Levitra enthält Vardenafil, das eine kürzere Wirkdauer als Tadalafil hat, dafür aber schnell einsetzt. Männer, die diskret bestellen möchten, suchen häufig nach levitra kaufen ohne rezept. Dabei spielt die rechtliche Lage in der Schweiz eine wichtige Rolle.
Remedy in the nhs: summaries of recent cases .pdf
Remedy in the NHSSummaries of recent cases
Remedy in the NHSSummaries of recent cases
Session 2007-2008
Presented to Parliament pursuant to
Section 14(4) of the Health Service Commissioners
Act 1993 (as amended)
The House of Commons
London: The Stationery Office
Crown Copyright 2008
The text in this document (excluding the Royal Arms and otherdepartmental or agency logos) may be reproduced free of chargein any format or medium providing it is reproduced accurately andnot used in a misleading context.
The material must be acknowledged as Crown copyright and thetitle of the document specified.
Where we have identified any third party copyright materialyou wil need to obtain permission from the copyrightholders concerned.
For any other use of this material please write to Office of PublicSector Information, Information Policy Team, Kew, Richmond,Surrey TW9 4DU or e-mail:
[email protected]
2 Remedy in the NHS June 2008
Remedy in the NHS June 2008
4 Remedy in the NHS June 2008
As Health Service Ombudsman, I conduct
confirm my own approach to recommending
independent investigations of complaints about
remedies when I have upheld a complaint.
NHS providers and practitioners: the final stage inthe complaints procedure. My investigations are
In terms of putting things right, the Principles are:
carried out in private but I occasional y publishanonymised summaries of selected cases.
• If possible, returning the complainant and,
where appropriate, others who have suffered
This is the first in what wil be an ongoing series
similar injustice or hardship to the position
of published summaries about NHS complaints
they would have been in if the
that I have investigated. My aim in publishing
maladministration or poor service had not
these summaries is to promote better and more
consistent complaint handling in the NHS and todemonstrate how I expect the NHS to put things
• If that is not possible, compensating the
right when things have gone wrong.
complainant and such others appropriately.
The cases have been chosen as apt il ustrations of
• Considering ful y and seriously al forms of
good or poor practice in putting things right
remedy (such as an apology, an explanation,
when they have gone wrong. They il ustrate the
remedial action to prevent a recurrence, or
variety and scope of my investigations about the
NHS and the types of remedies secured as aresult. Some of the cases focus specifical y on
• Providing the appropriate remedy in each case.
complaint handling (by the provider, thepractitioner, the Healthcare Commission or a
In some cases, a complainant might receive
combination of two or more of these). Others
financial compensation for direct financial loss.
involve failings in service provision – ranging from
Mrs G (page 33) feared her daughter's life was in
poor record keeping and poor communication
danger fol owing poor care and treatment for her
with patients, relatives and carers to more serious
eating disorder in an NHS unit. Mrs G took out a
clinical failings and, in one case, an avoidable
loan to pay for private treatment for her
daughter. In response to my recommendations,the Trust agreed to reimburse Mrs G the cost of
The cases also il ustrate my ‘Principles for
the private treatment and the interest paid on
Remedy'.1 These Principles (which fol ow on from
my ‘Principles of Good Administration'2) set outmy views on the Principles that should guide how
Financial compensation for non-financial loss may
public bodies provide remedies for injustice or
also be an appropriate remedy in some cases. For
hardship resulting from their maladministration or
example, in the case of Dr D (page 15), the
poor service. As wel as explaining how I think
complainant received financial compensation in
public bodies should put things right when they
recognition of the fact that the Trusts' poor
have gone wrong, the ‘Principles for Remedy' also
Remedy in the NHS June 2008
complaint handling resulted in her early
I have also included in this digest examples of
retirement and significantly disrupted her
cases where I have engaged a regulator (pages
personal and family life. In this case the
15 and 39), whether that is the Healthcare
complainant was a GP, il ustrating that the
Commission or Monitor, in taking forward my
Ombudsman can investigate complaints about
recommendations. In the case of Mrs J, I decided
the NHS from clinicians as wel as those from
to involve Monitor, the body which authorises
patients or carers.
and regulates NHS Foundation Trusts, because Iwas highly critical of the nursing care provided by
Many of the cases in this col ection highlight the
the Trust but was not satisfied that the Trust had
value of a sincere and timely apology and a
ful y learnt the lessons from the events which
wel -reasoned explanation for what went wrong.
prompted my investigation. Through the
In the case of Mrs N (page 21) I found that she
involvement of Monitor, I was assured that
was not given sufficient information about the
there would be an appropriate review of the
potential scarring she would have fol owing
Trust's progress in learning lessons from the
surgery, and therefore the validity of her consent
complaint. In this way, the regulator can work
was undermined. This was a case where financial
effectively with the Ombudsman to achieve
compensation could have been an appropriate
remedy for the injustice suffered, but Mrs N wassatisfied with an apology and an assurance that
The wider backdrop to this publication is the
lessons had been learnt and that action would be
changing landscape of complaint handling. A
taken to prevent a recurrence.
new system for handling health and social carecomplaints is due to come into place in
For those complained about, there can be
April 2009 and a pilot of the new arrangements
reputational risks of complaints to the
began in April this year, with support and advice
Ombudsman. Where appropriate, I wil not
from this Office. The changes also put my role,
hesitate to draw attention to those NHS
and that of the Local Government Ombudsman,
providers and practitioners involved so that poor
into sharper focus and give them greater
service is identified and lessons learnt.
prominence. This publication is therefore part ofan ongoing dialogue with the NHS about what
One case which I wish to highlight is that of
the Ombudsman expects of service
Dr Mrozinski (page 37). He refused to take part
commissioners, providers and complaint
appropriately in the local complaint handling
handlers under the new system.
process and refused to pay the financial redress Irecommended for the complainant in recognition
I responded jointly with the Local Government
of the unnecessary distress he had caused her.
Ombudsman to the proposals for a new system.
Such lack of insight and defensive behaviour
We specifically welcomed the emphasis on
deserve to be highlighted. I wil not hesitate to
effective complaint handling at local level;
use the sanction of publicity and draw
effective local leadership; a major cultural shift
Parliament's attention to such behaviour. It
by the NHS from a defensive application of
contrasts sharply with the cases I see where staff
process to a welcome for the learning from
providing NHS services respond openly and
complaints and a will to resolve them; the need
promptly to concerns.
for an outcome-based approach to complaints;
6 Remedy in the NHS June 2008
and effective governance arrangements across
complaint about health and social care and have
all organisations to underpin and support this
more such cases in the pipeline.
approach, and ensure that learning fromcomplaints is shared across the NHS and
In the short term, I recognise that the changes
social care.
will result in an increase in the number ofenquiries made to our Office and the number of
There is one other aspect of these proposals
investigations we undertake. We do not,
that has my strong support: that is, the direct
however, expect to take on the same number of
path from local resolution – if that should fail –
complaints for investigation as the Healthcare
to an independent Ombudsman.
Commission has done. As evidence, I note thatwhen the Scottish NHS complaints system
Currently, the second stage of the NHS
moved to a similar model (at the time of the
complaints procedure is provided by the review
introduction of the Healthcare Commission in
function of the Healthcare Commission, with a
England), the number of investigations increased,
possible third stage when a case goes to the
but not unmanageably so. The Scottish Public
Ombudsman. (Review by the Local Government
Services Ombudsman accounts for this by the
Ombudsman actually constitutes the fourth
focus, during the transition stages, on effective
stage in the social care complaints process.) The
local resolution, coupled with the disincentive
changes which are planned for April 2009 will
of a referral to the Ombudsman, with the
mean a simpler system that is less drawn out for
potential for adverse publicity which an
both the complainant and the service provider.
Ombudsman's finding can bring.
The regulator, the Care Quality Commission, willbe able to focus on its core business of
The focus on more effective local resolution is a
regulation and inspection, without the
key to making the new system work in practice. I
additional demand of complaint handling which
would like to play my part in assisting NHS
sits uneasily with its primary role. And a strategic
bodies to prepare for the changes. My ‘Principles
alliance between the Ombudsman and the
of Good Administration' set out the sorts of
regulator will ensure that any recommendations
behaviour I expect when public bodies deliver
the Ombudsman may make for systemic change
public services; my ‘Principles for Remedy' flow
are complied with, and followed up in the
from the ‘Principles of Good Administration'
inspection regime.
and, as noted above, set out my views on howpublic bodies should approach providing
I am working closely with the Local Government
remedies. I have also recently issued for
Ombudsmen to make sure that there is a fully
consultation my ‘Principles of Good Complaint
integrated approach to the complaints that cross Handling'.3boundaries between health and social care. Wehave already issued our first joint report into a
This latest set of Principles will set out forcomplainants and bodies in jurisdiction what the
Remedy in the NHS June 2008
Ombudsman expects by way of good complaint
culture. Is this an organisation which understands
handling. The same six Principles will underpin
and practises learning from complaints?
this document, as they do its two predecessors,but apply them in the complaint handling
As with al our Principles, those on complaint
handling wil not be a checklist to be appliedmechanical y. I am not in the business of
Getting it right wil be about getting the right
providing a manual of how to stay on the right
leadership, governance and culture – ownership at side of the Ombudsman. Rather, I am providing athe top of the organisation; about equipping and
framework of Principles. I expect public bodies to
empowering decision makers on complaints;
use their judgment in applying those Principles to
about focusing on outcomes not processes; and
produce reasonable, fair and proportionate
about signposting to the Ombudsman in the right
results in the circumstances. I wil adopt a similar
way at the right time.
Being customer focused wil be about providing
I hope that my framework of Principles wil prove
an accessible complaints service, with help to
useful to complaint handlers without tying them
make complaints for those who need it: a service
to precise and possibly unsuitable templates.
that is simple, speedy, joined-up with other
Over time I wil use my experience of them to
providers, flexible, sensitive and tailored to
feed back to the NHS lessons about both good
people's needs – not ‘one size fits al '.
and bad practice in complaint handling.
Being open and accountable wil be about
Final y, I did not think it was necessary to spel
publicising complaints procedures clearly and
out the value of complaints in this foreword; the
wel ; about keeping proper records of complaints;
cases speak powerful y for themselves about the
and about giving reasons for decisions.
individual and public benefit of effectivelyresolved complaints. However, I do want to do
Acting fairly and proportionately wil be about
more to tel the NHS about the Ombudsman's
decisions being reviewed by someone other than
role in the complaints system, and to encourage
the original decision maker; about natural justice
better and more consistent complaint handling
– to al the parties; and about not using
practice across the NHS. This document is a key
sledgehammers to crack nuts.
part of that ongoing process.
Putting things right wil be about remedy. Notonly apologies and explanations – important asthey are – and not only changes to prevent arecurrence – important as they are, as wel , but,as we have seen, financial remedies where they
are justified and appropriate.
Parliamentary and Health Service Ombudsman
Seeking continuous improvement wil be about
learning. But it wil also be about attitude and
8 Remedy in the NHS June 2008
Complaint about Basildon and Thurrock University Hospitals
NHS Foundation Trust (the Trust) and the Healthcare
Commission (the Commission)
Complaint about the care and treatment of a
The Trust's response to the complaint
critical y il child admitted with breathing
encompassed three letters and two meetings
problems, and complaint about the Commission's
with Mr and Mrs A between February and
subsequent review
August 2004. The Trust acknowledged someshortcomings, apologised and highlighted actionsarising from the case including the introduction
Background to the complaint
of individualised il ness management plans forchildren with complex conditions; a system of
Miss A, aged 17, suffered from multiple and severe
flagging children with special needs on the
health problems from birth and her parents were
patient administration system; and developing
her ful -time carers. As she required frequent
summary history sheets at the front of patients'
hospital contact, she had direct access to the
notes. The Trust also subsequently reported
paediatric unit. In August 2003 she was admitted
improved staffing levels.
to the paediatric unit with shortness of breathand coughing, on the advice of the Paediatric
In November 2004 Mr and Mrs A complained to
Triage Team, which her parents had contacted.
the Commission, which reviewed the case having
Some hours later, when her condition failed to
taken clinical advice. In February 2006 it
improve, she was transferred to the Intensive Care concluded that the Trust had taken steps toUnit; however, sadly, she died an hour later.
reduce the risk of similar problems occurring inthe future and that there was no scope to takethe complaint further.
The complaint to the Trust and the Commission
In January 2004 Mr and Mrs A complained to the
What we investigated
Trust about Miss A's care and treatment and inparticular her delayed admittance to the
Mr and Mrs A complained to the Ombudsman in
Intensive Care Unit, the failure to cal the duty
April 2006 and we investigated the complaint as
consultant when Miss A was admitted and the
put to the Trust as wel as the Commission's
fact that the consultant was not on the hospital
site. They believed that there had been a failurein care and that Miss A had not been adequately
We had access to Miss A's medical records for the
reviewed by a senior doctor. They also believed
last five years of her life and copies of al
that, had she been transferred to the Intensive
complaints correspondence. We also took clinical
Care Unit more quickly, she would have survived.
advice from a Senior Nurse with paediatricexperience and obtained a ful report from aConsultant Paediatrician.
Remedy in the NHS June 2008

What our investigation found
• Delay in transferring Miss A to a High
Dependency or Intensive Care Unit despite
Our investigation found the fol owing significant
clear indications that she needed more
failings during Miss A's admission:
intensive care than was available on thepaediatric ward.
• Inadequate monitoring.
We found that the standard of care provided to
• Poor record keeping in terms of both nursing
Miss A during her last il ness fel below a
and medical notes.
reasonable standard. This amounted to servicefailure on the part of the Trust. We concluded
• Failure to recognise the seriousness of
that, while it would never have been possible to
Miss A's condition.
say for certain whether Miss A would havesurvived her il ness had she been transferred to
• Delays in seeking and obtaining reviews by
the Intensive Care Unit at an earlier stage, there
seemed little doubt that her chances would havebeen improved.
• Delay in contacting the on-cal consultant.
10 Remedy in the NHS June 2008
We also found that the Trust had not
• the regular auditing of new joint medical and
acknowledged or apologised in relation to several
key issues from Mr and Mrs A's original complaint.
• the appointment of a paediatric clinical
We also concluded that the Commission's review
practice facilitator; and
was seriously flawed because it was not clear thatsufficient clinical advice had been taken from a
• the establishment of professional liaison with
properly qualified adviser and the clinical advice
the regional paediatric intensive care
had not been recorded properly on file (the
consortium as a resource for advice, training
Commission's files contained only a brief note of
and service strategy.
a discussion with an adviser which gave noindication of the adviser's qualification and did
The Commission wrote to Mr and Mrs A to
not make clear if the adviser had seen the
apologise for the shortcomings in its review and
relevant clinical records).
for any distress or frustration that this hadcaused. The Commission also explained that its
The investigation, which concluded in
policy now required that clinical advice be
September 2006, upheld the complaints against
recorded in appropriate detail (either the adviser's
the Trust and the Commission.
report or a signed record of a detaileddiscussion).
As a result of our recommendations the Trustwrote to Mr and Mrs A to apologise for theshortcomings identified in our report.
The Trust also drew up a comprehensive actionplan in response to our recommendations whichincluded:
• the commissioning of a designated paediatric
high dependency facility;
• the implementation of a paediatric early
warning system, which has been integratedwith an updated monitoring chart for critical yil children;
• staff induction and training programmes, which
include the recognition and resuscitation ofcritical y il children;
Remedy in the NHS June 2008
Complaint about University Hospital Birmingham NHS
Foundation Trust (the Trust) and the Healthcare Commission
Complaint about the care and treatment of an
discharge planning in general, with emphasis on
elderly patient with Alzheimer's disease and
older vulnerable adults who might have
coeliac disease fol owing an admission for
planned surgery, and complaint about the
Commission's subsequent review
Mrs L complained again, met with the Trust inApril 2006 and received a further writtenresponse in June 2006. The Trust acknowledged
Background to the complaint
and apologised for several errors, including: thefailure to order gluten-free meals; Mr L being
Mr L, aged 79, lived in a nursing home and had
unable to take anti-sickness medication as it was
Alzheimer's disease (he was not able to
prescribed in the wrong form; and failure to
communicate) and coeliac disease (he required a
dispense medication due to wrong information
gluten-free diet). In December 2005 Mr L was
on a prescription.
admitted to Sel y Oak Hospital (the Hospital) forsurgery to remove a squamous cel carcinoma
In July 2006 Mrs L complained to the Commission
lesion (a common type of skin cancer). The
which, in September 2006, asked the Trust to
referral letter to the Hospital explained about
provide Mrs L with a response to outstanding
Mr L's medical conditions and that he needed
issues, which they did in November 2006. Mrs L
assistance with eating and drinking. The
complained again to the Commission, but it
operation, which was successful, took place on
decided to take no further action.
the day after Mr L's admission. Eight days afterthe operation Mr L was discharged and returnedto the nursing home by ambulance.
What we investigated
Mrs L complained to the Ombudsman, in
The complaint to the Trust and the Commission
February 2007, about the care and treatmentprovided to Mr L, in particular:
Mrs L, Mr L's wife, complained to the Trust inJanuary 2006 about Mr L's discharge
• that the Hospital did not pay sufficient
arrangements, lack of adherence to his dietary
attention to her husband's mental state,
requirements, the decision to send him for
al owing him to be taken into theatre for
surgery when she was not present, and the
surgery and later discharged back to the
administration and prescription of drugs on
nursing home without her being present;
discharge (medication was prescribed in thewrong form and other medication could not be
• that Mr L was not provided with gluten-free
dispensed due to an error on the prescription).
meals during his time in the Hospital, despite
She said that an inexcusable lack of consideration
the fact that the staff knew about his
by the Trust had caused Mr L great distress. In
nutritional needs, and Mrs L was forced to
February 2006 the Trust offered a number of
bring food in for him herself; and
explanations and apologised for theinconvenience and distress caused and said that
• that Mr L's medication on discharge was wrong,
in the light of the complaint they had looked at
in that he was not given anti-nausea drugs to
12 Remedy in the NHS June 2008
prevent travel sickness and that his medication
trying to rectify the failing or provide
was not provided in a soluble form, despite his
difficulties with swal owing.
• There was unacceptable confusion over Mr L's
Our investigation considered Mrs L's complaints
medication, which meant that he was given
against the Trust as wel as the Commission's
tablets despite his difficulties with swal owing,
was prescribed the wrong medication ondischarge, and then did not receive the
We had access to al relevant documentation
medication because of an error.
including Mr L's medical records and thecomplaint correspondence. We also took clinical
• The Commission's investigation of Mrs L's
advice from an adviser with expertise in the
complaint was poor. There was little evidence
nursing of the elderly.
that an objective investigation was carried outand no clinical advice was passed on to Mrs L
We also took note of the relevant standards
about the standard of care and treatment
relating to clinical care and the treatment of older
provided to her husband, or about the
people. Of particular relevance were the National
adequacy of the Trust's proposed initiatives to
Service Framework for Older People (2001) and
address the problems.
the NHS Modernisation Agency's benchmarkingtool ‘Essence of Care'.
The investigation concluded in September 2007and we upheld Mrs L's complaints against theTrust and the Commission.
What our investigation found
• Mr L was caused avoidable distress by the
failure to ensure that his wife was presentwhen he was taken for surgery and when he
As a result of the Ombudsman's
was discharged. There was a lack of awareness
recommendations, the Trust took a number of
of his needs arising from his Alzheimer's
actions, including:
disease, because of the failure to adequatelyassess him upon arrival, the lack of a
• the production of ‘Al about me' (a document
personalised care plan, and the failure to begin
aimed at improving communication with
discharge planning at an early stage.
patients and those caring for patients withdementia, head injuries and learning
• The Hospital failed to provide a suitable diet
for Mr L, despite being told in advance of hisneeds. It was unreasonable that Mrs L was
• the development of a discharge care plan
placed in a position where she felt she had to
checklist to ensure safe and timely discharge
bring food in from home for her husband,
from hospital with provision of relevant
incurring expense and inconvenience. Hospital
information to patients and families;
staff had then accepted this situation without
Remedy in the NHS June 2008

• a range of dementia training and the
• annual benchmarking of the suitability of
nomination of an ‘older people's champion' in
wards to care for older people with mental
each ward or department to review the service
• an offer to include Mrs L's experience in the
• a review of the Trust's guidelines about
Trust's training programme; and
communicating with carers and relatives;
• nutrition link nurses to highlight the nutritional
• a successful bid to re-establish the post of
needs of older people and special diets.
Trust Mental Health liaison nurse;
As a result of the Ombudsman's recommendationthe Commission wrote to Mrs L to apologise forthe deficiencies identified in its review.
14 Remedy in the NHS June 2008
Complaint against Medway Primary Care Trust (Medway)
and West Kent Primary Care Trust (West Kent)
Remedy for a former general practitioner who
After Mrs B wrote back to Medway confirming
retired on health grounds as a result of the poorly her dissatisfaction with the Practice's response,
handled investigation of a complaint against her
they treated her letter as a request to proceed tothe second stage of the NHS ComplaintsProcedure. Responsibility for arranging a Review
Background to the complaint
was delegated to Kent Primary Care Agency (theAgency) which operated under the management
In August 2002 Mrs B took steps to register at the
of the then Dartford, Gravesham and Swanley
Practice at which Dr D worked. A ‘new patient'
Primary Care Trust (now West Kent). The
check was required before registration could be
paperwork relating to the complaint got lost in a
completed and was arranged for 3 September.
departmental move.
During that appointment an altercation tookplace between Mrs B and the nurse, which Dr D
On 2 October 2002 Dr D replied personal y to
overheard. She advised the nurse to tel Mrs B
Mrs B's complaint, apologising for the delay in
that she would not be accepted for registration.
responding, caused by her absence on leave, and
Mrs B left the surgery, verbal y abusing the nurse
setting out her view of the events of
as she left. Dr D fol owed Mrs B into the street,
3 September. On 11 November Medway realised
and told her ‘You do not cal my nurse a bitch,
that the Agency had not received the complaint
lady'. The same day Mrs B sent Dr D a letter of
documentation, and they forwarded the papers
complaint, to which the Practice Manager replied
again; Dr D's letter to Mrs B was not included. On
setting out the Practice's view of events.
15 November Dr D wrote to ask the Agency ifthey had taken account of her letter to Mrs B
On 6 September 2002 Mrs B wrote to the Chief
when considering the Review request. She
Executive of Medway to complain about Dr D,
pointed out that she had never consulted with
apparently not having received the Practice
Mrs B. Two weeks later the Agency told Mrs B
Manager's letter. Mrs B wrote to the Practice
and Dr D that a Convener had decided that a
Manager on 8 September, having by then received conciliator might help resolve the complaint.
her letter, explaining that she had complained to
They did not answer Dr D's question about her
Medway. On 16 September Medway asked Dr D to letter to Mrs B, nor address her point that sherespond to Mrs B's complaint letter and informed
had not consulted with her.
Mrs B that she could request an IndependentReview (Review) of her complaint if she was
In January 2003 Mrs B and Dr D were told that the
dissatisfied with the Practice's eventual response.
conciliation process had ended, and that Mrs B
Mrs B replied that she had already received a
could stil request a Review. She did so. The
response from the Practice, which she felt was
Practice Manager wrote to ask Medway and the
unsatisfactory. Medway told Mrs B that she now
Agency how a Review could be considered when
had the right to request a Review, but did not say
Mrs B was not a registered patient. The Agency
they had already asked Dr D to respond directly
responded that Mrs B had the same right to
complain as any visitor to the Practice. Medwaywrote to Dr D in response to the PracticeManager's letter; they said they understood that aReview Panel had been convened, but did not
Remedy in the NHS June 2008

answer the question about whether Mrs B wasentitled to pursue a complaint. In March Dr D'srepresentative wrote to Medway, repeating thatMrs B had never been a formal patient at thePractice.
The Panel met in June 2003 and partly upheldMrs B's complaint. They said that Dr D had notbreached her Terms of Service for GeneralPractitioners, because Mrs B had not beenregistered with the Practice. The Panel's reportnoted that the complaint arose out of Mrs B'sattempts to register, but nonetheless said that
‘such a complaint fal s within the guidelines of
the Health Service's Complaints Procedure'. Dr D's
mental state was such that the day of the hearingwas her last day in general practice. She took sickleave and was admitted in September to apsychiatric hospital with bipolar disorder. Sheretired from general practice on health grounds inMarch 2004.
Dr D complained to the Ombudsman inAugust 2003, wanting an investigation into theprocess that had led to the Panel sitting at al . She felt she had been the victim of a ‘witch hunt'
and said that the Trusts' mishandling of thecomplaint against her had cost her her career, and significantly disrupted her personal andfamily life.
What we investigated
• The management of the complaint against
Dr D, and whether the resulting stress had ledto the deterioration of her mental health andresignation from general practice.
• Dr D's al egations that both Trusts had been
biased against her in favour of Mrs B, had
16 Remedy in the NHS June 2008
failed to treat her objectively, and had not
• The Trusts' investigation lacked a sense of
properly supported her.
perspective and proportionality. It was drivenpurely by process, with an absence of overal
• The matter of the jurisdiction of Mrs B's
leadership and guidance to determine whether
original complaint, since this was a factor in
the progress and direction of the investigation
assessing the adequacy of the Trusts'
were appropriate to the nature of the
management of the investigations.
• There was no evidence of bias against Dr D, or
What our investigation found
that the Trusts had given her insufficientsupport throughout their investigation.
• Key documents were not sent to Dr D in a
We concluded our investigation in May 2007 andupheld Dr D's complaint. The maladministrative
• Medway did not inform Dr D that they had
handling of the complaint against her contributed
told Mrs B that she could ask for a Review,
to a significant change in the nature of a
despite asking Dr D to provide a local
pre-existing psychiatric il ness. There was
resolution letter.
extensive and persuasive medical evidence toindicate that that maladministration had led to
• Dr D's letter to Mrs B was unreasonably
Dr D's retirement on health grounds.
dismissed throughout the investigationbecause it arrived very slightly late, despitevalid reasons for the delay.
• The fact that a Review into the complaint had
Both Trusts agreed to:
been arranged was inappropriately disclosed toDr D as an aside in a letter.
• pay the sum of £25,000 to Dr D to remedy the
significant injustice to her;
• Both Trusts repeatedly failed to answer Dr D's
reasonable questions about whether they had
• write personal y to her to apologise for their
considered her letter to Mrs B, and whether
Mrs B was even entitled to pursue a complaintunder the NHS Complaints Procedure.
• use our investigation to inform a thorough
review of their existing complaint handling
• We made no finding, however, on the issue of
procedures, and use the findings of that
Mrs B's status as a patient with the Practice at
review to develop an action plan to be agreed
the time of the incident, since the matter
with the Healthcare Commission (in its role as
turned on technical arguments that could only
be settled in a court of law.
Remedy in the NHS June 2008
Complaint about Good Hope Hospital NHS Trust (the Trust)
(now Heart of England NHS Foundation Trust) and the
Healthcare Commission (the Commission)
Complaint about the care and treatment of a
The complaint to the Trust and the Commission
woman who was later found to have pulmonary
hypertension and who died fol owing surgery, and
Ms C's mother, Mrs C, complained in
a complaint that the Commission did not address
November 2003 about the failure to diagnose
the Trust's failure to fol ow the Commission's
pulmonary hypertension at an earlier stage. She
questioned whether the earlier commencementof specialist treatment for Ms C might haveprevented her death. The Trust could not find
Background to the complaint
Ms C's medical records. Mrs C had a meeting with Trust staff in April 2004, but this failed to
Ms C was 42 when she had a stroke in
resolve matters.
February 2002 and was admitted to hospital. She had a pulmonary embolus (a blood clot on
In September 2004 Mrs C complained to the
the lung) and was prescribed Warfarin (an
Commission which took clinical advice from a
anti-coagulating drug) which was stopped after
Consultant Cardiologist, who found a number of
six months. Tests were carried out to determine
failings in the care provided to Ms C. In
her blood clotting levels and to search for a
December 2005, the Commission asked the Trust
patent foramen ovale (a hole in the heart which
to provide explanations of those aspects of
would al ow blood clots to travel from the right
Ms C's care and to change clinical procedures. The
side of the heart to the left side and from there
Trust responded in February 2006.
to the brain thus causing a stroke). This test wasperformed initial y using a transthoracic and
In April 2006 Mrs C complained to the
subsequently a transoesophageal echocardiogram
Commission, which said that the Trust had
(an ultrasound test that can provide information
complied with most of its recommendations, but
about the structure and function of the various
asked them to respond on the issue of the review
areas of the heart).
of guidelines for management of pulmonaryembolism. The Trust sent a further reply to
After review as an out-patient, Ms C was
Mrs C in June 2006 which made no
discharged from care but was readmitted in
acknowledgement or apology for the failings
August 2002 and was found to have another
identified by the Commission.
pulmonary embolus. She was referred for an MRIscan which was due to take place in March 2003but, before this happened, she moved house.
What we investigated
She was subsequently diagnosed elsewhere ashaving pulmonary hypertension and a large
Mrs C complained to the Ombudsman in
patent foramen ovale. She was transferred to
September 2006. The complaints investigated by
Papworth Hospital for treatment but died
the Ombudsman were that:
shortly afterwards.
• the Trust had failed to respond adequately to
the Commission's recommendations fol owingits investigation; and
18 Remedy in the NHS June 2008
• the Commission had refused to take any
further action despite that failing by the Trust.
As a result of the Ombudsman's
We had access to al relevant documentation
recommendations the Trust made a payment of
including Ms C's medical records and the
£500 to Mrs C in the light of the serious failings in
complaints correspondence. We took clinical
their complaint handling and to recognise the
advice from a consultant cardiothoracic surgeon.
additional distress caused by their responses toMrs C fol owing the Commission's review.
What our investigation found
We found that the Commission had carried out
• apologised for the loss of records and
an appropriate initial review of Mrs C's complaint
explained that they had introduced a tracking
that identified failings by the Trust and made
system for physical documents, an electronic
patient record for clinical data and weremoving towards al patient documentation
We found that the Trust's response to the
being accessible electronical y;
Commission's recommendations was inadequate.
They had failed to acknowledge the failure in care
• produced an amended template for recording
and to explain the reasons for it. Neither had
and reporting echocardiograms to help ensure
they accepted the Commission's recommendation
that clear diagnosis is obtained;
that reporting procedures or guidelines neededto be reviewed.
• reviewed their guidelines for the
management of pulmonary embolism and
We found that the Commission had failed to
implemented those recommended by the
properly consider Mrs C's subsequent complaint
British Thoracic Society;
about the Trust's response.
• offered an explanation of the criteria that
We found that the Trust's actions (through
would have led to onward referral for Ms C,
mislaying papers and not responding
an acknowledgment of the fact that a referral
appropriately to the Commission's
could have been made earlier and an apology
recommendations) had caused Mrs C to suffer
that the process was so protracted. They said
distress and delay in receiving the explanation and
that training was to be provided to staff to
response to which she was entitled.
increase awareness of symptoms of pulmonaryhypertension and the need for onward referral;
The investigation concluded in July 2007 and weupheld Mrs C's complaint that the Trust failed to
• explained the procedure surrounding
respond adequately to the Commission's
transoesophageal echocardiogram tests and
recommendations and that the Commission failed
the reasons for delays in scheduling the MRI
to properly consider her subsequent complaint
scan for Ms C. They said that transoesophageal
about the Trust's response.
echocardiograms that do not provide clearresults would be discussed at regular meetings
Remedy in the NHS June 2008

and that transoesophageal echocardiogramresults would be audited for quality of dataand accuracy of interpretation. A leadconsultant for this work had been identifiedand staff training had led to British Society ofEchocardiography accreditation; and
• acknowledged and apologised for the failure
of care towards Ms C.
The Commission wrote to Mrs C to apologise forthe failings identified by our report.
20 Remedy in the NHS June 2008
Complaint about South Devon Healthcare
NHS Foundation Trust (the Trust) and the
Healthcare Commission (the Commission)
Complaint about the care and treatment of
The complaint to the Trust and the Commission
a patient in relation to a bilateral mastectomy,
and complaint about the Commission's
Two days after her discharge Mrs N complained to
subsequent review
the Trust in writing about the appropriateness ofthe surgery and the consent procedure in relationto the nature and extent of potential scarring. The
Background to the complaint
Chief Executive responded to the complaint inSeptember 2005 and said that the bilateral
In December 2004 Mrs N was referred by her GP
mastectomy was the correct procedure and that
for a mammogram which showed that she had
the surgeon had acted appropriately.
smal tumours in both breasts. A bilateralmastectomy (surgery to completely remove both
Mrs N remained dissatisfied and in October 2005
breasts) was recommended.
she complained to the Commission which foundthat the procedure was appropriate and the
In February 2005 Mrs N attended Torbay Hospital
scarring within normal range. It did, however, find
where she was provided with information about
shortcomings relating to consent and asked the
her condition. Mrs N discussed the issue of
Trust to look at those issues (both in terms of
scarring with the Breast Care Nurse and
reminders to staff about the importance of
emphasised that the position and cosmetic
ensuring that consent forms were completed ful y,
appearance of the resulting scars were both very
and giving patients the opportunity to ask
important considerations for her. Later that
questions when there is a time lag between
month, the Consultant Surgeon who was to
consent being given and an operation carried out)
perform the operation gave Mrs N a consent form and to inform Mrs N of resulting changes into sign; however, she had yet to decide whether
policy. The Commission, in two replies (February
she would proceed with the proposed surgery and and March 2006) concluded that, despite thedid not sign the form immediately.
shortcomings identified, consent had beenobtained on a properly informed basis.
In March 2005 Mrs N signed the consent form.
She was admitted to Torbay Hospital in early
April 2005, and underwent a bilateral mastectomy. What we investigated
When the bandages were removed Mrs N washorrified to discover that, rather than two scars
In April 2006 Mrs N complained to the
below the breast line, as she had been expecting,
Ombudsman. Our subsequent investigation
she had been left with what appeared to be a
single horizontal scar across her chest wal , aboveher breast line. Mrs N was shocked and extremely
• the Commission's handling of her case; and
distressed by the extent, position and appearanceof her scarring and raised her concerns
• the standard of care and treatment provided
immediately with a member of the Trust's staff.
by the Trust in terms of informed consent, and
Mrs N was discharged the next day.
the appropriateness of the procedure.
Mrs N made clear that she had pursued her
decide whether or not to go ahead with the
complaint in order to have it acknowledged that
surgery with ful knowledge of the potential risk
the operation she received was not the one for
which she gave consent, not to obtain financialcompensation.
The investigation found that, having reviewedappropriate evidence and sourced appropriate
We examined al the relevant documentation and
advice, the Commission's resulting decision that
obtained specialist clinical advice from a
Mrs N's consent was ful y informed was
Consultant Breast Surgeon who is also a Professor
unreasonable, as it did not properly reflect the
of Breast Cancer. We also took account of the
evidence assessed or clinical advice received.
relevant standards contained in the Department
This caused Mrs N additional inconvenience
of Health's ‘Reference Guide to Consent for
and distress.
Examination or Treatment' (2001) and the GeneralMedical Council's ‘Seeking patients' consent: The
The investigation concluded in February 2008 and
ethical considerations' (1998).
we upheld Mrs N's complaints against both theTrust and the Commission.
What our investigation found
We found that the bilateral mastectomy was anappropriate procedure for Mrs N.
As a result of our recommendations the Trust andthe Commission agreed to apologise to Mrs N for
We found that some parts of the consent process
the shortcomings identified in our report and the
were reasonable, insofar as different treatment
injustice she had suffered.
options were described, nursing staff wereinvolved in the consent-making process, and
In addition to the action they had taken as a
Mrs N was given the opportunity to reflect before result of the Commission's recommendations, theand after making a decision. However, we noted
Trust also agreed to give Mrs N an assurance that
that there was no review of the consent at the
lessons had been learnt from her complaint and
time of the admission immediately before the
an explanation of the changes made to prevent
operation. We also concluded that, based on the
such failures being repeated.
information given to Mrs N pre-operatively, itwould have been reasonable for her to expecttwo separate scars running horizontal y across thelower to middle part of her chest. The fact thatMrs N was not given more specific informationabout the risks of the procedure impacted on herability to give ful y informed consent. We foundthat, overal , there were sufficiently seriousshortcomings in the consent process toundermine the validity of the consent, with theresult that Mrs N was denied the opportunity to
22 Remedy in the NHS June 2008
Complaint about Southend Hospital NHS Trust (the Trust)
and the Healthcare Commission (the Commission)
Complaint about the care provided to an elderly
January 2003, he appeared to be better and was
dying man, the attitude of staff towards him and
sitting out of bed, although he was stil very
his wife, and about the way a complaint was
depressed. Over the next week, his condition
handled by both the Trust and the Commission
fluctuated as he became drowsy anduncommunicative, and unwil ing to eat or drink.
He refused further intervention and said that he
Background to the complaint
wanted to be left alone. As time went on, he wasin more pain; his opiate painkil er dose was
Mr V was 86 years old when he was admitted to
increased and given on a regular basis. He became
Southend Hospital in December 2002,
unresponsive, and his condition deteriorated
complaining of abdominal pain, intermittent
further. He died in mid-February 2003.
vomiting and diarrhoea. He had a history ofdiverticulitis (a digestive disease caused byinflammation of pouches which have formed on
The complaint to the Trust and the Commission
the outside of the colon) and irritable bowelsyndrome with chronic abdominal pain. On this
Mrs V, Mr V's wife, complained to the Trust in
occasion, the doctors diagnosed a smal bowel
December 2003. She attended a meeting with
obstruction: he was given intravenous fluids as
them in February 2004 at which statements by
the diarrhoea and vomiting had made him
nurses (which detailed their communications with
Mrs V about her husband's care) were read out.
Mrs V was extremely upset by those statements;
Mr V was cared for in the Intensive Care Unit for
the Trust then wrote to her expressing regret that
two days and, having made an initial recovery, was
the meeting had not resolved matters, but gave
transferred to a surgical ward and then, 13 days
no explanations about her husband's care. An
later, to a medical ward. Within a few days of this
exchange of letters fol owed and, in August 2004,
latter transfer, Mr V became less wel . He
Mrs V requested a further meeting; the Trust
complained of abdominal and back pain, became
refused and said that she could approach
constipated and had a poor appetite. His left arm
the Commission.
became swol en and pressure sores developed onhis elbows; MRSA was detected in the left elbow.
In May 2005 the Commission referred Mrs V's
He appeared depressed and was given an
complaint back to the Trust, asking that a
antidepressant. It seemed that a long-standing
conciliation meeting be held. Neither Mrs V nor
thyroid function problem was not being
the Trust agreed to this. In September 2005 Mrs V
adequately addressed, so his thyroxine daily dose
complained to the Ombudsman. As the
was increased.
complaint had not been investigated by theCommission, it was referred back for review. In
Mr V then developed a fever and blood tests
January 2006 the Commission wrote to Mrs V,
indicated an infection, so he was given
with their final decision, suggesting that she
intravenous antibiotics. Nine days later, Mr V
contact the Information Commissioner if she
complained of back pain and was prescribed an
wished to have medical records corrected. Mrs V
opiate painkil er. Over the fol owing fortnight,
contacted the Ombudsman again in
Mr V's chest condition improved. By the end of
February 2006.
Remedy in the NHS June 2008

What we investigated
• staff were unhelpful and unsympathetic to
both Mr and Mrs V; and
Mrs V remained concerned about the care herhusband received on the ward and subsequent
• neither the Trust nor the Commission had
complaint handling. Her complaints
responded adequately to her complaints.
correspondence made clear that she believedthat Mr V had been caused undue suffering and
We had access to Mr V's medical and nursing
stress and that she had been caused unnecessary
records and al of the complaints
distress by the way in which her complaints had
correspondence. We also took clinical advice
been handled. The main elements of her
from a Hospital Consultant with experience in the
Care of the Elderly and a Senior Hospital nurse.
• the nursing care provided to Mr V on the
In framing the recommendations on this case we
medical ward was inadequate;
made particular reference to the NHSModernisation Agency's benchmarking tool‘Essence of Care' (2003).
24 Remedy in the NHS June 2008
What our investigation found
We found that while there was evidence of
As a result of the Ombudsman's
reasonable medical and nursing care in most
recommendations the Trust:
areas, there had not been adequate planning forcommunication with Mr and Mrs V. Mrs V had
• wrote to Mrs V in October 2006 to apologise;
also been very concerned to see her husband inpain, and we found that pain relief interventions
• said that the Deputy Ward Manager would
could have been made at an earlier stage.
attend a specialist external training course onrecord keeping and then facilitate training
There was also evidence in the nursing records
sessions for staff on record keeping. These
and statements made by nursing staff that they
elements would also be emphasised in staff
had found it difficult to deal with Mrs V. It
induction and in ongoing training;
appeared that they had held negative perceptionsof Mrs V and had provided little support when
• put in place a programme to implement the
her husband died. We found that junior staff had
‘Essence of Care' communication standard and
not been wel supported by their seniors in
al other ‘Essence of Care' standards, with the
dealing with a difficult situation.
assessment of the medical ward to take placeas part of that programme; and
We found that the Trust had failed to addressMrs V's complaint adequately by not responding
• reviewed and republished their complaints
to her original concerns about Mr V's care and
policy and procedure (along with other
that this served to increase her distress.
supporting documentations) with particularemphasis on the support available to staff
We found that the Commission failed to
members in handling ‘Difficult situations or
adequately address Mrs V's concerns about the
complainants', the need to avoid judgmental
Trust as it misunderstood her complaint, believing
statements and a designated framework for
it to be about inaccuracies in medical records and
conducting local resolution meetings.
therefore advising her to approach theInformation Commissioner.
The investigation concluded in October 2006 andwe upheld Mrs V's complaints against the Trustand the Commission.
Remedy in the NHS June 2008
Complaint about Cambridge University Hospitals NHS
Foundation Trust (Cambridge) and Hinchingbrooke Health
Care NHS Trust (Hinchingbrooke)
Complaints about the assessment and
(ICU) lead – the difficulty of placing a breathing
management of an adolescent's scoliosis; the
tube in Q's throat because of his rigid neck. It was
post-operative care and treatment which led to
decided to pass a flexible fibre optic scope
his death; and the handling of complaints about
through Q's nose to visualise the opening of the
windpipe and to pass a breathing tube over thescope and into his windpipe. That wasaccomplished and the operation went according
Background to the complaint
to plan. Dr Y and Dr P decided to keep Q on abreathing machine for 24 to 48 hours after the
In January 2000 Q, then aged 13, attended a
surgery, by continuing to ventilate him through
combined Spinal Deformity Clinic at Cambridge
the nasal tube. After surgery Q was transferred to
(the Clinic), at which Mr M (Paediatric
the ICU, where he was placed on volume
Orthopaedic Surgeon) and Mr H (Visiting
control ed ventilation and received fluids. There
Consultant Orthopaedic Surgeon from
were unexpected problems with Q's care: he
Hinchingbrooke) assessed children and
developed Adult Respiratory Distress Syndrome
adolescents with scoliosis (a spinal deformity).
(ARDS – a severe form of acute lung injury) from
Q was assessed as having scoliosis and put on the
which he did not recover. He lost fluids and his
waiting list for surgery. In January 2001 Q's father,
blood pressure dropped. A central venous
Mr R, asked if the operation could be carried out
pressure line was inserted and a tracheostomy
in early summer. Mr H explained that many
was performed, al owing the nasal tube to be
parents wanted their children treated at a time
removed. Secretions on the tube from sinusitis
that did not interfere with schooling, but he
cultured positive for MRSA. Steroids were started
would do what he could.
as treatment for the acute lung injury but Q'scondition continued to deteriorate. He died on
In September 2001, shortly before the planned
27 July, aged 17.
operation, Mr H belatedly reviewed an MRI scantaken in April, which had been filed away. Thescan indicated a Syrinx (abnormal dilation of the
The complaint to the Trusts
central canal of the spinal cord). The surgery tocorrect that took priority over the scoliosis
In August 2003 Mr R asked both Trusts to review
surgery, and was carried out at Cambridge in
Q's treatment to find out what had contributed
April 2002. The procedure markedly decreased
to his son's death. He also raised concerns,
Q's neck mobility. It was noted that Q's parents
including the management of Q's scoliosis and his
preferred the scoliosis care to be continued at
care in the ICU. Hinchingbrooke's report to Mr R
Cambridge, but Mr M had no access to
contained explanations from the clinicians
appropriate beds there.
concerned. It concluded that Q's ‘untimely death
was not the result of a single or even several
Mr H and Mr M carried out the scoliosis surgery
specific incidences of carelessness, neglect or
at Hinchingbrooke on 17 June 2003. Before the
inadequate care'. Cambridge apologised for the
operation, the Consultant Anaesthetist at
failure to either forward Q's MRI scan results to
Hinchingbrooke (Dr Y) discussed with Dr P – the
Hinchingbrooke or for them to have been read
Consultant Anaesthetist and Intensive Care Unit
and acted upon at Cambridge. Mr R's subsequent
26 Remedy in the NHS June 2008
request for an Independent Review was refused by In considering Mr R's complaints, we soughtthe Convener, despite a Consultant Anaesthetist's
advice from a Consultant Orthopaedic Surgeon, a
report identifying shortcomings in Q's care and
Consultant Orthopaedic and Spinal Surgeon, a
treatment in the ICU. Mr R complained to the
Consultant in Paediatric Intensive Care, a
Ombudsman in December 2004.
Consultant Anaesthetist and a Nurse Consultantin Critical Care. We also considered evidenceprovided by Mr and Mrs R at interview and in
What we investigated
writing, the documents relating to the Trusts'response to Mr R's original complaint, relevant
In terms of the assessment and management of
clinical records, and the testimony of Mr M and
Q's scoliosis we investigated the fol owing
Mr H. We also discussed the management of Q's
anaesthesia and post-operative care with Dr Yand Dr P. We gathered information from the
• the nature of the scoliosis was not adequately
Trusts about planned changes to the Clinic and
took account of the ‘British Scoliosis SocietyGuide to Practice' (2001).
• investigations were not undertaken with
sufficient promptness and regularity;
What our investigation found
• there was a delay in reviewing the MRI scan;
Assessment and management of the scoliosis
• Q was not prioritised appropriately;
There should have been a paediatric assessmentfor Q because of the length of time since
• there was no reassessment about where the
his previous assessment (in 1995). Mr H now
scoliosis surgery should take place; and
ensures that al younger patients go for paediatric assessment.
• whether the organisation of the Clinic had any
detrimental effect on Q's assessment and
It was not common practice in 2000 to request an
surgical treatment.
MRI scan of a scoliosis patient until surgery wasclearly indicated, unless there were additional
On Q's post-operative care and treatment we
factors. In Q's case there were no abnormal
signs and surgery was not indicated untilDecember 2000. Although it would have been
• the management of ventilation and
best practice to order regular X-rays every six
months, the length of time between X-rays(December 2000 and September 2001) was
• the MRSA infection; and
not unreasonable.
• the standard of nursing care.
Clinicians must take responsibility for ensuringthat test results are reviewed; in this case there
We also investigated the Trusts'
was a failure to review an MRI scan promptly.
complaint handling.
Remedy in the NHS June 2008
Mr H was limited to six sessions a year to
undertake scoliosis surgery requiring two
The Trusts' responses to Mr R's original
surgeons and was faced with conflicting demands
complaints were inadequate and did not answer
from his patients. Problems with waiting times
his questions. Neither Chief Executive explained
and prioritisation for scoliosis patients were not
about the arrangements at the Clinic which led to
uncommon in 2000-01; therefore it was
some patients entering a different care pathway
unreasonable to hold Mr H individual y
from other patients with similar clinical needs.
responsible for the pressures on the service.
Hinchingbrooke's response to Mr R's complaintwas effectively provided by the clinicians
Because of his rigid neck and the degree of spinal
concerned, and their failure to thoroughly review
curvature, Q would have benefited had a
the factors which contributed to Q's unexpected
multi-disciplinary pre-operative discussion taken
death was unacceptable. We were highly critical
place in order to assess the risks of the
of the decision to refuse Mr R's request for an
anaesthesia and the most appropriate site for
Independent Review. While the ICU team
scoliosis surgery.
undertook a clinical review of Q's death,Hinchingbrooke did not take the opportunity to
The combined Clinic arrangements did not
analyse the failings which contributed to the
provide the necessary infrastructure to support
problems with Q's care and treatment and to
al scoliosis patients referred to it. Adolescent
learn lessons.
scoliosis patients entering the Hinchingbrooke‘stream', such as Q, were disadvantaged because
We upheld most aspects of Mr R's complaints.
they did not access the advice and support of
Individual and organisational failings resulted in
paediatric anaesthetists and paediatric intensive
the assessment and management of Q's scoliosis
care staff that was available to Mr M's patients.
fal ing below a reasonable standard. Althoughthese shortcomings were unlikely to have
Post-operative care and treatment
impacted on the correction of the scoliosis, they
The management of Q's post-operative
led to unnecessary delays and increased
ventilation was poor and, in al likelihood, had
discomfort and distress for Q. The organisation of
contributed to the damage to his lungs. The
the combined Clinic had a detrimental effect on
ventilatory parameters used immediately after
Q's assessment and surgical treatment, as Mr H's
surgery were too high for a patient of Q's age and
patients did not have the benefit of the
build, and the ventilation strategy used was not
multi-disciplinary support and assessment
consistent with accepted practice in 2003. The
available to Mr M's patients. There were avoidable
management of Q's fluid balance was deficient
factors which led to the development of ARDS
and the excessive fluid transfusion contributed to
and Q's subsequent death. Mr and Mrs R had a
the rapid onset of ARDS. We were satisfied that
right to expect a thorough, joint investigation of
MRSA did not contribute to Q's deterioration
the arrangements at the Clinic fol owing the
and we found no deficiencies in the nursing
devastating loss of their child, but the Trusts'
responses to their complaints and concerns were inadequate.
28 Remedy in the NHS June 2008
Our recommendations to Cambridge includedthat they:
We made 14 recommendations aimed at bringingabout systemic improvements to services for
• provide evidence that the arrangements for
adolescents with scoliosis, and assisting both
the transfer of the results of investigations,
Trusts in addressing the very serious issues raised
correspondence and other records for Mr H's
by our investigation. Al our recommendations
patients from the Clinic to Hinchingbrooke
Both Trusts agreed that:
In addition, both Trusts agreed to address thearrangements for pre-operative cardiopulmonary
• each Chief Executive would send a letter of
apology to Mr and Mrs R for the shortcomingsidentified and the failure to investigate theirson's death adequately; and provide them withdetails of the action taken in response to ourrecommendations and of the changes to theSpinal Deformity Service.
Among the recommendations we made toHinchingbrooke were that they:
• revise their management of ventilation and
fluids in intensive care and their managementof intra-operative fluid balance during anymajor operation with risk of significant bloodloss or prolonged surgery. In doing so, werecommended that they revisit the publishedresearch and rewrite their guidelines in linewith current knowledge and expert opinionfrom the local Network and the Royal Col egeof Anaesthetists; and
• ensure that the Chief Executive and the
Medical Director receive assurance thatcurrent anaesthetic and ICU practice is safeand that they consider the further stepsneeded to understand the factors thatcontributed to Q's death.
Remedy in the NHS June 2008
Complaint about Cambridgeshire and Peterborough Mental
Health Partnership NHS Trust (the Trust) and the Healthcare
Commission (the Commission)
Complaint about a decision to withdraw an
a private arrangement, largely by neighbours.
anti-dementia drug, Aricept, from an elderly
Mr S had been recently widowed, but he had two
patient, about the care and treatment
adult sons who monitored his situation closely. In
provided to him subsequently, and about
March 2004 Mr S's condition had deteriorated
the Commission's review
and he was admitted to hospital. Mr S remainedan in-patient until September 2004 when he wasdischarged to a nursing home.
Background to the complaint
Mr S was referred to the Trust by his GP in
The complaint to the Trust and the Commission
May 2002 because of poor memory and was seenby a Consultant Psychiatrist for Older People in
In July and August 2004 Mr S's son, Mr T,
June 2002. It was thought that Mr S had mild
complained to the Trust about a number of issues
cognitive impairment but that dementia might be
relating to Mr S's care including: the failure to
developing and an anti-dementia drug, Exelon,
inform Mr S's family and those caring for him
was prescribed. In July 2002 Exelon (which had
about the stopping of Aricept; the lack of a care
made Mr S unwel ) was replaced with a
plan fol owing that; and the fact that Mr S's
prescription for Aricept. Mr S attended further
condition had been al owed to deteriorate. The
appointments in September and November 2002.
Trust replied in September 2004 and provided a
At that stage it was intended that he would
number of explanations as wel as several
continue taking Aricept and that his mental
apologies relating to communication with Mr T
state would be assessed by a Community
and the provision of information to him.
Psychiatric Nurse.
Mr T complained to the Commission in
By May 2003 Mr S's GP considered that his mental
October 2004. In November 2005 the
state had deteriorated and asked for him to be
Commission told Mr T of its decision to refer
reassessed. When Mr S was reassessed in July and
matters back to the Trust to provide details
November 2003 it was noted that his memory
about the guidelines used to discontinue Aricept.
was continuing to deteriorate, that he wouldcontinue to be monitored and that the
In December 2005 Mr T complained to the
Community Psychiatric Nurse would keep in
Ombudsman. However, as the Commission had
touch with his carers to discuss any concerns.
not sought independent clinical advice, werecommended that it look at the complaint again.
In January 2004 Mr S was seen by a Staff Grade
The Commission sent its revised decision to Mr T
Psychiatrist for Older People, with the result that
in February 2006 advising that the clinical care
the Aricept was stopped and Mr S was discharged
given to Mr S was appropriate, that guidelines had
to the care of the Community Mental Health
been fol owed but that the Trust could have
Team. At this time Mr S was living in his own
provided more information to Mr T.
home and his day-to-day care was provided under
30 Remedy in the NHS June 2008
What we investigated
What our investigation found
In March 2006 Mr T complained to the
Our investigation found that the Trust failed to
Ombudsman. Our investigation covered the
communicate significant changes in Mr S's
fol owing concerns:
treatment plan (that is, the withdrawal of Aricept)to those most closely involved in his care.
• the Trust withdrew Aricept from Mr S in
January 2004 without informing Mr T, his
We found that the Trust did not identify and plan
carers, or the local social services department;
for the risk of Mr S's deterioration fol owing thedecision to discontinue Aricept and also failed to
• fol owing the decision to withdraw Aricept no
ensure that Mr S was adequately monitored after
care plan was devised and implemented, and
the Trust failed to monitor Mr S to avoiddeterioration;
We found that there would have been no benefitin re-prescribing Aricept to Mr S, even though
• Aricept was not re-prescribed to Mr S despite
this was recommended by a member of the
the opinion of a member of Trust staff that it
should be, and despite Mr T's repeatedrequests;
We found no documented evidence of anyconsideration of Mr S's individual circumstances in
• the Trust applied the National Institute of
the application of the NICE guidelines.
Clinical Excel ence (NICE) guidelines strictlyand without thought or consideration for
We found that Mr S was given the opportunity of
Mr S's individual circumstances;
review by an alternative Consultant Psychiatristfor Older People.
• the Trust denied Mr T's request for a change of
consultant for his father;
We found that the Commission did not takesteps to understand Mr T's complaint ful y;
• the Commission's handling of Mr T's complaint
failed on two occasions to take independent
was inadequate.
medical advice from an appropriately qualifiedperson with the necessary expertise; did not
We examined al relevant documentation
provide Mr T with an adequate explanation
concerning the case, including complaint
for its decision; and failed to respond in a
correspondence, Mr S's medical records, and the
Commission's papers. We also obtained clinicaladvice from an experienced Consultant
Our investigation concluded in March 2007
Psychiatrist. We also took into account the
and partly upheld the complaint against the
relevant NICE guidelines in place at the time,
Trust and ful y upheld the complaint against
‘Technology Appraisal Guidance No 19: Guidance
the Commission.
on the Use of Donepezil [Aricept], Rivastigmineand Galantamine for the Treatment ofAlzheimer's Disease'.
Remedy in the NHS June 2008

As a result of the recommendations made in ourfinal report the Trust also agreed to:
The Trust had, before our investigation concludedin March 2007, already taken some action in
• apologise to Mr T and provide him with
response to Mr T's complaints including:
evidence that senior medical staff have been
apologising for the lack of communication over
reminded of the importance of careful
the withdrawal of Aricept; revising their care plan
monitoring and fol ow-up of patients where
approach which includes the identification and
medication is discontinued; and
management of risk; undertaking to remind seniorstaff of the need for monitoring and fol ow-up
• conduct an audit of consensus meeting
where medication is discontinued; and a
documentation (to ensure that this format is
structured format for consensus meetings (which
used and that the requisite level of
should result in proper recording of the
information is recorded).
decision-making process and factors taken intoaccount when medication is discontinued).
The Commission agreed to apologise for thefailings identified in our report.
32 Remedy in the NHS June 2008
Complaint about Berkshire Healthcare NHS Trust (the Trust)
Remedy for poor treatment of an adolescent girl
her GP to refer Miss G to the private clinic.
suffering from anorexia nervosa
Mrs G took out a loan of £45,000 to pay for thetreatment. Al the other patients at the clinicwere said to be NHS-funded. Miss G put on
Background to the complaint
weight and was discharged in December.
Miss G was 15 years old when she was referred tothe Berkshire Adolescent Unit (the Unit), because
Complaint to the Trust
of weight loss and self-induced vomiting, inNovember 2002. She was assessed at the Unit in
Mrs G complained to the Trust in August 2003
January 2003, and admitted to a re-feeding
and received the Chief Executive's response in
programme in February. Miss G used laxatives and
November. Amongst other things, the letter said
diuretics and made herself sick in order to lose
that the matter of Miss G having absconded
any weight gained. She left the programme in
would be fol owed up in the Unit. Mrs G was
March, and a week later took an overdose, having
dissatisfied with the response and approached
felt guilty about eating something at a barbeque.
the Independent Complaints Advocacy Servicefor help. They referred her complaint to the
In May 2003 Miss G was readmitted to the
Ombudsman in May 2004.
programme, but continued to lose weight. On14 May the Consultant Psychiatrist, Dr Z, metMiss G for the first time. Because of Miss G's
What we investigated
poor progress at the Unit, her mother askedabout a transfer to a specialist unit within the
We investigated Mrs G's al egations that the Unit
NHS or to the private sector. Fol owing this
had not provided adequate care for Miss G; that
meeting Miss G attended the Unit as an in-
there were failings in the care provided by the
patient on weekdays, but she stil felt distressed if Unit, in that she was able to abscond from there;she put on weight.
and that Miss G was not seen personal y by theConsultant Psychiatrist until May 2003. Mrs G told
Miss G absconded from the Unit four times in
us that she did not want any other family to have
June 2003. On the first occasion she telephoned
the same experience. She had sought help from
her mother to let her know that she had left the
the private sector, when she thought her
Unit; Unit staff were unaware that she had gone.
daughter's life was in danger, and wanted to be
Miss G took another overdose in July, fol owing
reimbursed for the loan.
which Mrs G asked Dr Z if her daughter could betransferred to a named private clinic (which
A Consultant and Professor of Adolescent
specialised in treating anorexia nervosa in children
Psychiatry and two Psychiatric Nursing Assessors
and adolescents) as an NHS patient because she
provided us with advice on clinical issues and
felt that her daughter had deteriorated. In
nursing matters.
mid-July, at a time when Miss G was in a poorstate, Dr Z and others who might have advised
As the National Institute for Clinical Excel ence
Mrs G about her daughter's ongoing care were al
(NICE) did not issue its guidelines about eating
on leave. Feeling she had no alternative, she asked
disorders in adolescents until 2004, we relied on
Remedy in the NHS June 2008
our clinical advisers to indicate the care standards
not offered other choices, nor given a clear sense
that Miss G and her family could reasonably have
of direction when al local options seemed to be
expected in 2003. We were advised that the
ineffective, inappropriate or unavailable.
response to treatment of young people withanorexia nervosa is very variable and tends to be
Although the Chief Executive told Mrs G in
poor when laxative and diuretic misuse and
November 2003 that the issue of Miss G having
self-harm are involved. Some aspects of progress
absconded would be fol owed up in the Unit, the
would be expected within six months, however,
letter was dated some five months fol owing the
and it would be of concern if none of these were
event. It was not apparent that an urgent
apparent. These include some engagement with
investigation had been carried out immediately
treatment aims and development of good
fol owing Miss G's undetected absence.
relationships with one or two key staff; and somecontainment of the young person's maladaptive
The gap between Miss G's admittance to the Unit
eating and associated non-eating behaviours.
and being seen by Dr Z was unacceptable, givenher clear lack of progress, a moderate to high
We expected the Unit to have policies on
level of risk and high parental concern.
observation and assessment, and an approach tothe planning of care consistent with the Care
We concluded our investigation in
Programme Approach (CPA). Further guidance was
November 2007, and upheld Mrs G's complaint.
set out in ‘Modernising the Care Programme
The service failures described above, together
Approach', issued by the Department of Health in
with the fact that she was left without any clear
1999, which noted that risk assessment and
guidance about when a decision might be made
management are integral components of CPA,
about referring Miss G elsewhere left Mrs G
and that contingency planning should be an
fearing for her daughter's life.
element of risk management as a means ofpreventing and responding to crises.
Arrangements for handling crises are expected to
be included in care plans.
The Trust agreed to apologise to Mrs G for theirfailures and for the distress caused to her, and to
What our investigation found
pay her compensation of £500; to reimburse Mr and Mrs G the ful cost of the private
We found that the Unit had no adequate systems
treatment and to pay the interest on the loan;
in place for care planning, communication, risk
to ensure that they have a clear policy on
assessment and risk management to provide
out-of-area treatment that can be shared with
Miss G and her parents with a sense of
parents and patients; and to implement the NICE
engagement and containment, nor did it give
Clinical Guideline 9 (‘Eating disorders – Core
them a clear sense of direction about Miss G's
interventions in the treatment and management
care. She lost weight and her health and safety
of anorexia nervosa, bulimia nervosa and related
were compromised by a lack of effective
eating disorders').
arrangements to manage the risk that herbehaviour presented. Miss G and her parents were
34 Remedy in the NHS June 2008
Complaint about Peterborough and Stamford Hospitals NHS
Foundation Trust (the Trust) and the Healthcare Commission
Complaint about a decision to discharge from
acknowledged by the Trust in their discharge
hospital an elderly vulnerable patient, who died
letter and said that the Trust were being asked to
shortly after readmission, and complaint about
explain what action they had taken on that point.
the Commission's review.
In December 2005 the Trust sent a furtherresponse to Mr F. They apologised for any distress
Background to the complaint
caused and explained that they were trialing anelectronic discharge letter. They said also that a
Mr E, aged 88 years, went to live in a nursing
letter used for inter-hospital transfers was being
home in September 2004. He suffered with
extended to transfers to nursing homes in
severe dementia. In January 2005 he was admitted
complex cases and that the importance of
to Peterborough District Hospital with signs of
providing complete and legible information in
internal bleeding and a chest infection, and,
discharge letters was being emphasised in training
17 days later he was discharged back to the
and in staff meetings.
nursing home. Three days later he was readmittedto the hospital where he died at the beginning
In December 2005 Mr F complained to the
of February.
Ombudsman but as the Commission had notsought independent clinical advice during itsreview it was asked to look at the complaint
The complaint to the Trust and the Commission
again. In February 2006 the Commission sent itsrevised decision to Mr F and said that, having
Mr E's son, Mr F, complained to the Trust in
taken clinical advice, it took the view that
February 2005. He raised concerns about the
the Trust's documented actions, including the
discharge decision and its planning, and their
recommended fol ow-up actions, appeared
communication with the nursing home and
The Trust replied in March 2005 that Mr E had
What we investigated
been properly assessed and discharged safely.
They apologised for the fact that the Ward
In March 2006 Mr F complained to the
Manager had failed to inform the nursing home
Ombudsman. The investigation covered the
that Mr E was no longer diabetic and for a lack of
fol owing concerns:
information in the discharge letter to Mr E's GP.
• the Trust should not have discharged Mr E
Mr F remained dissatisfied and in June 2005 the
from hospital in January 2005;
Commission confirmed that it would look at hiscomplaint. The Commission then looked at Mr F's
• the Trust did not discharge Mr E with a care
complaint and replied in November 2005. It
plan. Instead, the hospital left it to the staff at
referred to a breakdown in communication
the nursing home to devise a care plan but did
between the hospital and the nursing home but
not provide them with sufficient information
said it was not apparent that this was the fault of
with which to write one;
the Trust's nursing staff. It referred to the gaps
Remedy in the NHS June 2008
• neither the nursing home nor Mr E's GP was
they apologised for the fact that Mr E was
properly informed about his condition and
discharged without more investigation into his
treatment on discharge from hospital. Proper
procedures for the discharge of vulnerablepatients were not fol owed;
We found that the Trust were under noobligation to discharge Mr E with a care plan.
• the Trust refused to provide the nursing home
with information about Mr E's condition;
We found that the Trust's discharge letter wasinadequate, that the use of a telephone cal from
• the Commission's handling of Mr F's complaint
the Trust to the nursing home to provide
was inadequate.
additional information was not an appropriateway to handle this complex discharge and that
We examined al relevant documentation
good practice would have involved a higher level
including complaint correspondence, copies of
of pre-discharge liaison with the nursing home.
Mr E's medical records and the Commission'spapers. We also obtained advice from a
We did not find any evidence to support the
geriatrician and from a nurse with significant
complaint that the Trust refused to provide the
experience of older people's care.
nursing home with information about Mr E.
We took account of the prevailing standard
We found that the Commission's handling of
which in this case was the Department of
Mr F's complaint was inadequate as it failed to
Health's ‘Discharge from hospital: pathway,
obtain independent clinical advice from an
process and practice' (2003).
appropriately qualified person with the necessaryexpertise and did not give an adequateexplanation for its decision.
What our investigation found
Our investigation concluded in March 2007 and
We did not find evidence to support the Trust's
we partly upheld Mr F's complaint against the
decision that Mr E was ready to be discharged
Trust and ful y upheld his complaint against
from hospital. This is not to say that, had he
the Commission.
remained in hospital, the outcome for Mr E wouldhave been any different. Rather, the Trust shouldhave carried out a more thorough assessment of
his needs at that time and of the ability of thenursing home to care for him. Because the acute
The Trust agreed to review their documentation
il nesses that Mr E was suffering from had
on pre-discharge planning and their procedures to
improved and his vital signs were within normal
ensure compliance with Department of Health
limits, it was assumed that Mr E was fit for
guidance on the proper discharge of complex
discharge. Instead, the totality of relevant factors
elderly patients.
should have been considered. The Trust agreedthat Mr E should have remained in hospital until a
The Commission agreed to apologise to Mr F for
ful assessment was made before discharge and
the shortcomings identified in our report.
36 Remedy in the NHS June 2008
Complaint about Dr Mrozinski, a locum GP
Complaint that a GP unreasonably prescribed
The complaint to Trafford North/South Primary
amoxicil in to a patient recorded as being al ergic
Care Trust (the Trust) and the Healthcare
to penicil in, and mishandled the patient's
Commission (the Commission)
subsequent complaint
On 28 June 2004 Mrs K complained to the Trust,asking for an apology and compensation for her
Background to the complaint
ruined honeymoon and the distress Dr Mrozinskihad caused her. After Dr Mrozinski failed to
Mrs K's history of penicil in al ergy, based on her
attend a local resolution meeting arranged by
account of a previous reaction, was marked on
Mrs K's GP, she told the Trust that she wanted a
her medical summary card, on her Lloyd George
ful written response to her complaint from
(paper) folder and on her computer records.
Dr Mrozinski. His eventual reply did not provide
On 3 June 2004, shortly before her honeymoon
an account of his actions nor explain why he had
in Mexico, Mrs K had an appointment for
prescribed antibiotics. He said that if Mrs K was
vaccinations at the surgery. The Nurse was
questioning his clinical competence or claiming
concerned about vaccinating Mrs K, who was
gross professional misconduct she should contact
congested, and arranged for her to see
the General Medical Council (GMC). If she was
Dr Mrozinski. By Mrs K's account Dr Mrozinski
claiming medical negligence she should expect a
asked her if she was al ergic to antibiotics, to
possible counterclaim. The Trust made several
which she replied: not that she was aware of.
attempts to engage Dr Mrozinski in the
(Mrs K was aware of her penicil in al ergy but did
complaints process, and reminded him of his
not associate antibiotics with penicil in.)
responsibilities under the GMC guidance and
Dr Mrozinski prescribed a five-day course of
NHS Complaints Procedure. When no substantive
amoxicil in, an antibiotic of the penicil in family.
response was forthcoming, Mrs K took hercomplaint to the Commission, which began
Mrs K flew to Mexico on 9 June 2004. The next
an investigation.
day a rash appeared on her back and arms. Herbody became red, swol en and hard to the touch,
The Case Manager visited the surgery, where
covered in lumps and blisters. She assumed she
Mrs K's GP demonstrated the warning notice
had been prescribed penicil in. Mrs K spent the
displayed on the computer when an attempt was
last days of her holiday in her hotel room, and
made to prescribe a drug to a patient with a
she described the flight home as ‘painful and
recorded sensitivity or al ergy. It was noted that
frightening'. She immediately saw her regular GP,
the warning could be manual y overridden. The
who told her that Dr Mrozinski had written on
GP pointed out Dr Mrozinski's computer entry,
her notes that he had asked her if she was al ergic
prescribing amoxicil in for Mrs K. The Commission
to penicil in, to which she had answered that
wrote to Dr Mrozinski three times asking for a
she was not. Mrs K disputed that account of
response to Mrs K's complaint, but received no
the consultation.
reply. With Mrs K's agreement the Commissionreferred her complaint direct to the Ombudsmanin April 2005, as we have powers to obtainevidence from witnesses.
Remedy in the NHS June 2008
What we investigated
Dr Mrozinski's initial response to Mrs K'scomplaint was unhelpful, negative and bel igerent
We investigated whether Dr Mrozinski had
in tone, and his threat of a counterclaim did not
unreasonably prescribed amoxicil in to Mrs K and
comply with NHS complaints regulations and
whether he had appropriately handled her
GMC guidance. It was only after we contacted
complaint about that. We took account of the
Dr Mrozinski about Mrs K's complaint, that he
GMC's 2001 publication, ‘Good Medical Practice',
provided a response to the substance of it, but
which stated that clinicians must explain ful y and
there was no explanation of why he had not
promptly what has happened if harm has been
provided an earlier explanation and no apology.
suffered. It also stated they should appropriately
Dr Mrozinski's refusal before then to explain his
apologise and that patients who complain about
actions showed a blatant disregard of GMC
care or treatment they have received have a right
guidance and the NHS Complaints Procedure.
to a prompt, open, constructive and honestresponse. We also bore in mind the NHS
We concluded our investigation in
Executive's Guidance on the NHS Complaints
September 2006 and upheld Mrs K's complaints.
Procedure for General Practices which reminds
Although it was not clear that she had suffered as
GPs of the need to ‘listen careful y and
a result of Dr Mrozinski's prescription, he should
understand the person's perspective
not have prescribed antibiotics without further
discussion, and should have told her that it wasrecorded that she was al ergic to penicil in.
Dr Mrozinski's handling of Mrs K's complaint was
What our investigation found
total y unacceptable; his repeated refusal torespond to the substance of her complaint put
We concluded, on the basis of clinical advice
her to unnecessary time and trouble, and added
from the Ombudsman's GP Adviser, that it was
to her distress.
not certain that amoxicil in was the cause ofMrs K becoming unwel : although Mrs K was notaware of it, she had twice been prescribed
penicil in (in 1994) with no il effect.
We recommended that Dr Mrozinski send Mrs K a
Mrs K's penicil in al ergy was clearly recorded;
written apology and pay her £250 compensation
although Dr Mrozinski did not total y disregard
for the unnecessary distress he had caused her.
the need to check if she was al ergic before
He refused to do so and wrongly questioned the
writing a prescription, he should not have
Ombudsman's authority to investigate clinical
disregarded the al ergy warnings, or overridden a
matters. At our suggestion, the Trust made the
computer alert, without discussion with her. He
payment to Mrs K themselves, on the basis that
should also have recorded that Mrs K's
‘the patient is more important than the principle'.
understanding that she was not al ergic toantibiotics was inconsistent with her medicalrecords. There was conflicting evidence aboutwhat Dr Mrozinski had asked Mrs K during theconsultation, which could not be resolved.
38 Remedy in the NHS June 2008
Complaint about Gloucestershire Hospitals NHS Foundation
Trust (the Trust) and the Healthcare Commission
Complaint about the care and treatment of an
accuracy of the death certificate. Mrs J believed
elderly patient who died during an in-patient
that Mr W had been caused undue suffering and
admission, and complaint about the Commission's
stress during his admission and that their family
subsequent review
had been caused unnecessary distress.
Mrs J complained to the Trust in March 2003; they
Background to the complaint
responded in July 2003. A local resolution meetingwas held in August 2004. Mrs J was unhappy with
Mr W, aged 74, was admitted to Gloucester Royal
the action taken by the Trust and complained to
Infirmary as an emergency in August 2002 for
the Commission in October 2004.
treatment of an infective exacerbation(pneumonia) of chronic obstructive pulmonary
In November 2005 the Commission referred
disease. He was treated in the Intensive
some aspects of the complaint back to the Trust
Treatment Unit until the end of August when he
for action (requesting an update on
was transferred to a respiratory ward. Mr W then
improvements to record keeping and
had episodes of confusion, difficulty with oxygen
communications between staff and families) and
intake and some bleeding from a catheter site.
asked them to look at the timing of Mr W's
He later contracted MRSA, developed diarrhoea
transfer from the Intensive Treatment Unit. Mrs J
and was found to be infected with C.difficile.
complained, again, to the Commission in
Mr W was transferred to Standish Hospital at the
December 2005, which said, in May 2006, that it
start of October, where he suffered with
would take no further action as it was satisfied
recurrent C.difficile infection. Mr W died in
with the Trust's actions and responses.
November 2002, with the cause of death notedas respiratory failure.
What we investigated
The complaint to the Trust and the Commission
Mrs J asked us to investigate al aspects of hercomplaint against both the Trust and the
Mrs J, Mr W's daughter, questioned whether the
Trust's actions had contributed towards hisdeterioration and death. She had specific
We considered al the available evidence and took
concerns about the care and treatment that he
clinical advice from an experienced General
had received, including: his transfer from the
Physician (who is also a Consultant in Elderly Care
Intensive Treatment Unit; the timing of medical
Medicine) and an experienced Nurse. We also
reviews fol owing that transfer; the general
took account of the relevant standards and
standard of hygiene and nursing care (Mr W had
guidelines including the Department of Health's
been found by his family with bloodstained
National Service Framework for Older People
pyjamas and bedclothes and there was a delay in
(2001), the British Society of Geriatrics' ‘Standards
providing continence pads when he suffered from
of Medical Care for Older People' (revised 2003),
diarrhoea); effectiveness of communication (both
the Nursing & Midwifery Council's ‘Standards for
between staff members and with the family); the
Records and Record Keeping', the NHS
management of MRSA and C.difficile and the
Modernisation Agency's benchmarking tool
Remedy in the NHS June 2008
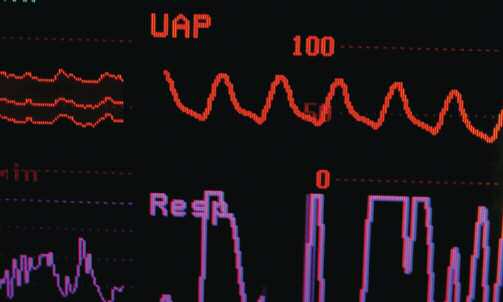
‘Essence of Care' and the March 2001 guidance
• a lack of monitoring while Mr W waited to be
about resuscitation decisions published jointly by
transferred from the Intensive Treatment Unit;
the British Medical Association, Royal Col ege ofNursing and the Resuscitation Council.
• a delay in carrying out a medical review;
• extremely poor nursing care in relation to care
What our investigation found
planning, communication, pain management,infection management, patient privacy and
We found that the timing of Mr W's discharge
dignity, and monitoring fluid intake/output;
from the Intensive Treatment Unit wasappropriate; that the medical care in late
• a lack of multi-professional working and senior
August/early September 2002 was general y
reasonable; that there was no objective evidenceof MRSA being implicated in Mr W's death; that
• poor record keeping; and
the medical management of C.difficile wasappropriate; and that the Trust's response on the
• poor end-of-life care (including lack of a
accuracy of the death certificate was reasonable.
care plan and no discussion with the family
However, when taken in the round, the evidence
about resuscitation and the seriousness of
we saw pointed to serious failings in the Trust's
Mr W's prognosis).
service to Mr W and his family which were:
40 Remedy in the NHS June 2008
We concluded that, irrespective of the poor
practice identified, the final outcome for Mr Wwould not have been different, but that the
In this case we decided to involve Monitor, the
failings identified would have significantly
body which authorises and regulates NHS
affected Mr W's quality of life and the level of
Foundation Trusts, because we were highly critical
distress he suffered. We also found that Mr W's
of the nursing care at the Trust and were keen to
family were caused undue distress due to the
ensure that there was an appropriate review of
condition in which they sometimes found Mr W
the Trust's progress in learning lessons from the
and because they had no opportunity to come to
terms with the fact that his life was ending and tomake suitable arrangements.
The Trust agreed to:
We acknowledged the time and effort the Trust
• write to Mrs J and her family to acknowledge
took in attempting to resolve Mrs J's concerns
and apologise for the failings identified;
and that they readily acknowledged severalfailings and took action to address them.
• review the areas where we had identified
However, we concluded that Mrs J's complaint
serious failings in order to ensure that their
should have prompted a wider review of nursing
practices were in accordance with current
care which may have led to a more co-ordinated
guidance and standards;
approach to implementing improvements and, inturn, provided reassurance for Mrs J that her
• provide Monitor with information to
complaint was being taken seriously.
demonstrate that their practices (in the areaswhere we had identified serious failings) are in
We found maladministration in the Commission's
line with current standards; and
handling of Mrs J's complaint (including failure to seek clinical advice, not providing her with
• report back to Mrs J on the action taken in
regular updates and failure to assess the priority
response to our recommendations.
of the case) which had exacerbated her worry and distress.
The Commission agreed to write to Mrs J and herfamily with an apology and pay £250
The investigation concluded in March 2008 and
compensation in recognition of the worry and
we upheld Mrs J's complaints against both the
distress caused by its poor complaint handling.
Trust and the Commission.
Remedy in the NHS June 2008
Printed in the UK by The Stationery Office Limited on behalf of the Control er of Her Majesty'sStationery Office
Printed on Paper containing 75% recycled fibrecontent minimum.
42 Remedy in the NHS June 2008
Switchboard: 020 7217 3000
Fax: 020 7217 4000
Email: phso.enquiries@
Please note
The telephone numbers of the Parliamentary and Health Service Ombudsman changed on 15 March 2009.
The new contact details are:
Helpline: 0345 015 4033
Fax: 0300 061 4000
Published by TSO (The Stationery Office) and available from:
Mail, Telephone Fax & E-Mail
TSO
PO Box 29 Norwich NR3 1GN
Telephone orders/General enquiries 0870 600 5522
Order through the Parliamentary Hotline Lo-Cal 0845 7 023474
Fax orders: 0870 600 5533
E-mail: [email protected]
Textphone: 0870 240 3701
TSO Shops
16 Arthur Street Belfast BT1 4GD
028 9023 8451 Fax 028 9023 5401
71 Lothian Road Edinburgh EH3 9AZ
0870 606 5566 Fax 0870 606 5588
The Parliamentary Bookshop
12 Bridge Street, Parliament Square London SW1A 2JX
TSO@Blackwel and other Accredited Agents
Source: http://www.ombudsman.org.uk/__data/assets/pdf_file/0005/1031/Remedy-in-the-NHS-recent-case-summaries.pdf
Lack of bystander activation shows that localization exterior tochromosome territories is not sufficient to up-regulate gene expression Céline Morey, Clémence Kress and Wendy A. Bickmore 2009 19: 1184-1194 originally published online April 23, 2009 Genome Res. This article cites 34 articles, 19 of which can be accessed free at: Receive free email alerts when new articles cite this article - sign up in the box at the
ednesday, April 10, 2013 American Conference 17.72. 10. Eric Agee-Floyd ATU 200 100 x 5:07.37. 2. Manuel Alvarez 2. Marcus Lindsey (NLR), 2. Aulexis Pippen (CRO), 26.74. 5. Makayla Daniel Spring Championships, Fullerton, both White Hall, Katie Slaughter and Brit- (LRC), 5:18.18. 3. Christo- 132-5. 3. Charlie Donerson 15.62. 3. Shadeanna Gatlin (NLR), 27.33. 6. Maryma