Prostatitis-forum.com

Vol. 169, 592–596, February 2003
HE JOURNAL OF UROLOGY
Printed in U.S.A.
Copyright 2003 by AMERICAN UROLOGICAL ASSOCIATION
TERAZOSIN THERAPY FOR CHRONIC PROSTATITIS/CHRONIC PELVIC
PAIN SYNDROME: A RANDOMIZED, PLACEBO CONTROLLED TRIAL
PHAIK YEONG CHEAH,* MEN LONG LIONG, KAH HAY YUEN, CHU LEONG TEH,
TIMOTHY KHOR, JIN RONG YANG, HIN WAI YAP AND JOHN N. KRIEGER†
From the School of Pharmaceutical Sciences, University of Science Malaysia, Department of Urology, Lam Wah Ee Hospital, Department
of Urology, Penang Adventist Hospital, Department of Urology, Gleneagles Medical Center, Department of Urology, Penang Hospital,
Department of Urology, Island Hospital, Penang, Malaysia, and the Department of Urological Surgery, University of Washington School
of Medicine, Seattle, Washington
Purpose: We evaluate terazosin therapy for chronic prostatitis/chronic pelvic pain syndrome.
Materials and Methods: The study included 100, 20 to-50-year-old subjects who met the
consensus criteria for chronic prostatitis/chronic pelvic pain syndrome and had not receivedprevious ␣-blockers. Subjects were randomized to receive terazosin with dose escalation from 1to 5 mg. daily or placebo for 14 weeks. The primary criterion for response was scoring 2 or less("delighted-to-mostly satisfied") on the National Institutes of Health Chronic Prostatitis Symp-tom Index (NIH-CPSI) quality of life item. The secondary criterion for response was greater than50% reduction in NIH-CPSI pain score at 14 weeks. Other outcomes included total and NIH-CPSIdomain scores, International Prostate Symptom Score, peak urinary flow rate, post-void residualurine and adverse effects.
Results: Using the primary criterion 24 of 43 evaluable subjects (56%) responded in the
terazosin group compared to 14 of 43 (36%) in the placebo group (p ⫽ 0.03). Using the secondarycriterion 26 of 43 subjects (60%) responded in the terazosin group compared to 16 of 43 (37%) inthe placebo group (p ⫽ 0.03). The terazosin group had greater reductions (p ⬍0.05) in NIH-CPSItotal score, individual domain scores and International Prostate Symptom Score than the placebogroup. There was no difference in peak urinary flow rate or post-void residual. In the terazosingroup 18 patients (42%) had side effects compared to 9 (21%) in the placebo group (p ⫽ 0.04).
Conclusions: Terazosin proved superior to placebo for patients with chronic prostatitis/chronic
pelvic pain syndrome who had not received ␣-blockers previously.
KEY WORDS: prostate, chronic disease, pelvic pain, prostatitis, drug therapy
Chronic prostatitis/chronic pelvic pain syndrome afflicts
reported a 3-arm crossover study with placebo, baclofen and
2% to 10% of men.1, 2 It decreases quality of life3 and causes
phenoxybenzamine, a nonselective ␣-blocker.7 This study
major economic losses.4 Despite its importance as a cause of
was difficult to interpret because it involved baclofen, a stri-
morbidity, there are only limited evidence based treatment
ated muscle relaxant, and there was no washout period
recommendations. No drug or surgical procedure has proven
among the treatment arms. Neal and Moon reported symp-
to have lasting benefits. During the last 30 years many
tomatic improvement with terazosin, a selective ␣-blocker,
treatments have been investigated in pilot studies, including
but it was difficult to discern the true treatment benefits
␣-blockers, antibiotics, nonsteroidal anti-inflammatory
from the natural history of chronic prostatitis in this open
agents, pentosan polysulfate, allopurinol, quercetine, finas-
label study.8 de la Rossette9 and Lacquaniti10 et al reported
teride, trice-weekly ejaculation, transurethral and "subtotal"
randomized, placebo controlled studies using selective
prostate resection, transurethral incision of the prostate, bal-
␣-blockers. de la Rossette et al studied only 25 patients,9
loon dilation, hyperthermia, transurethral needle ablation
while Lacquaniti et al did not specify their diagnostic crite-
and radical prostatectomy.5 This wide variety of treatments
ria.10 Despite these limitations, ␣-blockers are among the
clearly reflects patient and clinician frustrations.
most frequently prescribed drugs for chronic prostatitis. We
Because symptoms of chronic prostatitis/chronic pelvic
determine the effectiveness of terazosin therapy for patients
pain syndrome and benign prostatic hyperplasia (BPH) over-
who met the National Institutes of Health (NIH) consensus
lap somewhat, investigators hypothesized that drugs effec-
definition for chronic prostatitis/chronic pelvic pain syn-
tive for BPH might help some patients with chronic prostati-
drome in a randomized, placebo controlled study.
tis/chronic pelvic pain syndrome. Urodynamic studiessuggested that some patients have functional obstruction at
MATERIALS AND METHODS
the bladder neck or external urethral sphincter.6 Severalstudies demonstrated that ␣-blockers improved chronic pros-
Subject selection. Patients who met the clinical criteria for
tatitis/chronic pelvic pain syndrome symptoms. Osborn et al
chronic prostatitis/chronic pelvic pain syndrome11 were re-cruited during a prostatitis awareness campaign targeting a
Accepted for publication August 16, 2002.
diverse population in Northern Malaysia2 and from those
Supported by an unrestricted grant from Abbott Laboratories,
seeking treatment at participating hospitals. Eligibility re-
* Financial interest and/or other relationship with Abbott
quirements included age between 20 and 50 years, score of 1
or greater on items 1 and 2 (presence of pelvic pain and
† Requests for reprints: Department of Urological Surgery,
quality of life) and 4 or greater on item 9 ("mostly dissatis-
University of Washington School of Medicine, VA Puget Sound HealthCare System, 1660 S. Columbian Way, Seattle, Washington 98108.
fied," "unhappy" or "terrible") of the National Institutes of

TERAZOSIN FOR CHRONIC PROSTATITIS
Health Chronic Prostatitis Symptom Index (NIH-CPSI),12
tis/chronic pelvic pain syndrome or those that affect the lower
symptoms for 3 or greater months and a desire to be treated.
urinary tract function during the study. They were asked to
Potential subjects were excluded from study if they met cri-
report new medications at each clinic visit.
teria for chronic bacterial prostatitis after lower urinary tract
Outcomes. Because prostatitis is associated with substan-
localization studies,13 had previous urinary tract infection or
tial reduction in quality of life,3 the primary outcome meas-
a uropathogen documented within the last year, had signif-
ure was the NIH-CPSI quality of life item, and the primary
icant medical problems, had any NIH consensus exclusion
criterion for response was a score of 0 to 2 ("delighted" to
criteria,11 had been treated with ␣-blockers previously or
"mostly satisfied") at week 14 (compared to 4 to 6, "mostly
were taking medications that could affect lower urinary tract
dissatisfied" to "terrible" at baseline). Since all patients had
pelvic pain, the secondary criterion for response was a
Study design and procedures (fig. 1). The protocol adhered
greater than 50% reduction in the baseline NIH-CPSI pain
to the International Committee of Harmonization guidelines
domain score. Other outcomes included mean NIH-CPSI to-
for Good Clinical Practice and was approved by a Joint School
tal score and the individual domain scores, I-PSS, peak uri-
of Pharmaceutical Sciences, University of Science Malaysia-
nary flow rate and post-void residual between treatment
Penang Hospital Committee on Clinical Studies. Each sub-
groups. Also during each followup visit subjects were asked if
ject had a baseline NIH-CPSI score, International Prostate
they experienced any adverse effects.
Symptom Score (I-PSS),14 peak urinary flow rate and post-
The NIH-CPSI, a prostatitis specific symptom index devel-
void residual urine. In addition, prostate size was measured
oped and validated in North America,12 evaluates 3 domains
by ultrasound and serum prostate specific antigen (PSA) was
(pain, urinary and quality of life impact), and has been rec-
determined (normal range less than 4 ng./ml.).
ommended as an outcome measure in research trials.5 The
Subjects were assigned following a random number table
I-PSS, peak urinary flow rate and post-void residual were
to receive either terazosin or placebo. The terazosin dosage
analyzed because patients with chronic prostatitis/chronic
was 1 mg. for 4 days, 2 mg. for 10 days and 5 mg. for 12
pelvic pain syndrome often experience urinary tract symp-
weeks. Placebo tablets compounded from lactose had a sim-
toms that terazosin might ameliorate. The NIH-CPSI and
ilar appearance to terazosin tablets. Subjects were assessed
the I-PSS were translated into other major languages (Malay
for treatment outcomes at weeks 2, 6 and 14. Patients were
and Chinese) spoken by the local population with the accu-
not permitted to take other medications for chronic prostati-
racy verified by back translation into English as described
FIG. 1. Primary (NIH-CPSI quality of life item), secondary (NIH-CPSI pain domain) and other (NIH-CPSI urinary and quality of life
impact domains and total score, I-PSS, peak urinary flow rate, post-void residual and adverse effects) outcomes were measured at baselineand each followup visit. Placebo tablets had similar appearance to terazosin tablets at all dose levels.

TERAZOSIN FOR CHRONIC PROSTATITIS
previously.2 Peak urinary flow rate was measured using a
group was 1.5-fold greater than the 37% reduction in the
weight transducer flow meter with values considered evalu-
placebo group after 14 weeks (p ⫽ 0.01). Improvements in
able only if the voided volume was at least 150 ml. Post-void
NIH-CPSI pain, urinary and quality of life impact domains in
residual was measured by transabdominal ultrasound.
the terazosin group were each significantly greater (p ⬍0.05)
Statistical analyses. A sample size of 80 subjects (40 per
than those in the placebo group after 14 weeks.
arm) was powered for a difference of at least 30% between the
The terazosin group experienced a 62% reduction in mean
terazosin (p ⫽ 60%) and placebo groups (p ⫽ 30%) with a
I-PSS (12.1 ⫾ 9.8 at baseline to 4.6 ⫾ 6.0 at week 14) than the
95% CI (␣ ⫽ 0.05) and statistical power of 80% ( ⫽ 0.2).15
35% in the placebo group (14.1 ⫾ 2.3 at baseline to 9.1 ⫾ 3.9
Allowing for 20% dropout the enrollment goal was 100 sub-
at week 14, p ⫽ 0.03). There was no difference between the
groups in regard to peak urinary flow rate (terazosin 15.4 ⫾
Prostate size and PSA at baseline were compared using the
6.9 to 18.7 ⫾ 8.1 ml. per second in terazosin and placebo
Student t test, and for age the Mann-Whitney U statistic was
18.1 ⫾ 2.3 to 19.7 ⫾ 3.9 ml. per second). There was also no
calculated. Chi-square statistics were calculated to compare
difference in post-void residual (terazosin 24.8 ⫾ 25.6 to
racial distributions, duration of symptoms, as well as propor-
17.1 ⫾ 20.8 ml. and placebo 20.6 ⫾ 24.5 to 16.0 ⫾ 18.1 ml.).
tion of responders between treatment groups. Analysis of
In the terazosin group 18 of 43 (42%) patients complained
variance procedures for a 2-factorial, split-plot experimental
of side effects compared to 9 of 43 patients (21%) in the
design16 were used to evaluate outcome parameters between
placebo group (chi-square 4.4, df 1, p ⫽ 0.04). Side effects in
the treatment groups. Within group changes for each param-
the terazosin and placebo groups included dizziness (7 versus
eter were assessed using the extended Tukey test, and p
2 patients), asthenia (7 versus 3), postural hypotension (1
⬍0.05 was considered significant.
versus 0), palpitation (1 versus 2), flu syndrome (1 versus 0),drowsiness (2 versus 1), headache (2 versus 2) and rashes (0
versus 1). No patient withdrew from study because of sideeffects.
Demographics and clinical presentation. Between April 1,
Responders in the terazosin group had lower NIH-CPSI
2000 and September 30, 2001, 100 subjects were recruited for
pain scores at baseline (mean 10.5, SD 2.9) than nonre-
study. The terazosin and placebo groups were comparable at
sponders (mean 13.1, SD 3.5, p ⫽ 0.01). Malays were most
baseline in all variables assessed (tables 1 and 2). There were
likely to respond (78.6%) followed by Chinese (64.3%),
more subjects with a symptom duration of 3 to 6 months in
Indians (50.0%) and other races (11.1%) (chi square 10.7, df 3,
the terazosin group compared to the placebo group, while the
p ⫽ 0.01). Parameters that were not associated with response
reverse was true for symptom duration of 7 to 12 months and
included age, baseline urinary and quality of life impact
greater than 12 months. However this difference was not
domains, NIH total score, I-PSS, peak urinary flow rate,
statistically significant. The terazosin group also appeared to
post-void residual and symptom duration. In contrast, within
have higher mean NIH-CPSI domain and I-PSS scores com-
the placebo group there was no difference between respond-
pared to the placebo group but these differences were not
ers and nonresponders in any parameter assessed.
significant and were not reflected in the median scores. Ofthe 100 subjects 86 completed all followup assessments. Thedropout rate was 14% in both groups. Reasons for dropout
included "did not have time" (5 patients), "moved to another
Terazosin proved superior to placebo therapy for patients
town/country" (4) and "ineffective treatment" (2). We could
with chronic prostatitis/chronic pelvic pain syndrome who
not contact the 3 remaining subjects.
had a quality of life score of 4 or greater (mostly dissatisfied)
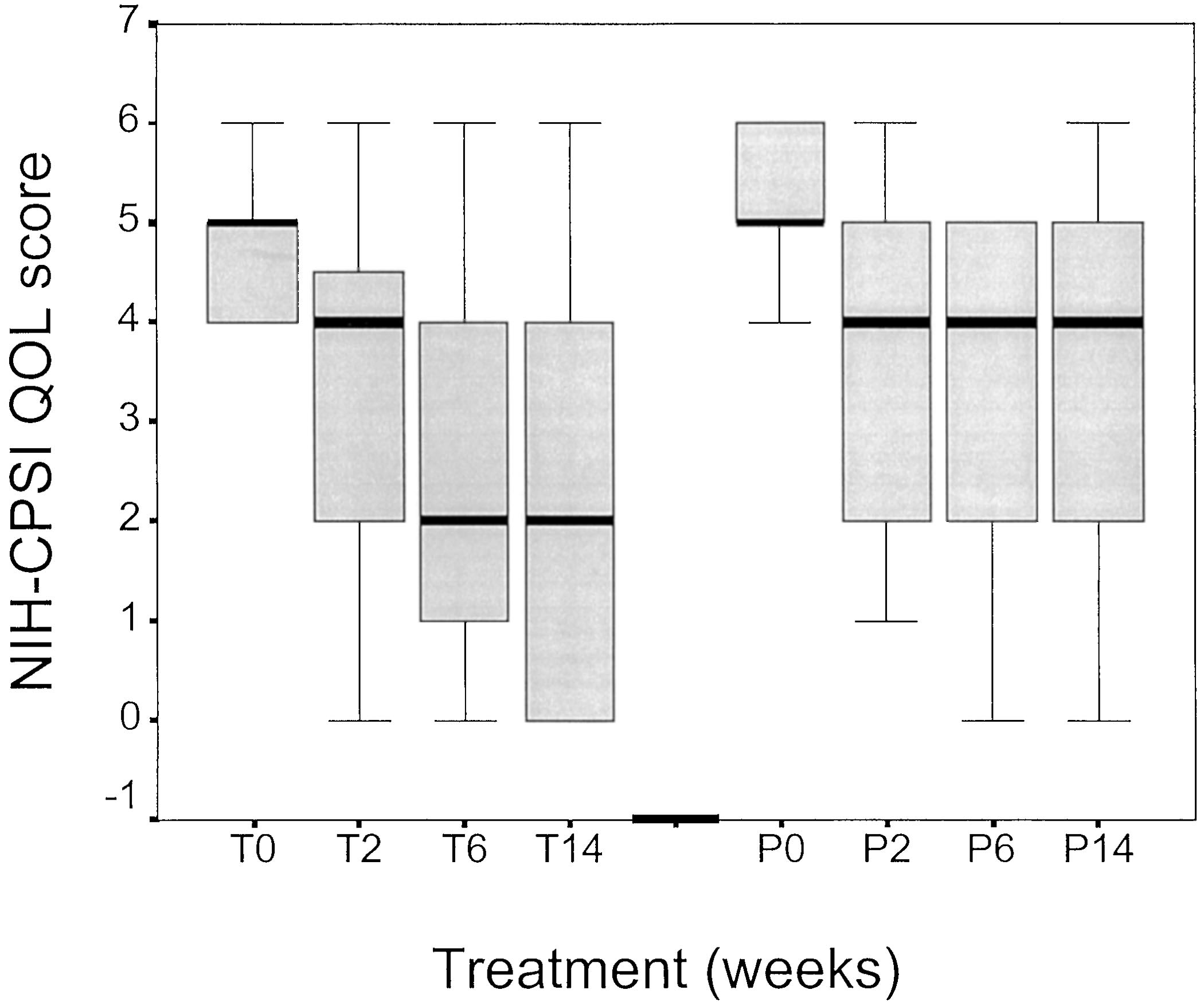
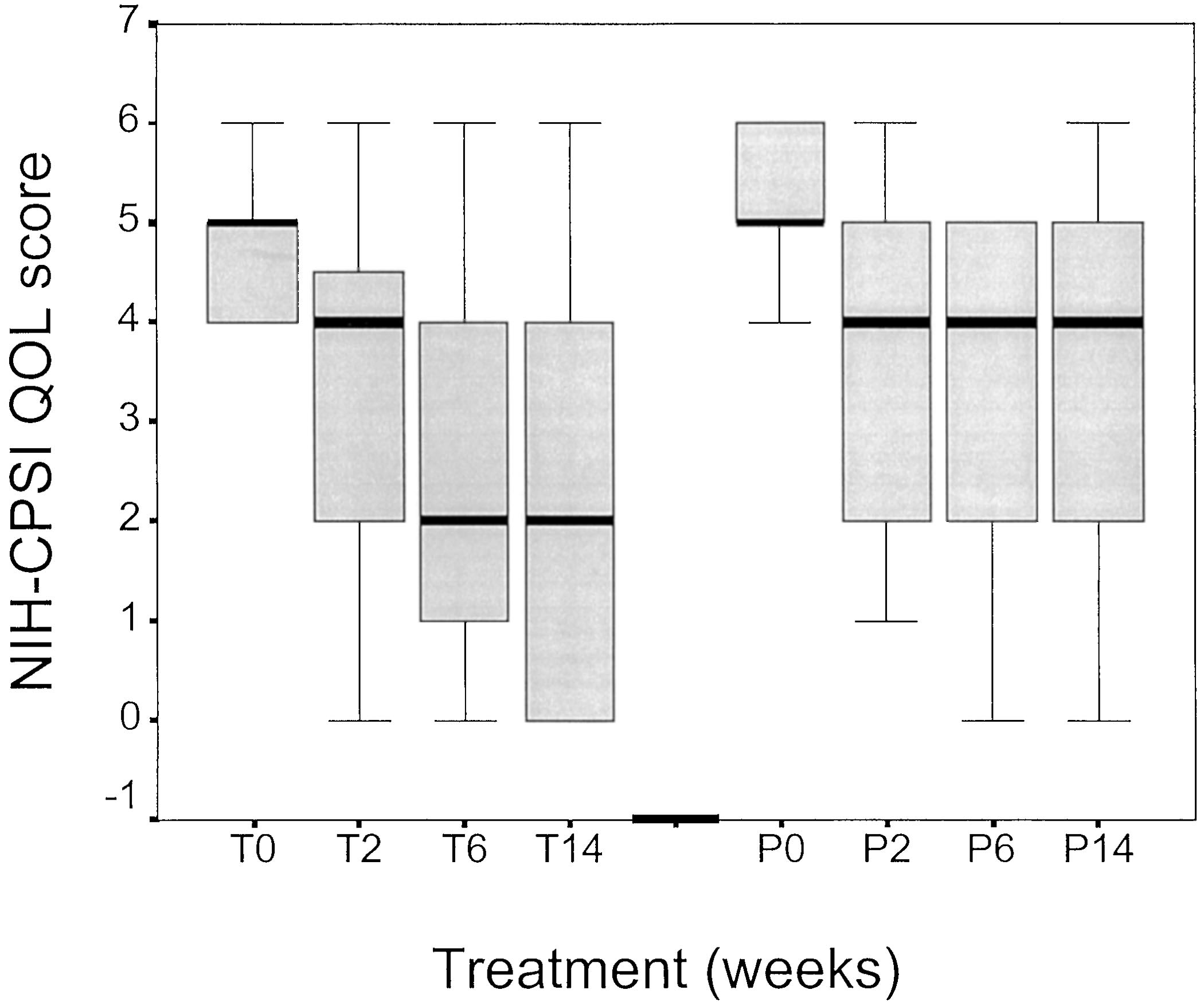
Efficacy. Figure 2 shows a box plot of the NIH-CPSI quality
and had not received previous treatment with ␣-blockers.
of life score for patients in the terazosin and placebo groups
Because prostatitis reduces quality of life substantially,3
at baseline and all followup visits. Median quality of life score
global quality of life assessment was selected as the primary
decreased to 2 in the terazosin group, and decreased to 4 and
outcome measure. After 14 weeks 56% of subjects in the
plateaued after week 2 in the placebo group. Of 43 subjects
terazosin group had a quality of life at least "mostly satisfied"
24 (56%) responded in the terazosin group and 14 of 43
(primary response criterion) compared to 33% in the placebo
subjects (33%) responded in the placebo group (chi square
group. Of subjects in the terazosin group 60% had a greater
4.7, df 1, p ⫽ 0.03, fig. 2). Of 43 subjects 26 (60%) in the
than 50% reduction in the NIH-CPSI pain score (secondary
terazosin group had greater than 50% reduction in baseline
response criterion) compared to 37% in the placebo group
pain score at week 14 compared to 16 of 43 subjects (37%) in
(p ⫽ 0.03). Other outcomes were consistent with these find-
the placebo group (chi square 4.6, df 1, p ⫽ 0.03).
ings. Improvements in the mean NIH-CPSI total and domain
The terazosin group had a 57% reduction in mean NIH-
scores as well as the I-PSS at the final visit were all greater
CPSI total score (25.1 ⫾ 7.1 at baseline to 10.8 ⫾ 9.0 at week
in the terazosin group (p ⬍0.05). Patients who had lower
14, p ⬍0.001) versus a 37% decrease in the placebo group
baseline pain scores or were of ethnic Malay or Chinese
(27.2 ⫾ 7.7 at baseline to 17.0 ⫾ 12.1 at week 14, p ⬍0.001).
origin were more likely to respond to terazosin. Our data also
The 57% reduction in NIH-CPSI total score in the terazosin
suggest that 5 mg. terazosin should be given for at least 14
TABLE 1. Comparison of baseline demographic and clinical characteristics of patients
Median age (range)
0.68 (Mann Whitney U)
% Racial distribution:
0.68 (chi-square)
% Symptom duration (mos.):
0.32 (chi-square)
Mean prostate size (SD)
Mean ng./ml. PSA (SD)

TERAZOSIN FOR CHRONIC PROSTATITIS
TABLE 2. Other outcome measures
NIH-CPSI Quality of
NIH-CPSI Total Score
Peak Urinary Flow Rate Post-Void Residual
* Voided volume of at least 150 ml.).
† No significant difference between the terazosin and placebo groups with regard to baseline outcome parameters.
‡ Terazosin dose was escalated from 1 mg. daily for 4 days to 2 mg. daily for 10 days.
§ From week 2 and after terazosin dose was 5 mg. daily.
outlet function. Mayo et al found that few patients referred totheir prostatitis clinic had bladder outlet obstruction.18Urodynamic assessments of select patients in this study re-vealed no patients with bladder outlet obstruction (data notshown). ␣ Receptors are reported to be present in the humanbladder19 and may mediate relief of irritative urinary symp-toms experienced by subjects in this study. Also, an animalstudy showed that ␣ receptors exist in the spinal cord andganglia, suggesting that terazosin may affect these areas inthe central nervous system.20
Differences in the response rate of subjects from different
ethnic groups in our study suggest the possibility that theremight be more than 1 mechanism involved in the etiology ofchronic prostatitis/chronic pelvic pain syndrome. For exam-ple, the lowest rate of responders was among subjects of otherethnic origins, mainly foreign unskilled workers. It is possi-ble that they experienced greater stress that might exacer-bate prostatitis symptoms.
Our findings emphasize the importance of a placebo group
and double-blind assessment in studies of chronic prostatitis/chronic pelvic pain syndrome. The study was powered todetect a difference between the terazosin and placebo groups
FIG. 2. Box plot of NIH-CPSI quality of life (QOL) score (primary
despite the high placebo effect observed (33%). The popula-
outcome measure) of subjects who completed treatment with either
tion included carefully selected subjects who met the NIH
terazosin or placebo (43 in each arm). Bold line represents medianscore, upper and lower bounds of box 25th to 75th percentiles, re-
consensus criteria for chronic prostatitis/chronic pelvic pain
spectively, and bars maximum and minimum scores. At clinical end
syndrome. No subject was older than 50 years or had been
point of 14 weeks 56% responded to therapy (NIH-CPSI quality of life
treated previously with ␣-blockers. We used the NIH-CPSI
score 0 to 2, "mostly satisfied to delighted") in terazosin group com-
and other established outcome measures for patient assess-
pared to 33% in placebo group (chi-square 4.7, df 1, p ⫽ 0.03). T0, T2,
T6, T14, terazosin treatment at weeks 0, 2, 6 and 14. P0, P2, P6, P14,
ment. As terazosin was tittered to 5 mg. daily and given for
placebo treatment at weeks 0, 2, 6 and 14.
14 weeks, we do not know the efficacy of higher doses orlonger duration of treatment. We also do not know if terazo-sin changed the natural history of chronic prostatitis/chronic
weeks to obtain maximum response (fig. 2 and table 2). These
pelvic pain syndrome.
findings agree with previous data suggesting that terazosinand perhaps other ␣-blockers may have a role in treating
chronic prostatitis/chronic pelvic pain syndrome, especiallyin patients who have not been treated previously with these
Terazosin proved superior to placebo therapy for chronic
drugs. Our findings also agree with earlier recommendations
prostatitis/chronic pelvic pain syndrome as documented by
that ␣-blockers merit priority for research in chronic pros-
significant reductions in NIH-CPSI quality of life and pain
tatitis/chronic pelvic pain syndrome.5 Based on the primary
scores. In addition, terazosin also reduced the urinary and
and secondary response criteria, the results obtained were
quality of life impact scores of the NIH-CPSI as well as the
quite similar (56% and 60% for the terazosin group), suggest-
I-PSS. Our results support use of terazosin in patients with
ing that pelvic pain was an important determining factor in
chronic prostatitis/chronic pelvic pain syndrome who have
quality of life, consistent with published data that pelvic pain
not been treated previously with ␣-blockers. These findings
symptoms represent the predominant symptoms of chronic
support the need for further studies to determine the clinical
prostatitis/chronic pelvic pain syndrome.4, 17
characteristics of patients most likely to respond to
Terazosin improved lower urinary tract symptoms as doc-
-blockers, and the optimal drug, dose and duration of ther-
umented by decreases in the NIH-CPSI and I-PSS. However,
there was no difference in the mean peak urinary flow rate or
Drs. Chong Siang Tan, Chek Lang Ding, Chit Sin Loh and
post-void residual values between the terazosin and placebo
Keong Tatt Foo provided advice, support and comments; Dr.
groups. It is possible that terazosin improved the prostatitis
Prashanta K. Das and Mr. Leng Chee Leong provided labo-
symptoms by mechanisms other than changes in bladder
ratory support, and Mr. Kok Heng Heng, Ms. Siew Kin Yang,

TERAZOSIN FOR CHRONIC PROSTATITIS
Ms. Nohana Arif, Ms. Colina Wong and Ms. Jayalakshmi
bacterial prostatitis: a randomized placebo-controlled study.
Nagor assisted with the clinical work.
Arch Ital Urol Androl, 71: 283, 1999
11. Krieger, J. N., Nyberg, L., Jr. and Nickel, J. C.: NIH consensus
definition and classification of prostatitis. JAMA, 282: 236,
1. Nickel, J. C., Downey, J., Hunter, D. and Clark, J.: Prevalence of
12. Litwin, M. S., McNaughton-Collins, M., Fowler, F. J., Jr., Nickel,
prostatitis-like symptoms in a population-based study using
J. C., Calhoun, E. A., Pontari, M. A. et al: The National
the National Institutes of Health Chronic Prostatitis Symptom
Institutes of Health Chronic Prostatitis Symptom Index: de-
Index. J Urol, 165: 842, 2001
velopment and validation of a new outcome measure. J Urol,
2. Cheah, P. Y., Liong, M. L., Yuen, K. H., Teh, C. L. and Khor, T.:
162: 369, 1999
Chronic prostatitis: symptom survey with follow-up clinical
13. Meares, E. M., Jr. and Stamey, T. A.: Bacteriologic localization
evaluation. J Urol, suppl., 167: 27, abstract 109, 2002
patterns in bacterial prostatitis and urethritis. Invest Urol, 5:
3. Wenninger, K., Heiman, J. R., Rothman, I., Berghuis, J. P. and
Berger, R. E.: Sickness impact of chronic nonbacterial pros-
14. Barry, M. J., Fowler, F. J., Jr., O'Leary, M. P., Bruskewitz, R. C.,
tatitis and its correlates. J Urol, 155: 965, 1996
Holtgrewe, H. L., Mebust, W. K. et al: The American
4. Calhoun, E. A., McNaughton-Collins, M. and Oleary, M. P.:
Urological Association symptom index for benign prostatic
What is the economic impact of chronic prostatitis? J Urol,
hyperplasia. J Urol, 148: 1549, 1992
suppl., 165: 25, abstract 106, 2001
15. Casangrande, J. T. and Pike, M. C.: An improved approximate
5. Nickel, J. C., Nyberg, L. M. and Hennenfent, M.: Research guide-
formula for calculating sample sizes for comparing binomial
lines for chronic prostatitis: consensus report from the First
distributions. Biometrics, 34: 483, 1978
16. Kirk, R. E.: Split-plot design—factorial design with block treat-
Network. Urology, 54: 229, 1999
6. Barbalias, G. A.: Prostatodynia or painful male urethral syn-
ment confounding. In: Experimental Design: Procedures for
drome? Urology, 36: 146, 1990
the Behavioral Sciences. California: Brooks/Cole Publishing
7. Osborn, D. E., George, N. J., Rao, P. N., Barnard, R. J., Reading,
Co., pp. 245–318, 1968
C., Marklow, C. et al: Prostatodynia-physiological character-
17. Krieger, J. N., Egan, K. J., Ross, S. O., Jacobs, R. and Berger,
istics and rational management with muscle relaxants. Br J
R. E.: Chronic pelvic pains represent the most prominent
Urol, 53: 621, 1981
urogenital symptom for "chronic prostatitis." Urology, 48: 715,
8. Neal, D. E., Jr. and Moon, T. D.: Use of terazosin in prostato-
dynia and validation of a symptom score questionnaire.
18. Mayo, M. E., Ross, S. O. and Krieger, J. N.: Few patients with
Urology, 43: 460, 1994
"chronic prostatitis" have significant bladder outlet obstruc-
9. de la Rosette, J. J., Karthaus, H. F., van Kerrebroeck, P. E., de
tion. Urology, 52: 417, 1998
Boo, T. and Debruyne, F. M.: Research in ‘prostatitis syn-
19. Malloy, B. J., Price, D. T., Price, R. R., Bienstock, A. M., Dole,
dromes': the use of Alfuzosin (a new alpha 1-receptor-blocking
M. K., Funk, B. L. et al: ␣ -Adrenergic receptor subtypes in
agent) in patients mainly presenting with micturition com-
human detrusor. J Urol, 160: 937, 1998
plaints of an irritative nature and confirmed urodynamic ab-
20. Ishizuka, O., Persson, K., Mattiasson, A., Naylor, A., Wyllie, M.
normalities. Eur Urol, 22: 222, 1992
and Andersson, K.: Micturition in conscious rats with and
10. Lacquaniti, S., Destito, A., Servello, C., Candidi, M. O., Weir,
without bladder outlet obstruction: role of spinal alpha
J. M., Brisinda, G. et al: Terazosin and tamsulosin in non
1-adrenoceptors. Br J Pharmacol, 117: 962, 1996
Source: http://www.prostatitis-forum.com/docs/terazosin.pdf
14 Other Important Primary In addition to the major primary immunodeficiencies described in other chapters, there are other less common, but wel -described, immunodeficiencies. These less common disorders can be classified into four categories: Less common antibody deficiencies Less common cel ular deficiencies Less common phagocytic cel deficiencies Less common innate immune defects
Lara et al, Cancerología 1 (2006): 283-295 Manejo del Paciente Terminal Argelia Lara Solares, Antonio C. Tamayo Valenzuela, Sandra P. Gaspar Carrillo Unidad de Medicina del Dolor y Paliativa. Instituto Nacional de Ciencias Médicas y Nutrición "Salvador Zubirán" A Terminal disease is by definition, an advanced progressive and not curable il ness that does not respond to a specific