
• early signs and symptoms (e.g. extreme fatigue, headache, faint-
management after cardiac arrest (see Section 5 Post-resuscitation
ing, facial flushing, vomiting and diarrhoea);
defibrillation using standard energy levels. Animal
• cardiovascular
studies suggest the prognosis is poor compared with normothermic
cardiac arrest.risk of unfavourable neurological outcome
• respiratory dysfunction including acute respiratory distress syn-
increases by 2.26 (odds ratio) for each degree of body temperature
>37 ◦C.
• central nervous system dysfunction including seizures and
• liver and renal failure
• coagulopathy;
• rhabdomyolysis.
Hypovolaemia is a potentially treatable cause of cardiac arrest
that usually results from a reduced intravascular volume (i.e. hae-
Other clinical conditions presenting with increased core tem-
morrhage), but relative hypovolaemia may also occur in patients
perature need to be considered, including drug toxicity, drug
with severe vasodilation (e.g. anaphylaxis, sepsis). Hypovolaemia
withdrawal syndrome, serotonin syndrome, neuroleptic malignant
from mediator-activated vasodilation and increased capillary per-
syndrome, sepsis, central nervous system infection, endocrine dis-
meability is a major factor causing cardiac arrest in severe
orders (e.g. thyroid storm, phaeochromocytoma).
from blood loss, is a leading cause
The mainstay of treatment is supportive therapy
of death in traumatic cardiac arrest.blood loss is usually
and rapidly cooling the patient.cooling in the prehospi-
obvious, e.g. trauma, haematemesis, haemoptysis, but may be more
tal setting if possible. Aim to rapidly reduce the core temperature
challenging to diagnose when occult, e.g. gastrointestinal bleed-
to approximately 39 ◦C. Patients with severe heat stroke need to
ing or rupture of an aortic aneurysm. Patients undergoing major
be managed in an ICU environment. Large volumes of fluids and
surgery are at high-risk from hypovolaemia due to post-operative
correction of electrolyte abnormalities may be required (see hypo-
haemorrhage and must be appropriately monitored (see perioper-
/hyperkalaemia and other electrolyte disorders).
ative cardiac arrest).
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
Depending on the suspected cause, initiate volume therapy with
The European Academy of Allergy and Clinical Immunology's
warmed blood products and/or crystalloids, in order to rapidly
(EAACI) Taskforce on Anaphylaxis state that anaphylaxis is highly
restore intravascular volume. At the same time, initiate immedi-
likely when any one of the following three criteria is
ate intervention to control haemorrhage, e.g. surgery, endoscopy,
1. Acute onset of an illness (minutes to several hours) with involve-
endovascular techniques,treat the primary cause (e.g. anaphy-
ment of the skin, mucosal tissue, or both (e.g. generalised hives,
lactic shock). In the initial stages of resuscitation use any crystalloid
pruritus or flushing, swollen lips–tongue–uvula) and at least one
solution that is immediately available. If there is a qualified sono-
of the following:
grapher able to perform ultrasound without interruption to chest
compressions, e.g. during rhythm check or ventilations, it may be
bronchospasm, stridor, reduced peak expiratory flow (PEF),
considered as an additional diagnostic tool in hypovolaemic cardiac
b. Reduced blood pressure or associated symptoms of end-organ
Treatment recommendations for cardiac arrest and periarrest
dysfunction, e.g. hypotonia (collapse), syncope, incontinence.
situations in anaphylaxis and trauma are addressed in separate
2. Two or more of the following that occur rapidly after exposure
sections because of the need for specific therapeutic approaches.
to a likely allergen for that patient (minutes to several hours):
a. Involvement of the skin–mucosal tissue, e.g. generalised
hives, itch-flush, swollen lips–tongue–uvula.
Definition. A precise definition of anaphylaxis is not important
for its emergency treatment.European Academy of Allergy
bronchospasm, stridor, reduced PEF, hypoxaemia.
and Clinical Immunology Nomenclature Committee proposed
c. Reduced blood pressure or associated symptoms, e.g. hypoto-
the following broad definition:is a severe, life-
nia (collapse), syncope, incontinence.
threatening, generalised or systemic hypersensitivity reaction. This
d. Persistent gastrointestinal symptoms, e.g. crampy abdominal
is characterised by rapidly developing life-threatening airway
pain, vomiting.
and/or breathing and/or circulation problems usually associated
3. Reduced blood pressure after exposure to known allergen for
with skin and mucosal changes.
that patient (minutes to several hours):
a. Infants and children: low systolic blood pressure (<70 mmHg
from 1 month to 1 year; <70 mmHg + (2 × age) from 1 year to
Epidemiology. Anaphylaxis is common and affects about 1 in 300
10 years; <90 mmHg from 11 to 17 years) or >30% decrease in
of the European population at some stage in their lives, with an
systolic blood pressure.
incidence from 1.5 to 7.9 per 100,000
b. Adults: systolic blood pressure of <90 mmHg or >30% decrease
laxis can be triggered by any of a very broad range of triggers with
from that person's baseline.
food, drugs, stinging insects, and latex the most commonly iden-
tified triggers.is the commonest trigger in children and
Treatment. The evidence supporting specific interventions for
drugs the commonest in adults.any food or drug can
the treatment of anaphylaxis is limited.systematic ABCDE
be implicated, but certain foods (nuts) and drugs (muscle relax-
approach to recognise and treat anaphylaxis is recommended
ants, antibiotics, nonsteroidal anti-inflammatory drugs and aspirin)
with immediate administration of intramuscular (IM) adrenaline
cause most reactions.significant number of cases of anaphy-
(Treat life-threatening problems as you find them. The
laxis are idiopathic. Between 1992 and 2012 in the UK, admission
basic principles of treatment are the same for all age groups. Moni-
and fatality rates for drug- and insect sting-induced anaphylaxis
tor all patients who have suspected anaphylaxis as soon as possible
were highest in the group aged 60 years and older. In contrast,
(e.g. by ambulance crew, in the emergency department, etc.). Min-
admissions due to food-triggered anaphylaxis were most common
imum monitoring includes pulse oximetry, non-invasive blood
in young people, with a marked peak in the incidence of fatal food
pressure and a 3-lead ECG.
reactions during the second and third decades of life.
Patients with anaphylaxis can deteriorate
The overall prognosis of anaphylaxis is good, with a case fatal-
and are at risk of cardiac arrest if made to sit up or stand up.
ity ratio of less than 1% reported in most population-based studies.
patients should be placed in a comfortable position. Patients with
The European Anaphylaxis Registry reported that only 2% of 3333
airway and breathing problems may prefer to sit up, as this will
cases were associated with cardiac arrest.intensive care unit
make breathing easier. Lying flat with or without leg elevation is
admission is required, survival to discharge is over 90%. Over the
helpful for patients with a low blood pressure.
period 2005–2009, there were 81 paediatric and 1269 adult admis-
Remove the trigger (if possible).
Stop any drug suspected of
sions with anaphylaxis admitted to UK critical care units. Survival
causing anaphylaxis. Remove the stinger after a bee/wasp sting.
to discharge was 95% for children, and 92% for adults.
Early removal is more important than the method of
Anaphylaxis and risk of death is increased in those with pre-
not delay definitive treatment if removing the trigger is not feasible.
existing asthma, particularly if the asthma is poorly controlled,
Cardiac arrest following anaphylaxis.
Start CPR immediately and
severe or in asthmatics who delay treatment.anaphy-
follow current guidelines. Prolonged CPR may be necessary. Rescu-
laxis is fatal, death usually occurs very soon after contact with the
ers should ensure that help is on its way as early ALS is essential.
trigger. From a case series, fatal food reactions cause respiratory
Airway obstruction.
Anaphylaxis can cause airway swelling and
arrest typically within 30–35 min; insect stings cause collapse from
obstruction. This will make airway and ventilation interventions
shock within 10–15 min; and deaths caused by intravenous med-
(e.g. bag-mask ventilation, tracheal intubation, cricothyroidotomy)
ication occur most commonly within 5 min. Death never occurred
difficult. Consider early tracheal intubation before airway swelling
more than 6 h after contact with the trigger.
makes this difficult. Call for expert help early.
Recognition of an anaphylaxis. Anaphylaxis is the likely diagno-
sis if a patient who is exposed to a trigger (allergen) develops
Adrenaline (first line treatment). Adrenaline is the most impor-
a sudden illness (usually within minutes) with rapidly develop-
tant drug for the treatment of there
ing life-threatening airway and/or breathing and/or circulation
are no randomised controlled is a logical
problems usually associated with skin and mucosal changes. The
treatment and there is consistent anecdotal evidence suppor-
reaction is usually unexpected.
ting its use to ease bronchospasm and circulatory collapse. As an
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
Fig. 4.2. Anaphylaxis treatment algorithm.
Reproduced with permission from Elsevier Ireland Ltd.
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
alpha-receptor agonist, it reverses peripheral vasodilation and
paediatric settings by those familiar with its use (e.g. paediatric
reduces oedema. Its beta-receptor activity dilates the bronchial air-
anaesthetists, paediatric emergency physicians, paediatric inten-
ways, increases the force of myocardial contraction, and suppresses
sivists) and if the patient is monitored and IV access is already
histamine and leukotriene release. Activation of beta-2 adrenergic
available. There is no evidence on which to base a dose recom-
receptors on mast cell surfaces inhibit their activation, and early
mendation – the dose is titrated according to response. A child
adrenaline attenuates the severity of IgE-mediated allergic reac-
may respond to a dose as small as 1 mcg kg−1. This requires very
tions. Adrenaline is most effective when given early after the onset
careful dilution and checking to prevent dose errors.
of the adverse effects are extremely rare with cor-
rect IM doses.
Adrenaline intravenous/intraosseous dose (in cardiac arrest only).
Give adrenaline to all patients with life-threatening features.
Cardiac arrest with suspected anaphylaxis should be treated with
If these features are absent but there are other features of a sys-
standard doses of IV or intraosseous (IO) adrenaline for cardiac
temic allergic reaction, the patient needs careful observation and
arrest. If this is not feasible, consider IM adrenaline if cardiac arrest
symptomatic treatment using the ABCDE approach.
is imminent or has just occurred.
The intramuscular (IM) route is the
best for most individuals who have to give adrenaline to treat
Oxygen (give as soon as available).
Initially, give the highest
anaphylaxis. Monitor the patient as soon as possible (pulse, blood
concentration of oxygen possible using a mask with an oxy-
pressure, ECG, pulse oximetry). This will help monitor the response
gen high-flow oxygen (usually greater than
to adrenaline. The IM route has several benefits:
10 L min−1 to prevent collapse of the reservoir during inspiration.
If the patient's trachea is intubated, ventilate the lungs with high
There is a greater margin of safety.
concentration oxygen using a self-inflating bag.
It does not require intravenous access.
• The IM route is easier to learn.
Fluids (give as soon as available).
Large volumes of fluid may
• Patients with known allergies can self-administer IM adrenaline.
leak from the patient's circulation during anaphylaxis. There will
also be vasodilation. If IV access has been gained, infuse IV fluids
The best site for IM injection is the anterolateral aspect of the
immediately. Give a rapid IV fluid challenge (20 mL kg−1) in a child
middle third of the thigh. The needle for injection needs to be long
or 500–1000 mL in an adult and monitor the response; give further
enough to ensure that the adrenaline is injected into
doses as necessary. There is no evidence to support the use of col-
The subcutaneous or inhaled routes for adrenaline are not recom-
loids over crystalloids in this setting. Consider colloid infusion as
mended for the treatment of anaphylaxis because they are less
a cause in a patient receiving a colloid at the time of onset of an
effective than the IM
anaphylaxis and stop the infusion. A large volume of fluid may be
Adrenaline intramuscular dose.
The evidence for the recom-
mended doses is limited. The EAACI suggests IM adrenaline
If IV access is delayed or impossible, the IO route can be used for
(1 mg mL−1) should be given a dose of 10 mcg kg−1 of body weight
fluids or drugs. Do not delay the administration of IM adrenaline
to a maximum total dose of 0.5
while attempting IO access.
The following doses are based on what is considered to be safe
Antihistamines (give after initial resuscitation).
and practical to draw up and inject in an emergency (equivalent
are a second line treatment for anaphylaxis. The evidence to
volume of 1:1000 adrenaline is shown in brackets):
support their use is limited, but there are logical reasons for
>12 years and adults
500 microgram IM (0.5 mL)
their use.1-antihistamines help counter histamine-mediated
300 microgram IM (0.3 mL)
vasodilation, bronchoconstriction, and particularly cutaneous
>6 months–6 years
150 microgram IM (0.15 mL)
symptoms. There is little evidence to support the routine use of an
150 microgram IM (0.15 mL)
H2-antihistamine (e.g. ranitidine, cimetidine) for the initial treat-
Repeat the IM adrenaline dose if there is no improve-
ment of anaphylaxis.
ment in the patient's condition within 5 min. Further doses can
be given at about 5-min intervals according to the patient's
Glucocorticosteroids (give after initial resuscitation).
roids may help prevent or shorten protracted reactions, although
Intravenous adrenaline (for specialist use only).
the evidence is limited.asthma, early corticosteroid treatment
greater risk of causing harmful side effects by inappropriate
is beneficial in adults and children. There is little evidence on which
dosage or misdiagnosis of anaphylaxis when using intravenous (IV)
to base the optimum dose of hydrocortisone in anaphylaxis.
adrenaline.adrenaline should only be used by those expe-
Other drugs.
rienced in the use and titration of vasopressors in their normal
The presenting symptoms and signs of severe
clinical practice (e.g. anaesthetists, emergency physicians, inten-
anaphylaxis and life-threatening asthma can be the same. Consider
sive care doctors). In patients with a spontaneous circulation, IV
further bronchodilator therapy with salbutamol (inhaled or IV),
adrenaline can cause life-threatening hypertension, tachycardia,
ipratropium (inhaled), aminophylline (IV) or magnesium (IV) (see
arrhythmias, and myocardial ischaemia. If IV access is not available
asthma). IV magnesium is a vasodilator and can make hypotension
or not achieved rapidly, use the IM route for adrenaline. Patients
who are given IV adrenaline must be monitored – continuous ECG
Cardiac drugs.
Adrenaline remains the first line vasopressor
and pulse oximetry and frequent non-invasive blood pressure mea-
for the treatment of anaphylaxis. There are animal studies and
surements as a minimum. Patients who require repeated IM doses
case reports describing the use of other vasopressors and inotropes
of adrenaline may benefit from IV adrenaline. It is essential that
(noradrenaline, vasopressin, terlipressin metaraminol, methoxam-
these patients receive expert help early.
ine, and glucagon) when initial resuscitation with adrenaline and
Adrenaline intravenous dose (for specialist use only).
fluids has not been these drugs only in spe-
• Adults: Titrate IV adrenaline using 50 microgram boluses accord-
cialist settings (e.g. ICU) where there is experience in their use.
ing to response. If repeated adrenaline doses are needed, start an
Glucagon can be useful to treat anaphylaxis in a patient taking
IV adrenaline infusion.
a case reports of cardiac arrest suggest
• Children: IM adrenaline is the preferred route for children hav-
cardiopulmonary bypassmechanical chest compression
ing anaphylaxis. The IV route is recommended only in specialist
devices may also be helpful.
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
Investigations. Undertake the usual investigations appropriate for
treatment of reversible causes, which takes priority over chest com-
a medical emergency, e.g. 12-lead ECG, chest X-ray, urea and elec-
trolytes, arterial blood gases, etc.
Mast cell tryptase.
The specific test to help confirm a diagnosis
Diagnosis. The diagnosis of traumatic cardiac arrest is made clin-
of anaphylaxis is measurement of mast cell tryptase. Tryptase is the
ically. The patient presents with agonal or absent spontaneous
major protein component of mast cell secretory granules. In ana-
respiration and absence of a central pulse.
phylaxis, mast cell degranulation leads to markedly increased blood
A peri-arrest state is characterised by cardiovascular instabil-
tryptase concentrations. Tryptase concentrations in the blood may
ity, hypotension, loss of peripheral pulses in uninjured regions and
not increase significantly until 30 min or more after the onset of
a deteriorating conscious level without obvious central nervous
symptoms, and peak 1–2 h after onset.half-life of tryptase is
system (CNS) cause. If untreated, this state is likely to progress to
short (approximately 2 h), and concentrations may be back to nor-
cardiac arrest. Rapid focused ultrasound assessment may be help-
mal within 6–8 h, so timing of any blood samples is very important.
ful in the immediate diagnosis and management, but should not
The time of onset of the anaphylaxis is the time when symptoms
delay resuscitative
were first noticed.
It is vital that a medical cardiac arrest is not misdiagnosed as
(a) Minimum: one sample at 1–2 h after the start of symptoms.
a TCA and must be treated with the universal ALS algorithm. Car-
(b) Ideally: Three timed samples:
diac arrest or other causes of sudden loss of consciousness (e.g.
• Initial sample as soon as feasible after resuscitation has started –
hypoglycaemia, stroke, seizures) may cause a secondary traumatic
do not delay resuscitation to take sample.
event. Some observational studies have reported that about 2.5%
• Second sample at 1–2 h after the start of symptoms.
of non-traumatic OHCAs occur in these cases, shock-
• Third sample either at 24 h or in convalescence (for example in a
able rhythms (VF/pVT) are more common.primary cause of
follow-up allergy clinic). This provides baseline tryptase levels –
the cardiac arrest can be elucidated from information about past
some individuals have an elevated baseline level.
medical history, events preceding the accident (if possible), and a
systematic post-ROSC assessment, including a 12-lead ECG.
Serial samples have better specificity and sensitivity than a sin-
gle measurement in the confirmation of anaphylaxis.
Prognostic factors and withholding resuscitation. There are no reli-
able predictors of survival for traumatic cardiac arrest. Factors
Discharge and follow-up. Patients who have had suspected anaphy-
that are associated with survival include the presence of reactive
laxis (i.e. an airway, breathing or circulation problem) should be
pupils, an organised ECG rhythm and respiratory activity.
treated and then observed in a clinical area with facilities for treat-
Short duration of CPR and prehospital times have also been associ-
ing life-threatening ABC problems. Patients with a good response
ated with positive outcomes.
to initial treatment should be warned of the possibility of an early
A large systematic review reported an overall survival rate of
recurrence of symptoms and in some circumstances should be kept
3.3% in blunt and 3.7% in penetrating trauma, with good neuro-
under observation. The exact incidence of biphasic reactions is
logical outcome in 1.6% of all cases.is age dependent,
unknown. Although studies quote an incidence of 1–20%, it is not
with children having a better prognosis than is
clear whether all the patients in these studies actually had anaphy-
considerable variation in reported mortality (range 0–27%) reflect-
laxis or whether the initial treatment was appropriate.is
ing heterogeneity in casemix and care in different systems. PEA,
no reliable way of predicting who will have a biphasic reaction. It
which in TCA may initially be a low output state, and asystole are
is therefore important that decisions about discharge are made for
the prevalent heart rhythms in TCA. Ventricular fibrillation (VF) is
each patient by an experienced clinician.
rare but carries the best prognosis.
Before discharge from hospital, all patients must:
One study reported good neurological outcome in 36.4% of TCA
Be reviewed by an allergy specialist and have a treatment plan
patients presenting with VF, but only in 7% with PEA and 2.7% of
based on their individual risk.
those in other studies of patients in non-shockable
Be given clear instructions to return to hospital if symptoms
rhythms have reported 100% mortality.American Col-
lege of Surgeons and the National Association of EMS physicians
Be considered for an adrenaline auto-injector, or given a
recommend withholding resuscitation in situations where death
ensured that appropriate training has
is inevitable or established and in trauma patients presenting with
apnoea, pulselessness and without organised ECG
Have a plan for follow-up, including contact with the patient's
ever, neurologically intact survivors initially presenting in this state
have been therefore recommend the following
Patients need to know the allergen responsible (if identified)
and how to avoid it. Patients need to be able to recognise the early
Consider withholding resuscitation in TCA in any of the follow-
symptoms of anaphylaxis, so that they can summon help quickly
and prepare to use their emergency medication. Although there
• no signs of life within the preceeding 15 min;
are no randomised clinical trials, there is evidence that individual-
• massive trauma incompatible with survival (e.g. decapitation,
ised action plans for self-management should decrease the risk of
penetrating heart injury, loss of brain tissue).
We suggest termination of resuscitative efforts should be con-
Traumatic cardiac arrest
sidered if there is:
Introduction. Traumatic cardiac arrest (TCA) carries a very high
• no ROSC after reversible causes have been addressed;
mortality, but in those where ROSC can be achieved, neurolog-
• no detectable ultrasonographic cardiac activity.
ical outcome in survivors appears to be much better than in
other causes of cardiac arrest.response to TCA is time-
Trauma care systems throughout Europe vary considerably
critical and success depends on a well-established chain of survival,
and we recommend establishing regional guidelines for treat-
including advanced prehospital and specialised trauma centre
ment of TCA and tailoring patient pathways to infrastructure and
care. Immediate resuscitative efforts in TCA focus on simultaneous
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
Fig. 4.3. Traumatic cardiac arrest algorithm.
Treatment. Emphasis on rapid treatment of all potentially
aetiology. In cardiac arrest caused by hypovolaemia, cardiac tam-
reversible pathology is the basis of treatment guidelines. These
ponade or tension pneumothorax, chest compressions are unlikely
principles are addressed in several treatment algorithms.
to be as effective as in normovolaemic cardiac arrest.
All algorithms attempt to rapidly address reversible causes of TCA
Because of this fact, chest compressions take a lower priority
in the prehospital and in-hospital phases of care. a
than the immediate treatment of reversible causes, e.g. thoraco-
traumatic cardiac (peri-) arrest algorithm, which is based on the
tomy, controlling haemorrhage, etc. In an out-of-hospital setting,
only essential life-saving interventions should be performed on
scene followed by rapid transfer to the nearest appropriate
Effectiveness of chest compressions.
Chest compressions are still
the standard of care in patients with cardiac arrest, irrespective of
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
manoeuvres and second-generation supraglottic airways to main-
Damage control
re suscitation
tain oxygenation if tracheal intubation cannot be accomplished
Positive pressure ventilation worsens hypotension by imped-
Hypotensive
Haemostatic
Damage control
ing venous return to the heart, particularly in hypovolaemic
tidal volumes and slow respiratory rates may
help optimise cardiac preload. Monitor ventilation with continuous
waveform capnography and adjust to achieve normocapnia.
Fig. 4.4. Principles of damage control resuscitation in trauma.
Thirteen percent of all cases of TCA are
caused by tension pneumothorax.decompress the chest in
Uncontrolled haemorrhage is the cause of trau-
TCA, perform bilateral thoracostomies in the 4th intercostal space,
matic cardiac arrest in 48% of all treatment of severe
extending to a clamshell thoracotomy if required. In the presence of
hypovolaemic shock has several elements. The main principle is
positive pressure ventilation, thoracostomies are likely to be more
to achieve ‘haemostasis without delay', usually with surgical or
effective than needle thoracocentesis and quicker than inserting a
radiological intervention. Temporary haemorrhage control can be
chest tube (see tension pneumothorax).
Cardiac tamponade and resuscitative thoracotomy.
Treat compressible external haemorrhage with direct pressure
ponade is the underlying cause of approximately 10% of cardiac
(with or without a dressing), use tourniquets if needed and/or
arrest in there is TCA and penetrating trauma
apply topical haemostatic
to the chest or epigastrium, immediate resuscitative thoracotomy
Non-compressible haemorrhage is more difficult. Use splints
(RT) via a clamshell be life chance
(pelvic splint), blood products, intravenous fluids and tranexamic
of survival is about 4 times higher in cardiac stab wounds than in
acid while moving the patient to surgical haemorrhage control.
Over the past 10 years the principle of ‘damage control resusci-
Resuscitative thoracotomy is also applied for other life threaten-
tation' has been adopted in trauma resuscitation for uncontrolled
ing injuries; the evidence was examined in guidelines
haemorrhage. Damage control resuscitation combines permissive
produced which recommend that, after arrival in hospital, the deci-
hypotension and haemostatic resuscitation with damage control
sion to proceed with RT should include the following criteria:
surgery. Limited general consensus have sup-
• blunt trauma patients with less than 10 min of prehospital CPR;
ported a conservative approach to intravenous fluid infusion, with
• penetrating torso trauma patients with less than 15 min of CPR.
permissive hypotension until surgical haemostasis is achieved. Per-
missive hypotension allows intravenous fluid administration to a
These guidelines estimate survival rates for RT of approximately
volume sufficient to maintain a radial pulse.
15% for all patients with penetrating wounds and 35% for patients
Haemostatic resuscitation is the very early use of blood prod-
with a penetrating cardiac wound. In contrast, survival from RT
ucts as primary resuscitation fluid to prevent exsanguination
following blunt trauma is dismal, with survival rates of 0–2% being
by trauma-induced coagulopathy.recommended ratio of
packed red cells, fresh frozen plasma and platelets is
Successful RT is time critical. One UK service recommends that
services have also started using blood products in the prehospital
if surgical intervention cannot be accomplished within 10 min after
loss of pulse in patients with penetrating chest injury, on scene RT
Simultaneous damage control surgery and haemostatic resus-
should be considered.on this approach, of 71 patients who
citation using massive transfusion protocols are the
underwent RT at scene, 13 patients survived and 11 of these made
principles of damage control resuscitation in patients with exsan-
a good neurological recovery.
guinating injuries
The prerequisites for a successful RT can be summarised as the
Although the evidence for permissive hypotension during resus-
‘four Es rule' (4E):
citation is limited, particularly with regards to blunt trauma,
permissive hypotension has been endorsed in both civilian and
Expertise: teams that perform RT must be led by a highly trained
military aiming for a systolic blood pressure
and competent healthcare practitioner. These teams must oper-
of 80–90 mmHg. Caution is advised with this strategy in patients
ate under a robust governance framework.
with traumatic brain injury were a raised intracranial pressure
Equipment: adequate equipment to carry out RT and to deal with
may require a higher cerebral perfusion pressure. The duration
the intrathoracic findings is mandatory.
of hypotensive resuscitation should not exceed 60 min, because
Environment: ideally RT should be carried out in an operating the-
the risks of irreversible organ damage then exceed its intended
atre. RT should not be carried out if there is inadequate physical
access to the patient, or if the receiving hospital is not easy to
Tranexamic acid (TXA) (loading dose 1 g over 10 min followed
by infusion of 1 g over 8 h) increases survival from traumatic
Elapsed time: the time from loss of vital signs to commencing a
is most effective when administered within the
RT should not be longer than 10 min.
first hour and certainly within the first 3 h following
If any of the four criteria is not met, RT is futile and exposes the
Give TXA in the prehospital setting when possible.
team to unnecessary risks.
Hypoxaemia due to airway obstruction and trau-
Needle aspiration of tamponade, with or without ultrasound
matic asphyxia has been reported as cause of traumatic cardiac
guidance, is unreliable because the pericardium is commonly
arrest in 13% of all airway management and
full of clotted blood.thoracotomy is not possible, how-
ventilation can reverse hypoxic cardiac arrest and it is essential
ever, consider ultrasound guided pericardiocentesis to treat TCA
to establish and maintain oxygenation of trauma patients with
associated with suspected cardiac tamponade. Non-image guided
a severely compromised airway. Tracheal intubation in trauma
pericardiocentesis is an alternative, only if ultrasound is not avail-
patients is a difficult procedure with a high failure rate if car-
able. Placement of a pericardial drain may be beneficial in some
ried out by less experienced care providers.basic airway
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
Diagnostics. Ultrasonography should be used in the evaluation of
to re-tension. Chest drain tubes may become blocked with lung or
the compromised trauma patient to target life-saving interven-
blood clots and have the potential to kink.
tions if the cause of shock cannot be established
Haemoperitoneum, haemo- or pneumothorax and cardiac tampo-
nade can be diagnosed reliably in minutes, even in the prehospital
whole-body computed tomography (WBCT) scan-
ning as part of the primary survey may improve outcome in major
Cardiac tamponade occurs when the pericardial sac is filled with
is increasingly employed to identify the source
fluid under pressure, which leads to compromise of cardiac function
of shock and to guide subsequent haemorrhage control.
and ultimately cardiac arrest. The condition most commonly occurs
after penetrating trauma and cardiac surgery. Mortality is high and
Prehospital care. Short prehospital times are associated with
immediate decompression of the pericardium is required to give
increased survival rates for major trauma and TCA. The time elapsed
any chance of survival.
between injury and surgical control of bleeding should therefore
be minimised and the patient should be immediately transferred
to a trauma centre for ongoing damage control resuscitation.
Thoracotomy. The criteria and prerequisites for resuscitative tho-
‘scoop and run' concept for these patients may be life saving.
racotomy in patients with penetrating trauma to the chest or
epigastrium are described in section on traumatic cardiac arrest.
Treatment of the tamponade following cardiac surgery is addressed
in the section on cardiac arrest following cardiac surgery.
Tension pneumothorax defined as haemodynamic compro-
Pericardiocentesis. If
mise in a patient with an expanding intrapleural air mass is a
ultrasound-guided pericardiocentesis to treat cardiac arrest
treatable cause of cardiac arrest and should be excluded during
associated with suspected traumatic or non-traumatic cardiac
CPR.pneumothorax can occur in a variety of clinical
tamponade. Non-image guided pericardiocentesis is an alternative,
situations including trauma, asthma and other respiratory dis-
only if ultrasound is not available.
ease, but can also be iatrogenic following invasive procedures, e.g.
attempts at central venous catheter insertion. It is more common
and often more severe in patients undergoing positive pressure
incidence of tension pneumothorax is approx-
Pulmonary embolism
imately 5% in major trauma patients treated in the prehospital
Introduction. Cardiac arrest from acute pulmonary embolism is the
setting (13% of those developing TCA), and less than 1% of adults
most serious clinical presentation of venous thromboembolism, in
most cases originating from a deep venous thrombosis
The reported incidence of cardiac arrest caused by pulmonary
embolism is 2–9% of all OHCAs,5–6% of all in-hospital
Diagnosis of tension pneumothorax in a patient with cardiac
cardiac it is likely to be underestimated. Over-
arrest or haemodynamic instability must be based on clinical
all survival is treatments for cardiac arrest
examination. The symptoms include haemodynamic compromise
resulting from pulmonary embolism include administration of fib-
(hypotension or cardiac arrest) in conjunction with signs suggestive
rinolytics, surgical embolectomy and percutaneous mechanical
of a pneumothorax (preceding respiratory distress, hypoxia, absent
unilateral breath sounds on auscultation, subcutaneous emphy-
sema) and mediastinal shift (tracheal deviation and jugular venous
Diagnosis. Diagnosis of acute pulmonary embolism during cardiac
distention).CPR, presentation is not always classical, but
arrest is difficult. One study has reported correct recognition of
when it is suspected in the presence of cardiac arrest or severe
the underlying causes in up to 85% of all in-hospital resuscitation
hypotension, chest decompression should be carried out immedi-
accurate prehospital diagnosis of acute pulmonary
ately before radiographic confirmation.
embolism is particularly
The 2014 European Society of Cardiology Guidelines on
the diagnosis and management of acute pulmonary embolism
Needle decompression. Needle chest decompression is rapid and
define ‘confirmed pulmonary embolism' as a probability of pul-
within the skill set of most ambulance personnel but is of limited
monary embolism high enough to indicate the need for specific
value.significant proportion of patients have chest wall
thickness which makes needle decompression with a standard
Clinical history and assessment, capnography and echocardiog-
length 14-gauge cannula ineffective.are also prone
raphy (if available) can all assist in the diagnosis of acute pulmonary
to kinking and attempt at needle decompression
embolism during CPR with varying degrees of specificity and sen-
should be followed by insertion of a chest tube (see asthma).
• Common symptoms preceding cardiac arrest are sudden onset of
Thoracostomy. Tracheal intubation, positive pressure ventilation
dyspnoea, pleuritic or substernal chest pain, cough, haemoptysis,
and formal chest decompression effectively treats tension pneu-
syncope and signs of DVT in particular (unilateral low extremity
mothorax in patients with TCA. Simple thoracostomy is easy
swelling).pulmonary embolism may not be symp-
to perform and used routinely by several prehospital physician
tomatic until it presents as sudden cardiac
consists of the first stage of standard chest
• Obtain information about past medical history, predisposing fac-
tube insertion – a simple incision and rapid dissection into the
tors, and medication that may support diagnosis of pulmonary
pleural space in the positive pressure ventilated patient (see trau-
embolism, although none of these are specific,
matic cardiac arrest). Chest tube insertion is then carried out after
◦ Previous pulmonary embolism or DVT
the resuscitation phase. This requires additional equipment, takes
◦ Surgery or immobilisation within the past four weeks
longer to perform and creates a closed system that has the potential
◦ Active cancer
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
◦ Clinical signs of DVT
• Consider the use of a mechanical chest compression device when
◦ Oral contraceptive use or hormone replacement therapy.
maintenance of high quality chest compressions is needed for a
◦ Long-distance flights
prolonged time.
In as many as 30% of the patients with pulmonary embolism, no
Extracorporeal CPR.
Some observational studies suggest the
risk factors are apparent.
use of extracorporeal life support (ECLS) if cardiac arrest is asso-
• If a 12-lead ECG can be obtained before onset of cardiac arrest,
ciated with pulmonary embolism.implementation of
changes indicative of right ventricular strain may be found:
ECLS requires considerable resource and training. Its use should
◦ Inversion of T waves in leads V1–V4
be considered as a rescue therapy for those patients in whom ini-
◦ QR pattern in V1
tial ALS measures are unsuccessful and/or to facilitate pulmonary
◦ S1 Q3 T3 pattern (i.e. a prominent S wave in lead I, a Q wave
and inverted T wave in lead III)
Surgical embolectomy and mechanical thrombectomy.
◦ Incomplete or complete right bundle-branch block
of patients who underwent surgical embolectomy during CPR due
to pulmonary embolism was reported as 13% and 71% in two case
Cardiac arrest commonly presents as
series,these results were not compared with standard
2 readings (about 1.7 kPa/13 mmHg) while perform-
treatment. Routine use of surgical embolectomy or mechani-
ing high quality chest compressions may support a diagnosis of
cal thrombectomy for cardiac arrest from suspected pulmonary
pulmonary embolism, although it is a non-specific sign.
embolism is not recommended, but these methods may be con-
Consider emergency echocardiography performed by a qualified
sidered when pulmonary embolism is the known cause of cardiac
sonographer as an additional diagnostic tool to identify pul-
monary embolism if it can be performed without interruptions to
Percutaneous pulmonary thrombectomy.
In one case series, per-
chest compressions, e.g. during rhythm check. Echocardiographic
cutaneous pulmonary thrombectomy during CPR was successful in
findings are evident after acute obstruction of more than 30%
six of seven patients,larger studies are needed to validate
of the pulmonary arterial tree.echocardiographic
this method.
findings are an enlarged right ventricle with a flattened inter-
ventricular septum,absence of these features does
not exclude pulmonary of right ventricular
Post-resuscitation care. In patients with sustained ROSC, exclude
overload or dysfunction may also be caused by other cardiac or
intra-abdominal and intra-thoracic CPR-related injuries, especially
if a mechanical chest compression device was used simultaneously
More specific diagnostic methods, e.g. D-dimer testing, (com-
with administration of fibrinolytics.to identify and
puted tomographic) pulmonary angiography, lung scintigraphy,
treat the original cause of the pulmonary embolism. Evaluate the
or magnetic resonance angiography, are not recommended for a
risks of a further pulmonary embolism and treat accordingly.
cardiac arrest situation.
Coronary thrombosis
Modifications to cardiopulmonary resuscitation. A meta-analysis,
Coronary heart disease is the most frequent cause of OHCA.
which included patients with pulmonary embolism as a cause of
The peri-resuscitation management of acute coronary syndromes
cardiac arrest, concluded that fibrinolytics increased the rate of
is addressed in a separate chapter (see Section 8 Initial manage-
ROSC, survival to discharge and long-term neurological
ment of acute coronary syndromes).cardiac arrest centres,
A subgroup analysis of patients treated with thrombolytics com-
coronary artery occlusion or high degree stenoses can be identi-
pared with placebo in a randomised controlled not
fied and treated. Of all patients in OHCA, however, at least half are
prove survival difference. However, this study was not designed for
not transported to hospital when ROSC is not achieved (see Section
treatment of pulmonary embolism and not powered to reach signif-
10 Ethics of resuscitation and end-of-life decisions).
icance in this small subgroup. Some other non-randomised studies
proper diagnosis of the cause may be difficult in a patient already
have also documented use of thrombolytics in the treatment of
in cardiac arrest, if the initial rhythm is VF it is most likely that the
cardiac arrest due to acute pulmonary embolism, but evidence
cause is coronary artery disease with an occluded large coronary
for improved neurologically intact survival to hospital discharge
Consider transportation to hospital with ongoing CPR if treat-
In a cardiac arrest presumed to be caused by acute pul-
ment options are available that cannot be applied in the prehospital
monary embolism, follow the standard guidelines for ALS (see adult
setting, such as immediate coronary angiography, primary per-
advanced life decision to treat for acute pulmonary
cutaneous coronary intervention (PPCI) or other interventions
embolism must be taken early, when a good outcome is still possi-
such as (more rarely) pulmonary embolectomy (see pulmonary
ble. The following treatment modifications are recommended:
embolism). The decision to transport is complex and may depend
• Consider administration of fibrinolytic therapy when acute pul-
on local circumstances. Prehospital initiation of extracorporeal car-
monary embolism is a known or suspected cause of cardiac arrest.
diopulmonary life support (ECLS) requires specialised expertise
Ongoing CPR is not a contraindication to fibrinolysis. Despite
and its feasibility on a wide-scale has not been established.
increased risk of severe bleeding, fibrinolysis may be an effective
Mechanical chest compression devices maintain high quality CPR
treatment, which can be initiated without delay, even outside
during transport and PCI (see cardiac arrest in HEMS and air
specialised healthcare facilities. The potential benefit of fibri-
nolysis in terms of improved survival outweighs potential risks
There is limited evidence for recommending routine trans-
in a location where no alternative exists, e.g. in the prehospital
port to hospital with ongoing CPR. The decision will depend on
patient selection, availability of optimal methods for mechanical
• Once a fibrinolytic drug is administered, continue CPR for at least
or circulatory support during and after transport to the hospital,
60–90 min before terminating resuscitation attempts.
management of underlying pathology, treatment after ROSC, com-
vival and good neurological outcome have been reported in cases
plication rate and outcome. There are no large outcome studies
requiring in excess of 100 min of
available, but small case series suggest benefit in selected
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
Before definitive recommendations can be made, controlled studies
prolonged CPR, extracorporeal life support
Transport with ongoing CPR and immediate access to the
• Consult regional or national poisons centres for information on
catheterisation laboratory may be considered if a prehospital and
treatment of the poisoned patient. The International Programme
in-hospital infrastructure is available with teams experienced in
on Chemical Safety (IPCS) lists poison centres on its website:
mechanical or haemodynamic support and rescue PPCI with ongo-
ing CPR. Excellent cooperation is required between prehospital
• On-line databases for information on toxicology and hazardous
and in-hospital teams. A decision to transport with ongoing CPR
chemicals may be helpful:
should take into consideration a realistic chance of survival (e.g.
witnessed cardiac arrest with initial shockable rhythm (VF/pVT)
Specific therapeutic measures
and bystander CPR). Intermittent ROSC also strongly favours a deci-
There are few specific therapeutic measures for poisoning that
are useful immediately and improve outcomes: decontamination,
enhancing elimination, and the use of specific antidotes.
Many of these interventions should be used only based on expert
advice. For up-to-date guidance in severe or uncommon poisonings,
General considerations
seek advice from a poisons centre.
Introduction. Overall, poisoning rarely causes cardiac arrest or
hospital admissions are common, accounting for as
Decontamination. Decontamination is a process of removal of the
many as 140,000 admissions each year in the by
toxin from the body determined by the route of exposure:
therapeutic or recreational drugs and by household products are
• For dermal exposures initial management consists of clothing
the main reasons for hospital admission and poison centre calls.
removal and copious irrigation with water, except in case of reac-
Inappropriate drug dosing, drug interactions and other medication
tive alkali metals that can ignite.
errors can also cause harm. Accidental poisoning is commonest in
• Routine use of gastric lavage for gastrointestinal decontamina-
children. Homicidal poisoning is uncommon. Industrial accidents,
tion is no longer recommended. In the rare instances (e.g. lethal
warfare or terrorism can also cause exposure to toxins. Evidence
ingestion with recent exposure), it should only be performed
for treatment consists primarily of animal studies, case reports and
by individuals with proper training and expertise. Gastric lavage
may be associated with life-threatening complications, e.g. aspi-
ration pneumonitis, aspiration pneumonia, esophageal or gastric
Prevention of cardiac arrest. Assess the patient using system-
perforation, fluid and electrolyte imbalances, arrhythmia. It is
atic ABCDE approach. Airway obstruction and respiratory arrest
contraindicated if the airway is not protected and if a hydrocar-
secondary to a decreased conscious level is a common cause
bon with high aspiration potential or a corrosive substance has
of death after self-poisoning (benzodiazepines, alcohol, opiates,
tricyclics, tracheal intubation of uncon-
• The preferred method of gastrointestinal decontamination in
scious patients by trained personnel may decrease the risk of
patients with an intact or protected airway is activated charcoal. It
aspiration. Drug-induced hypotension usually responds to IV fluids,
is most effective if given within 1 h of the time of the
but occasionally vasopressor support (e.g. noradrenaline infusion)
Activated charcoal does not bind lithium, heavy metals and toxic
is required. Measure electrolytes (particularly potassium), blood
alcohols. Most common side effects are vomiting and consti-
glucose and arterial blood gases. Retain samples of blood and urine
pation. The evidence that active charcoal improves outcome is
for analysis. Patients with severe poisoning should be cared for in
• Based mainly on volunteer studies, consider whole-bowel
irrigation in potentially toxic ingestions of sustained-release or
Modifications to resuscitation.
enteric-coated drugs particularly for those patients presenting
Have a low threshold to ensure your personal safety where there
later than 2 h after drug ingestion when activated charcoal is
is a suspicious cause or unexpected cardiac arrest. This is espe-
less effective. It may be also used for the removal of substantial
cially so when there is more than one casualty.
amounts of iron, lithium, potassium, or packets of illicit drugs.
Avoid mouth-to-mouth breathing in the presence of chemicals
Whole-bowel irrigation is contraindicated in patients with bowel
such as cyanide, hydrogen sulphide, corrosives and organophos-
obstruction, perforation, ileus, and haemodynamic
• Avoid routine administration of laxatives (cathartics) and do not
Treat life-threatening tachyarrhythmias with cardioversion
use emetics (e.g. ipecac
according to the peri-arrest arrhythmia guidelines (see adult
advanced life support).includes correction of electrolyte
and acid-base abnormalities (see hypo-/hyperkalaemia and other
Enhanced elimination. Modalities removing a toxin from the body
once it has been absorbed include multiple-dose activated char-
• Try to identify the poison(s). Relatives, friends and ambulance
coal (MDAC), urinary alkalinisation and extracorporeal elimination
crews can provide useful information. Examination of the patient
may reveal diagnostic clues such as odours, needle marks, pupil
• MDAC, multiple doses of activated charcoal administered over
abnormalities, and signs of corrosion in the mouth.
several hours, can increase certain drug elimination.
• Measure the patient's temperature because hypo- or hyperther-
an initial dose of 50–100 g in adults (25–50 g in children).
mia may occur after drug overdose (see hypo-/hyperthermia).
• Urinary alkalinisation (urine pH ≥ 7.5) involves an IV sodium
• Be prepared to continue resuscitation for a prolonged period, par-
bicarbonate infusion. It is most commonly performed in patients
ticularly in young patients, as the poison may be metabolised or
with salicylate intoxication who do not need dialysis. Consider
excreted during extended resuscitation measures.
urine alkalinisation with high urine flow (about 600 mL h−1)
• Alternative approaches which may be effective in severely
in severe poisoning by phenobarbital and herbicides, e.g.
poisoned patients include: higher doses of medication than
2,4-dichlorophenoxyacetic acid or methylchlorophenoxypropi-
in standard protocols (e.g. high-dose insulin euglycemia)
onic acid (mecoprop). Hypokalaemia is the most common
non-standard drug therapies (e.g. IV lipid
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
• Haemodialysis removes drugs or metabolites with low molec-
A widening QRS complex (>100 ms) and right axis deviation
ular weight, low protein binding, small volumes of distribution
indicates a greater risk of arrhythmias.sodium bicar-
and high water solubility. In case of hypotension, use continuous
bonate (1–2 mmol kg−1) for the treatment of tricyclic-induced
veno-venous hemofiltration (CVVH) or continuous veno-venous
ventricular no study has investigated
haemodialysis (CVVHD) alternatively.
the optimal target arterial pH with bicarbonate therapy, a pH of
7.45–7.55 is of bicarbonate
Specific poisons
may resolve arrhythmias and reverse hypotension even in the
These guidelines address only some of the more common poi-
sons causing cardiac arrest.
Intravenous lipid infusions in experimental models of tricyclic
toxicity have suggested benefit but there are few human data.
Benzodiazepines. Overdose of benzodiazepines can cause loss of
Anti-tricyclic antibodies have also been beneficial in experimental
consciousness, respiratory depression and hypotension. Flumaze-
models of tricyclic small human study
nil, a competitive antagonist of benzodiazepines, may be used
provided evidence of safety but clinical benefit has not been
for reversal of benzodiazepine sedation when there is no his-
tory or risk of seizures. Reversal of benzodiazepine intoxication
There are no randomised controlled trials evaluating conven-
with flumazenil can be associated with significant toxicity
tional versus alternative treatments for cardiac arrest caused by
(seizure, arrhythmia, hypotension, and withdrawal syndrome) in
tricyclic toxicity. One small case series showed improvement
patients with benzodiazepine dependence or co-ingestion of pro-
with the use of sodium bicarbonate but the concomitant use of
convulsant medications such as tricyclic
physostigmin prevents the ability to generalise its results.
The routine use of flumazenil in the comatose overdose
patient is not recommended.There are no specific modifica-
Cocaine. Sympathetic overstimulation associated with cocaine
tions to the ALS algorithm required for cardiac arrest caused by
toxicity can cause agitation, tachycardia, hypertensive crisis,
hyperthermia and coronary vasoconstriction causing myocardial
ischaemia with angina.
Opioids. Opioid poisoning causes respiratory depression followed
In patients with severe cardiovascular toxicity, alpha blockers
by respiratory insufficiency or respiratory arrest. The respiratory
(lorazepam, diazepam),
effects of opioids are reversed rapidly by the opiate antagonist
calcium channel blockers sub-
lingual be used as needed to control
In severe respiratory depression caused by opioids, there are
hypertension, tachycardia, myocardial ischaemia and agitation.
fewer adverse events when airway opening, oxygen administration
The evidence for or against the use of beta-blocker drugs,
and ventilation are carried out before giving naloxone
including those beta-blockers with alpha blocking properties
use of naloxone can prevent the need for intubation. The preferred
(carvedilol and labetolol) is limited.optimal choice of
route for giving naloxone depends on the skills of the rescuer: intra-
anti-arrhythmic drug for the treatment of cocaine-induced tach-
venous (IV), intramuscular (IM), subcutaneous (SC), intraosseous
yarrhythmias is not known. If cardiac arrest occurs, follow standard
(IO) and intranasal (IN) routes are all non-
IV routes can be quicker because time is saved in not having to
establish IV access, which may be difficult in an IV drug abuser.
Local anaesthetics. Systemic toxicity of local anaesthetics involves
The initial doses of naloxone are 0.4–2 mg IV, IO, IM or SC, and
the central nervous and cardiovascular systems. Severe agitation,
may be repeated every 2–3 min. Additional doses may be needed
loss of consciousness, seizures, bradycardia, asystole or ventricu-
every 20–60 min. Intranasal dosing is 2 mg IN (1 mg in each nos-
lar tachyarrhythmias can all occur. Toxicity typically occurs in the
tril) which may be repeated every 5 min. Titrate the dose until the
setting of regional anaesthesia, when a bolus of local anaesthetic
victim is breathing adequately and has protective airway reflexes.
inadvertently enters an artery or vein (see perioperative cardiac
Large opioid overdoses may require a total dose of up to 10 mg of
patients treated with naloxone must be
Although there are many case reports and case series of patients
who were resuscitated after administration of IV lipid emulsion,
Acute withdrawal from opioids produces a state of sympathetic
evidence for its benefit in treating local anaesthetic-induced car-
excess and may cause complications such as pulmonary oedema,
diac arrest is limited. Despite the paucity of data, patients with
ventricular arrhythmias and severe agitation. Use naloxone rever-
both cardiovascular collapse and cardiac arrest attributable to local
sal of opioid intoxication with caution in patients suspected of
anaesthetic toxicity may benefit from treatment with intravenous
opioid dependence.
20% lipid emulsion in addition to standard ALS.an initial
There are no data on the use of any additional therapies beyond
intravenous bolus injection of 20% lipid emulsion 1.5 mL kg−1 over
standard ALS guidelines in opioid-induced cardiac arrest. In respi-
1 min followed by an infusion at 15 mL kg−1 h−1. Give up to a max-
ratory arrest there is good evidence for the use of naloxone, but not
imum of two repeat boluses at 5-min intervals and continue until
for any other adjuncts or changes in interventions.
the patient is stable or has received up to a maximum cumulative
dose of 12 mL kg−1 of lipid cardiac
Tricyclic antidepressants. This section addresses both tricyclic and
arrests drugs (e.g. adrenaline) should be given according to ALS
related cyclic drugs (e.g. amitriptyline, desipramine, imipramine,
guidelines, although animal studies provide inconsistent evidence
nortriptyline, doxepin, and clomipramine). Self-poisoning with
for their role in local anaesthetic toxicity.
tricyclic antidepressants is common and can cause hypotension,
seizures, coma and life-threatening arrhythmias. Cardiac toxicity
Beta-blockers. Beta-blocker toxicity causes bradyarrhythmias and
mediated by anticholinergic and Na+ channel-blocking effects can
negative inotropic effects that are difficult to treat, and can lead to
produce a wide complex tachycardia (VT). Hypotension is exacer-
cardiac arrest.
bated by alpha-1 receptor blockade. Anticholinergic effects include
Evidence for treatment is based on case reports and ani-
mydriasis, fever, dry skin, delirium, tachycardia, ileus, and urinary
mal studies. Improvement has been reported with glucagon
retention. Most life-threatening problems occur within the first 6 h
(50–150 mcg kg−1insulin and glucose,
after ingestion.
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
extracorporeal and intra-aortic balloon pump support,
In the case of cardiac arrest caused by cyanide, standard
calcium salts.
treatment fails to restore spontaneous circulation as long as cel-
lular respiration is blocked. Antidote treatment is needed for
Calcium channel blockers. Calcium channel blocker overdose is
reactivation of cytochrome oxidase.
emerging as a common cause of prescription drug poisoning
deaths.of short-acting drugs can rapidly progress
Carbon monoxide. Carbon monoxide poisoning is common. There
to cardiac arrest. Overdose by sustained-release formulations can
were about 25,000 carbon monoxide related hospital admissions
result in delayed onset of arrhythmias, shock, and sudden cardiac
reported yearly in the United monoxide levels do
collapse. The treatment for calcium channel blocker poisoning is
not correlate with the presence or absence of initial symptoms or
supported by low-quality
with later who develop cardiac arrest caused
Give calcium chloride 10% in boluses of 20 mL (or equivalent
by carbon monoxide rarely survive to hospital discharge, even if
dose of calcium gluconate every 2–5 min in severe bradycardia
ROSC is achieved.
or hypotension followed by an infusion if needed.
Give oxygen as soon as possible. The use of hyperbaric oxy-
While calcium in high doses can overcome some of the
gen has been used to treat carbon monoxide exposure in order to
adverse effects, it rarely restores normal cardiovascular status.
reduce the incidence of adverse neurologic
Haemodynamic instability may respond to high doses of insulin
two Cochrane reviews failed to demonstrate convincing benefit
(1 unit kg−1 followed by an infusion of 0.5–2.0 units kg−1 h−1) given
from hyperbaric oxygen therapy for patients with carbon monox-
with glucose supplementation and electrolyte monitoring in addi-
ide role of carbon monoxide in nitric oxide
tion to standard treatments including fluids and vasopressors (e.g.
release, reactive oxygen species formation, and its direct action
dopamine, norepinephrine, vasopressin).life
on ion channels may be more significant than its higher affinity
support (ECLS) was associated with improved survival in patients
for haemoglobin, which is treated by oxygen therapies.is
with severe shock or cardiac arrest at the cost of limb ischaemia,
unproven benefit for transporting critically ill post-arrest patients
thrombosis, and bleeding.Studies on decontamination, 4-
to a hyperbaric facility and such decision must be considered on
aminopyridine, atropine, glucagon, pacemakers, levosimendan,
a case-by-case basis.who develop myocar-
and plasma exchange reported variable
dial injury caused by carbon monoxide have an increased risk of
cardiac and all-cause mortality lasting at least seven years after
the event; it is reasonable to recommend cardiology follow-up for
Digoxin. Although cases of digoxin poisoning are fewer than those
involving calcium channel and beta-blockers, the mortality rate
from digoxin is far greater. Other drugs including calcium channel
blockers and amiodarone can also cause plasma concentrations of
B – SPECIAL ENVIRONMENTS
digoxin to rise. Atrioventricular conduction abnormalities and ven-
tricular hyperexcitability due to digoxin toxicity can lead to severe
Cardiac arrest in healthcare facilities
arrhythmias and cardiac arrest.
Specific antidote therapy with digoxin-specific antibody frag-
Perioperative cardiac arrest
ments (digoxin-Fab) should be used if there are arrhythmias
Introduction. Although the safety of routine surgical procedures
associated with haemodynamic instability.Digoxin-
has increased over recent decades, the greater number of proce-
Fab therapy may also be effective in poisoning from plants
dures being performed, particularly in more elderly patients and in
(e.g. oleander) and Chinese herbal medications containing car-
emergency situations has resulted in a broadly stable incidence of
diac Digoxin-Fab interfere with digoxin
perioperative cardiac arrests over the past decade.
immunoassay measurements and can lead to overestimation of
Although the features of perioperative cardiac arrest are often
plasma digoxin concentrations. In acute poisoning, give an initial
different to those of cardiac arrests occurring in the general hospital
bolus of 2 vials digoxin-Fab (38 mg per vial) and repeat dose if
population, the principles of treatment are similar. Perioperative
necessary.a cardiac arrest, consider administration of 2 up
cardiac arrest may be caused by the underlying condition being
to 10 vials IV over 30 min.
treated, physiological effects of the surgery, anaesthetic drugs and
fluids, complications relating to existing co-morbidities, or adverse
Cyanides. Cyanide is generally considered to be a rare cause of acute
poisoning; however, cyanide exposure occurs relatively frequently
in patients with smoke inhalation from residential or industrial
Epidemiology. The overall incidence of perioperative cardiac arrest
fires. Cyanides are also used in several chemical and industrial pro-
ranges from 4.3 to 34.6 per 10,000 wide
cesses. Its main toxicity results from inactivation of cytochrome
range reflects differences in case-mix (some include neonates
oxidase (at cytochrome a3), thus uncoupling mitochondrial oxida-
and/or cardiac surgery) and in the definition of perioperative. The
tive phosphorylation and inhibiting cellular respiration, even in the
incidence is higher in high-risk groups such as the elderly where
presence of adequate oxygen supply. Tissues with the highest oxy-
it has been reported as 54.4 per 10,000 in patients
gen needs (brain and heart) are the most severely affected by acute
undergoing emergency surgery where an incidence of 163 per
cyanide poisoning.
10,000 cases has been reported.age (<2 years old),
Patients with severe cardiovascular toxicity (cardiac arrest, car-
cardiovascular and respiratory comorbidities, increasing American
diovascular instability, metabolic acidosis, or altered mental status)
Society of Anesthesiologists (ASA) physical status classification,
caused by known or suspected cyanide poisoning should receive
preoperative shock, and surgery site have all been identified as
cyanide antidote therapy in addition to standard resuscitation, incl.
risk factors for perioperative cardiac
oxygen. Initial therapy should include a cyanide scavenger (either
The incidence of cardiac arrest attributable primarily to anaes-
hydroxocobalamin 100 mg kg−1 IV or a nitrite – i.e. IV sodium
thesia is a relatively small proportion of this overall incidence
nitrite and/or inhaled amyl nitrite), followed as soon as possible
and in recent studies is estimated to be 1.1–3.26 per 10,000
by IV sodium thiosulfate.and nitrites are
survival from perioperative cardiac
equally effective but hydroxocobalamin is safer because it does not
arrest is higher than from OHCA, with survival to hospital discharge
cause methaemoglobin formation or hypotension.
rates of 30–36.6% being reported
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
General versus regional anaesthesia.
The incidence of perioper-
cardiac arrest, ensuring that sufficient skilled assistance is
ative cardiac arrest during general anaesthesia (GA) is higher than
that of regional anaesthesia (RA). The incidence of cardiac arrest for
Catastrophic haemorrhage is usually obvious, but may
patients receiving general anaesthesia in a study from the Mayo
be occult it if involves bleeding into body compartments
Clinic was higher (almost 3 times higher, at 4.3 per 10,000) than
(abdomen, chest) or into soft tissues in patients with
that for those receiving regional anaesthesia or monitored anaes-
multiple limb fractures. Pelvic and retroperitoneal
thesia care. The incidence however decreased significantly over a
haemorrhage can also cause rapid hypovolaemia and
should be excluded, e.g. by ultrasound if pre-operative
haemodynamic instability. In cases where direct surgical
intervention is unable to control haemorrhage, early
Causes of cardiac arrest. Overall causes of cardiac arrest have been
interventional radiography should be considered.
Loss of the airway is a common cause of perioperative
• Hypovolaemia (e.g. bleeding).
cardiac arrest. Assess the airway carefully before
induction of anaesthesia. Prepare all equipment,
including suction and an operating table or trolley that
can be tipped head-down (Trendelenburg position).
Drug-induced (e.g. muscle relaxants).
Ensure that difficult airway equipment is immediately
◦ Anaesthesia related.
available, and brief the team on a failed intubation drill
Airway loss.
if appropriate. Always use waveform capnography.
Children are particularly prone to loss of the airway
Anaphylaxis (drugs, blood products).
from laryngospasm; ensure an appropriate
neuromuscular blocker is available and give before
The commonest cause of anaesthesia-related cardiac arrest
significant hypoxaemia has occurred in order to break
the laryngospasm.
medication-related events, complications associated with cen-
Undiagnosed tension pneumothorax is a readily
tral venous access, and perioperative myocardial infarction are
treatable cause of cardiac arrest. Although usually
also children, airway obstruction from laryn-
associated with trauma, consider early in the
gospasm, hypovolaemia from blood loss and hyperkalemia from
management of all patients who arrest, particularly
transfusion of stored blood are additional
those with chronic obstructive pulmonary disease and
Cardiac arrest caused by bleeding had the highest mortality in
severe asthma. A sudden increase in airway pressures
non-cardiac surgery, with only 10.3% of these patients surviving to
may indicate a tension pneumothorax or problems with
the breathing tubing, but also consider asthma and
hospital discharge.primary arrest rhythms during perioper-
ative cardiac arrest recorded in the Mayo Clinic series were asystole
Cardiovascular collapse has several causes, but in the
in 41.7%, VF in 35.4%, PEA in 14.4% and unknown in 8.5%. Contrary
context of perioperative cardiac arrest, common causes
to studies of cardiac arrest in general, the rhythm associated with
include hypovolaemia, anaphylaxis, and vagal
the best chance of survival to hospital discharge was asystole (43%
stimulation. Use of transthoracic echocardiography is a
useful tool to exclude cardiac tamponade (if suspected)
and to assess myocardial contractility and
Management of perioperative cardiac arrest. Patients in the operat-
ing room are normally fully monitored and, as such, there should be
The incidence of immune-mediated anaphylaxis
little or no delay in diagnosing cardiac arrest. High-risk patients will
during anaesthesia ranges from 1 in 10,000 to 1 in
often have invasive blood pressure monitoring, which is invaluable
Neuromuscular blocking drugs are the commonest cause, being
in the event of cardiac arrest. If cardiac arrest is a strong possibil-
associated with 60% of cases. The associated morbidity and mor-
ity, apply self-adhesive defibrillation electrodes before induction of
tality are high, particularly if there are delays in the diagnosis and
anaesthesia, ensure adequate venous access and prepare resusci-
management. Initial management of anaphylaxis follows the ABC
tation drugs and fluids. Use fluid warmers and forced air warmers
approach and the management principles outlined in the chapter
to limit perioperative hypothermia and monitor the patient's tem-
on anaphylaxis. Adrenaline is the most effective drug in anaphylaxis
and is given as early as possible. It is appropriate for anaesthetists
In the event of cardiac arrest, follow the ALS algorithm, but
to give adrenaline by the intravenous route. Repeated doses may
with appropriate modifications. Adjust the position and height
be necessary.
of the operating table or trolley to optimise delivery of chest
If cardiac arrest ensues despite correct treatment for the
compressions. CPR is optimal in the supine position, but is pos-
anaphylaxis (see anaphylaxis), continue resuscitation using the
sible in patients who are prone and where immediate turning to
standard ALS algorithm (see adult advanced life
a supine position is not factors for cardiac
Systemic toxicity of local anaesthetics.
Cardiac arrest is a rare but
arrest in prone patients include cardiac abnormalities in patients
well recognised complication of local anaesthetic (LA) overdose,
undergoing major spinal surgery, hypovolaemia, air embolism,
especially following inadvertent intravascular injection. Direct
wound irrigation with hydrogen peroxide, occluded venous
action of the LA on cardiac myocytes causes cardiovascular collapse,
usually within 1–5 min of injection, but onset may range from 30 s
Identification of causes.
In many cases of perioperative car-
to as long as 60 min.hypotension, dysrhythmias, and
diac arrest, physiological deterioration is gradual and the cause
seizures are typical manifestations, but diagnosis may be one of
of the cardiac arrest is known and hence the arrest antici-
pated. In those where this is not the case, follow the standard
IV lipid therapy has been used as a rescue therapy to treat cardio-
ABC algorithm to identify and treat reversible causes. If patients
vascular collapse and cardiac arrest, but its efficacy is
deteriorate, call for senior help immediately. Inform the peri-
In the absence of documented harm, guidelines recommend that
operative team of the deterioration and possible impending
20% lipid emulsion should be available for use wherever patients
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
receive large doses of LA (e.g. operating rooms, labour wards
assistance until ROSC is achieved, but in patients with invasive arte-
and the emergency department).injecting the LA and
rial monitoring, aim for a diastolic blood pressure >25
call for help. Secure and maintain the airway and, if neces-
titrating it to this level (after chest compressions are optimised) by
sary, intubate. Give 100% oxygen and ensure adequate ventilation
administration of a vasopressor, if necessary. This goal is based on
(hyperventilation may help by increasing plasma pH in the
expert consensus derived from experimental and limited clinical
presence of metabolic acidosis). Control seizures using a benzodi-
azepine, thiopental or propofol. Give an initial IV bolus injection
Waveform capnography is a minimum monitoring standard
of 20% lipid emulsion at 1.5 mL kg−1 over 1 min and then start
during anaesthesia and therefore immediately available during a
an infusion at 15 mL kg−1 h−1. If ROSC has not been achieved at
perioperative cardiac arrest. In addition to its use for patients with
5 min, double the rate of lipid infusion and give a maximum of
tracheal intubation where it is particularly valuable to confirm
two additional lipid boluses at 5-min intervals until ROSC has
correct tracheal tube placement, it may also be used in patients
been achieved. Do not exceed a maximum cumulative dose of
with supraglottic airway devices (although an air leak may limit
12 mL kg−1.
quantitative evaluation). An end-tidal carbon dioxide (ETCO2) value
<1.4 kPa/10 mmHg suggests a low cardiac output and rescuers may
Diagnosis of cardiac arrest.
Asystole and ventricular fibrillation
be able to adjust their technique to optimise this variable. An abrupt
(VF) will be detected immediately, but the onset of PEA might not be
sustained increase to a normal value (4.7–5.4 kPa/35–40 mmHg) or
so obvious – loss of the pulse oximeter signal and very low end-tidal
even higher may be an indicator of ROSC. Optimise CPR to achieve
2-values will be good clues and should provoke a pulse check. Do
kPa/20 mmHg, while ventilating the lungs at about
not waste time attempting to obtain a non-invasive blood pressure
10 breaths min−1, with only minimal chest
Team working.
Every resuscitation event should have a des-
Management of cardiac arrest.
The management of a cardiac
ignated team leader who directs and coordinates all staff and
arrest follows the principles of the ALS algorithm. Chest compres-
the components of the resuscitation, with a central focus on
sion in the prone position can be achieved with or without sternal
delivering high-quality CPR. Stop operative surgery unless it
counter-pressure. In one study of prone CPR with sternal counter
is addressing a reversible cause of the cardiac arrest. Patient
pressure (provided by a sandbag) versus standard CPR, higher mean
access and resuscitation tasks may necessitate covering the sur-
arterial pressures were achieved with the prone technique.
gical field and withdrawing the surgical team from the patient.
sider open cardiac compressions in patients where the thorax is
Prioritise team tasks, ensure good quality basic life support
open or the heart can be easily accessed.
(BLS), identify reversible causes and avoid non-priority
In the case of VF, call for a defibrillator.
If the patient is not responding to resuscitative efforts (i.e.
If one is not immediately available, apply a precordial thump. If
kPa/20 mmHg), try to improve the quality of CPR by
that is unsuccessful, give chest compressions and ventilation until
optimising: (1) compression fraction, (2) compression rate, (3)
the defibrillator arrives. Look for reversible causes immediately –
compression depth, (4) leaning, and (5) by avoiding of excessive
hypoxaemia and hypovolaemia will be the most common in this
Stop any surgical activity likely
to be causing excessive vagal activity – if this is the likely cause –
Post-resuscitation care. Depending on the circumstances, patients
give 0.5 mg atropine IV/IO (not 3 mg). Start CPR and immediately
successfully resuscitated after a very brief period of cardiac arrest,
look for other reversible causes. Exclude a completely straight line,
e.g. asystole from excessive vagal stimulation may not require
which suggests an ECG monitoring lead has become detached.
anything more than standard post-operative care. All those resusci-
Pulseless electrical activity.
Start CPR while looking quickly for
tated successfully after longer periods of cardiac arrest will require
reversible causes of PEA. Give fluid unless you are certain that the
admission to an ICU – unless further active treatment is deemed
intravascular volume is adequate. Stop administration of the anaes-
inappropriate. In most circumstances, anything but immediately
thetic. While a vasopressor will be required, in these circumstances
life-saving surgery should be abandoned to enable admission to
1 mg of adrenaline (as directed by the standard ALS guidelines) may
ICU for post-resuscitation care. Patients resuscitated after a pro-
be excessive. Give a smaller dose (e.g. 1 mcg kg−1) of adrenaline,
longed period of cardiac arrest may develop a marked systemic
or another vasopressor initially; if this fails to restore the cardiac
inflammatory response syndrome (SIRS) with the risk of multi-
output, increase the dose while continuing to perform chest com-
ple organ failure. They will require optimisation of mean arterial
pressions and ventilation.
pressure, oxygenation and ventilation. These patients may have
sustained a significant cerebral insult. Some may be suitable for
Monitoring and feedback during CPR.
Unlike OHCAs where mon-
targeted temperature management, but this requires careful con-
itoring if often limited, patients arresting in the perioperative
sideration, given the lack of data on this therapy in the setting of
period can often be monitored with a greater degree of precision.
perioperative cardiac arrest. Active bleeding would certainly be
Monitoring enables assessment of rescuer performance and
a contraindication to induced mild hypothermia but, at the very
patient response:
least, prevent fever in all cases. Avoidance of hyperthermia, from
• Rescuer CPR performance.
overwarming or a post-cardiac arrest important to
optimise neurological recovery.
Feedback sensors (e.g. accelerometers) improve the delivery of
effective chest compressions and enable the rescuer to tailor their
Do not attempt resuscitation decisions. Patients with DNAR deci-
performance accordingly. Their use should be considered whenever
sions presenting for surgery present a dilemma for the anaesthetist.
available. Performance feedback can be obtained from invasive and
The anaesthetic will induce cardiovascular instability, many of the
non-invasive patient monitoring and the rescuer should have direct
routine interventions undertaken could be considered as resusci-
visualisation of monitors displaying these data.
tative, and the chances of surviving a perioperative cardiac arrest
• Patient response.
are better than those from in-hospital cardiac arrest in general.
Consider each case on its individual merits and discuss with the
Monitoring of the patient requires adequate lighting and
patient and/or relatives. Some patients may wish a DNAR decision
patient exposure.Non-invasive blood pressure is unlikely to be of
to remain valid despite the increased risk of a cardiac arrest and the
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
presence of potentially reversible causes; others will request that
failed, and should be performed within 5 min of the cardiac arrest
the DNAR decision is suspended temporarily. Discuss and agree on
by anyone with appropriate training.
the time at which the DNAR decision is reinstated.
These guidelines are also appropriate for patients following
non-sternotomy cardiac surgery, but surgeons performing these
Cardiac arrest following cardiac surgery
operations should have already made clear their instructions for
Introduction. Cardiac arrest following major cardiac surgery is rel-
chest reopening in an arrest.
atively common in the immediate post-operative phase, with a
Special considerations regarding treatment of patients with
reported incidence of is usually preceded by phys-
ventricular assist devices (VADs) are addressed in the section on
iological it can occur suddenly in stable
special patients (see patients with ventricular assist devices).
are usually specific causes of cardiac arrest, such
as tamponade, hypovolaemia, myocardial ischaemia, tension pneu-
Cardiac arrest in a cardiac catheterisation laboratory
mothorax, or pacing failure. These are all potentially reversible and
Cardiac arrest may occur during percutaneous coronary inter-
if treated promptly cardiac arrest after cardiac surgery has a rel-
vention (PCI) for ST-elevation myocardial infarction (STEMI) or
atively high survival rate. Key to the successful resuscitation of
non-STEMI, but it may also be a complication of an angiography
cardiac arrest in these patients is recognition of the need to per-
such as catheter wedging, air or thrombus embolism in the coro-
form emergency resternotomy early, especially in the context of
nary artery, coronary artery intima dissection from the tip of the
tamponade or haemorrhage, where external chest compressions
angiography catheter or caused by pericardial tamponade from a
may be ineffective.
perforated coronary artery during the procedure. Most complica-
tions will result in VF with immediate need for defibrillation. For
Starting CPR. If VF or asystole is diagnosed, immediately admin-
this reason, patients must be continuously monitored and a defi-
ister external defibrillation or emergency temporary pacing at
brillator must be available in the angiography room. Self-adhesive
maximum amplitude. Otherwise start external chest compressions
radiolucent defibrillation pads may already be placed at the begin-
immediately in patients who arrest with monitoring indicating
ning of the procedure in high-risk patients.
no output. Verify the effectiveness of compressions by looking
In this special setting with immediate response to monitored
at the arterial trace, aiming to achieve a systolic blood pressure
VF, defibrillation without preceding chest compressions is recom-
>60 mmHg [Society of Thoracic Surgeons (STS) Clinical Practice
mended. As the patient is early in the electrical phase of a cardiac
guidelines in preparation – personal communication from Joel
arrest, in contrast to the guidelines for unmonitored and OHCAs,
Dunning] and a diastolic blood pressure >25 a rate
the result of defibrillation (VF termination and ROSC) can be deter-
of 100–120 min−1. Inability to obtain this goal with external
mined before chest compressions are started. If needed for failed
chest compressions indicates that cardiac tamponade or extreme
defibrillation or immediately recurring VF, immediate defibrilla-
hypovolaemia is likely and emergency resternotomy should be per-
tion may be repeated up to two times.
If VF persists after the initial three shocks or ROSC not
Consider other reversible causes:
immediately established with certainty, chest compressions and
• Hypoxia – check tracheal tube position, ventilate with 100% oxy-
ventilations must be initiated without further delay and a cause
for the unresolved problem sought with further coronary angiog-
• Tension pneumothorax – check tracheal position, listen for air
raphy. It is of extreme importance that chest compressions are
not interrupted for angiography. On an angiography table with the
• Pacing failure – check pacing box output and pacing wire
image intensifier above the patient, delivering chest compressions
integrity. In asystole, secondary to a loss of cardiac pacing, chest
with adequate depth and rate is almost impossible and exposes
compressions may be delayed momentarily as long as the surgi-
the rescuers to dangerous radiation. Therefore, early transition
cally inserted temporary pacing wires can be connected rapidly
to the use of a mechanical chest compression device is strongly
and pacing re-established (DDD at 100 min−1 at maximum ampli-
recommended.the problem is not rapidly resolved, very
low quality evidence suggests that the use of extracorporeal life
support (ECLS) can be considered as a rescue strategy if the infra-
Defibrillation. There is concern that external chest compressions
structure is available, and probably to be preferred over intra-aortic
can cause sternal disruption or cardiac damage.the post-
balloon pump is no evidence to recommend circu-
cardiac surgery ICU, a witnessed and monitored VF/pVT cardiac
latory support with the Impella pump only during cardiac arrest.
arrest should be treated immediately with up to three quick suc-
If the cardiac arrest is caused by a non-shockable rhythm, imme-
cessive (stacked) defibrillation attempts. Three failed shocks in the
diate transthoracic echocardiography should identify pericardial
post-cardiac surgery setting should trigger the need for emergency
tamponade or other conditions.
resternotomy. Further defibrillation is attempted as indicated in the
universal algorithm and should be performed with internal paddles
Cardiac arrest in a dialysis unit
at 20 J if resternotomy has been performed.
Introduction. Sudden cardiac death is the most common cause of
death in haemodialysis patients and is usually preceded by ventri-
Emergency drugs. Use adrenaline very cautiously and titrate to
cular contributes to 2–5% of deaths
effect (IV doses of up to 100 mcg in adults). Consider amiodarone
amongst haemodialysis accounts for up to 24%
300 mg in patients with refractory shockable rhythms (VF/pVT),
of emergency haemodialysis session in haemodialysis
but do not delay resternotomy. Atropine is not recommended for
The frequency of cardiac arrest is highest on the first session of
asystole and temporary or external pacing should be employed.
haemodialysis of the week (i.e. Monday or Tuesday) as fluid and
electrolyte disturbances peak after the weekend interval.
Emergency resternotomy. This is an integral part of resuscitation
mary prevention of cardiac arrest in dialysis patients include the
after cardiac surgery, once all other reversible causes have been
avoidance of low potassium dialysate solutions and proper use of
excluded. Once adequate airway and ventilation has been estab-
medication, e.g. beta blockers or angiotensin-converting enzyme
lished, and if three attempts at defibrillation have failed in VF/pVT,
inhibitors.is little evidence to guide the treatment of
undertake resternotomy without delay. Emergency resternotomy
cardiac arrest during haemodialysis, although some special con-
is also indicated in asystole or PEA, when other treatments have
siderations have been suggested.
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
Initial steps.
Although life-threatening anaphylaxis is rare, it is a documented
• Call the resuscitation team and seek expert help immediately.
cause of death during dental procedures. In addition to chlorhexi-
• Follow the universal ALS algorithm.
dine mouthwash, other common causes may include penicillin and
• Assign a trained dialysis nurse to operate the dialysis machine.
latex. Anaphylaxis to local anaesthetics is very rare and a reaction
• Stop ultrafiltration (i.e. fluid removal) and give a fluid bolus.
to this class of drug is usually due to a direct intravascular injec-
• Return the patient's blood volume and disconnect from the
tion of adrenaline contained in the solution. True anaphylaxis (all
dialysis machine.
causes) occurs in only 0.004–0.013 cases per dentist per year, com-
• Leave dialysis access open and use for drug administration.
pared with coronary symptoms (angina or myocardial infarction)
• Beware of wet surfaces (i.e. dialysis machines may leak).
occurring in 0.15–0.18 cases per year.
• Minimise delay in delivering defibrillation.
Treatment of cardiac arrest. The following modifications to the ini-
Modifications to cardiopulmonary resuscitation.
tial sequence of actions are recommended if cardiac arrest occurs
A shockable rhythm (VF/pVT) is more common
in a dental chair:
in patients undergoing haemodialysisin the gen-
In case of sudden loss of consciousness, immediately call for help.
eral safest method to deliver a shock during
Look into the victim's mouth. Check and remove all solid materi-
dialysis requires further study. Most haemodialysis machine man-
als from the oral cavity (e.g. retractor, suction tube, tampons, etc.).
ufacturers recommend disconnection from the dialysis equipment
Prevention of airway obstruction should preceed positioning the
prior to defibrillation.familiarity with local dialysis
patient on his back.
equipment and check if equipment has defibrillator-proof label
Recline the dental chair into a fully horizontal position. Cardiac
in accordance with the International Electrotechnical Committee
output can be restored if reduced venous return or vasodila-
(IEC) standards. Automated external defibrillators in nurse-led dial-
tion has caused loss of consciousness, e.g. vasovagal syncope,
ysis centres can facilitate early defibrillation by first responders
orthostatic hypotension. In these patients, raising the legs and/or
with appropriate
placing the patient in a head-down position may also help.
Vascular access.
Use dialysis access in life-threatening situa-
Simultaneously open the airway and check breathing (look, lis-
tions and cardiac
ten, feel). If breathing is not normal or absent, assume a cardiac
Potentially reversible causes.
All of the standard reversible
arrest until proven otherwise. Send someone to get an AED if
causes (4 Hs and 4 Ts) apply to dialysis patients. Electrolyte dis-
orders, particularly hyperkalaemia (see hypo-/hyperkalaemia and
Some case reports describe successful CPR in a patient left on a
other electrolyte disorders), and fluid overload (e.g. pulmonary
dental simulation studies comparing the effec-
oedema) are most common causes.
tiveness of CPR on a dental chair and on the floor reported either
lower or equivalent CPR the patient
Post resuscitation care. Dialysis may be required in the early post
should not be moved from the dental chair because of the risk
resuscitation period guided by fluid status and serum biochemistry.
of injury to the patient and rescuers and the limited space that is
Patient transfer to an area with dialysis facilities (i.e. intensive care
likely to be available on the floor next to the patient.
unit or renal high dependency unit) is essential.
that the dental chair is fully reclined into the horizontal position,
support its head with a stool to increase stability, and start chest
Cardiac arrest in the dental surgery
Introduction. Dental surgery emergencies include a variety of situ-
• If feedback devices are used to monitor CPR quality, those using
ations ranging from psychosomatic disorders precipitated by fear
accelerometers may overestimate depth of compressions if used
and anxiety to life-threatening situations requiring immediate life-
saving procedures. Cardiac arrest in primary dental practice is rare
• Follow the standard compression:ventilation ratios for adults and
with an incidence of 0.002–0.011 cases reported per dentist per
children. Consider the over-the-head technique of CPR if access
to either side of the chest is
The most frequent medical emergencies include vasovagal
• Maintain the airway and ventilate the patient with a bag-
(pre-) syncope, orthostatic hypotension, hypertensive crisis, hyper-
valve-mask device, using the two-hand technique if necessary.
ventilation, seizures, moderate allergic reactions, hypoglycaemia,
Supraglottic airways may be inserted if the operator is skilled in
and angina.majority of dentists responded that they
their use, but tracheal intubation is not a recommended inter-
would be capable of performing initial treatment of common emer-
vention required of dental practitioners and should be avoided.
gencies, while many felt unable to treat anaphylaxis, myocardial
• Switch on the AED and follow the instructions. Deliver the first
infarction, or cardiac
shock as soon as possible if indicated.
A cardiac arrest occurring in a dental surgery is an event wit-
• Continue with CPR until signs of life return, or the patient's han-
nessed by medical professionals who have a duty of care and are
dover to the professional resuscitation team (see adult basic life
required to be competent in the delivery of CPR.
support and automated external
Causes of cardiac arrest. Causes of cardiac arrest usually relate
Equipment and training. Follow national guidelines for recom-
to pre-existing comorbidities or complications of the procedure.
mended equipment to treat medical emergencies in a dental
The life-threatening emergencies commonly arise from myocardial
practice.resuscitation equipment should be available
infarction, grand mal seizures or exacerbation of asthma. Dental
immediately in all primary care dental premises, including suc-
procedures may cause loss of airway patency related to the pri-
tion, self-inflating bag with face masks, oxygen, and emergency
mary pathology or complications of the procedure (e.g. bleeding,
drug kit.role of early defibrillation should be empha-
secretions, tissue swelling). Choking is rare, with a reported inci-
sised to increase the availability of AEDs in dental
dence of 0.07–0.09 cases per dentist per year.addition
which is still unsatisfactory, ranging from a reported 0.5–2.6% in
of sedation is a contributory risk in these cases, although provision
Europe11% in the United States.recommend that
of dental treatment under both local anaesthesia and sedation has
all dental practices delivering clinical care have immediate access
an excellent safety
to an AED, with all staff trained in its use. Advanced equipment
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
and special training is needed if analgesia or sedation is used in
Consider the following modifications to CPR:
dental surgeries.patients with pacemakers, ECG monitor-
Introduce yourself to the cabin crew and state your professional
ing and immediate availability of a defibrillator is recommended
if electrical devices are used (e.g. diathermy, electric pulp tester,
In case of cardiac arrest, performance of CPR is limited in an
aircraft aisle due to space restrictions. Immediately transfer the
There is rightly a public expectation that dental prac-
patient to a suitable location, e.g. galley or exit area. Consider an
titioners and all other dental care professionals should be
over-the-head technique of CPR if access precludes conventional
competent in treating cardiorespiratory arrest. However, only
0.2–0.3% dentists have experience in treating a patient in car-
During CPR, attach oxygen to the facemask or self-inflating bag.
diac their training in CPR varies significantly
Request immediate flight diversion to the nearest appropriate
between knowledge and com-
airport. In other non-critical medical emergencies, coordinate an
petence to deal with medical emergencies must be an important
optimal course of action with the flight crew. Considerations for
part of the training of dentists. All dental care professionals should
flight diversion will depend on the patient's condition and on
undergo annual practical training in the recognition and manage-
the need for immediate treatment in a hospital: e.g. acute coro-
ment of medical emergencies, and the delivery of CPR, including
nary syndrome, stroke, persistently altered mental status; but
basic airway management and the use of an AED.
also technical and operational factors.
• Ask cabin crew whether medical consultation is provided by the
Cardiac arrest in transportation vehicles
airline, e.g. radiotelephony or satellite
• An AED with a monitor can be safely attached to a non-arrested
In-flight emergencies aboard airplanes
patient for monitoring heart rhythm, e.g. syncope, chest pain, or
Introduction. Worldwide, 3.2 billion passengers fly on commercial
airlines annually. The incidence of in-flight medical emergen-
• Concerns about legal responsibility may arise when travelling
cies has been reported to be one event per 10,000–40,000
physicians are asked for help. Based on ethical duties, every
passengers.probability of at least one medical inci-
physician is required to offer help within his or her scope
dent reaches 95% after 24 intercontinental of
of practice, but the legal duty is only applicable for certain
the cases involve middle-aged people.Two large studies
countries. However, the so-called Good Samaritan Act and other
recently reviewed more than 22,000 in-flight emergencies from
regulations, depending on the origin of an aircraft, always pro-
five American and two European airlines. The most common
tect healthcare providers helping on board from possible legal
medical problems were syncope or presyncope (37.4–53.5%), respi-
ratory symptoms (12.1%), gastrointestinal problems (8.9–9.5%),
• Death on board can legally be confirmed only by a physician. If a
and cardiac conditions (4.9–7.7%) with some variations across
dead person is found, or CPR has been terminated (see ethics of
airlines.problems (e.g. deep venous thrombosis,
resuscitation and end-of-life diversion is not
appendicitis, gastrointestinal bleeding) were seen rarely
In-flight incapacitation of the flight crew is very rare, the most
Education and equipment.
common cause being acute myocardial
Flight crew training.
Both pilots and cabin crew must receive
The in-flight medical emergencies have very limited access to
initial and recurrent training on emergency medical event proce-
medical care, but the majority can be managed conservatively with
dures and operation of emergency medical equipment, including
fluids, oxygen and other treatment available from first aid kits on
AEDs and first aid kits, but local operational procedures may also
board. However, a quarter of these patients subsequently require
additional evaluation in a diversion of an
Although civil aviation is regulated by a variety of national and
aircraft is requested in 2.4–7.3% of all incidents, most commonly
international laws, some studies imply that the majority of in-flight
due to chest pain, suspected stroke, and
emergencies stay unreported or are reported inconsistently.
Cardiac arrest on board has an incidence of 1 per 5–10 million
Documentation of in-flight emergencies needs standardisation in
passenger flights. An initial shockable rhythm is present in 25–31%
order to improve cabin crew training and pre-flight assessments of
the in-flight use of an AED can result in
selected groups of passengers.
33–50% survival to hospital contribut-
On-board emergency equipment.
The Federal Aviation Adminis-
ing to a high survival rate include a witnessed event, cabin crew
tration (FAA) requires every US registered commercial aircraft with
trained in BLS and in 73–86% of cases, travelling medical profes-
a maximum payload capacity of more than 7500 pounds and with at
sionals also providing immediate assistance.
least one flight attendant to carry an AED, intravenous drugs, and
approximately 1000 lives are lost per year in International Airlines
advanced emergency equipment,related regulations in
Transport Association (IATA) carriers. Some studies have shown
Europe are less precise.every commercial aircraft registered
that 41–59% of cardiac arrests on board are unwitnessed, occur-
in Europe, there must be a first-aid kit that all cabin crewmembers
ring during sleep. There were no survivors if the initial rhythm was
are trained to use. Aircraft with at least 30 seats must also carry an
asystole or an idioventricular
advanced medical kit, which can be used by competent personnel,
although the contents vary significantly and may be inadequate for
Cardiopulmonary resuscitation on the airplane. In case of cardiac
all but the most basic of most large
arrest, follow the universal algorithm for BLS (see adult basic life
European airlines carry AEDs, some of them only do so for intercon-
support and automated external
tinental flights, but some do not even provide any equipment for
request an AED and a first aid kit from cabin crew. Physicians
and trained medical providers, e.g. nurses or EMS personnel,
Based on the outcome data from survivors of cardiac arrest and
should also ask for advanced medical equipment. According to
in the absence of any alternative treatment for shockable rhythms
competencies and equipment available, provide the patient with
on board, we strongly recommend mandatory AEDs in all commer-
advanced treatment, assuring that there is high quality CPR ongo-
cial European aircraft, including regional and low-cost carriers.
ing, and an AED was deployed appropriately (see adult advanced life
Healthcare professionals should be aware of the on-board
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
conditions in order to provide appropriate emergency treat-
death (SCD) is the most common cause of death of athletes dur-
ment on of supportive information to
ing competition and training. Estimates of the incidence of SCD
travelling physicians should be encouraged, e.g. ‘Doctor on Board'
vary according to the methodology but recently the incidence has
programme introduced by Lufthansa and Austrian Airlines in 2006.
been quoted as 1:11,394 in basketball players, 1:21,293 for swim-
mers and 1:41,695 for cross-county athletes with a wide variation
Cardiac arrest in HEMS and air ambulances
between male and female athletes (incidence expressed as number
Introduction. Air ambulance services operate either a helicopter
of athletes per cardiomyopathy (HCM) and
emergency medical service (HEMS) or fixed-wing air ambulances
arrhythmogenic right ventricular cardiomyopathy (ARVC) are the
that routinely transport critically ill patients directly to specialty
most common causes in under 35 year olds whilst atherosclerotic
centres and perform secondary transfers between hospitals. Car-
coronary artery disease accounts for 80% of sudden cardiac arrests
diac arrest may occur in flight, both in patients being transported
in over 35 year coronary artery abnormalities
from an accident site and also critically ill patients being trans-
have been reported in 12–33% of
ported between hospital.a retrospective analysis of 12,140
Commotio cordis, the disruption of cardiac rhythm by a blow to
aeromedical journies, the incidence of cardiac arrest in flight was
the precordium, has a quoted incidence of striking object
low (1.1%). Fourty-three percent were medical patients and 57%
must strike the chest within the cardiac silhouette within a 20 ms
were patients with traumatic injuries. In the medical cohort, the
window of the upstroke of the overall survival rate
rate of ROSC was 75%.
from commotio cordis is reported to have improved with survival
The extent of treatment available on board of an air ambulance
rates of up to 58% reported in recent years.
varies and depends on medical and technical factors, e.g. crew com-
Whatever the cause the sudden collapse of an athlete there
petences and configuration, cabin size and equipment. Ideally, all
should be an immediate response from the officials or medical
interventions should be performed before flight so that the need
team. The standard resuscitation procedures must be followed but
for unplanned treatment during flight is avoided.
with certain additional considerations as described below.
Pre-flight preparation. When preparing transport of a critically ill
Access. The medical team should gain immediate access to the field
patient, ensure that all necessary monitoring is attached and func-
of play. It is important that the medical team do observe access
tioning. Check that IV access is secured and easily accessible and
rules to the field of play but it would be hoped that the field of play
that all necessary drugs and medical equipment are available dur-
officials will recognise or be alerted to the collapsed athlete and
ing flight.
halt play so that it is safe to approach the competitor.
Where there is no medical team, during informal competition
Diagnosis. In monitored patients, asystole and shockable rhythms
or in practice it is the responsibility of the referee, the coach or of
(VF/pVT) can be immediately identified, but recognition of PEA may
the athletes' colleagues to recognise the collapse and to initiate a
be challenging, especially under sedation or general anaesthesia.
call for help and resuscitation.
Unexpected loss of consciousness (in alert patients), change of ECG
pattern, and loss of the pulse oximeter signal should provoke a
Calling for help. The call for help is essential to providing the col-
pulse and patient check. A sudden decrease in ETCO2 values in
lapsed athlete with the best chance of survival. It is essential that
those being ventilated or loss of a waveform in those breathing
sports officials, coaches and sports organisers have a plan for med-
spontaneously with ETCO2 monitoring are also indicators of cardiac
ical collapse or trauma. In its simplest form this could include
ensuring the availability of a mobile telephone and knowledge of
the site/address of the sport arena (field of play, club house) to
Treatment. Cardiac arrest in the air ambulance services should be
provide best access for the ambulance. It would be hoped that more
treated according to the universal ALS algorithm. Start chest com-
officials and coaches will be trained in BLS and AED usage.
pressions and ventilation immediately after confirmation of cardiac
arrest, attach monitoring (if not already), and follow universal ALS
Resuscitation. If the athlete is unresponsive and not breathing nor-
a shockable rhythm (VF/pVT) is recognised in a
mally, commence BLS. If available attach an AED and follow the
monitored patient and defibrillation can be accomplished rapidly,
instructions; if this is SCD then the rhythm will probably be ventri-
immediately give up to three-stacked shocks before starting chest
cular fibrillation and will respond to defibrillation.
compressions. In a US study, 33% of patients achieving ROSC fol-
The sports field of play is often an open arena and in major com-
lowing defibrillation did not require any chest compressions.
petition may be on view to many thousands of spectators and a
In smaller helicopters, there may be insufficient room to per-
television audience. Although treatment must not be compromised
form effective resuscitation and an emergency landing may be
moving the collapsed athlete to a quieter and more private site
necessary to allow better patient access.
for continued treatment may be considered. Where there is not an
Mechanical chest compression devices enable delivery of high
immediate response to treatment and there is an organised medi-
quality chest compressions in the confined space of an air ambu-
cal team, this move could be accomplished after three defibrillation
lance and their use should be a cardiac arrest
attempts on the rationale of providing the highest efficacy of defi-
during flight is thought to be a possibility, consider fitting the
brillation in the first three shocks. The move, if decided, should be
patient within a mechanical chest compression device during pack-
agreed and may need to be accomplished in stages to allow for near
continuous chest compressions. Where there is no medical team or
a defibrillator is not immediately available then BLS must continue
Cardiac arrest during sports activities
until advanced care arrives.
If the athlete responds to resuscitation then they must be
Resuscitation on the field of play
transported immediately to the nearest cardiac centre for further
Introduction. The sudden and unexpected collapse, not associ-
evaluation and treatment. As there is a possibility of the rhythm
ated with contact or trauma, of an athlete on the field of play
reverting this transportation must be under the supervision of a
is probably cardiac in origin and requires rapid recognition and
healthcare professional who is equipped and capable of adminis-
effective treatment if the victim is to survive. Sudden cardiac
tering resuscitation and further defibrillation.
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
Prevention. In an effort to predict and prevent SCD, the Inter-
national Olympic Committee Medical Commission (IOC Medical
Detailed summaries of the pathophysiology of drowning have
Commission 2014) and many International Sport Federations have
been published.brief, following submersion, the
recommended cardiac screening for athletes. However, there is
victim initially breath holds by reflex. During this time the victim
much debate about the effectiveness of the techniques being used
frequently swallows water. As breath holding continues, hypoxia
and the population that should be screened.
and hypercapnia develop. A reflex laryngospasm may temporarily
prevent the entrance of water into the lungs. Eventually these
Water rescue and drowning
reflexes abate and the victim aspirates water. The key feature to
note in the pathophysiology of drowning is that bradycardia as a
consequence of hypoxia occurs before sustaining a cardiac arrest.
Drowning is a common cause of accidental
Correction of hypoxaemia by ventilation-only resuscitation is crit-
and effective actions by bystanders, trained rescuers and emer-
ical and in itself may lead to return of spontaneous ventilation or
gency medical personnel can make the difference between life and
circulation (ROSC) in some cases, probably because the presence of
guidelines provide advice about the initial res-
a circulation had not been
cue and resuscitation of victims involved in drowning incidents.
They are intended for healthcare professionals and certain groups
Drowning chain of survival
of lay responders that have a special responsibility in the care of
The Drowning Chain of Survival describes five critical links for
the drowning victim, e.g. lifeguards, lifeboat crews, swimming pool
improving survival from drowning (first two links
instructors and water rescue teams.
cover prevention of drowning and recognition of distress.
This chapter provides guidance on removal from water, initial and
post resuscitation care.
The World Health Organization (WHO) reports that every hour
of every day, more than 40 people lose their lives to drowning;
372,000 deaths each year.WHO acknowledges that the true
Bystander response. Bystanders play a critical role in initial
number of drownings worldwide is much higher. More than 90% of
attempts at rescue and the same
these deaths occur in low and middle-income countries. The inci-
time, bystanders who attempt a rescue have died during the res-
dence of drowning varies between countries, with eastern Europe
cue attempt, mostly when drowning occurs in surf or fast moving
having the highest rates in risk groups vary
possible, bystanders should attempt to save
between countries, in general males are much more likely to drown
the drowning victim without entry into the water. Talking to the
than females. Most accidental drownings are children who are
victim, reaching with a rescue aid (e.g. stick or clothing), or throw-
unable to swim. In countries where aquatic leisure in combination
ing a rope or buoyant rescue aid may be effective if the victim is
with alcohol and drug use is common, young adults are a second
close to dry land. If entry into the water is essential, take a buoyant
group of countries also report a slight increase of
rescue aid, flotation device or boat.is safer to enter the water
drowning in the age groups above 70 years related to accidents and
with two rescuers than alone. Never dive head first in the water
physical activities close to water. Drowning is commonest in inland
when attempting a rescue. You may lose visual contact with the
waters (e.g. lakes, rivers) and during summer
victim and run the risk of a spinal injury.
Definitions, classifications and reporting
Trained rescuer response. Trained rescuers are often professionals
The International Liaison Committee on Resuscitation (ILCOR)
who work in teams with specialist equipment to assist with search
defines drowning as a process resulting in primary respiratory
and rescue. Where the rescue takes time, the teams often seek guid-
impairment from submersion/immersion in a liquid medium.
ance on the likelihood of survival. For this reason, ILCOR reviewed
Implicit in this definition is that a liquid/air interface is present
specific prognostic indicators and noted that submersion dura-
at the entrance of the victim's airway, preventing the victim from
tions of less than 10 min were associated with a very high chance
breathing air. The victim may live or die after this process, but
of favourable outcome; submersion durations longer than 25 min
whatever the outcome, he or she has been involved in a drown-
were associated with a low chance of favourable
ing occurs when the face is underwater
Age, emergency medical services (EMS) response time, fresh or
or covered in water. Asphyxia and cardiac arrest occurs within a
salt water, water temperature, and witness status were not useful
matter of minutes of submersion. Immersion, by contrast, is when
for predicting survival. Submersion in ice-cold water may prolong
the head remains above water, in most cases by means of the sup-
the window of survival and justify extended search and rescue
port of a lifejacket. In most situations of immersion, the victim
remains immersed with an open airway and becomes hypother-
mic, although aspiration of water may occur if water splashes over
In-water resuscitation. Trained individuals may undertake in
the face or if the victim becomes unconscious with their face in
water ventilation ideally with the support of a buoyant rescue
the water. The difference between submersion and immersion is
a rescuer, in general a surf-lifeguard, finds a non-
important in understanding the difference in epidemiology, patho-
responding drowning victim in deep open water, the rescuer may
physiology, clinical course and prognostic parameters between the
start ventilation when trained to do so before moving the victim
two drowning processes.
to dry land or rescue craft. Some victims may respond to this. If
If the casualty is rescued, the process of drowning is interrupted,
not responding, and depending on the local situation, such as sea
which is termed a non-fatal drowning. If the person dies at any time
conditions, distance to shore, availability of rescue boat or res-
as a result of drowning, the term is fatal drowning. Avoid terms
cue helicopter, the rescuer should then decide to bring the victim
such as dry and wet drowning, active and passive drowning, silent
to shore as quickly as possible without further ventilation while
drowning, secondary drowning and improve
rescue-swimming with the victim or continue on the spot with in-
consistency in information between studies use the Utstein-style
water ventilation until support by crews of a rescue boat or rescue
registration template for drowning when reporting outcomes from
helicopter arrives to take over the resuscitation. One study suggests
that the second option has a higher survival
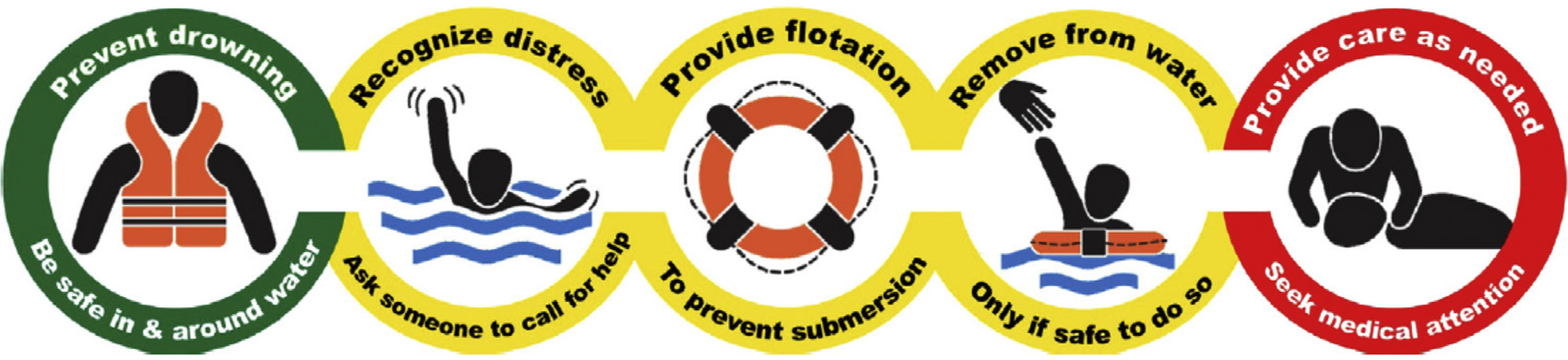
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
Fig. 4.5. Drowning chain of
Reproduced with permission from Elsevier Ireland Ltd.
Removal from water. Remove the victim from the water promptly.
rise. However it often takes more time to insuflate air than under
The chances of a drowning victim sustaining a spinal injury are
normal conditions due to reduced compliance and high airway
very precautions are unnecessary unless there is a
resistance. The higher inflation pressure may precipitate inflation
history of diving in shallow water, or signs of severe injury after
of the stomach with regurgitation and also reduce cardiac output.
water-slide use, waterskiing, kite-surfing, or watercraft racing. If
Expert opinion suggests that cricoid pressure applied by trained
the victim is pulseless and apnoeic, remove them from the water
and skilled personnel in casualties without a secured airway may
as quickly as possible while attempting to limit neck flexion and
reduce gastric inflation and enhance ventilation in drowning.
extension. Hypovolaemia after prolonged immersion may cause
a circum-rescue collapse/arrest. Keep the victim in a horizontal
Chest compressions. If the victim has not responded to initial venti-
position during and after retrieval from the water.
lations, they should be placed on a firm surface before starting chest
compressions, as compressions are ineffective in the
Initial resuscitation once retrieved from water
Provide CPR in a ratio of 30 compressions to 2 ventilations. Most
Follow the standard BLS sequence, initially by checking for
drowning victims will have sustained cardiac arrest secondary to
response, opening the airway and checking for signs of life. The
hypoxia. In these patients, compression-only CPR is likely to be
drowning victim rescued from the water within a few minutes of
ineffective and should be avoided.
submersion is likely to exhibit abnormal (agonal) breathing. Do not
If sufficient rescuers are present, the person performing the
confuse this with normal breathing.
aquatic rescue should be relieved of continuing CPR once on land
as they are likely to be fatigued, which may impair the quality of
Rescue breaths/ventilations. The BLS sequence in drowning
reflects the critical importance of rapid alleviation of hypoxia.
Inflation should take about 1 s and be sufficient to see the chest
Automated external defibrillation. Defer using an AED until after CPR
has commenced. Dry the victim's chest, attach the AED pads and
turn the AED on. Deliver shocks according to the AED prompts.
not breathing normally?
Fluid in the airway. In some situations, massive amounts of foam
caused by admixing moving air with water are seen coming out of
the mouth of the victim. Do not try and attempt to remove the foam
as it will keep coming. Continue rescue breaths/ventilation until an
ALS provider arrives and is able to intubate the victim. Regurgita-
and call eme
tion of stomach contents and swallowed water is common during
resuscitation from drowning.this prevents ventilation com-
pletely, turn the victim on their side and remove the regurgitated
material using directed suction if possible.
Modifications to advanced life support
Airway and breathing. During the initial assessment of the spon-
taneously breathing drowning victim, give high-flow oxygen
oxygen if possible
(10–15 L min−1), ideally through an oxygen mask with reservoir
victims who fail to respond to these initial meas-
ures, who have a reduced level of consciousness or are in cardiac
Signs of li
arrest, consider early tracheal intubation and controlled ventilation
by skilled personnel. Reduced pulmonary compliance requiring
high inflation pressures may limit the use of a supraglottic air-
way device.care to ensure optimal preoxygenation before
rt CPR 30:2
attempting tracheal intubation. Pulmonary oedema fluid may pour
from the airway and may need continuous suctioning to enable a
view of the larynx. After the position of the tracheal tube is con-
firmed, titrate the inspired oxygen concentration to achieve a SpO2
Attach AED and
of 94–98%.oximetry can give spurious readings following
follow inst
ructions
rescue from adequate oxygenation and ven-
tilation with arterial blood gases once available. Set positive end
Fig. 4.6. Drowning treatment algorithm for rescuers with a duty to respond.
expiratory pressure (PEEP) to at least 5–10 cm H2O. However, PEEP
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
levels of 15–20 cm H2O may be required if the patient is severely
Wilderness and environmental emergencies
the stomach with a gastric tube.
Difficult terrain and remote areas
Geographical and meteorological considerations. Compared to urban
Circulation and defibrillation. Palpation of the pulse as the sole indi-
areas some terrains will be more difficult to access and are remote
cator of the presence or absence of cardiac arrest is not always
from organised medical care. Exposed and steep terrain may ren-
reliable. As soon as possible, use information from monitoring
der extrication dangerous and challenging. The chances of a good
modalities such as the ECG trace, ETCO
2 and echocardiography to
outcome from cardiac arrest may be reduced because of delayed
confirm the diagnosis of cardiac arrest.
access and prolonged transport. Furthermore, some environments
If the victim is in cardiac arrest, follow standard ALS pro-
are harsher than urban areas (e.g. cold, windy, wet, very bright due
tocols. If the victim is hypothermic, modify the approach in
to light-reflection on ice and snow). Human and material resources
accordance with the guidance for treatment of hypothermia (see
may be greatly restricted.
Compared with the partial pressure of oxygen at sea level (PO
After prolonged immersion, most victims will have become
about 21 kPa/159 mmHg), the PO
high (>1500 m above sea
hypovolaemic due to the cessation of the hydrostatic pressure of
level), very high (3500–5500 m) and extreme altitude (>5500 m)
water on the body. Give rapid IV fluid to correct hypovolaemia. This
will be progressively lower, constraining the physical activity of
should commence out-of-hospital if transfer time is prolonged.
rescuers. There is a physiological limit to acclimatisation (e.g.
short term–hyperventilation and increased cardiac output; long-
Discontinuing resuscitation efforts
term–haemoglobin increase). The highest permanent settlement is
Making a decision to discontinue resuscitation efforts on a
11 kPa/84 mmHg). Above 7500 m the risk of
victim of drowning is notoriously difficult. No single factor can
lethal acute altitude illness is very high.
accurately predict good or poor survival with certainty. Frequently,
There are no epidemiological data on the causes of cardiac arrest
decisions made in the field later prove to have been
at high altitude. However, it is conceivable that primary cardiac
Continue resuscitation unless there is clear evidence that such
arrest is the major (60–70%) cause of sudden cardiac arrest. Thus,
attempts are futile (e.g. massive traumatic injuries, rigour mortis,
public access defibrillator (PAD) programmes in populated areas
putrefaction, etc.), or timely evacuation to a medical facility is not
at altitude seem reasonable. For instance, public access defibrilla-
possible. Neurologically intact survival has been reported in several
tors (PADs) should be placed in popular ski areas, busy mountain
victims submerged for longer than 25 min, however these rare case
huts and restaurants, at mass-participation events, and in remote
reports almost invariably occur in children submerged in ice-cold
but often-visited locations that are not medically covered.
water, when immersion hypothermia has preceeded hypoxia or in
areas where physicians are regularly involved in mountain res-
submersion of car occupants.retrospective study of
cue operations, the provided on-site treatment is more in line with
160 children who drowned in the Netherlands found that outcomes
were extremely poor if ALS took longer than 30 min to achieve ROSC
even if hypothermia was present.
Decision making. Continuous monitoring and treatment may be dif-
ficult during transport because the patient will be insulated from
Post resuscitation care
the harsh environment within a rescue bag, being well wrapped
Salt versus fresh water. Small differences in electrolyte disturbance
and secured on a stretcher. During transport, CPR may be limited
are rarely of any clinical relevance and do not usually require
in quality and nearly impossible in some circumstances (e.g. while
carrying the patient, during abseiling or winching). In danger-
ous and difficult terrain where continuous CPR is impossible,
Lung injury. The predominant pathophysiological process in the
delayed and intermittent CPR has been proposed for hypothermic
lungs is driven by surfactant wash-out and dysfunction, alveolar
resuscitation devices may help to improve
collapse, atelectasis, and intrapulmonary shunting. The severity of
CPR quality during difficult extrication and prolonged
lung injury varies from a mild self-limiting illness to refractory
hypoxaemia. Many victims of drowning are at risk of develop-
ing acute respiratory distress syndrome there
Effective and safe immobilisation and splinting will reduce mor-
are no randomised controlled trials undertaken specifically in this
bidity and mortality.possible, transport the patient
population of patients, it seems reasonable to include strategies
with air rescue.organisation of the helicopter emergency
such as protective ventilation that have been shown to improve
medical service (HEMS) affects the outcome.
survival in patients with membrane
oxygenation (ECMO) has been used for those in refractory car-
diac arrest, those with refactory hypoxaemia and in selected cases
High altitude illness
of submersion in ice cold water, although success rates remain
Given the increasing popularity of travel at altitude, an
low.is common after drowning. Prophylactic
increasing number of tourists at altitude have cardiovascular
antibiotics have not been shown to be of benefitthey may be
and metabolic risk factors for cardiac arrest. The pO2 falls with
considered after submersion in grossly contaminated water such
increasing altitude and this oxygen deficiency may lead to acute
as sewage. Give broad-spectrum antibiotics if signs of infection
manifestations of mountain sickness.
Persons travelling to an altitude of >3500 m are at risk of devel-
Neurological outcome. Neurological outcome, notably severe per-
• acute mountain sickness (AMS) with headache, nausea, fatigue
manent neurological damage, is primarily determined by the
duration of hypoxia. Attempts have been made to improve neuro-
• high altitude pulmonary oedema (HAPO) with severe dyspneoa
logical outcome following drowning with the use of barbiturates,
intracranial pressure (ICP) monitoring, and steroids. None of these
• high altitude cerebral oedema (HACO) with gate disorder, disori-
interventions has altered outcome.
entation and confusion.
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
Risk factors include a fast rate of ascent and a previous history
• buried > 60 min (or if the initial core temperature is <30 ◦C) and
of mountain sickness. If not treated promptly, HAPO and HACO
in cardiac arrest with an obstructed airway on extrication;
may progress rapidly to loss of consciousness, severe respiratory
• buried and in cardiac arrest on extrication with an initial serum
distress, circulatory instability and cardiac arrest. The most impor-
potassium > 8 mmol L−1.
tant actions are immediate descent or transport to lower levels of
altitude, administration of oxygen (2–6 L min−1, target > 90% SpO
Full resuscitative measures, including extracorporeal rewarm-
treatment in a portable hyperbaric chamber, in cases of HACO
ing, are indicated for all other avalanche victims without evidence
administration of dexamethasone 4–8 mg every 8 h, and in cases
of an unsurvivable injury.
of HAPO, nifedipine 30 mg every 12 h.
Avalanches occur in areas that are difficult to access by rescuers
Resuscitation at high altitude does not differ from standard CPR.
in a timely manner, and burials frequently involve multiple vic-
With the lower pO
tims. The decision to initiate full resuscitative measures should be
2, CPR is more exhausting for the rescuer than at
sea level, and the average number of effective chest compressions
determined by the number of victims and the resources available,
may decrease within the first mechanical chest
and should be informed by the likelihood of adher-
compression devices whenever possible.
ence to present guidelines is poor,use of a standardised
Commonly, no physician will be present to give guidance to
nurses or paramedics on when to stop CPR. Guidelines have there-
fore been proposed for these situations.
Management of completely buried avalanche victims. The algorithm
for the management of buried avalanche victims is shown in
CPR may be withheld or terminated in a patient with absent vital
In all cases, extricate the body gently and use spinal precautions.
• the risk is unacceptable to the rescuer
• Consider withholding resuscitation at the scene if it increases risk
• the rescuer is exhausted
to the rescue team or if the victim is lethally injured or completely
• extreme environments prevent CPR
• any of the following apply:
• Determine the duration of burial. If unknown, core temperature
may substitute for decision-making.
◦ truncal transection
• If the duration of burial is ≤60 min (or initial core tempera-
◦ whole body incinerated
ture is ≥30 ◦C) and cardiac arrest is confirmed, follow standard
ALS guidelines (see adult advanced life CPR,
measure core temperature, monitor ECG, give oxygen and apply
◦ avalanche victim in asystole with obstructed airway and burial
insulation and heat packs to the trunk. Give drugs and fluids only
time > 60 min (see avalanche burial below).
if IV or IO access can be established within a few minutes. Resus-
citation may be terminated in a normothermic asystolic patient
CPR may be also terminated when all of the following criteria
if ALS is not successful after 20 min, in an absence of reversible
cause (see ethics of resuscitation and end-of-life decisions).
• unwitnessed loss of vital signs;
• Transport survivors with concern of respiratory (e.g. pulmonary
• no ROSC during 20 min of CPR;
oedema) or other-system critical illness or injury to the most
• no shock advised at any time by AED or only asystole on ECG;
appropriate medical centre. Provide specific trauma care as indi-
• no hypothermia or other reversible causes warranting extended
cated. The admitting hospital must be capable of advanced active
external or core internal rewarming.
• If the duration of burial is > 60 min (or initial core temperature
In situations where transport is not possible, and correc-
is < 30 ◦C) and cardiac arrest is confirmed, start CPR and attach
tion of reversible causes is not possible, further resuscitation is
monitor. If there is any electrical activity or a patent airway in
futile and CPR should be terminated. These recommendations
an asystolic patient, continue CPR. Defibrillation beyond three
should be interpreted in the context of local conditions and
attempts may be delayed until core temperature ≥30 ◦C.
• Transport all patients who present with cardiovascular instability
(i.e. ventricular arrhythmias, systolic blood pressure < 90 mmHg)
or core temperature < 28 ◦C to an ECLS rewarming centre. Follow
Introduction. In Europe and North America together, there are
regional hypothermia protocols if needed.
about 150 snow avalanche deaths each year. Most are sports-
• If direct transport to an ECLS rewarming centre is not possible in a
related and involve skiers, snowboarders and snowmobilers.
timely manner, e.g. by HEMS, check potassium level at the nearest
Fatalities are mainly due to asphyxia, sometimes associated with
hospital. If potassium exceeds > 8 mmol L−1, consider terminating
trauma and hypothermia. Prognostic factors are severity of injury,
resuscitation (after excluding crush injuries and considering if
duration of complete burial, airway patency, core temperature and
depolarizing muscle relaxants were used).
serum potassium.buried avalanche victims die from
asphyxia within 35 min if the airway is obstructed. The average
Lightning strike and electrical injuries
cooling rate is 3 ◦C h−1from 0.6 ◦C h−1 to 9 ◦C h−1
Introduction. Electrical injury is a relatively infrequent but poten-
moderate to severe hypothermia may become important after
tially devastating multisystem injury with high morbidity and
60 min of burial if the airway is patent. The highest recorded potas-
mortality, causing 0.54 deaths per 100,000 people each year. Most
sium in an avalanche victim who was successfully resuscitated is
electrical injuries occur indoors. In adults, electrical injuries are
6.4 mmol L−1survival rate of avalanche victims pre-
common in the workplace and are generally associated with high
senting with cardiac arrest ranges from 7% to 17%.
voltage, whereas children are at risk primarily at home, where the
patterns differ across countries due to terrain, climate and prehos-
voltage is lower (220 V in Europe, Australia and Asia; 110 V in the
United States and from lightning strikes
is rare, but worldwide it causes 1000 deaths each year.
Decision-making on scene. Avalanche victims are not likely to sur-
Electric shock injuries are caused by the direct effects of current
vive when they are:
on cell membranes and on vascular smooth muscle. The thermal
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
Fig. 4.7. Avalanche accident algorithm. Management of completely buried victims. (ECLS, extracorporeal life support).
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
energy associated with high-voltage electrocution will also cause
wise to move to a safer environment, particularly if lightning has
burns. Factors influencing the severity of electrical injury include
been seen within 30
whether the current is alternating (AC) or direct (DC), voltage, mag-
nitude of energy delivered, resistance to current flow, pathway of
Resuscitation. Patients struck by lightning are most likely to die if
current through the patient, and the area and duration of contact.
they sustain immediate cardiac or respiratory arrest and are not
Skin resistance is decreased by moisture, which increases the likeli-
treated rapidly. When multiple victims are struck simultaneously
hood of injury. Electric current follows the path of least resistance;
by lightning, rescuers should give highest priority to patients in
conductive neurovascular bundles within limbs are particularly
respiratory or cardiac arrest. Victims with respiratory arrest may
prone to damage. Contact with AC may cause tetanic contraction
require only ventilation to avoid secondary hypoxic cardiac arrest.
of skeletal muscle, which may prevent release from the source of
Resuscitative attempts may have higher success rates in lightning
electricity. Myocardial or respiratory failure may cause immediate
victims than in patients with cardiac arrest from other causes, and
efforts may be effective even when the interval before the resuscita-
• Respiratory arrest may be caused by paralysis of the central respi-
tive attempt is or non-reactive pupils should
ratory control system or the respiratory muscles.
never be used as a prognostic sign, particularly in patients suffering
• Current may precipitate ventricular fibrillation (VF) if it tra-
verses the myocardium during the vulnerable period (analogous
Start standard BLS and ALS without delay:
to an R-on-T current may also cause
• Airway management may be difficult if there are electrical burns
myocardial ischaemia because of coronary artery spasm. Asystole
around the face and neck. Early tracheal intubation is needed in
may be primary, or secondary to asphyxia following respiratory
these cases, as extensive soft-tissue oedema may develop caus-
ing airway obstruction. Head and spine trauma can occur after
electrocution. Immobilise the spine until evaluation can be per-
Current that traverses the myocardium is more likely to be fatal.
A transthoracic (hand-to-hand) pathway is more likely to be fatal
• Muscular paralysis, especially after high voltage, may persist
than a vertical (hand-to-foot) or straddle (foot-to-foot) pathway.
for several ventilatory support is required during this
There may be extensive tissue destruction along the current path-
• VF is the commonest initial arrhythmia after high-voltage AC
Associated injuries are common. Blast (hyperbaric) injuries,
shock; treat with prompt attempted defibrillation. Asystole is
injuries from being thrown from the point of contact and tetanic
more common after DC shock; use standard protocols for this
contraction causing limb fractures have all been reported.
and other arrhythmias.
• Remove smouldering clothing and shoes to prevent further ther-
Lightning strike. Lightning strikes deliver as much as 300 kV over a
few milliseconds. Most of the current from a lightning strike passes
Vigorous fluid therapy is required if there is significant tis-
over the surface of the body in a process called ‘external flashover'.
sue destruction. Maintain a good urine output to enhance the
Both industrial shocks and lightning strikes cause deep burns at
excretion of myoglobin, potassium and other products of tissue
the point of contact. For industrial shocks the points of contact are
usually on the upper limbs, hands and wrists, whereas for lightning
Consider early surgical intervention in patients with severe ther-
they are mostly on the head, neck and shoulders. Injury may also
mal injuries.
occur indirectly through ground current or current splashing from a
Maintain spinal immobilisation if there is a likelihood of head or
tree or other object that is hit by lightning.force may
neck trauma.
cause blunt trauma.pattern and severity of injury from a
Conduct a thorough secondary survey to exclude traumatic
lightning strike varies considerably, even among affected individ-
injuries caused by tetanic muscular contraction or by the person
uals from a single with industrial and domestic
electric shock, death is caused by cardiacrespiratory
Electrocution can cause severe, deep soft-tissue injury with rel-
those who survive the initial shock, extensive cate-
atively minor skin wounds, because current tends to follow
cholamine release or autonomic stimulation may occur, causing
neurovascular bundles; look carefully for features of compart-
hypertension, tachycardia, non-specific ECG changes (including
ment syndrome, which will necessitate fasciotomy.
prolongation of the QT interval and transient T-wave inversion),
Although rare, consider abdominal visceral injuries caused
and myocardial necrosis. Creatine kinase may be released from
directly by electrical damage.
myocardial and skeletal muscle. Lightning can also cause central
and peripheral nerve damage; brain haemorrhage and oedema,
There are conflicting reports on the vulnerability of the fetus
and peripheral nerve injury are common. Mortality from lightning
to electric shock. The clinical spectrum of electrical injury ranges
injuries is as high as 30%, with up to 70% of survivors sustaining
from a transient unpleasant sensation for the mother with no effect
on her fetus, to placental abruption, fetal burn or intrauterine fetal
death either immediately or a few days later. Several factors, such
Diagnosis. The circumstances surrounding the incident are not
as the magnitude of the current and the duration of contact, are
always known. Unique pattern of skin lesions called feathering or
thought to affect outcome.
Lichtenberg figure is a pathognomonic symptom that is seen only
in patients struck by patients with lin-
Further treatment and prognosis. Immediate resuscitation of young
ear or punctuate burns (feathering) should be treated as victims of
victims in cardiac arrest from electrocution can result in long-term
survival. Successful resuscitation has been reported after prolonged
life support.
Safety measures. Ensure that any power source is switched off and
All those who survive electrical injury should be monitored in
do not approach the casualty until it is safe. High-voltage (above
hospital if they have a history of cardiorespiratory problems or have
domestic mains) electricity can arc and conduct through the ground
for up to a few metres around the casualty. It is safe to approach
• loss of consciousness
and handle casualties after lightning strike, although it would be
• cardiac arrest
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
• electrocardiographic abnormalities
breathing is triaged as dead. If an unresponsive victim is breath-
• soft tissue damage and burns.
ing normally, turn them into the recovery position and label as
immediate (highest priority) for treatment. Further assessment
Severe burns (thermal or electrical), myocardial necrosis, the
of casualties, e.g. respiratory rate, capillary refill time, etc., and
extent of central nervous system injury, and secondary mul-
depends on individual triage protocols.
tisystem organ failure determine the morbidity and long-term
• The decision to use an MCI triage sieve, and withhold CPR to those
prognosis. Bone marrow embolism has also been reported in some
with imminent death (including victims without signs of life), is
cases.is no specific therapy for electrical injury, and the
the responsibility of a medical commander who is usually the
management is supportive. Prevention remains the best way to
most experienced EMS clinician on scene.
minimise the prevalence and severity of electrical injury.
• Triage inaccuracy may have fatal consequences in patients with
survivable injuries. Healthcare professionals must be regularly
Mass casualty incidents
trained to use the triage protocols during simulations and live
technologies such as educational video
games enhance learning and improve subsequent performance
Mass casualty incidents (MCIs), characterised by greater
when compared to traditional educational methods, e.g. card-
demand for medical care than available resources, are rare events.
sort allows fast and correct recognition of
Among the 19.8 million yearly emergency medical services (EMS)
those requesting life-saving procedures, and reduces the risk of
activations in the United States, 0.3% had an MCI code, but incidence
inappropriate care given to futile cases.
of real disasters is much International Federation of
• Consider assigning a higher triage risk level to the elderly and to
Red Cross and Red Crescent Societies (IFRC) reports about 90 disas-
survivors of high-energy trauma in order to reduce preventable
ters in Europe and 650 events worldwide MCI or
deaths. After an aeroplane crash in the Netherlands, 9% of the
disaster can be caused by variety of chemical, biological, radiologi-
minor injuries (lowest priority), and 17% of all walking casual-
cal or nuclear (CBRN) incidents, but traumatic incidents (e.g. traffic
ties were undertriaged while suffering serious injuries.the
accidents, acts of crime, or natural and industrial disasters) play a
National Trauma Database (NTDB), patients in all triage levels
leading role in developed countries.triage of casualties
were compared to mortality outcomes. There were 322,162 sub-
enables identification of patient care priorities. Unlike normal cir-
jects assigned to the lowest priority triage level of which 2046
cumstances, CPR is not usually initiated in MCI, in order to avoid
died before hospital discharge. Age was the primary predictor of
delaying potentially effective treatment for salvageable victims.
This critical decision depends on available resources in relation to
• Perform life-saving interventions in patients triaged as imme-
the number of casualties.
diate (highest priority) to prevent cardiac arrest: control major
haemorrhage, open airway using basic techniques, perform chest
Triage and decision-making on scene
decompression for tension pneumothorax, use antidotes, and
consider initial rescue breaths in a non-breathing child.
In children, use of a special triage tape or a paediatric-specific
Safety at scene is paramount. Those first on scene must identify
MCI triage system (e.g. JumpSTART, Team Life Support, Inc.,
the actual and potential hazards and appropriate assistance must
FL, USA, ) or a universal SALT
be requested immediately. The presence of multiple unconscious
it is not available, use any triage system for
victims should always alert rescuers to the possibility of a CBRN
incident. Unexpected danger may be present at crime scenes,
or places polluted by noxious substances e.g. carbon monoxide,
industrial cyanides or other chemicals. During sarin attacks in
C – SPECIAL PATIENTS
Japan, 10% of 1363 EMS technicians developed poisoning, mostly
from primary victims in poorly ventilated ambulances.
Cardiac arrest associated with concomitant diseases
• Use adequate protection measures and consider potential risks
before approaching casualties. Be aware that wearing some
personnel protective equipment may adversely affect perfor-
Introduction. Worldwide, approximately 300 million people of all
mance of treatment interventions and limit the care that can
ages and ethnic backgrounds have asthma.worldwide
be given in contaminated zones. Simulation studies have shown
prevalence of asthma symptoms ranges from 1 to 18% of the popu-
reduced success rate of advanced airway techniques, prolonged
lation with a high prevalence in some European countries (United
time for securing IV and IO access, and difficulties with drug
Kingdom, Scandinavia and Netherlands) and in
recent years, the prevalence of asthma and its related morbidity and
mortality appears to have plateaued and may even have decreased
in some countries, especially in children and adolescents.
The World Health Organization (WHO) has estimated that 15 mil-
Use a triage system to prioritise treatment, e.g. START (Simple
lion disability-adjusted life years (DALYs) are lost annually from
Triage and Rapid Transport), Newport Beach Fire Depart-
asthma, representing 1% of the global disease burden. Annual
ment, CA, USA,(Sort-Assess-Lifesaving Interventions-
worldwide deaths from asthma have been estimated at 250,000.
Treat/Transport).prehospital teams involved in
The death rate does not appear to be correlated with asthma
the initial scene triage must avoid overtriage. Repeated triage
and international guidance for the man-
(re-triage) is needed on entering the hospital and responsible per-
agement of severe asthma already guidance focuses
sonnel at all stages of emergency care must be familiar with the
on the treatment of patients with near-fatal asthma and subsequent
triage system used.
cardiac arrest.
If the START triage sieve is used, everyone able to walk is directed
to clear the scene, and respiratory status of non-walking patients
is assessed. If the casualty does not breathe, open the airway using
Patients at risk of asthma-related cardiac arrest. The risk of near-
basic manoeuvers (head tilt and chin lift, or jaw thrust). Look, lis-
fatal asthma attacks is not necessarily related to asthma
ten and feel for no more than 10 s. A patient who does not begin
Patients most at risk include those with:
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
• a history of near-fatal asthma requiring intubation and mechan-
Table 4.3
The severity of asthma (PEF, peak expiratory flow)
• hospitalisation or emergency care for asthma in the past
• low or no use of inhaled corticosteroids;
• increasing use and dependence of beta-2 agonists;
• anxiety, depressive disorders and/or poor compliance with
• food allergy in a patient with
A national confidential enquiry carried out in the UK in 2014
showed that the majority of asthma-related deaths occurred before
admission to hospital.with younger adults, older
adults have higher rates of near-fatal asthma-related events and
higher comorbidity-adjusted risk of
Causes of cardiac arrest. Cardiac arrest in a person with asthma is
often a terminal event after a period of hypoxaemia; occasionally,
it may be sudden. Cardiac arrest in those with asthma has been
• severe bronchospasm and mucous plugging leading to asphyxia
(this condition causes the vast majority of asthma-related
• cardiac arrhythmias caused by hypoxia, which is the commonest
cause of asthma-related arrhythmia.can also be
caused by stimulant drugs (e.g. beta-adrenergic agonists, amino-
phylline) or electrolyte abnormalities;
• dynamic hyperinflation, i.e. auto positive end-expiratory pres-
therapy for acute asthma in most of the world. Repeated doses
sure (auto-PEEP), can occur in mechanically ventilated asthmat-
every 15–20 min are often needed. Severe asthma may necessi-
ics. Auto-PEEP is caused by air trapping and ‘breath stacking' (air
tate continuous nebulised salbutamol. Nebuliser units that can be
entering the lungs and being unable to escape). Gradual build-up
driven by high-flow oxygen (at least 6 L min−1) should be available.
of pressure occurs and reduces venous return and blood pressure;
The hypoventilation associated with severe or near-fatal asthma
• tension pneumothorax (often bilateral).
may prevent effective delivery of nebulised drugs. If a nebuliser
is not immediately available, beta-2 agonists can be temporarily
Diagnosis. Wheezing is a common physical finding, but severity
administered by repeating activations of a metered dose inhaler
does not correlate with the degree of airway obstruction. The
via a large volume spacer device.adrenaline does
absence of wheezing may indicate critical airway obstruction,
not provide additional benefit over and above nebulised beta-2
whereas increased wheezing may indicate a positive response to
agonists in acute asthma.
bronchodilator therapy. SpO2 may not reflect progressive alve-
Nebulised anticholinergics (iprat-
olar hypoventilation, particularly if oxygen is being given. SpO2
ropium, 0.5 mg 4–6 hourly) may produce additional bronchodi-
may initially decrease during therapy because beta-agonists cause
lation in severe asthma or in those who do not respond to
both bronchodilation and vasodilation, initially increasing intra-
pulmonary shunting.
Nebulised magnesium sulphate.
Although limited evidence sug-
Other causes of wheezing include: pulmonary oedema,
gests that magnesium sulphate has some bronchodilator
chronic obstructive pulmonary disease (COPD), pneumonia,
a review of 16 randomised or pseudo-randomised controlled tri-
foreign bodies, pulmonary embolism,
als in adults and children with acute asthma showed that inhaled
magnesium alone or in combination with inhaled beta(2)-agonists
The severity of an asthma attack is defined in
(with or without inhaled ipratropium) was not associated with
significant benefit in terms of improved pulmonary function or
Prevention of cardiac arrest. A patient with severe asthma requires
reduced hospital of small studies in adults
immediate and aggressive medical management to prevent dete-
with severe exacerbations of asthma showed improvements in
rioration. Base the assessment and treatment on a systematic
pulmonary function with additional inhaled magnesium, however
ABCDE approach. Patients with SpO2 < 92% or with features of
evidence was too limited to come to a definite conclusion. Inhaled
life-threatening asthma are at risk of hypercapnia and require
magnesium sulphate is currently not recommended for the treat-
arterial blood gas measurement. Experienced clinicians should
ment of acute asthma.
treat these high-risk patients in a critical-care area. The specific
Intravenous magnesium sulphate.
Studies of IV magnesium sul-
drugs and the treatment sequence will vary according to local
phate in acute severe and life-threatening asthma have produced
conflicting systematic review assessing 14 stud-
Use a concentration of inspired oxygen that will
ies (three of which were multicentre trials) including a total of
achieve an SpO2 94–98%.oxygen by mask is some-
2313 adult or mostly adult patients treated for acute asthma in
times necessary. Lack of pulse oximetry should not prevent the use
the emergency department showed that a single infusion of 1.2 or
2 g IV MgSO4 over 15–30 min significantly reduced hospital admis-
Nebulised beta-2 agonists.
Inhaled beta-2 agonists are first line
sions compared with placebo (odds ratio [OR] 0.75, 95% confidence
drugs in patients with an acute asthma attack and should be admin-
interval [CI] 0.60–0.92) and improved lung
istered as early as possible. Intravenous beta-2 agonists should
in almost all of the studies had already been given at least oxy-
be reserved for those patients in who inhaled therapy cannot be
gen, nebulised short-acting beta-2-agonists and IV corticosteroids
used reliably. Salbutamol, 5 mg nebulised, is the cornerstone of
in the emergency department. No difference was observed for other
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
outcomes such as intensive care admissions and length of hospital
adrenaline 0.5 mg IM according to the anaphylaxis guidelines may
be appropriate (see anaphylaxis).
Give a single dose of IV magnesium sulphate to patients
Referral to intensive care.
An intensive care specialist should
with acute severe asthma (PEF < 50% best or predicted) who
assess patients that fail to respond to initial treatment, or develop
have not had a good initial response to inhaled bronchodila-
signs of life-threatening asthma. Intensive care admission after
tor therapy. The most commonly reported adverse effects of IV
asthma-related cardiac arrest is associated with significantly
magnesium sulphate are flushing, fatigue, nausea, headache and
poorer outcomes compared with those in who a cardiac arrest does
Early use of systemic corticoste-
Consider rapid sequence induction and tracheal intubation if,
roids for acute asthma in the emergency department significantly
despite efforts to optimise drug therapy, the patient has:
reduces hospital admission rates, especially for those patients not
receiving concomitant corticosteroid therapy.there
• a decreasing conscious level, or coma;
is no difference in clinical effects between oral and IV formu-
• persisting or worsening hypoxaemia;
lations of IV route is preferable because
• deteriorating respiratory acidosis, despite intensive therapy;
patients with near-fatal asthma may vomit or be unable to
• severe agitation, confusion and fighting against the oxygen mask
(clinical signs of hypoxaemia);
There is a lack of definitive evi-
• progressive exhaustion;
dence for or against the use of IV bronchodilators in this setting.
• respiratory or cardiac arrest.
Trials have primarily included spontaneously breathing patients
with moderate- to life-threatening exacerbations of asthma; evi-
Elevation of the PCO2 alone does not indicate the need for tra-
dence in ventilated patients with life-threatening asthma or cardiac
cheal the patient, not the numbers. All patients
arrest is sparse. The use of IV bronchodilators should generally
transferred to intensive care units should be accompanied by a
be restricted to patients unresponsive to nebulised therapy or
doctor suitably equipped and skilled to intubate.
where nebulised/inhaled therapy is not possible (e.g. a patient
receiving bag-mask ventilation). A Cochrane review of intravenous
decreases the intubation rate and mortality in however,
beta-2 agonists compared with nebulised beta-2 agonists found no
its role in patients with severe acute asthma is uncertain. There is
evidence of benefit and some evidence of increased side effects
insufficient evidence to recommend its routine use in asthma.
compared with inhaled treatment.may be given
as either a slow IV injection (250 mcg IV slowly) or continuous
Treatment of cardiac arrest.
infusion of 3–20 mcg min−1.
Basic life support.
Give BLS according to standard guidelines.
A Cochrane review of intravenous amino-
Ventilation will be difficult because of increased airway resistance;
phylline found no evidence of benefit and a higher incidence of
try to avoid gastric inflation.
adverse effects (tachycardia, vomiting) compared with standard
Advanced life support.
Modifications to standard ALS guide-
care Whether aminophylline has a place as an
lines include considering the need for early tracheal intubation.
additional therapy after treatment with established medica-
The peak airway pressures recorded during ventilation of patients
tions such as inhaled beta-agonists and systemic corticosteroids
with severe asthma (mean 67.8 ± 11.1 cmH2O in 12 patients) are
remains uncertain. If, after obtaining senior advice, the deci-
significantly higher than the normal lower oesophageal sphincter
sion is taken to administer IV aminophylline, give a loading
pressure (approximately 20 cmH2is a significant risk of
dose of 5 mg kg−1 over 20–30 min (unless on maintenance ther-
gastric inflation and hypoventilation of the lungs when attempting
apy), followed by an infusion of 500–700 mcg kg−1 h−1. Maintain
to ventilate a severe asthmatic without a tracheal tube. During car-
serum theophylline concentrations below 20 mcg mL−1 to avoid
diac arrest this risk is even higher, because the lower oesophageal
sphincter pressure is substantially less than
Leukotriene receptor antagonists.
There are few data on the use
Respiratory rates of 8–10 breaths per minute and a tidal vol-
of intravenous leukotriene receptor evi-
ume required for a normal chest rise during CPR should minimise
dence suggests improvement of lung function and a non-significant
dynamic hyperinflation of the lungs (air trapping). Tidal volume
trend towards reduced hospital admission when the intravenous
depends on inspiratory time and inspiratory flow. Lung emptying
leukotriene receptor antagonist montelukast was used as a res-
depends on expiratory time and expiratory flow. In mechani-
cue therapy in adults with acute studies are
cally ventilated severe asthmatics, increasing the expiratory time
required to confirm the usefulness of leukotriene receptor antago-
(achieved by reducing the respiratory rate) provides only moderate
nists in this setting.
gains in terms of reduced gas trapping when a minute volume of
Intravenous fluids and electrolytes.
Severe or near-fatal asthma
less than 10 L min−1 is
is associated with dehydration and hypovolaemia, and this will
Some case reports have reported ROSC in patients with air trapp-
further compromise the circulation in patients with dynamic
ing when the tracheal tube was disconnected.dynamic
hyperinflation of the lungs. If there is evidence of hypovolaemia or
hyperinflation of the lungs is suspected during CPR, compression of
dehydration, give IV crystalloids. Beta-2 agonists and steroids may
the chest while disconnecting tracheal tube may relieve air trapp-
induce hypokalaemia, which should be monitored and corrected
ing. Although this procedure is supported by limited evidence, it is
with electrolyte supplements as required.
unlikely to be harmful in an otherwise desperate situation.
Heliox is a mixture of helium and oxygen (usually 80:20
Dynamic hyperinflation increases transthoracic
or 70:30). A meta-analysis of four clinical trials did not support
but modern impedance-compensated biphasic defibrillation wave-
the use of heliox in the initial treatment of patients with acute
forms are no less effective in patients with a higher impedance.
As with standard ALS defibrillation protocols, consider increasing
Sometimes it may be difficult to dis-
defibrillation energy if the first shock is unsuccessful and a manual
tinguish severe life-threatening asthma from anaphylaxis. Treat
defibrillator is available.
patients presenting with severe ‘asthma-like' symptoms, but with-
There is no good evidence for the use of open-chest cardiac
out pre-existing pulmonary disease (asthma, COPD), as if the
compressions in patients with asthma-associated cardiac arrest.
cause was anaphylaxis. In these circumstances, administration of
Working through the four Hs and four Ts will identify potentially
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
reversible causes of asthma-related cardiac arrest. Tension pneu-
resternotomy or extracorporeal membrane oxygenation (ECMO) is
mothorax can be difficult to diagnose in cardiac arrest; it may
a reasonable option.
be indicated by unilateral expansion of the chest wall, shifting of
the trachea and subcutaneous emphysema. Pleural ultrasound in
Cardiac arrest associated with neurological disease
skilled hands is faster and more sensitive than chest X-ray for the
Causes of cardiac arrest. Cardiac arrest associated with acute neu-
detection of a pneumothorax is suspected,
rological disease is relatively uncommon and can occur with
perform needle decompression using a large gauge cannula and
subarachnoid haemorrhage, intracerebral haemorrhage, epileptic
being careful to avoid direct puncture of the lung. Any attempt at
seizures, and ischaemic addition brain injury associ-
needle decompression should be followed by insertion of a chest
ated with trauma can cause cardiac arrest.
tube. Always consider bilateral pneumothoraces in asthma-related
Cardiac arrest associated with neurological disease can be due
cardiac arrest (see tension pneumothorax).
ECLS can ensure both organ perfusion and gas exchange in cases
Loss of consciousness, causing airway obstruction, hypoxaemia
of otherwise refractory respiratory and circulatory failure. Cases
and respiratory arrest followed by cardiac arrest. Loss of con-
of successful treatment of asthma-related cardiac arrest in adults
sciousness is also associated with an increased risk of aspiration
using ECLS have been reportedhowever, the role of ECLS
of gastric contents into the lungs.
in cardiac arrest caused by asthma has never been investigated in
Respiratory and cardiac depression caused by compression of the
controlled studies. The use of ECLS requires appropriate skills and
equipment that may not be available in all hospitals.
Arrhythmias and myocardial dysfunction associated with acute
neurological injury and in particular sub-arachnoid haemorr-
Patients with ventricular assist devices
Introduction. All clinicians caring for patients with ventricular
Sudden unexpected death in epilepsy (SUDEP) effects about 1 in
assist devices (VADs) should have received full training in the pro-
every 1000 people with epilepsy.
cedures for equipment failure and the cardiac arrest situation. The
management of patients with VADs is more complex, in that a car-
Neurological symptoms. Patients can have prodromal signs suggest-
diac arrest may be due to mechanical failure and in this situation
ing a neurological cause before cardiac arrest such as headache,
there may be actions specific to the device that are required. The
seizures, impaired consciousness, and focal these are
use of external chest compression in patients with ventricular assist
often non-specific and can include syncope, shortness of breath and
devices has been reviewed.are isolated case reports of
chest pain. Cardiac or respiratory arrest occurs in between 3 and
successful external chest compression without damage to the VAD.
11% of patents with subarachnoid haemorrhage,the initial
External chest compression may be particularly useful to decom-
rhythm is usually non-shockable.
press a non-functional right ventricle in cardiac arrests and often
the right ventricle may be the cause of the loss of output.
Treatment. Preventive measures for cardiac or respiratory arrest
should be aimed at treating the underlying cause. Once cardiac
Diagnosis of cardiac arrest. Confirming cardiac arrest in these
arrest occurs, follow standard BLS and ALS guidelines. If ROSC is
patients may be difficult. A patient with invasive monitoring should
achieved, address the underlying cause in addition to standard post
be considered to have arrested if the arterial line reads the same
resuscitation care.
as the central venous pressure (CVP) line. In patients without
Patients with subarachnoid haemorrhage may have ECG
invasive monitoring, if the patient has no signs of life and is
changes that suggest an acute coronary
not breathing, then they should be considered to have suffered a
features such as a young age, female gender, non-shockable ini-
cardiac arrest. Transthoracic/transoesophageal echocardiography
tial rhythm and neurological antecedents (e.g. headache, seizures,
(TTE/TOE), capnography or Doppler flow readings in a major artery
neurological deficits) are common but non-specific for neurolog-
may assist in the diagnosis of whether there is meaningful per-
ical cause.with neurological prodromal symptoms
fusion. These devices also display pump flow and this should be
who achieve ROSC may be considered for CT brain scan. Whether
used to assist in a diagnosis of whether there has been a genuine
this is done before or after coronary angiography will depend on
loss of blood flow, or whether there is just a low flow situation with
clinical judgement regarding the likelihood of a subarachnoid hae-
reduced conscious level.
morrhage versus acute coronary syndrome.
Management of cardiac arrest. Patients with an implantable left
Outcome. Survival depends on the underlying cause and tradi-
ventricular assist devices (LVAD) such as a HeartMate (Thoratec,
tional factors (e.g. witnessed, bystander CPR) associated with
Pleasanton, CA, USA) or HeartWare (HeartWare, Framingham, MA,
is poor in those with ROSC after a subarach-
USA) device should have the same algorithm followed as the
noid who achieve ROSC after a
algorithm for arrest after cardiac surgery (see cardiac arrest fol-
primary neurological cause of cardiac arrest will often fulfil neu-
lowing cardiac surgery). Check the rhythm; perform defibrillation
rological criteria for death and should be considered as potential
for shockable rhythms (VF/pVT), start pacing for asystole. In pulse-
organ donors.
less electrical activity (PEA), turn the pacing off and verify there is
no underlying VF, which must be treated by defibrillation. External
chest compressions should be performed if immediate resuscitative
efforts fail. Importantly, the airway and breathing checks should
Introduction. Worldwide obesity has more than doubled since
always be performed.
1980. In 2014, more than 1.9 billion (39%) adults were overweight,
It is possible for a patient to have asystole or VF, but still have
and of these over 600 million (13%) were obese.
adequate cerebral blood flow due to adequate and continued pump
The World Health Organization (WHO) uses body mass index
flow. If the patient is conscious and responding then you will have
(BMI; weight in kg divided by height in m2) to define obesity in
more time in which to resolve this arrhythmia and external chest
compressions will not be needed.
• overweight (25.0–29.9 kg m−2);
Resternotomy should be performed in an established car-
• obese (30.0–34.9 kg m−2);
diac arrest within 10 days of surgery and after this time, either
• very obese (≥35.0 kg m−2).
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
Many clinical studies have linked BMI to outcomes for a wide
operations may cause secondary transportation trauma, or even
variety of cardiovascular and non-cardiovascular
prohibit safe transfer of obese patient to the
Traditional cardiovascular risk factors (hypertension, diabetes, lipid
profile, prevalent coronary heart disease, heart failure, and left
Outcome. The relation between obesity and outcome from cardiac
ventricular hypertrophy) are common in obese patient. Obesity is
arrest is unclear. One large registry study has shown that survival
associated with increased risk of sudden cardiac
from cardiac arrests caused by shockable rhythms (VF/pVT) was
causes of death are dilated cardiomyopathy and severe coronary
highest in overweight patients but was significantly lower in those
who were very contrast, survival to discharge of non-
shockable rhythms was similar across all BMI groups. Evidence
Modifications to cardiopulmonary resuscitation. No changes to
from clinical cohort studies has suggested that overweight and
sequence of actions are recommended in resuscitation of obese
obese patients may actually have a more favourable short-term and
patients, but delivery of effective CPR may be challenging. Physical
long-term prognosis than leaner patients once they are successfully
and physiological factors related to obesity may adversely affect
resuscitated from cardiac arrest.
the delivery of CPR, including patient access and transportation,
patient assessment, difficult IV access, airway management, qual-
Cardiac arrest associated with pregnancy
ity of chest compressions, the efficacy of vasoactive drugs, and the
efficacy of defibrillation because none of these measures are stan-
dardised to a patient's BMI or weight.rescuers than usual
Mortality related to pregnancy is relatively rare in Europe (esti-
may be required to assist in moving the patient and rescuer fatigue,
mate 16 per 100,000 live births) although there is a large variation
particularly in relation to the delivery of chest compressions, may
between fetus must always be considered when
necessitate more regular changes of the rescuer than normal.
an adverse cardiovascular event occurs in a pregnant woman. Fetal
Chest compressions.
As with all cardiac arrests, chest compres-
survival usually depends on maternal survival and initial resusci-
sions are most effective when performed with the patient lying on
tation efforts should focus on the pregnant mother. Resuscitation
a firm surface, but it may be unsafe for the patient and rescuers to
guidelines for pregnancy are based largely on case series, extrapola-
attempt to move the patient down onto the floor. However, it is not
tion from non-pregnant arrests, manikin studies and expert opinion
always necessary in obese patients because the heavier torso sinks
based on the physiology of pregnancy and changes that occur in
into the mattress, leaving less potential for mattress displacement
during chest compression.
Significant physiological changes occur during pregnancy, e.g.
In order to maintain sufficient depth of chest compresisons
cardiac output, blood volume, minute ventilation and oxygen con-
(approximately 5 cm but no more than 6 cm), rescuer fatigue may
sumption all increase. Furthermore, the gravid uterus can cause
necessitate the need to change rescuers more frequently than the
significant compression of iliac and abdominal vessels when the
standard 2 min interval. Use of mechanical resuscitation devices is
mother is in the supine position, resulting in reduced cardiac output
limited by the slope of the anterior chest wall, thoracic dimensions
and hypotension.
(sternum height up to 303 mm, and maximal width of 449 mm for
piston devices (LUCAS); chest circumference up to 130 cm and max-
imal chest width of 380 mm for devices with a load-distributing
Causes of cardiac arrest
band), and patient weight (up to 136 kg) (AutoPulse).
In developed regions, haemorrhage, embolism (thromboem-
Optimal defibrillation energy levels in obese
bolic and amniotic fluid), hypertensive disorders of pregnancy,
patients are unknown. Unlike monophasic defibrillators, mod-
abortion and genital tract sepsis account for most deaths directly
ern biphasic defibrillators are impedance-compensated and adjust
associated with pregnancy, and pre-existing medical conditions for
their output according to the patient's impedance. Two small ret-
those indirectly related to pregnancy.review of over 2 million
rospective studies have demonstrated no apparent weight-based
pregnancies in the UK showed that maternal deaths (death dur-
influence on defibrillation a biphasic waveform of
ing pregnancy, childbirth, or within 42 days after delivery) were
150 J achieving high shock success rates without need for energy
associated with cardiac disease, neurological conditions, psychi-
protocols for obese patients should
atric conditions, and malignancies.quarter of pregnant women
therefore follow those recommended for patients with a normal
who died in the UK had sepsis, and 1 in 11 had influenza. Pregnant
BMI. Consider higher shock energies for defibrillation if initial defi-
women can also sustain cardiac arrest from the same causes as
brillation attempts fail.
women of the same age group.
Higher inspiration pressure is needed for positive
pressure ventilation due to increased intraabdominal
Prevention of cardiac arrest in pregnancy
Early tracheal intubation by an experienced provider removes the
In an emergency, use a systematic ABCDE approach. Many car-
need for prolonged bag-valve-mask ventilation, and may reduce
diovascular problems associated with pregnancy are caused by
any risk of aspiration. In all patients with extreme obesity, difficult
intubation must be anticipated, with a clear failed intubation drill if
Treat a pregnant patient as follows:
necessary.intubation fails, use of a supraglottic airway device
• Place the patient in the left lateral position or manually and gently
(SAD) with oesophaegeal drainage tube is a suitable option.
displace the uterus to the left.
• Give oxygen, guided by pulse oximetry to correct any hypox-
Logistical considerations. A patient's BMI should be considered
when organising prehospital resuscitation, especially with regard
• Give a fluid bolus if there is hypotension or evidence of hypo-
to technical support and number of ambulance crew
Special response vehicles modified to carry extremely obese
• Immediately re-evaluate the need for any drugs being given.
patients, equipped with extra-wide interiors, reinforced stretch-
• Seek expert help early. Obstetric and neonatal specialists should
ers and specialised lifting gear, should be used if possible. Weight
be involved early in the resuscitation.
limits of both stretchers and hospital beds must be checked prior
• Identify and treat the underlying cause, e.g. rapid recognition and
to use.of the technical aspects of rescue
treatment of sepsis, including early intravenous antibiotics.
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
Modifications to basic life support
third trimester of pregnancy are narrower compared with their post
From 20 weeks' gestation, the uterus can compress both the
partum state and to non-pregnant intubation
inferior vena cava (IVC) and aorta, impeding venous return and
may be more difficult in the pregnant patient.help, a
cardiac output. Uterine obstruction of venous return can cause pre-
failed intubation drill and the use of alternative airway devices may
arrest hypotension or shock and, in the critically ill patient, may
precipitate cardiac cardiac arrest, the compro-
mise in venous return and cardiac output by the gravid uterus limits
Intravascular access. Early intravenous or intraosseous access will
the effectiveness of chest compressions.
enable drug and fluid administration. Aiming for access above the
Non-arrest studies show that left lateral tilt improves mater-
diaphragm may address any theoretical concerns associated with
nal blood pressure, cardiac output and stroke volume
delayed circulation caused by IVC compression if drugs are infused
improves fetal oxygenation and heart rate.cardiac
through sites below the IVC.
arrest data show that the gravid uterus can be shifted away from
the IVC in most cases, by placing the patient in 15◦ of left lateral
Reversible causes
decubitus position.value of relieving aortic or IVC compres-
Rescuers should attempt to identify common and reversible
sion during CPR is, however, unknown. Unless the pregnant victim
causes of cardiac arrest in pregnancy during resuscitation (see spe-
is on a tilting operating table, left lateral tilt is not easy to perform
cial causes). The 4 Hs and 4 Ts approach helps identify all the
whilst maintaining high-quality chest compressions. A variety of
common causes of cardiac arrest in pregnancy. Pregnant patients
methods to achieve a left lateral tilt have been described including
are also at risk of all the other causes of cardiac arrest for their age
placing the victim on the rescuers or blankets,
group (e.g. anaphylaxis, drug overdose, trauma).
or the Cardiff wedgetheir efficacy in actual cardiac
Consider the use of abdominal ultrasound by a skilled opera-
arrests is unknown. Even when a tilting table is used, the angle
tor to detect possible causes during cardiac arrest; however, do
of tilt is often a manikin study, the ability to
not delay other treatments and minimise interruptions to chest
provide effective chest compressions decreased as the angle of left
lateral tilt increased and at an angle of greater than 30◦ the manikin
Specific causes of cardiac arrest in pregnancy include the fol-
The key steps for BLS in a pregnant patient are:
Haemorrhage. Life-threatening haemorrhage can occur both ante-
Call for expert help early (including an obstetrician and a neona-
natally and Postpartum haemorrhage is the
commonest single cause of maternal death worldwide and is esti-
Start BLS according to standard guidelines.
mated to cause one maternal death every 7 min.
Ensure high-quality chest compressions with minimal interrup-
include ectopic pregnancy, placental abruption, placenta praevia,
placenta accreta, and uterine rupture.massive haemorrhage
The hand position for chest compressions may need to be slightly
protocol must be used in all units and should be updated in conjunc-
higher on the sternum for patients with advanced pregnancy e.g.
tion with the blood bank. Women at high risk of bleeding should be
third trimester.
delivered in centres with facilities for blood transfusion, intensive
Manually displace the uterus to the left to reduce IVC compres-
care and other interventions, and plans should be made in advance
for their management. Treatment is based on an ABCDE approach.
Add left lateral tilt if this is feasible and ensure the chest remains
The key step is to stop the bleeding.
supported on a firm surface (e.g. in the operating room) – the
Consider the following
optimal angle of tilt is unknown. Aim for between 15 and 30◦.
• Fluid resuscitation, including use of rapid transfusion system and
Even a small amount of tilt may be better than no tilt. The angle
of tilt used needs to enable high-quality chest compressions and
• Oxytocin and prostaglandin analogues to correct uterine
if needed, allow Caesarean delivery of the fetus.
Start preparing for emergency Caesarean section (see below) –
• Massaging the uterus.
the fetus will need to be delivered if initial resuscitation efforts
• Correction of coagulopathy including use of tranexamic acid
and/or recombinant activated factor
• Uterine balloon tamponade or packing.
Modifications to advanced life support
• Uterine compression
Defibrillation. For cardiac arrest with a shockable rhythm (VF/pVT)
• Angiography and endovascular embolisation.
attempt defibrillation as soon as possible. There is no change
in transthoracic impedance during pregnancy, suggesting that
• Aortic cross-clamping in catastrophic haemorrhage.
standard shock energies for defibrillation attempts should be used
in pregnant is no evidence that shocks from a
Cardiovascular disease. Myocardial infarction and aneurysm or
direct current defibrillator have adverse effects on the fetal heart.
dissection of the aorta or its branches, and peripartum cardiomy-
opathy cause most deaths from acquired cardiac disease.
Airway management. During pregnancy, there is a greater potential
Patients with known cardiac disease need to be managed in a
for gastro-oesophageal sphincter insufficiency and risk of pul-
specialist unit. Pregnant women may develop an acute coronary
monary aspiration of gastric contents.pregnant
syndrome, typically in association with risk factors such as obesity,
patients are at risk of aspiration, oxygenation and ventilation is
older age, higher parity, smoking, diabetes, pre-existing hyperten-
the priority over aspiration prevention. Early tracheal intubation
sion and a family history of ischaemic heart
will however make ventilation of the lungs easier in the presence
patients can have atypical features such as epigastric pain and
of increased intra-abdominal pressure.
vomiting. Percutaneous coronary intervention (PCI) is the reper-
A tracheal tube 0.5–1 mm internal diameter (ID) smaller than
fusion strategy of choice for ST-elevation myocardial infarction
that used for a non-pregnant woman of similar size may be nec-
in pregnancy. Thrombolysis should be considered if urgent PCI is
essary because of maternal airway narrowing from oedema and
unavailable. A review of 200 cases of thrombolysis for massive
swelling.study documented that the upper airways in the
pulmonary embolism in pregnancy reported a maternal death rate
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
of 1% and concluded that thrombolytic therapy is reasonably safe
of the twelve women had ROSC after delivery, with two maternal
and five newborn survivors. Maternal case fatality rate was 83%.
Increasing numbers of women with congenital heart disease are
Neonatal case fatality rate was
becoming pregnant.failure and arrhythmias are the com-
Delivery will relieve IVC compression and may improve chances
monest problems, especially in those with cyanotic heart disease.
of maternal resuscitation. The Caesarean delivery also enables
Pregnant women with known congenital heart disease should be
access to the infant so that newborn resuscitation can begin.
managed in specialist centres.
Decision-making for emergency hysterotomy (Caesarean section).
Pre-eclampsia and eclampsia. Eclampsia is defined as the devel-
The gravid uterus reaches a size that will begin to compro-
opment of convulsions and/or unexplained coma during preg-
mise aorto-caval blood flow at approximately 20 weeks gestation;
nancy or postpartum in patients with signs and symptoms of
however, fetal viability begins at approximately 24–25
sulphate is effective in preven-
Portable ultrasound is available in some emergency departments
ting approximately half of the cases of eclampsia developing
and may aid in determination of gestational age (in experienced
in labour or immediately postpartum in women with pre-
hands) and positioning, provided its use does not delay the decision
eclampsia.Use magnesium sulphate infusion for the
to perform emergency
treatment of eclampsia.
At gestational age less than 20 weeks, urgent Caesarean delivery
need not be considered, because a gravid uterus of this size is
Pulmonary embolism. The estimated incidence of pulmonary
unlikely to significantly compromise maternal cardiac output.
embolism is 1–1.5 per 10,000 pregnancies, with a case fatality of
At gestational age approximately 20–23 weeks, initiate emer-
3.5% (95% CI factors include obesity, increased
gency hysterotomy to enable successful resuscitation of the
age, and immobility. Successful use of fibrinolytics for massive,
mother, not survival of the delivered infant, which is unlikely at
life-threatening pulmonary embolism in pregnant women has been
this gestational age.
• At gestational age approximately ≥24–25 weeks, initiate emer-
gency hysterotomy to save the life of both the mother and the
Amniotic fluid embolism. Amniotic fluid embolism (AFE) usually
presents around the time of delivery with sudden cardiovascu-
lar collapse, breathlessness, cyanosis, arrhythmias, hypotension
Post resuscitation care
and haemorrhage associated with disseminated intravascular
Post resuscitation care should follow standard guidelines. Tar-
coagulopathy.Patients may have warning signs preceding
geted temperature management (TTM) has been used safely and
collapse including breathlessness, chest pain, feeling cold, light-
effectively in early pregnancy with fetal heart monitoring and
headedness, distress, panic, a feeling of pins and needles in the
resulted in favourable maternal and fetal outcome after a term
fingers, nausea, and vomiting. The UK Obstetric Surveillance System
cardioverter defibrillators (ICDs) have
(UKOSS) identified 120 cases of AFE between 2005 and 2014 with
been used in patients during pregnancy.
a total and fatal incidence estimated as 1.7 and 0.3 per 100,000,
respectively, and association with older maternal age, multiple
Preparation for cardiac arrest in pregnancy
pregnancy, placenta praevia and induction of labour, instrumental
ALS in pregnancy requires coordination of maternal resuscita-
vaginal and Caesarean
tion, Caesarean delivery of the fetus and newborn resuscitation
Treatment is supportive, as there is no specific therapy based on
ideally within 5 min.
an ABCDE approach and correction of coagulopathy. Successful use
To achieve this, units likely to deal with cardiac arrest in preg-
of extracorporeal life support techniques for women suffering life-
threatening amniotic fluid embolism during labour and delivery is
have plans and equipment in place for resuscitation of both the
pregnant woman and newborn
Peri-mortem delivery of the fetus
ensure early involvement of obstetric, anaesthetic and neonatal
Consider the need for an emergency hysterotomy or Cae-
sarean section as soon as a pregnant woman goes into cardiac
ensure regular training in obstetric
arrest. In some circumstances immediate resuscitation attempts
will restore a perfusing rhythm; in early pregnancy this may enable
the pregnancy to proceed to term. Three observational studies
of 154 subjects collectivelyvery low quality evi-
dence regarding the use of peri-mortem Caesarean section. Based
More than 50% of people resuscitated from OHCAs in the United
on expert opinion, when initial resuscitation attempts fail, delivery
States are aged 65 years or incidence of cardiac arrests
of the fetus may improve the chances of successful resuscitation of
in elderly people is likely to increase as the world population ages.
the mother and fetus.systematic review documented 38
The incidence of cardiac arrest increases with age. In males, the
cases of Caesarean section during CPR, with 34 surviving infants and
incidence of OHCA at 80 years of age is about seven times greater
13 maternal survivors at discharge, suggesting that Caesarean sec-
than at 40 years of females above 70 years of age it is more
tion may have improved maternal and neonatal outcomes.
than 40 times greater than in women below 45 years of age. In an
best survival rate for infants over 24–25 weeks' gestation occurs
observational study on in-hospital cardiac arrest patients above 65
when delivery of the infant is achieved within 5 min after the
years of age accounted for 46% of the total hospital admissions in the
mother's cardiac requires that the provider
study period and for 65% of the ward cardiac this study,
commence the hysterotomy at about 4 min after cardiac arrest. At
the incidence of arrests was more than twice that in the younger
older gestational ages (30–38 weeks), infant survival is possible
patient population (2.2 versus 1.0 per 1000 patient admissions).
even when delivery was after 5 min from the onset of maternal
cardiac case series suggests increased use of Caesarean
Causes of cardiac arrest
section during CPR with team in this series no deliv-
The incidence of both coronary heart disease and chronic heart
eries were achieved within 5 min after starting resuscitation. Eight
failure increases with age. As a consequence, elderly people have
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
an increased incidence of cardiac causes of arrest.the
showed a significantly lower long-term survival than an age- and
proportion of deaths that are sudden (i.e. due to a primary ven-
gender-matched controls, while this was not observed in younger
tricular arrhythmia) decreases with age, due to a parallel increase
in the proportion of deaths due to other cardiovascular
In those who do survive, neurological outcome is good in elderly
The incidence of PEA as the first recorded rhythm increases signif-
survivors of cardiac arrest, with 95% having a cerebral performance
icantly with a parallel decrease of the incidence of
category (CPC) score of 1–2 on discharge from ICU72% at
shockable rhythms
Deterioration of vital signs leading to cardiac arrest is detected
Decision to resuscitate
less accurately in elderly patients, compared with younger
Elderly patients with cardiac arrest are significantly less likely
signs of acute life-threatening conditions such
to receive resuscitation than younger decid-
as sepsis,myocardial heart failure
ing to resuscitate elderly patients, age alone should not be the only
often blunted or non-specific in elderly patients, resulting in less
criterion to consider and other more established criteria, i.e. wit-
physiological aberration and a lower Modified Early Warning Score
nessed status, resuscitation times, and first recorded rhythm, are
(MEWS) in the 4 h preceding cardiac arrest.
important addition, we suggest that pre-arrest fac-
tors, such as the degree of autonomy, quality of life, mental status
and the presence of major comorbidities, should also be consid-
Management of periarrest conditions. Ageing is associated with sev-
ered. Whenever possible, a decision to resuscitate or not, should be
eral pathophysiological changes that should be taken into account
discussed in advance with the patient and his/her family (see ethics
when managing peri-arrest conditions. Increasing age is associated
of resuscitation and end-of-life decisions).
with autonomic and baroreflex dysfunction and with myocar-
dial stiffening which impairs early diastolic addition,
elderly critically ill patients are often hypovolaemic due to a reduc-
tion of both fluid intake and urine-concentrating
changes compromise the cardiovascular response to fluid loss or
Alessandro Barelli, Intensive Care Medicine and Clinical Toxicology,
postural changes and increase the hypotensive effect of sedatives
Catholic University School of Medicine, Rome, Italy
and other vasoactive drugs. Elderly patients are at increased risk of
Bernd W. Böttiger, Department of Anaesthesiology and Intensive
severe hypotension during emergency airway management.
Care Medicine, University Hospital of Cologne, Cologne, Germany
Atrial fibrillation is the most common supraventricular arrhyth-
Marios Georgiou, American Medical Center, Nicosia, Cyprus
mia in the elderly. It often causes cardiovascular compromise due
Anthony J. Handley, Honorary Consultant Physician, Colchester, UK
to loss of the atrial contribution for diastolic filling, particularly in
Thomas Lindner, Department of Anaesthesiology and Intensive Care,
the elderly who have reduced ventricular compliance. Hypotension
Stavanger University Hospital, Stavanger, Norway; Norwegian Air
and an increased heart rate may reduce coronary perfusion and
Ambulance Foundation, Drøbak, Norway
precipitate cardiac ischaemia, which is more likely in an elderly
Mark J. Midwinter, NIHR Surgical Reconstruction and Microbiology
population with a greater incidence of coronary artery disease.
Research Centre, University of Birmingham, UK
Older patients are more likely to develop apnea or respi-
Koenraad G. Monsieurs, Emergency Medicine, Faculty of Medicine
ratory depression following the administration of opioid or
and Health Sciences, University of Antwerp, Antwerp, Belgium;
lower baseline oxygen tension also
Faculty of Medicine and Health Sciences, University of Ghent,
increases the risk of developing hypoxia. Advancing age is asso-
Ghent, Belgium; Emergency Medicine, Ghent University, Ghent,
ciated with an increased rate of comorbidities. Elderly patients
often take several medications, which may interfere with drugs
Wolfgang A. Wetsch, Department of Anaesthesiology and Intensive
administered in peri-arrest conditions. The incidence of adverse
Care Medicine, University Hospital of Cologne, Cologne, Germany
drug reactions in the elderly is 2–3 times higher than in younger
Conflicts of interest
Management of cardiac arrest. No modifications of standard resus-
citation protocols are needed when managing aged patients in
Anatolij Truhláˇr
No conflict of interest reported
cardiac arrest. Rescuers, however, should be aware that the risk
No conflict of interest reported
of both sternal and rib fractures is higher in
No conflict of interest reported
incidence of CPR-related injuries increases with duration of
Charles D. Deakin
Director Prometheus Medical Ltd
No conflict of interest reported
No conflict of interest reported
No conflict of interest reported
Older age is associated with an increasingly lower short-term
Gamal Eldin Abbas
No conflict of interest reported
survival rate after cardiac a large registry of OHCAs,
survival to discharge was 8% for those aged 65–79 years, 4% for
Editor Resuscitation
octogenarians and 2% for another study, the
Guttorm Brattebø
Chair BEST foundation
adjusted risk for 30-day mortality in elderly resuscitated comatose
Medical advisor EURAC/ICAR alpine
patients was 1.04 (95% CI 1.03–1.06) per year of
Increasing age is also associated with lower long-term sur-
Editor Resuscitation
vival after resuscitation. In a retrospective cohort study on elderly
patients discharged alive after CPR from in-hospital cardiac arrest
Speakers honorarium CARDICA
the risk-adjusted rate of 1-year survival was 63.7%, 58.6%, and
Joost J.L.M. Bierens
Board member/Advisor KNRM; KNRD;
49.7% among patients 65–74, 75–84, and ≥85 years of age, respec-
Life Saving societies
tively (P < 0.001).another study patients ≥65 years of age
Karl-Christian Thies
Chair European Trauma Course
discharged alive after resuscitation from VF/pVT cardiac arrest
Organisation ETCO
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
Speakers honorarium Vidacare, Zoll
Medical advisor Physio Control and
HeartSine; Research grants Physio
Control, Philips, Zoll, Cardiac Science,
Defibtech, Jolife
No conflict of interest reported
Hunyadi-Antiˇcevi ´c
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
60. Brown D, Ellerton J, Paal P, Boyd J. Hypothermia evidence. Afterdrop,
and practical experience. Wilderness Environ Med 2015,
. Mar 27. [Epub ahead of print].
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
478. Quality standards for cardiopulmonary resuscitation practice and training.
Primary dental care – Quality standards for CPR and training; 2013. Avail-
500. Safe sedation practice for healthcare procedures: standards and guid-
ance; 2013. Available from:
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
537. Global Report on Drowning. Preventing a Leading Killer; 2014. Available from:
516. Emergency medical equipment training, advisory circular no. 121-34B;
2006. Available from:
518. Emergency medical equipment, advisory circular no. 121-33B; 2006. Available
519. Commission Regulation (EC) No 859/2008 of 20 August 2008 amending Council
Regulation (EEC) No 3922/91 as regards common technical requirements and
administrative procedures applicable to commercial transportation by aero-
plane. Off J Eur Union 2008. Available from:
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
635. World Disasters Report 2014; 2014. Available from:
668. SIGN 141 British guideline on the management of asthma; 2014. Available
653. Mikalsen IB, Skeiseid L, Tveit LM, Engelsvold DH, Oymar K. Decline in admis-
sions for childhood asthma, a 26-year period population-based study. Pediatr
Allergy Immunol 2015, Mar 18. [Epub
ahead of print].
663. Why asthma still kills: the national review of asthma deaths (NRAD). Confi-
dential Enquiry Report 2014; 2014. Available from:
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
712. Obesity and overweight. Fact sheet no. 311; 2015. Available from:
725. Trends in Maternal Mortality: 1990 to 2013. Estimates by WHO, UNICEF,
UNFPA, The World Bank and the United Nations Population Division;
2013. Available from:
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
788. Fitzpatrick K, Tuffnell D, Kurinczuk J, Knight M. Incidence, risk fac-
population-based cohort and nested case–control study. BJOG 2015,
. Feb 12. [Epub ahead of print].
A. Truhláˇr et al. / Resuscitation 95 (2015) 148–201
Source: http://www.medycynakatastrof.wl.cm.uj.edu.pl/documents/89149582/cf8617e1-6f23-4551-812c-e87322ba8cf3
> REPLACE THIS LINE WITH YOUR PAPER IDENTIFICATION NUMBER (DOUBLE-CLICK HERE TO EDIT) < Charge Density Study using Low Electrode Diameter in Epiretinal Prosthesis Diego Luján Villarreal, Dietmar Schroeder and Wolfgang H. Krautschneider. Abstract—Reducing electrode size can be advantageous for Having as a rule of thumb that one should avoid the onset of
Part 1: HealtH-cHallenged Skin By Mórag Currin The professional skin care industry is often in a better position Diabetes mellitus, commonly known simply as diabetes, is a chronic health condition where the body medical industry to deliver preventive health is unable to produce enough insulin and properly break care recommendations, providing services in an